Herniated Disc
What is a Herniated Disc?
A herniated disc occurs when the soft, gelatinous center of an intervertebral disc ruptures out through a weak area in the tough outer layer of the disc. This inner portion then protrudes and presses against the nerves of the spine. Ruptured discs and slipped discs are other names for herniated discs.
Introduction
The spine is made up of bones called vertebrae that stack on top of each other, with an intervertebral disc in between each vertebra that allows for flexibility. These discs act as shock absorbers and also allow a range of motion.
Each disc has a tougher fibrous outer band called the annulus fibrosus and a soft, jelly-like center called the nucleus pulposus. When the annulus fibrosus weakens due to injury or repeated stress, it can tear and allow the nucleus pulposus to extrude. This is called a herniated disc.
Location
Herniated discs can occur along the entire length of the spine, but are most common in the lumbar (low back) and cervical (neck) regions.
Cervical Spine: This is the neck region, containing 7 vertebrae labeled C1 to C7.
- C1-C2: The top two vertebrae connect to the skull. Herniated discs are rare here due to limited mobility.
- C3-C4 & C4-C5: Middle neck area. Discs here can press on nerve roots leading to symptoms like neck pain and stiffness, muscle weakness, and tingling or numbness in shoulders, arms, and hands.
- C5-C6 & C6-C7: Lower neck, where the spinal cord transitions into the nerves of the spinal column. Most common sites for cervical disc herniations. In addition to nerve compression symptoms, herniations here may affect control and strength of the diaphragm or shoulder.
Thoracic Spine: The mid back or upper trunk area with vertebrae T1 to T12.
- Less common area for disc herniations but can occur between mid-back vertebrae. May cause radiating chest pain, abdominal discomfort, or changes to sensation in the trunk.
Lumbar Spine: Lower back containing vertebrae L1 to L5. The highest frequency of herniated discs is due to mobility and stress factors.
- L4-L5 and L5-S1 levels: Over 90% of lumbar herniated discs occur at these bottom two levels. L4-L5 allows for lumbar flexion and rotation while L5-S1 enables bending and heavy lifting. High mechanical stress makes injury here very common.
- L3-L4: Approximately 5% of lumbar herniations. Can allow disc material to compromise L3 or L4 nerve roots.
- L1-L2 and L2-L3: Least common lumbar levels, each accounting for only 1-3% of herniations. Still can generate symptoms like low back pain that radiates down the hips and thighs.
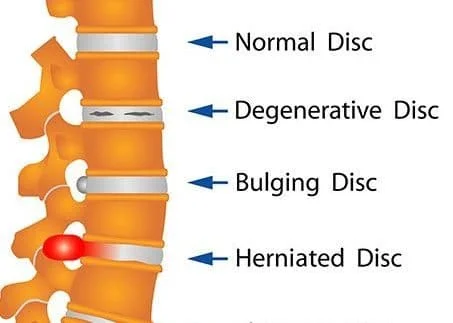
Types and Stages of Disc Herniation
Types of Herniated Disc
- Posterolateral Disc Herniation: Typically, the protrusion of the disc occurs in the posterolateral direction towards the vertebral canal. The protruded disc tends to compress the nerve that is immediately below it as the nerve passes through the level of the disc towards its foramen. For instance, when the disc at the level of L5 protrudes, it usually affects the S1 nerve.
- Cental (posterior) Herniation: This type of herniation is less common. When a disc protrudes above the second vertebra, it may compress the spinal cord itself or result in Cauda Equina Syndrome.
- Lateral Disc Herniation: In this case, the compression of the nerve root occurs above the level of herniation. The L4 nerve root is frequently involved in lateral disc herniation.
