Rheumatoid Arthritis
What is a Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by inflammation of the synovial joints, leading to pain, stiffness, and swelling. Unlike osteoarthritis, which primarily affects cartilage, rheumatoid arthritis targets the lining of the joints, known as the synovium, causing damage and eventually resulting in joint deformity and disability.
Early RA is described as having symptoms for less than six months, whereas established RA has symptoms for more than six months.
Rheumatoid arthritis (RA) is a chronic (long-term) autoimmune disease primarily affecting joints. RA arises when the immune system, which usually protects the body from infection and disease, targets its tissues. The condition causes joint discomfort, swelling, stiffness, and loss of function.
Additional aspects of rheumatoid arthritis may include the following:
- It affects the joint lining, causing tissue destruction to the ends of the bones of a joint.
- RA usually presents symmetrically, which means that if one knee or hand is affected, the other hand or knee is likely to be as well.
- It may damage the joints of the wrists, hands, elbows, shoulders, feet, spine, knees, and mouth.
- RA can induce fatigue, fevers, and loss of appetite.
- RA can cause medical problems in regions other than the joints, including the heart, lungs, blood, nerves, eyes, and skin.
- No laboratory test can identify rheumatoid arthritis. Patients with rheumatoid arthritis require both pharmaceutical and non-pharmacological therapies. Today’s standard of care is early treatment with disease-modifying anti-rheumatic medications.
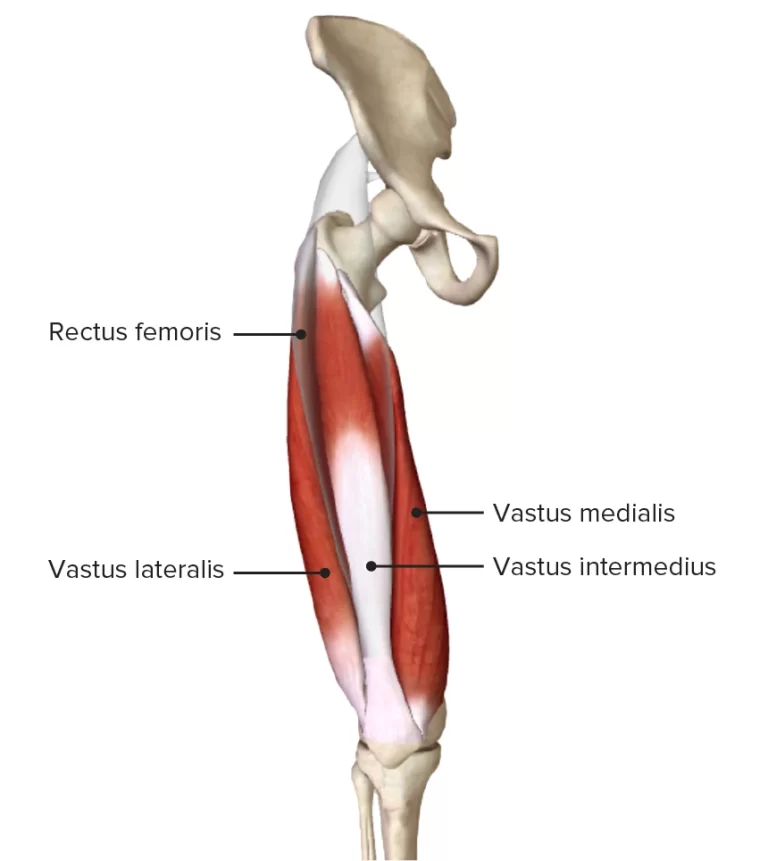
Anatomy
A joint connects the ends of two or more bones. The body has several types of joints, the most common of which is the synovial joint. These joints, such as the knee, hip, and shoulder, are designed to facilitate mobility.
Strong connective tissues known as ligaments and tendons connect the bones of a synovial joint to each other as well as the surrounding muscles that stabilize the joint. The ends of bones are cushioned with articular cartilage, a slippery substance that allows the bones to slide smoothly across each other during movement.
Synovial joints are surrounded by a thin layer of tissue known as synovium. The synovium secretes hyaluronic acid and other chemicals that lubricate and make the joint easier to move.
Tendons that pass through narrow tunnels (known as tendon sheaths) are also surrounded by synovium, which helps them glide through the tunnels. These sheaths are located in the fingers, wrists, ankles, and toes. Tenosynovium refers to the synovial tissue that exists within tendon sheaths. Rheumatoid arthritis can occasionally affect tenosynovium, causing swelling in the tendon sheaths. When this occurs, tenosynovial tissue can infect and damage the tendons, causing them to rupture (partially or totally).
What happens during rheumatoid arthritis?
Doctors don’t understand why the immune system targets joint tissues. However, they are aware that rheumatoid arthritis can develop after a succession of events. This sequence of events includes:
- A combination of genetic and environmental factors initiates the development of RA.
