Traction
What is Traction Therapy?
One kind of treatment called traction involves exerting a longitudinal strain on the spine’s axis. In other words, sections of the spinal column are tugged in opposite directions to stabilize or modify the position of injured spinal segments. The force is generally given to the head by a series of weights or a fixation device, and the patient must remain in bed or wear a halo vest.
A physical treatment technique called traction is used to lessen strain on painful spinal discs. Traction is a manual stretch of the spine that releases pressure on the discs that are causing the discomfort.
Cervical traction is often conducted manually, mechanically, or motorized (with a head or chin sling) or with a supine posterior distraction device. Mechanical cervical traction was performed in the supine position to lower head weight while increasing resistance. This posture also provides for better control of the head by the patient and is often more comfortable.
Lumbar traction takes substantially more force to divert the vertebral segments than cervical traction. Some of the traction equipment that is frequently utilized include an auto traction table, a split traction table, an inversion, and a thoracic or chest belt with a pelvic belt. Split traction tables feature two halves: one movable and one fixed. Auto traction tables allow both table segments to move independently and are controlled by the patient.
By pulling on an overhead bar, the patient applies active traction and assumes the least uncomfortable posture. The patient then uses his or her feet to operate a bar that alternates between compressive and distracting stresses.
Mechanism of action:
Several hypotheses have been offered to explain the potential therapeutic benefits of traction treatment. Distracting the motion segment is hypothesized to alter the location of the nucleus pulposus about the posterior annulus fibrosus or the disc-nerve contact.
These effects are feasible based on research into the biomechanics of the lumbar spine during traction therapy. In addition to separate vertebrae, traction has been demonstrated to enhance foraminal space and lower nucleus pulposus.
However, mechanical abnormalities discovered in a prone position are unlikely to continue when a patient resumes an upright, weight-bearing posture. Traction treatment’s impact on the mechanobiology of the motor segment or brain tissues increases the likelihood of a long-term therapeutic response.
Complicating matters further is the fact that not all traction treatments provide the same force to the spine, and animal studies have shown that the mechanobiology of the disc is sensitive to the amount, duration of loading, and frequency.
Some kinds of traction may accelerate disc or joint healing while others promote tissue degeneration. Although these characteristics have not been well investigated, even in animal models, what we know about disc mechanobiology should alert us to the likelihood that not all traction treatments are the same. Diverse traction techniques may result in differing clinical outcomes if interfering with disc and joint mechanobiology is impacted by the spine.
Systematic evaluations of lumbar traction treatment have seldom taken into account the possibility of varied effects depending on force and duration. Patients with a wide range of clinical complaints have commonly participated in traction trials, including back-dominant lower back pain (LBP), leg-dominant LBP, or both.
A patient with just dominant LBP and no radiculopathy, on the other hand, is most likely experiencing pain from a sclerotome source, such as facet joints or a disc, whereas sciatic pain, even if caused by disc herniation, can be exclusively neural. Although it is fair to believe that traction therapy impacts various illnesses differently, there is inadequate data to support this claim.
Distraction manipulation and positional distraction differ mechanically from typical traction (intermittent or continuous). Instead of allowing pressure to travel throughout the lumbar tissues, these therapies try to concentrate it on a specific location. AT, for example, allows the patient to concentrate the force by locating the position that most reduces their pain and using distraction in that position.
Distraction manipulation, which chiropractors and physical therapists most commonly employ, is conducted on treatment tables that allow the operator to control the direction and time of the distractive force. These methods include the FD (Cox) approach, the Leander technique, and the Saunders Active Trac method, among others.
What percentage of body weight must be used?
When choosing the appropriate traction weight, two things need to be taken into account:
Determine the weight that can overcome friction between the body and the bed, as well as the force necessary to affect the lumbar spine.
Judovich demonstrated that overcoming friction requires a traction force equal to 26% of the patient’s body weight.
The use of a split tabletop with frictionless rollers reduces this to negligible proportions. In its absence, a force greater than 26% of the body weight is required to generate any impact on the lumbar spine.
Optimal weights for traction have been examined under the assumption that intervertebral enlargement or decrease of disc protrusion provides the traction effect; however, only the former has been empirically demonstrated. Despite the investigations, it is unknown how much power is necessary to have the desired impact on the complete human spine.
The mechanism by which traction exerts its effects is not entirely known, and neuromodulation of pain, which may necessitate very little weight, must also be considered. However, healthcare specialists recommend employing motorized traction on a friction-free surface and including a variety of traction weights in their treatment plans. Maitland advises 10 to 65kg, with an average of 30 to 45kg; Grieve says 13 to 34kg.