Stages of Herniated Disc
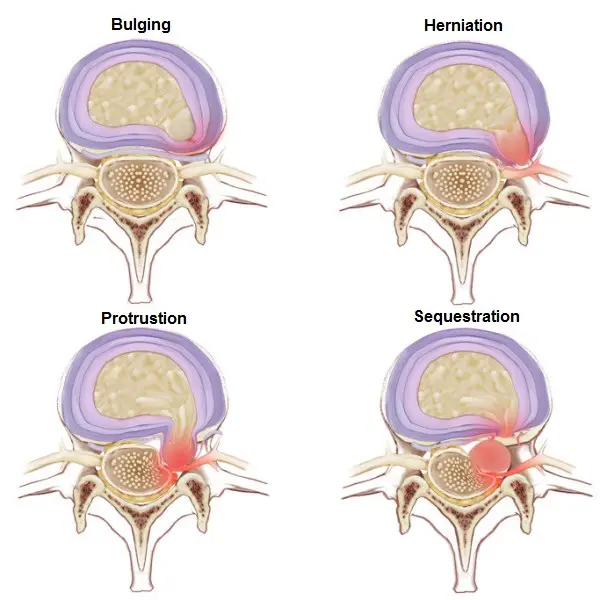
Bulging Disc:
- During this stage, the disc margin extends beyond the nearby endplates of the vertebrae.
- The posterior longitudinal ligament remains intact.
- The annulus fibrosus, the tough exterior of the disc, experiences pressure from the nucleus pulposus, the jelly-like substance inside the disc.
- Symptoms that may be observed include localized pain and stiffness.
Disc Protrusion:
- The disc bulges even more beyond its normal boundaries.
- The posterior longitudinal ligament remains intact.
- The annulus fibrosus is affected by the pressure from the nucleus pulposus.
- Symptoms that may be experienced include pain that radiates, tingling and weakness in the affected nerve distribution.
Disc Extrusion:
- The disc ruptures, causing the nucleus pulposus to partially escape through the annulus fibrosus.
- There may be a partial rupture of the posterior longitudinal ligament.
- Symptoms become more pronounced, including severe pain, numbness, and muscle weakness.
Disc Sequestration:
- This is the most severe stage, where the nucleus pulposus completely separates from the disc.
- The nucleus pulposus can move away from the disc space.
- Symptoms that may occur include intense pain, nerve compression, and potential complications like cauda equina syndrome.
Causes of Herniated Disc
Several factors can lead to or contribute to the development of a herniated disc. The main causes include:
Degenerative Disc Disease
As intervertebral discs age, they lose flexibility and elasticity. The outer ring becomes more brittle and susceptible to cracks and tears. This natural aging and “wear and tear” of the discs is known as degenerative disc disease, and makes disc herniation much more likely.
Injury/Trauma
Improper Lifting
Lifting heavy objects incorrectly is a frequent cause of disc injury. Rounding the back during lifting puts tremendous pressure on the discs. Twisting while lifting also strains areas like the lumbar discs.
Car Accident
The sudden force of an impact from a vehicle accident can tear or rupture discs. Whiplash injuries during collisions also commonly lead to cervical disc herniations.
Fall
The impact of falling onto the lower back or neck can traumatically injure discs and allow disc material to herniate.
Repetitive Strain
Regular activities like improper posture during sitting or repetitive motions lead to microscopic tears in the outer disc layers. Over time, these small injuries can accumulate, weakening the structure of the disc and making herniation more likely.
Obesity
Excess body weight puts heightened and constant strain on many structures including spinal discs, and often accelerates disc degeneration. Abdominal obesity can also contribute to increased compressive loading. This makes injury or tears more likely over time.
Smoking
Coughing puts pressure on the spine, and the chemicals in cigarettes have been shown to contribute to disc degeneration. As such, smoking is considered a risk factor for developing disc herniations.
Age
Disks degenerate as part of the natural aging process. As people get older, their discs start to lose structural integrity, increasing the risk of herniation. Most herniated discs occur in people ages 35-50.
Symptoms of Herniated Disc
A herniated disc can cause a variety of symptoms ranging from mild to severe depending on the level of nerve compression. Common symptoms include:
Pain
Sharp, Shooting Pain
A major symptom is sharp bursts of pain from the compressed or inflamed nerve. This occurs more frequently when changing positions or moving.