- The immune system may become engaged years before symptoms arise.
- The autoimmune process may begin in other parts of the body, but the impact of the immune dysfunction is often concentrated in the joints.
- Immune cells create inflammation in the joint’s inner lining, known as the synovium.
- Chronic inflammation causes the synovium to thicken due to increased cell activity, protein production, and other variables in the joint, resulting in pain, redness, and warmth.
- As RA advances, the enlarged and inflamed synovium pushes further into the joint, destroying the cartilage and bone within.
- As the joint capsule extends, the forces alter the joint structure.
- Over time, the surrounding muscles, ligaments, and tendons that support and stabilize the joint weaken and cease to function properly. This might result in additional discomfort, joint damage, and difficulty using the affected joint.
Weakened ligaments can cause:
- Joint deformity.
- Contractures are severe tightness that causes the joint to shorten and harden.
- Increased pain.
Rheumatoid arthritis can affect blood vessels, skin, lungs, eyes, heart, and nervous system. It can cause poor bone mass and osteoporosis.
Early diagnosis and treatment of RA can help control the disease and prevent long-term damage to joints and other structures.
Epidemiology
The total prevalence is 0.5-1%, with women being 2-3 times more likely to get the condition.
Onset occurs in adulthood, with increases in the fourth and fifth decades. The pediatric condition Juvenile Idiopathic Arthritis (JIA) is discussed separately at the connection.
Causes of Rheumatoid arthritis.
The cause of this condition is unknown (probably multiple factors).
Genetics:
- An autoimmune response directed against synovial structures and other organs has been suggested to be caused by a genetic predisposition (for example, HLA-DR B1, the most prevalent allele of HLA-DR4 implicated in rheumatoid arthritis) and an environmental trigger (for example, Epstein-Barr virus, which has been proposed as a potential antigen but has yet to be proved).
- Activation of macrophages and synovial cells, as well as the production of cytokines (e.g., L4 and TNF), increase synovial cell proliferation and increase macrophage production of destructive enzymes (e.g., elastase and collagenase).
- B cell lymphocytes produce antibodies, including rheumatoid factor, causing immune complexes to deposit in tissues and contribute to further injury. Increased production of VCAM1 directly activates endothelial cells, increasing inflammatory cell adhesion and accumulation. RANKL then activates osteoclasts, resulting in subchondral bone destruction.
- Pannus is the result of an inflammatory response.
Pannus:
- It is an oedematous, thickened, hyperplastic synovium infiltrated with T and B lymphocytes, plasmocytes, macrophages, and osteoclasts.
- It will gradually break down exposed parts first, then the articular cartilage.
- Fibrous ankylosis eventually leads to ossification.
Environmental Factors:
- Smoking: Smoking is a major risk factor for getting RA, and quitting can greatly lower your risk.
- Age: While RA can develop at any age, it is most typically diagnosed between the ages of 40 and 60.
- Sex: Women are two to three times as likely as males to get arthritis.
- Other infections: While not conclusively confirmed, recent evidence suggests that some illnesses may cause RA in genetically sensitive individuals.
- Diet: Although dietary relationships are still being investigated, several studies suggest a correlation between specific dietary habits and RA risk.
- Obesity: Being overweight or obese increases your chances of acquiring RA.
- Environmental exposures: Certain medications, such as silica dust, asbestos, and secondhand smoke, may contribute to RA risk in some individuals.
Clinical Symptoms
Symptoms of rheumatoid arthritis may include:
- Tender warmed up, and swollen joints. Joint stiffness is typically more difficult in the mornings and after inactivity.
- Fatigue, fever, loss of appetite.
- The smallest joints are typically the first to be affected by early rheumatoid arthritis, especially those that unite your fingers to your hands and your toes to your feet.
As the condition advances, symptoms may spread to the wrists, knees, ankles, elbows, hips, and shoulders. In most cases, symptoms appear in the same joints on both sides of the body.
Approximately 40% of persons with rheumatoid arthritis develop non-joint symptoms. Areas that may be affected are:
- Skin, eyes, and lungs
- Heart Kidneys
- Saliva glands
- Nerve tissue
- Bone Marrow
- Blood vessels
Rheumatoid arthritis symptoms might be moderate or severe, and they may happen irregularly. Periods of increasing disease activity, known as flares, alternate with periods of relative remission, during which swelling and discomfort reduce or cease. Rheumatoid arthritis can cause joints to change form and move out of position.
Joint pain is at the forefront of rheumatoid arthritis symptoms. The symptoms of RA are:
- Polyarthritis of the hands’ tiny joints, including the proximal interphalangeal (PIP), metacarpophalangeal (MCP), and wrist. Some patients could have monoarticular joint involvement.
- Joint involvement typically develops gradually over months, however, in specific situations, it might occur over weeks or overnight.
- Other joints that are commonly affected are the wrist, elbows, shoulders, hips, knees, ankles, and metatarsophalangeal (MTP) joints.