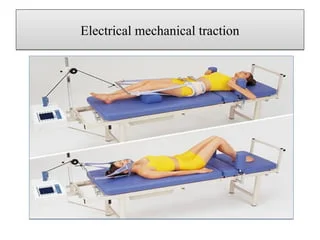
Motorized traction is the most fascinating form of traction since it is the only one that can be effectively standardized and is widely utilized in clinical practice. It is also the only type of traction that can be accurately standardized in terms of weight applied.
What are the different forms of traction therapy?
Spinal traction treatment can be performed manually or mechanically, depending on your requirements.
- Manual traction:
Manual spinal traction involves a physical therapist using their hands to hold patients in a traction position. Then they use manual force on the joints and muscles to enlarge the gaps between the vertebrae. In most cases, the traction phase is brief. Manual traction may appear scary, but it is a safe therapeutic option that can be beneficial for some conditions. - Mechanical traction:
Extending the muscles and spinal vertebrae is known as mechanical traction, a specific therapeutic technique. Mechanical traction permits continuous or intermittent stretching on a traction table while administering heat, vibration, and/or massage.- These tables can employ computer-based methods to apply precise pressure levels and/or fluctuations. Mechanical traction is not recommended for individuals with significant bone illnesses such as osteoporosis, osteomyelitis, and bone malignancy, as well as those with heart disease and spinal cord disease.
- It is also unsuitable for people who have spinal fractures or arthritis. To guarantee efficacy and safety, this sort of treatment should only be considered after a thorough examination and diagnosis and under the supervision of a licensed physical therapist or doctor.
How does it work?
A disc is a circular structure located between each vertebra in the spine. It has a strong outer covering that protects fragile inside tissue. When a disc is compressed and damaged, the tough outer layer is destroyed, and the soft inside protrudes through the gap.
The protrusion compresses adjacent nerves, producing discomfort. Traction moves the vertebra away from the disc, relieving pressure on it. As a result, the disc’s soft portion can now return to the disk. This decompresses the nerve and relieves pain. it also helps to rehydrate the disc.
Traction relieves pressure on the spine and lowers pain. Cervical traction and lumbar traction are similar, but there are several major distinctions. Cervical traction involves gently stretching or pulling the head away from the neck. Lumbar traction uses mild force to separate the pelvis from the lower back. Both of these therapies are successful in manipulating the spine while providing ease.
Benefits of Traction Therapy:
Traction Therapy is particularly successful in treating chronic neck and spinal cord pain.
Muscle relaxation
The problem is that the spinal column’s position puts too much strain on the muscles. As a result, the muscles are continually being stressed. However, traction will assist to relax the muscles and relieve tension.
Pain alleviation
The applied force facilitates the controlled straightening of the spinal column. It will relieve the pressure that might otherwise create pain. It will also provide a better physical environment, accelerating the healing process.
Avoid surgery
You can easily avoid surgical procedures by choosing a mechanical way of pain management and spinal realignment. The therapist or the machine will use the appropriate force.
promotes total recovery
Accurate pressure applied on the disc releases healing nutrients, triggering your body’s intrinsic healing mechanism. Of course, it will promote a speedier overall recovery.
Complements other treatments
The procedure does not need any surgery. As a result, enduring further therapies such as heat and cold therapy, electric stimulation, and ultrasonic applications is entirely safe.
The entire procedure is minimally invasive. However, you may only get the benefits if you go through the procedure with inexperienced practitioners who have enough expertise and understanding to do mechanical or manual treatments.
Physiological Effects of Traction:
Traction produces the most repeatable consequence in the cervical spine: elongation. In a famous research, Cyriax reported using 300 pounds of force manually, resulting in a 1 cm increase in cumulative lumbar spine interspace distance.
Studies have indicated that 25 pounds is the ideal weight for cervical traction to achieve vertebral separation. Furthermore, it has been demonstrated that with 25 pounds of tractive force or more, the cervical spine may be elongated by 2-20mm. Studies have shown that the anterior intervertebral region has the greatest rise in cervical flexion at 30°.
Traction in the extended position is typically not suggested since it causes discomfort and increases the risk of consequences from vertebral basilar insufficiency or spinal instability. Once friction has been overcome in the lumbar spine, the primary physiologic impact of traction is elongation. Researchers have discovered that the expansion of lumbar interspaces requires between 70 and 300 pounds of force.