Dull, Aching Pain
Many sufferers also have dull, constant pain from the mechanical injury and inflammation. This ranges from mild to severe.
Radiating Pain
Radiating pain follows the distribution of an affected nerve root. Sciatica refers to pain radiating down the leg along the sciatic nerve from a lumbar disc herniation. Cervical radiculopathy causes radiating arm pain.
Increased Pain with Coughing/Sneezing
This occurs because these actions increase intradiscal pressure, putting more compression on the nerve root.
Numbness/Tingling Sensations
Compression and inflammation of the nerve can lead to abnormal nerve signaling felt as burning, tingling, or numbness along the nerve pathway into the extremity. Numbness often occurs in the hand or foot of the affected side.
Muscle Weakness
Nerve inflammation or compression can cause decreased strength or coordination of the muscles supplied by that nerve. Hand grip weakness can manifest from a cervical herniation. Foot drops can be seen in cases of lumbar herniation.
Lack of Coordination
Nerve compression affects the transmission of position sense and muscle action potential. This leads to problems with balance or coordinated movement like tripping frequently.
Bowel/Bladder Changes
In rare severe cases, a large lumbar herniated disc in the lower spine can significantly compromise the cauda equina nerve roots controlling bowel and bladder function. This requires prompt surgical treatment.
Diagnosis
Diagnosing a herniated disc often starts with a thorough medical history and physical examination, then typically involves imaging tests to confirm the herniation.
Physical Exam
A physician completes an in-depth neurological exam testing various aspects of nerve function to determine if they indicate a compressed nerve from a herniated disc.
Reflex Testing
Abnormal or diminished reflexes can indicate nerve damage. Doctors test reflexes in the arms and legs, like the knee-jerk reflex using a reflex hammer.
Sensation
Tests A pinprick or light touch test checks sensation in different dermatomes (patches of skin) corresponding to specific nerves. Numbness or dulling of sensation can indicate nerve involvement.
Muscle Strength Tests
Testing the strength and function of muscles in the arms, legs, or torso helps determine if they are impacted by nerve damage. Shoulder abduction strength or foot dorsiflexion may be assessed.
Tension Signs Tests like the straight leg raise putting tension on the sciatic nerve help determine the level of nerve root impingement. Positive signs cause radiating pain.
Balance and Coordination Testing
The patient is assessed walking normally, walking on their toes, and hopping on one foot. The inability to properly perform these due to limb weakness or numbness indicates a neurological deficit.
Imaging Tests
If physical exam findings suggest a herniated disc, the physician will order imaging scans to confirm and visualize the herniation.
- MRI Scan: The gold standard imaging test due to its detailed visualization of soft tissues like disc material and nerve roots.
- CT Scan: Can provide images of herniated disc material pressing on the spinal canal or nerve roots.
- X-ray: Helps rule out other spinal issues like fractures. Limited utility for directly viewing disc herniations.
Discogram
A discogram involves injecting dye into a disc space to view tear patterns in affected discs using X-ray or CT imaging. It helps identify discs that are causing pain.
Treatment of Herniated Disc
Nonsurgical Treatment
Most patients with a herniated disc will improve with conservative nonsurgical therapy for 6-12 weeks. The main components involve medication, physical modalities, lifestyle changes, and time for the injury to heal.
Medications
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are often first-line medications to reduce nerve inflammation and provide pain relief.
- Muscle relaxants such as cyclobenzaprine or tizanidine can relieve painful muscle spasms associated with disc herniations.
- Oral corticosteroids such as prednisone taken on a short taper schedule can rapidly decrease localized swelling and inflammation around damaged nerve roots.
- Some patients also benefit from topical medications such as lidocaine patches or menthol gels applied locally for pain.
Epidural Steroid Injections
- Injecting corticosteroid medication into the epidural space surrounding irritated spinal nerve roots provides targeted anti-inflammatory effects.