- Morning joint stiffness might linger for several hours, but it is regularly more than an hour. Flexor tenosynovitis may have caused the patient to have a “trigger finger”.
Rheumatoid arthritis has advanced characteristics, including erosive subluxation of the MCP joints and ulnar deviation. The ulnar carpal articulation also shows significant degenerative changes. Take note of osteopenia, particularly in the MCP areas. Upon examination,
- Synovitis, which causes swelling, stiffness, deformity, and discomfort in the PIP, MCP wrist, and knee joints, can also result in a reduced range of motion.
- Deformity, discomfort, weakness, and restricted movement result in loss of function.
- Rheumatoid nodules can be found on extensor surfaces at elbows, heels, and toes in up to 20% of rheumatoid arthritis patients.
- Late in the course of the disease, patients may present with “boutonniere” (flexion at PIP and extension at DIP), swan neck (flexion at DIP and extension at PIP) deformities, MCP joint subluxation, and ulnar deviation.
- Other characteristics may include carpal tunnel syndrome, tenosynovitis, and finger abnormalities.
- Examine the joints for swelling, palpable pain, movement-related pain, restricted range of motion, distortion, and instability.
- Slow gait and a weak grip significantly predict functional degradation among RA patients.
Rheumatoid arthritis can damage practically all organs in the body.
- The most common complaints are pain, morning stiffness, and fatigue.
- Muscular strength, muscular endurance, and aerobic endurance are typically lower in rheumatoid arthritis sufferers than in healthy individuals.
- In 80-90% of patients with rheumatoid arthritis, the cervical spine is involved, which can cause instability due to ligamentous laxity (most commonly between the first and second cervical vertebrae). This instability can cause pain and neurological symptoms, such as headaches and finger tingling.
- Individuals with RA are eight times more likely to have functional disability than adults in the general population from the same community.
Classification of Functional Status
The American College of Rheumatology classified functional status in rheumatoid arthritis as follows:
- Class I: Completely capable of doing regular everyday activities (self-care, vocational, and avocational).
- Class II: Capable of doing routine self-care and vocational tasks, but limited in avocational activities.
- Class III: Capable of doing routine self-care tasks, but limited in vocational and avocational activities.
- Class IV: Limited capacity to undertake typical self-care, vocational, and social activities.
Diagnosis
Disease progression: Stages
- There are no damaging alterations on the X-rays.
- There is x-ray evidence of periarticular osteoporosis and subchondral bone loss, but no joint deformity.
- X-rays indicated cartilage and bone degradation, as well as joint deformity and periarticular osteoporosis.
- Bony or fibrous ankylosis combined with stage 3 features
The first step to effective RA treatment is to have an accurate diagnosis as soon as possible. A doctor with specialized training in arthritis treatment (known as a rheumatologist) is most qualified to provide an accurate diagnosis based on a medical history, physical examination, and lab testing.
Medical history.
Rheumatoid arthritis can be difficult to identify in its early stages due to the gradual progression of symptoms.
As part of the office visit, your doctor will take a comprehensive medical history, which includes questions about:
- Consider your overall health and
- the medications you take.
- Your joint pain and other symptoms – when they started and if they have altered over time.
- If you or a family member have a history of arthritis or any autoimmune problems
Physical exam.
The doctor will examine for joint soreness, swelling, warmth, painful or restricted movement, lumps under the skin, or a low-grade fever.
Throughout the physical examination, the doctor will look for:
- Signs of RA include swollen or painful joints, limited joint motion, and early deformity.
- Signs of irritated tendon sheaths in the wrists or hands Tendon ruptures (full or partial tears).
- Rheumatoid arthritis is commonly present bilaterally, so the doctor will examine both sides of the body.
Lab Tests
Certain blood tests may identify indications of RA:
- Rheumatoid factor is an antibody that is present in around 85% of persons with RA.
- Anti-CCP antibodies. Many persons with RA have antibodies to cyclic citrullinated peptides/proteins, which are more specific to RA than the rheumatoid factor.
- Erythrocyte sedimentation rate (ESR or “sed” rate) and C-reactive protein (CRP) are standard tests for measuring inflammation in the body. ESR and/or CRP levels are typically increased in RA patients.
- When analyzed collectively, these blood tests are extremely beneficial in diagnosing RA. It is crucial to highlight that rheumatoid arthritis can occur while having normal bloodwork (negative rheumatoid factor). When this occurs, the condition is known as seronegative rheumatoid arthritis.
Imaging testing.
Rays. X-rays produce images of dense structures such as bones. Because bone and joint deterioration develops later in the disease’s course, X-rays may be ineffective in diagnosing RA in its early stages, while soft tissue swelling around a joint can be visible on a standard X-ray.
Your doctor may, however, use X-rays to rule out additional possible conditions. If you have RA, your doctor may use periodic X-rays to check the disease’s progression.