This widening averaged somewhat more than 3 mm at one intervertebral level. The duration of the dissociation is unknown, however, studies have shown distractions lasting 10-30 minutes following treatment.
Traction-induced lumbar disc dimensions and pressure alterations have not been conclusively studied. Decreases in intradiscal pressure with 50-100 pounds of traction have been observed, although there is evidence that certain applications increase intradiscal pressure.
Because of this, the findings are unclear, although there is strong evidence to suggest that the herniated portion of an abnormal lumbar disc may temporarily reduce when traction is applied.
According to certain beliefs about the physiological consequences of traction, stimulating proprioceptive receptors in the spinal ligaments and monosegmental muscles can change or block aberrant neural input from those structures. There is limited scientific evidence to support this theory on the physiology of traction, as with others.
What conditions can be treated with traction therapy?
The process of traction is used to stretch soft tissues and separate bone fragments or joint surfaces. The force applied must be sufficient in magnitude and duration in the right direction while opposing the body’s movement with an equal and opposite force. People with particular spinal disorders benefit from this treatment, which is most typically used to treat;
- Slipped discs.
- Bone spurs.
- Degenerative disc disease.
- Herniated discs.
- Facet illness.
- Sciatica.
- Foraminal stenosis 8: Pinched nerves
- Cervical Spondylosis
- Lumbar Spondylosis.
What does traction therapy feel like?
Traction therapy is an effective method for releasing pressure on the spine or other regions of the muscular and skeletal system. Here’s how traction therapy feels:
Stretching feeling: During traction therapy, patients often feel a slight stretching feeling in the targeted location. This stretching helps to decompress the spine or joints, reducing pressure and increasing relaxation.
soothing: Traction treatment is soothing for many patients because it reduces muscular tension and increases blood flow to the afflicted region.
Mild Discomfort: While traction therapy is typically well-tolerated, some patients may suffer little discomfort or soreness during or after the procedure, especially if the traction force is excessively powerful or performed improperly.
How does cervical traction work?
There are two kinds of cervical traction:
Manual cervical traction: Your healthcare professional will grasp your head and gently move it away from your body. They will normally pull on your neck in various positions or degrees of flexion.
Mechanical cervical traction: You will lie down while your healthcare practitioner places your head and neck in a cervical traction device. There are several sorts of devices they may utilize, but all of them contain a mechanism for gently tugging on your head to create room in your neck. Mechanically cervical traction often lasts longer than manual cervical traction since the device requires not much exertion from your healthcare professional.
How is spinal traction administered?
Spinal traction treatment can be performed manually or mechanically, depending on your requirements.
Manually spinal traction is when an exercise therapist uses their hands to place patients in a traction position. Then they use manual force on the joints and muscles to enlarge the gaps between the vertebrae.
Mechanical spinal traction involves lying on a table with specially designed equipment to stretch the spine. A physical therapist will utilize a rope, slings, or pulley to relieve pressure on your body mechanically.
What does spinal traction accomplish?
Spinal traction extends the spine, relieving pressure on pinched discs. This straightens the spine and increases the body’s ability to mend itself.
Several forms of lumbar traction have been described.
The first method is mechanical traction, which involves a device and a partitioned table.
[1] The gadget applies a specified amount of stress to produce the traction. The patient wears a harness with two rings for support.
[2] Autotraction also uses a table separated into two portions, with the patient providing traction force by pulling with the arms and/or pressing with the feet.
[3] Finally, the therapist does manual traction by pushing on the patient’s ankles. Another method of manual traction is for the patient to place his legs over the therapist’s shoulders, while the therapist places his arms on the patient’s thighs and pulls.
[4] Continuous traction is used for several hours with a minimal amount of weight. Sustained traction is shorter in duration yet has a higher tension force.
[5] Intermittent traction is identical to continuous traction, except that it alternates between providing and releasing traction force at regular intervals.
How many traction therapy sessions will a patient need?
The patient’s health, the intensity of their symptoms, and their response to therapy will all determine how many traction therapy sessions are needed in total. Traction treatment often consists of multiple sessions spaced out across weeks or months. Your physiotherapist will evaluate your progress and modify your treatment plan accordingly.
What are the possible side effects of traction therapy?
While traction treatment is deemed safe for most people, some possible adverse effects include:
1: Muscle Spasms: Traction treatment can cause muscle spasms in certain people, particularly if the force is excessively strong or performed incorrectly.
2: Soreness: Some patients may feel transient soreness or discomfort in the treated region after traction treatment. This is often moderate and resolves on its own.