- Can reduce pain signaling and allow patients to participate more fully in physical therapy.
- Effects are temporary but injections may be repeated.
Alternative Therapy Approaches
- Chiropractic adjustments can realign areas of vertebral subluxation.
- Acupuncture helps relieve localized pain.
- Massage therapy loosens tense muscles.
- Mindfulness therapy and biofeedback decrease the perception of pain.
Lifestyle Modifications
- Losing weight reduces mechanical load on the spine.
- Smoking cessation limits disc degeneration and symptoms.
- Proper ergonomics and modifying activities prevent further injury.
Surgical Treatment
If conservative treatment fails, the herniated disc is severely compressing neural structures, or the patient has significant pain, numbing, and muscle weakness, surgery may be warranted.
Discectomy
- The goals are removing the herniated portion of the disc and decompressing affected nerve roots.
- Is performed open or microscopically with small incisions.
- The surgeon accesses the disc space and removes loose disc fragments or cartilage pressing on nerves.
- The procedure takes 1-2 hours with patients going home the same day or the next morning.
- Up to 90% see relief of leg pain but low back pain may continue.
Laminectomy
- Involves removing the lamina bone and ligaments surrounding the spinal canal.
- Creates more space and allows the nerve roots and spinal cord to shift away from pressure.
- Often done in combination with a discectomy.
- Recovery takes 2-4 weeks with restrictions on bending and lifting temporarily.
Spinal Fusion
- Removes the damaged disc and permanently joins two vertebrae together using bone grafts.
- Adds stability but reduces flexibility and range of motion due to the loss of a disc.
- May utilize metal screws, rods, or cages to enhance bony fusion.
- Takes approximately 3 months for complete bone fusion to occur.
Disc Replacement
- The damaged intervertebral disc is removed and a prosthesis implant is inserted in the disc space.
- Composed of metal and plastic with a rubbery nucleus.
- The goal is to reduce pain while approximating healthy spine biomechanics.
- Quicker recovery than fusion but longer-term device durability remains unknown.
Choosing the appropriate surgery relies heavily on shared decision-making between the physician and patient based on symptom chronicity/severity and patient age, health status, occupation, goals, risk tolerance, and surgical approach offered by the spine surgeon.
Physical Therapy Treatment
Physical therapy is a core component of conservative treatment for a herniated disc, with important benefits for reducing nerve compression and restoring function.
Goals of Physical Therapy
- Decrease pain and inflammation
- Improve spine and core muscular support
- Increase flexibility and range of motion
- Optimize biomechanics and movement patterns
- Prevent the recurrence of injury
Modalities to Reduce Pain and Inflammation
Heat therapy
- Heating pads, hot packs, warm compresses
- Increase blood flow, and relax muscles
- Reduce pain signals and muscle spasms
Cold therapy
- Ice packs, gel packs
- Reduce inflammation, swelling
- Numb areas temporarily
TENS unit
- Use electrodes on the skin over the back
- Sends small electrical impulses along nerve pathways
- Helps block pain signals
Ultrasound
- Use sound waves directed at the herniated disc
- Creates deep heat to promote healing
Traction tables/devices
- Motorized tables that gently pull or elongate the spine
- Takes pressure off nerve roots and discs
Exercises
Exercises for Herniated Disc Recovery
Rest on the Belly
- Lie on your stomach with your head turned to the side and your arms resting by your sides.
- Focus on relaxing and releasing the muscles in your lower back.
- Maintain this position for 2 minutes.

Prone Press-Up
- Begin by lying on your stomach with your palms on the bottom just above your chest.
- Push your upper body off the floor while holding your lower back and buttock muscles relaxed.
- Stay in this position for 5 seconds and complete 10 press-ups.