RA can cause the ends of bones in a joint to wear down (erosions). An X-ray, ultrasound, or MRI (magnetic resonance imaging) scan may identify erosions. However, if they do not appear on the first tests, it may indicate that RA is in its early stages and has not yet caused bone damage. Imaging data can also indicate how well the treatment is working.
Diagnostic Criteria for Early-Stage Rheumatoid Arthritis
To help prevent RA from increasing to joint degeneration, the American College of Rheumatology has devised specific, thorough criteria to help doctors diagnose RA in its early stages.
In general, a positive diagnosis of RA can be obtained if the following criteria are satisfied:
- Inflammatory arthritis in three or more joints.
- Arthritis symptoms that have been maintained for at least 6 weeks
- Positive serological test: the presence of rheumatoid factor in blood and/or positive anti-CCP
- Increased erythrocyte sedimentation rate (ESR or “sed” rate) or high C-reactive protein (CRP)
- Other probable sources of symptoms have been ruled out.
If your doctor suspects you have RA, they may recommend you to a rheumatologist. Although your symptoms and the findings of a physical examination and testing may indicate RA, a rheumatologist can make an accurate diagnosis. There are additional, less frequent kinds of inflammatory arthritis to consider.
Diagnosis procedure: Rheumatoid arthritis patients’ lab assessment includes acquiring rheumatoid factor, an antibody against the Fc component of IgG. Approximately 45% to 75% of RA patients have rheumatoid factor. However, the presence of rheumatoid factor does not indicate rheumatoid arthritis. It can be found in connective tissue disorders, chronic infections, and healthy people, usually at low titers.
Anti-citrullinated protein antibodies (ACPA) are identified in around 50% of patients with early arthritis, who are later diagnosed with RA.
- Acute-phase reactants, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels may be raised during the active phase of arthritis.
- X-rays of both hands and feet are regularly done to check for erosions, a pathognomonic hallmark of rheumatoid arthritis (plain radiographs do not indicate early disease changes).
- MRI and ultrasound of joints detect erosions faster than X-rays. MRI and ultrasound are more sensitive than clinical examinations in detecting synovitis and joint effusion.
Differential Diagnosis
- Lupus
- Chronic Lyme disease.
- Osteoarthritis
- Septic Arthritis
- Psoriatic arthritis and Sjogren’s syndrome
- Sarcoidosis
Treatment of Rheumatoid Arthritis
The goals of RA treatment include:
- Stop or reduce inflammation to the lowest possible degree (remission).
- Relieve symptoms.
- Avoid joint and organ damage.
- Improve functionality and general well-being.
- Minimise long-term problems.
The doctor will utilize the next techniques:
- Early and intensive treatment to lessen or eliminate inflammation as soon as possible.
- Targeting remission or another objective (known as “treat-to-target”) to achieve minimal or no indicators of active inflammation.
- Tight management is used to limit inflammation to a minimum.
Treatment for rheumatoid arthritis aims to improve symptoms and slow disease progression.
Because the condition affects so many different organs, it is best addressed by an interprofessional team. The key is patient education by nurses, chemists, and primary care physicians. The nurse should educate the patient on the signs and symptoms of various organ systems and when to seek medical attention. To restore joint function, a physiotherapist should prescribe an activity program. An occupational therapy consultation can assist the patient with daily life activities. The chemist should inform the patient about the various medications used to treat rheumatoid arthritis and their potential negative effects.
Medical Management
The usage of drugs:
- Nonsteroidal anti-inflammatory medications (NSAIDs)
- Disease-modifying anti-rheumatic medications (DMARDs)
- There are three types of DMARDs: traditional synthetic (e.g. methotrexate, leflunomide, prednisolone), biological (e.g. TNF-α inhibitors like infliximab, tocilizumab, abatacept, rituximab), and targeted synthetic (e.g. tofacitinib).
- The condition causes a severe level of disability. Life expectancy is likewise decreasing, with extra death typically caused by non-articular symptoms.
Medical management involves the use of medications as The benefits of physical therapy interventions are extensively proven.
- Physical therapists play an important role in the nonpharmacological treatment of RA.
- Physiotherapy helps clients manage chronic pain and impairment by developing programs that address flexibility, endurance, aerobic condition, range of motion (ROM), strength, bone integrity, coordination, balance, and fall risk.
the four most typical components of physical and occupational therapy for RA hands are:
- Treatments provided include exercise therapy, joint protection recommendations, and functional splinting and assistive equipment.
- Massage treatment and patient education.
The therapy goals in the majority of situations are: Improved understanding of disease management, Improvements include:
- Pain relief,
- Improved daily activities,
- Reduced joint stiffness (range of motion).
- Prevent joint damage,
- Increase strength,
- Reduce tiredness,
- Improve quality of life, and improve aerobic condition.
- Improve stability and coordination.