3: Nerve Irritation: In rare cases, traction treatment may worsen nerve problems in certain people, causing further pain or suffering. Proper approach and monitoring can assist in reducing this danger.
4: Skin Irritation: The traction device may cause minor skin irritation or redness at the contact locations. Ensuring adequate cushioning and modifications might assist in avoiding this.
Risks of spinal traction:
Spinal traction does not pose any long-term dangers. Some adverse effects may appear during or following therapy. Many patients get muscular spasms following traction. Some people are experiencing discomfort in the treated locations. Spinal traction isn’t for everyone. Based on your medical history, a physician can decide if the dangers outweigh the possible benefits.
Spinal traction can have several consequences. For example, traction can help:
- Reduce compression forces and distract vertebral bodies. It may assist in mobilizing the facet joints of the spine. This can improve the intervertebral space where spinal nerves leave, reducing discomfort.
- Enhance disc and nerve nutrition.
- Decrease muscular spasms.
- Stretch the muscles and connective structures of the spine.
- Improve circulation and reduce joint discomfort in the spine.
- Spinal elongation and flattening of curvature in the spine.
It may assist with the following spinal conditions:
- Nerve pain and paralysis down the arm and legs caused by disc and nerve injuries; radiculopathies
- Advanced degenerative changes in the spine and stenosis
- biomechanical joint stiffness in the spine
- Your physical therapist should carefully evaluate your situation to determine whether spinal traction is suitable. Your signs and symptoms determine this, the severity of your injury and stage of recovery, your prior and present medical history, and your reaction to previous therapy. When carefully and correctly chosen by you and your physical therapist, spinal traction can be an effective therapy option.
Precautions When Applying Spinal Traction:-
- Joint hypermobility.
- Acute inflammation.
- Claustrophobia or anxiety related to traction
- The risks of cardiac or respiratory insufficiency
- Pregnancy (increased ligamentous laxity, danger of abdominal compression)
- Traction can worsen symptoms, and utilizing a chin strap may cause TMJ dysfunction (cervical).
Contraindications of traction therapy:
- Acute strains
- Sprains
- Inflammation
- Respiratory problem
- Claustrophobia
- Conditions include osteoporosis and infection.
- Tumour
- Rheumatoid arthritis
- Pregnancy
- Cardiovascular illness
- Hernia
- Cauda equina syndrome
- Neoplasms
- Pott’s Disease and all inflammatory disorders of the vertebrae
- Vascular or cardiac illness, and breathing issues
- Post-operative patients within three months following back surgery
FAQs
What is the purpose of traction therapy?
Traction treatment is intended to ease pain, reduce pressure, and enhance the spine’s range of motion and flexibility.
Any adverse effects or hazards related to traction therapy?
While traction therapy is usually regarded as a safe method of pain relief, there are certain risks, such as momentary pain or discomfort, headaches, dizziness, and nausea. Side effects can be minimized by ensuring that the therapeutic force is properly calibrated and delivered exclusively by a skilled and competent physical or occupational therapist.
Under what conditions is traction used?
Intermittent traction is often the chosen therapy for degenerative disc disease and/or joint hypomobility. On the other hand, prolonged traction is most commonly used to treat neck discomfort caused by disc herniations, muscles, or soft tissues.
What are the different forms of traction used in physiotherapy?
Manual traction, mechanical traction, and positional traction are three forms of traction used in physiotherapy, all of which seek to relieve pain and promote joint mobility by controlled force application.
What are the advantages of traction devices?
Begin rehydrating, then increase the disc height.
Strengthen the discs, ligaments, and tendons.
Assists in preventing injury.
Helps damaged tissues recover faster and improves injured joints.
Increase the nourishment and lubrication of your spinal joints.
References
- P. (n.d.). Effective Traction Therapy at Physiotattva. PhysioTattva. https://www.physiotattva.com/therapies/traction-therapy
- What is Traction Therapy? What conditions are treated by Traction Therapy? Who will benefit from Traction Therapy? (n.d.). Cbphysiotherapy. https://cbphysiotherapy.in/therapies-offered/traction-therapy
- Lumbar Traction. (n.d.). Physiopedia. https://www.physio-pedia.com/Lumbar_Traction
- Professional, C. C. M. (n.d.). Cervical Traction. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/23093-cervical-traction
- V. (2023, October 17). Use of Traction in Physiotherapy: Spinal Lumbar Cervical Traction. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/use-of-traction-in-physiotherapy/







2 Comments