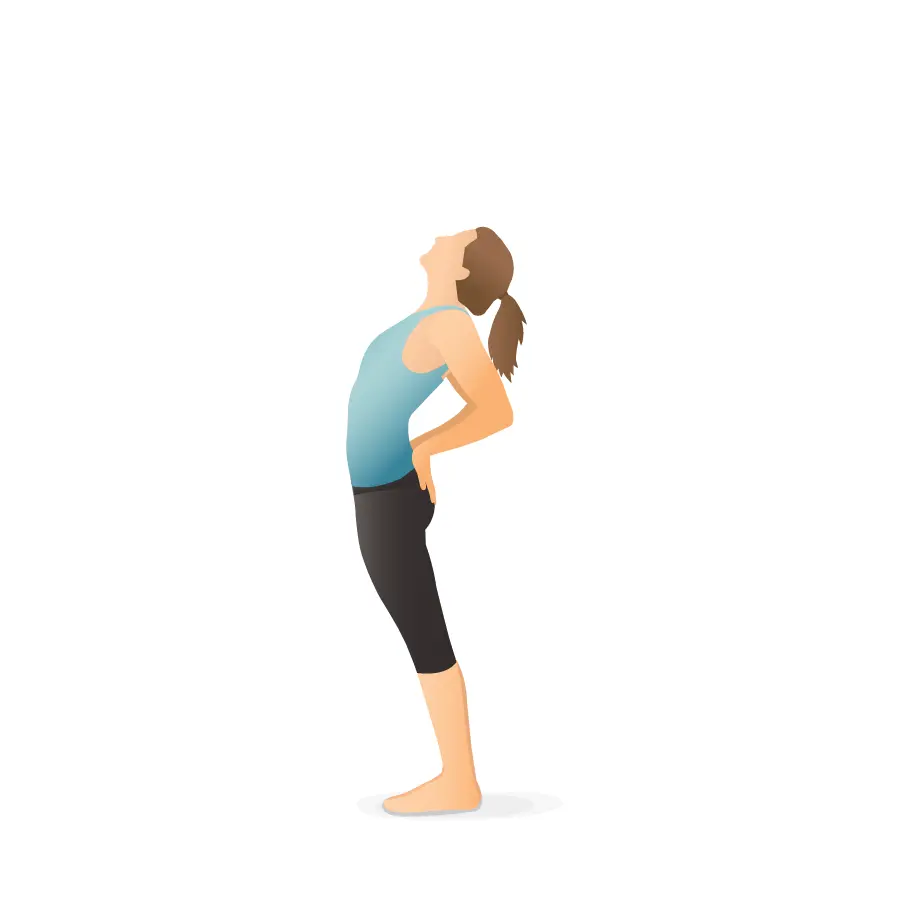
Backward Bend
- Stand with your feet shoulder-width separated and put your hands on your waist.
- Slowly lean backward without closing your knees, going as far as is comfortable.
- Hold this standing for a few seconds before replacing it with an upright stance.
- Aim for 2 to 4 repetitions.

Cervical Retraction
- Sit in a chair with your arms at your sides and gaze straight ahead.
- Gently pull your chin backward, as if creating a slight double chin, without shrugging your shoulders or shaking your head.
- Maintain this position for 1 to 2 seconds before releasing the pressure in your neck. Complete 10 retractions.
Exercises for Herniated Disc Strengthening

Lateral Neck Flexion
- Look straight ahead and gradually lean your ear towards the shoulder on the impacted side of your neck.
- Avoid lifting your shoulders during this movement.
- Go as distant as you can without experiencing additional pain, and hold this position for a moment before returning to the starting point.
- Complete 2 to 3 sets of 10 repetitions.

Side Plank
- Lie on your side with your knees inflated and your forearm positioned under your shoulder.
- Lift your hips and knees off the ground while keeping your body from leaning backward.
- Keep this position for 15 to 30 seconds before dropping back down.
- Repeat this exercise 2 to 3 times on each side of your body.
Bird Dog
- Position yourself on all fours.
- To stabilize your lower back, contract your abdominal muscles.