Patient assessments, not joint counts, radiographic scores, or laboratory tests, are the most reliable predictors of severe 5-year outcomes in RA patients, such as functional status, employment impairment, expenses, joint replacement surgery, and premature death.
Physiotherapy Treatment
Exercise is an important component of a therapeutic plan. The physician and physical therapist may collaborate with patients to create an exercise program that strengthens the muscles surrounding affected joints without overworking them.
In some situations, your doctor may prescribe upper (arm) and/or lower (leg) extremity braces or splints for specific joints to assist relieve stress and avoid deformity.
- Cold/Hot Applications: cold for the acute phase, heat for the chronic phase, and used before activity.
- Pain is reduced with transcutaneous electrical nerve stimulation (TENS).
- Hydrotherapy-Balneotherapy: a workout that puts minimal strain on the joints.
- Joint Protection
- Massage Therapy: Massage and the manual trigger of an articular movement focused on improving the quality of function, pain reduction, disease activity, flexibility, and welfare (dimensions of depression, anxiety, mood, and pain).
Therapeutic Exercise
- Physical activity improves the patient’s physical capability.
- Exercise improves general muscular endurance and strength without affecting disease activity or discomfort in RA.
- Before beginning an exercise program, conduct an in-depth assessment of the circumstances, including joint inflammation (local or systemic), disease stage, patient age, and level of collaboration.
- Exercise therapy aims to improve everyday functioning and social involvement by increasing strength, aerobic capacity, range of motion, stability, and coordination.
Programs for Patients With RA
- Includes range-of-motion exercises, aerobic exercises, and stabilization/coordination exercises.
- Begin with a moderately intense fitness program.
- If possible, progress to a high-intensity training program to increase aerobic capacity, strength, and endurance.
Exercise
- In the acute phase, perform isometric/static workouts for 6 seconds and repeat 5-10 times a day with a weight of 40% 1RM. Chronic phase -> at least four repetitions of each joint in two to three days.
- These workouts increase joint mobility without loading it. Contractures can be held for six seconds and repeated five to ten times daily.
- Stretching should be avoided in acute situations.
- Strengthening
- Aerobic condition exercises: There are two divides of exercises for improving aerobic condition: intensive and moderate-intensive workouts. The difficult exercise therapy involves a minimum duration of 20 minutes per session, three times a week at an intensity of 65 to 90 percent of the maximal heart rate. Moderate-intensive exercise therapy requires a minimum duration of 30 minutes each session and is done five times a week at an intensity of 55 to 64 percent of the maximum heart rate. These exercises attempt to increase muscle endurance and aerobic capability. Examples include swimming, walking, and cycling.
- stabilized and coordinating exercises: Exercises that activate the sensorimotor system will help to improve the stability and coordination of a specific joint. For example, stand on a balance board.
- Motion control, balance, and coordination are all important things to consider throughout these workouts.
- Swimming, walking, and cycling are recommended conditioning exercises for people with chronic inactive RA.
The SARAH (Strengthening and Stretching for Rheumatoid Arthritis of the Hand) exercise program, shown in the table below, is part of routine daily activities. The SARAH experiment pits an intervention against conventional hand care. Standard care is combined with a hand and wrist training program that includes seven mobility exercises and four strength workouts against resistance.
- Use a modified Borg scale to determine the load (resistance) for strength workouts based on self-perception of effort.
- For each strength exercise, the patients’ perceived effort with their weaker hand determines the level of resistance.
- Exercise therapy for RA patients is used to improve daily functioning and social involvement by enhancing muscle strength, cardiovascular endurance, joint mobility, stability, and/or coordination.
- An active policy is preferred, particularly where the physiotherapist plays a supportive role.
- Individual situations may include passive therapies, such as manual surgeries.
Patient Education: providing information about their condition and the various therapies available to improve their quality of life. e.g., patients are taught how to protect their joints throughout normal life; altering their movement-behavior; and behavioral change by your patient (process with three phases: motivation, initial-behavioral change, and the phase where the intended behavior is maintained).
- Create achievable objectives with the patient.
- Provide adequate directions and ensure that the patient understands.
- Enough variety in the workouts is required to prevent boredom.
- The therapist must involve the partner and other important persons in the process since they play a vital motivational role. Also, the therapist must motivate the patient.
- Stay in touch with the patient to ensure that the treatment is helpful.
Management of flareups
- People with RA may also experience a phenomenon known as a “flare-up”. Typically, it occurs after experiencing a secondary disease, being involved in a high-stress environment, or overexerting oneself. What causes flare-ups is yet unknown. Strategies that can aid someone who is having a flare-up
- Balance is important; schedule plenty of downtime to reduce the likelihood of affected joints flaring up.
- Educate relatives, colleagues, and other people you deal with; they can assist you during flare-ups.
- Have a backup plan, be prepared in case of a flare-up, and become acquainted with warning signals for a flare-up.