- Extend one arm in the act of you while simultaneously raising the opposite leg behind you.
- After five seconds of holding this position, switch to the other arm and leg and repeat the exercise.
- Do ten reps on each side in total.
Dead Bug
- Lying on your back, put your feet flat on the ground and bend your knees.
- Flatten your lower back against the floor by contracting your abdominal muscles, and raise both arms upward.
- Slowly lift one foot a few inches off the ground, simultaneously pushing the arm on the same side a few inches over your head.
- Return your arm and foot to their starting positions and repeat the movement on the opposite side.
- Rotate back and forth until you complete 15 repetitions with each arm and leg.
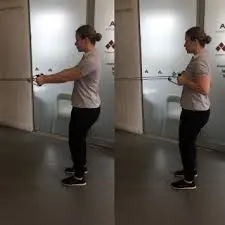
Shoulder Row
- Attach a resistance band in a doorway and hold one end of the band in each hand.
- While keeping your shoulder blades together, pull both arms back.
- Make sure to bypass shrugging your shoulders during this exercise.
- Perform 2 to 3 sets of 10 rows.
Bridge
- Bend your knees while resting on your back with your feet flat on the floor.
- Tighten your abdominal muscles and lift your buttocks off the ground, maintaining a pain-free range of motion.
- Hold this position for 10 seconds before falling back down.
- Complete 1 to 2 sets of 10 repetitions.
Movement and Exercises to Avoid
There are some kinds of motions and activities you should avoid if you have a disc herniation and are experiencing symptoms. These consist of:
- Leaning down or lifting anything and rounding your back.
- Heavy objects need to be lifted or held far from your body.
- Wearing shoes with high heels.
- Prolonged sitting or standing.
- Any additional activities that aggravate your pain.
- Furthermore, it’s critical to stay away from any movements that make your symptoms worsen and extend into your arms or legs.
Manual Therapy Techniques
Soft tissue mobilization
- Massage, myofascial release
- Relax paraspinal musculature
Spinal manipulations
- High-velocity thrusts to mobilize fixed spinal segments
- Improve mobility and movement patterns
Manual traction
- The therapist provides traction with specialized equipment
- Creates more space for nerve roots
Patient Education
- Body mechanics for lifting/bending
- Ergonomic optimization at work
- Disc protection strategies with activities
- Identifying and modifying exacerbating factors
- Home exercise program
Functional Training
- Maintaining activity tolerance
- Gradual return to work duties
- Simulating occupational or sports motions
- Progressively increase weight-bearing
A personalized physical therapy program lasting 4-6 weeks can resolve symptoms and restore movement for many patients, correcting underlying mechanical dysfunctions.
Prevention
While herniated discs sometimes occur spontaneously or due to unpreventable trauma, there are many proactive steps individuals can take to lower future risk.
Core Muscle Strengthening
- Developing strong abdominal and back muscle groups helps stabilize and support the spine.
- Targeted core programs improve muscle recruitment with activities.
- Yoga, Pilates, and other floor exercises that brace core muscles during movement are beneficial.
Use Proper Body Mechanics
- Maintain a neutral spine posture when lifting, and lowering objects properly using the legs.
- Bend at the knees and brace the core muscles during reaching or rotational movements.
- Avoid lifting and twisting simultaneously.
Optimize Ergonomics
- Set workstations, car seats, and mattresses at proper heights to reduce awkward bending postures.
Manage a Healthy Body Weight
- Excess weight puts more loading stress across spinal structures.
- Losing weight minimizes compressive and shear forces, especially during physical activity.
Stop Smoking
- Smoking limits blood flow to discs and other tissues, increasing disc degeneration.
Stay Active
- Moderate exercise 3-4 times per week maintains mobility and core stability.
- Avoid long sedentary periods with frequent positional changes.
Implementing prevention strategies makes it less likely that the intervertebral discs will develop damage over time or degenerate prematurely due to overloading or nutritional loss. Patients may still require periodic evaluation and guided care from a physical therapist or other healthcare provider to optimize spinal health.
Summary
A herniated disc, often referred to as a slipped or ruptured disc, occurs when the soft inner nucleus of an intervertebral spinal disc protrudes out through a tear in the tougher exterior and presses against the nerve roots or spinal cord. This most frequently occurs in the lumbar spine and cervical spine due to increased mobility and stress factors.
Symptoms of a herniation include localized pain, burning sensations, or numbness that radiates outward from the injury site, corresponding to the affected nerve distribution. Muscle weakness may also manifest. MRI is the gold standard for diagnosis, providing detailed imagery of the disc protrusion and nerve compressions.
Initial treatment focuses on non-surgical options for most patients, combining anti-inflammatory medications, physical therapy modalities, ergonomic modifications, and lifestyle changes. Surgery like a discectomy to cut out the herniated portion may be warranted for more severe compressions causing neurological deficits or intractable pain.
Preventative measures to reduce future risk include building core and spinal stabilizer strength, utilizing proper mechanics with bending and lifting, managing weight, and ensuring proper spinal health through routine activity and exercise. Implementing a proactive self-care approach makes it less likely that the intervertebral discs will prematurely degenerate or herniate due to excessive stresses and loads over time. Being informed on the causes, signs and symptoms of disc issues can also facilitate earlier diagnosis and intervention when needed.
FAQs
What is a herniated disc?
A herniated disc occurs when the jelly-like inner portion of an intervertebral disc breaks through a weak spot in the tougher exterior and presses on the nerve roots. This can cause pain, numbness, and weakness.
Where do herniated discs occur?
Herniated discs are most common in the lumbar spine (lower back) and cervical spine (neck) areas which undergo the most movement and stress. Over 90% of lumbar herniations occur at the L4-L5 and L5-S1 spinal levels.
What causes a herniated disc?
Common causes include repeated lifting with improper form, trauma from a fall or accident, or general wear and tear that weakens the exterior of the disc over time. Genetics and lifestyle factors like smoking also play a role.
What are the symptoms of a herniated disc?
Symptoms include localized back pain at the herniation site, shooting pain in the arms or legs, numbness/tingling, muscle weakness, and changes in reflexes. Pain may increase with coughing, sneezing, or straining.
How is a herniated disc diagnosed?
Diagnosis typically begins with a doctor evaluating symptoms and performing a physical exam to assess nerve function. If a herniation is suspected, imaging like an MRI can confirm the diagnosis and locate the herniated disc.
How are herniated discs treated?
Most patients improve with nonsurgical treatment involving medications, physical therapy, lifestyle modifications, and time. Surgery like a discectomy may be considered if conservative treatment fails and symptoms are severe.
What helps prevent herniated discs?
Prevention focuses on core strength training, proper body mechanics when lifting/bending, weight control, smoking cessation, and staying active. Routine exercise and movement nourish the spinal discs to maintain flexibility and shock absorption.
References
- Herniated disk – Symptoms and causes – Mayo Clinic. (2023, October 24). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/syc-20354095
- Disc Herniation. (n.d.). Physiopedia. https://www.physio-pedia.com/Disc_Herniation
- Lumbar Disk Disease (Herniated Disk). (2022, September 14). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/lumbar-disc-disease-herniated-disc
- Herniated Disc – Symptoms, Causes, Prevention and Treatments. (n.d.). https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Herniated-Disc
- Ocs, T. P. D. (2023, October 27). 16 Exercises for Herniated Disc (Back or Neck) Pain. Verywell Health. https://www.verywellhealth.com/exercises-for-herniated-disc-7642792#toc-movements-and-exercises-to-avoid
- Professional, C. C. M. (n.d.). Herniated Disk (Slipped, Ruptured, or Bulging Disk). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12768-herniated-disk#diagnosis-and-tests
- https://principalspineonline.com/wp-content/uploads/2021/10/Herniated-Disc2.jpg






17 Comments