Surgical Treatment
Your doctor may propose orthopedic surgery based on the level of cartilage damage and your reaction to nonsurgical treatments.
Synovectomy
A synovectomy removes the damaged synovial joint lining caused by rheumatoid arthritis, reducing discomfort and swelling.
Synovectomy may be useful if the disease is limited to the joint lining and has not already caused severe damage to the articular cartilage that surrounds the bones. Typically, the treatment is used to treat only the early stages of RA. The synovitis can come back (return) unless effective medical care is maintained. With the improved medical treatments available today, synovectomy is less common.
Tendon surgery
If tendons tear, reconstructive surgery can help restore function. Tendon repairs and transfers can be quite effective in the hand.
Trigger fingers and tenosynovitis in the hand and wrist may require:
- Partial release of tight tunnels
- and partial flexor tendon excision (removal) in the finger.
- Tenosynovectomy to avoid tendon ruptures.
Joint Rebalancing
During the early stages of rheumatoid arthritis, joints, particularly the tiny joints of the hands and fingers, can become loose and imbalanced, leading to deformities and contractures that impair function.
If the cartilage is still intact, a surgeon can use techniques to release tight structures, transfer tendons, and tighten loose ligaments to realign joint alignment and improve function. During joint replacement, bigger joints must be rebalanced to correct abnormalities and contractures.
Fusion
The most common RA surgery is the fusion of the afflicted joints. Fusion combines the two bones that make up a joint to produce a single bone. Fusions are most commonly used in foot and hand joints because they may reduce discomfort while maintaining full function.
During the procedure, the specific joint is exposed, and the remaining injured cartilage on each side is removed.
The ends of the two bones have been formed to fit tightly together and secured with screws or a combination of screws and plates. This keeps the bones from moving while allowing blood vessels and new bone-forming cells to cross the fusion site.
Fusion surgery removes motion from the joint, but patients rarely notice the loss of motion because the fusion makes the joint less painful and more stable, improving function. Orthopedic surgeons are trained to select the optimal position — angle or alignment — for the fused joint.
Because the mobility of the elbow, shoulder, hip, and knee is so important to proper function, fusions are rarely performed when joint replacement is an option. Ankle replacement has also become an option that is a possible alternative.
Joint Replacement Surgery
Joint replacement surgery can typically help restore painless joint movement. During this procedure, your doctor removes the damaged cartilage and bone before implanting new metal or plastic joint surfaces to restore joint function.
A combination of specialized tiny joint fusions and/or joint replacement greatly improves function, particularly in the hand. For key joints such as the elbow, shoulder, hip, and knee, these operations can represent the difference between incapacity and an active lifestyle.
Self Care
Working with your doctor to ensure you receive proper medical therapy is essential but you can also take steps on your own to manage your RA and relieve pain and fatigue. Diet, exercise, smoking cessation, and mental wellness are all important factors in maintaining good health and managing RA. Our pain resources can help you develop health goals and manage your discomfort.
- Healthy Eating. A balanced, nutritious diet that includes sufficient quantities of each food category promotes wellness and makes it simpler to maintain a healthy weight.
- Daily movement. Even if you don’t have time to exercise, work to include movement in your daily routine. Use the stairs instead of the elevator. Park in a location that requires you to walk a bit to get to a building. Travel to greater lengths to your office meeting.
- Balancing activity and rest. It is essential to keep physically active even during a flare, but rest is especially important when RA is active and joints are uncomfortable, swollen, or stiff. Rest helps to alleviate inflammation and fatigue associated with a flare. Taking breaks during the day protects joints and protects energy.
- Treatment options include both hot and cold. Heat therapies, such as heat pads or warm baths, are particularly effective for relieving stiff joints and weak muscles. Cold is ideal for acute discomfort and swollen joints. It may decrease pain and inflammation.
- Topical products. Creams, gels, and stick-on patches can help relieve joint or muscular pain. Some products contain medication, while others use nerve-irritating substances to alleviate pain.
- Stress reduction and complementary therapies. There are several methods for relaxing and shifting your concentration away from discomfort. Meditation, deep breathing, and imagining happy images are all examples. Massage can help relieve pain, relax tense muscles, and reduce stress and anxiety. Acupuncture involves placing small needles into the body at certain places to reduce pain. If you dislike needles, acupressure employs forceful pressure instead.
- Supplements. Curcumin/turmeric and omega-3 fish oil supplements have been shown in studies to relieve rheumatoid arthritis pain and morning stiffness. However, before taking any supplement, consult with your doctor about potential side effects and how they could interact with other medications you are taking.
- Positive Attitude and Support System. Create a network of friends, family, and coworkers who can offer emotional support. Take time to do things you enjoy to improve your mood and relax discomfort.
Risk Factor
- Increased RA frequency within families due to the combination of patient genetics and environment.
- Risk factors include female sex, occupational dust (silica), air pollution, high sodium and iron consumption, and low vitamin D levels. Smoking (seropositive for RA). Obesity and low socioeconomic status.
- Consumption of fish and omega-3 fatty acids, moderate alcohol consumption, a nutritious diet, oral contraception/hormone replacement therapy, and statin use all increase the chance of death.
You are more likely to develop rheumatoid arthritis if you have specific risk factors. This includes:
- Age. Although rheumatoid arthritis may occur at any age, the likelihood of developing the condition increases with age. Juvenile idiopathic arthritis, similar to rheumatoid arthritis, can affect children and young teenagers.
- Sex. Rheumatoid arthritis is more prevalent in women than in men. The disease affects approximately two to three times as many women as men. Researchers believe that reproductive and hormonal components may contribute to the disease’s development in some women.
- Family history and genetics. If you have a family history of RA, you may be more prone to the disease. Various genetic variables marginally increase the likelihood of developing RA.
- Smoking. According to research, long-term smokers are more likely to develop rheumatoid arthritis. For those who continue to smoke, the condition may improve.
- Obesity. According to some research, being obese may increase your likelihood of developing the disease while also limiting how much it may be addressed.
- Periodontitis. Gum disease may increase the risk of having RA.
- Lung diseases. Diseases of the lungs and airways may also cause the development of arthritis.
Precautions
- When the patient has an exacerbation and the joints are acutely inflamed, isometric exercises should be performed.
- Stretching should be avoided in acute situations.
- Revise the exercise program if pain continues two hours after the activity or if joint swelling increases.
- Patients with active rheumatoid arthritis in their knees should avoid mounting stairs or weight lifting, which can cause intra-articular pressure.
- Stretches should not cause too much stress on the tendons, and ballistic motions should be avoided.
Complications
RA has a variety of effects on people, including mortality, hospitalization, work incapacity, increased medical costs/expenses, decreased quality of life, and chronic pain. On average, chronic RA patients have two or more diseases. This is significant because of how comorbidities affect quality of life, functional status, prognosis, and outcome. Associated Complications Include:
- Infections
- Chronic anemia.
- Gastrointestinal cancers
- Pleural effusions.
- Osteoporosis
- Heart disease.
- Sicca Syndrome
- Felty Syndrome
- Lymphoma.
Damage to lung tissue (rheumatoid lung): CT shows significant pulmonary fibrosis in the mid and lower zones, as well as severe centrilobular emphysema in the upper zones. The fibrosis is caused by the patient’s known rheumatoid arthritis, whereas emphysema is the result of a long smoking history.
- Side effects of treatment and medicine.
- General deconditioning
- Complications of the neurological system
- Ocular complications
Rheumatoid arthritis raises the likelihood of developing:
- Osteoporosis. Rheumatoid arthritis, as well as awareness of the medications used to treat it, might raise your risk of developing osteoporosis, a condition that weakens your bones and makes them more prone to fracture.
- Rheumatoid nodules. These stiff tissue lumps typically grow at pressure areas like the elbows. However, these nodules can appear anywhere in the body, including the heart and lungs.
- Dry eyes and mouth. People with rheumatoid arthritis are more likely to develop Sjogren’s syndrome, a condition that causes a deficiency of moisture in the eyes and lips.
- Infections. Rheumatoid arthritis and many of the drugs used to treat RA can damage the immune system, leading to an increase in infections. Vaccinations can prevent infections like influenza, pneumonia, shingles, and COVID-19.
- Abnormal bodily composition. People with rheumatoid arthritis frequently have a larger proportion of fat to lean mass, even if their BMI is acceptable.
- Lung disease. People with rheumatoid arthritis are more likely to experience lung tissue inflammation and scarring, which may lead to shortness of breath over time.
- Lymphoma. The lymphatic system is the source of lymphoma, a type of blood cancer that is more common in people with rheumatoid arthritis.
Prognosis
Rheumatoid arthritis is chronic and progressing. Everyone has several exacerbations and remissions. Within ten years of being diagnosed with the condition, about half of all patients become disabled.
Aside from joint disease, individuals may experience a variety of other joint-related issues, which greatly affect their quality of life. The development of sickness varies by individual.
Rheumatoid arthritis is also related to cardiovascular risk factors, infections, respiratory disease, and the development of cancer. Patients with rheumatoid arthritis have a 2-3 times higher risk of death than the general population.
Conclusion
The prognosis for most patients with rheumatoid arthritis is unknown.
The condition has repeated relapses and remissions, with at least 40% of patients being disabled within ten years.
Some people have moderate disease, while others may have a severe disease that significantly reduces their quality of life.
Patients with a high self-antibody titer, HLA-DRB1 genotypes, age under 30, multiple joint involvement, female gender, and extra-articular involvement typically have poorer prognoses.
The medications used to treat rheumatoid arthritis have significant side effects that are frequently not well tolerated. As the condition advances, many individuals will experience unfavorable cardiac events that essentially to death. Result Criteria:
- Simplified disease activity (SDAI) index: tender joint count, swollen joint count, patient global assessment, physician global assessment, and CRP in mg/dL
- Clinical Disease Activity Index (CDAI): painful joint count, swollen joint count, patient global assessment, physician global assessment.
- DAS28-ESR (disease activity score) measures tender joint count, swollen joint count, patient global evaluation, and erythrocyte sedimentation rate in millimeters. DAS-Crp (disease activity score) measures tender joint count, swollen joint count, patient global assessment, and c reactive protein in milligrams/liter.
- The Rheumatoid Arthritis Disease Activity Index (RADAI-5) is A self-reported outcome measure consisting of five items in a Likert scale style that briefly evaluates the patient’s perceptions of their condition (both over the previous six months and current state).
- The DASH
- A 36-item short-form
- A fatigue severity scale.
FAQs
What is the best treatment for rheumatoid arthritis?
Use workouts and relaxation techniques to reduce pain and keep you busy. Communicate effectively with your healthcare team to get more control over your sickness. Get help to manage the physical, emotional, and mental effects of rheumatoid arthritis.
How does it feel to have rheumatoid arthritis?
Swelling, warmth, and redness
The lining of joints affected by rheumatoid arthritis becomes inflamed, causing the joints to swell and feel hot and sensitive to the touch. In certain people, hard swellings known as rheumatoid nodules may develop under the skin around damaged joints.
Can I function properly with rheumatoid arthritis?
Many persons with RA can lead healthy, active lives. For example, disease-modifying antirheumatic medications (DMARDs) have become an effective and widely available treatment for RA. These medications function by preventing the immune system and minimizing the harm they cause to joint tissue.
What’s the quickest approach to treating arthritis?
In many cases, arthritic symptoms can be alleviated by the following measures:
Weight loss,
Exercise. Regular exercise can help maintain joint flexibility.
Hot and cold. Heating pads and ice packs can help reduce arthritic pain.
assistive devices
What is Stage 1 rheumatoid arthritis?
During stage 1, there is inflammation within the joint. The tissue in the joint swells. For example, stage 1 RA in the hands can cause stiffness and pain in the finger joints and knuckles. These sensations typically disappear with movement.
Is rheumatoid arthritis serious?
Rheumatoid arthritis (RA) causes numerous physical and social repercussions, including a reduced quality of life. It can result in discomfort, incapacity, and early death. Premature heart illness.
Rheumatoid arthritis stays for how prolonged?
A flare can last a few hours, many weeks, or even longer. For some patients, medicines can help avoid attacks and keep symptoms from increasing. Medical medication and home remedies can help manage symptoms during a flare.
What are the top five vegetables to avoid for arthritis?
Some arthritis sufferers report that nightshade vegetables such as tomatoes, potatoes, eggplants, and peppers make their condition more serious. While there is not much proof that suggests a link between arthritis discomfort and most nightshades, tomatoes could be an exception. This is because they increase levels of uric acid.
What five foods are worst for arthritis?
Several foods can induce weight gain, increase inflammation, and exacerbate arthritic symptoms:
Sugary treats.
Refined carbs.
Foods that have been completely processed.
Drinks containing additional sugar.
Purines.
Alcohol.
Salty food
Can you live with RA without medication?
Because RA is a progressive condition, you cannot live with it without medical attention. If you do, the symptoms will worsen and become severe. Several natural therapies can help you relieve some of your problems. This includes using essential oils, receiving acupuncture, and more.
What is the lasting treatment for rheumatoid arthritis?
There is no cure for rheumatoid arthritis. However, clinical investigations have shown that early therapy with disease-modifying antirheumatic medicines (DMARDs) increases the likelihood of symptom remission.
Who develops rheumatoid arthritis?
Rheumatoid arthritis affects more women than men. The condition affects roughly two to three times more women than men. Researchers believe that reproductive and hormonal variables may contribute to the disease’s development in some women. Family History and Genetics
What is Stage 2 of RA?
Progression of Rheumatoid Arthritis: Stage 2 (Moderate)
The body will begin to produce antibodies, which can be observed in blood tests, causing the joints to swell and imaging to reveal genuine indications of inflammation. At this stage, the disease may cause inflammation in the lungs, eyes, skin, and/or heart.
How fast does rheumatoid arthritis spread?
Rheumatoid arthritis symptoms often appear gradually over several weeks, although rare instances may aggravate quickly over a few days. Symptoms vary from person to person. They can come and go and may vary with time.
References
- Rheumatoid Arthritis – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/rheumatoid-arthritis/
- Gout. (2024, January 30). Wikipedia. https://en.wikipedia.org/wiki/Gout
- Branch, N. S. C. A. O. (2023, July 27). Rheumatoid Arthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
- Rheumatoid arthritis – Symptoms and causes – Mayo Clinic. (2023, January 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
- Rheumatoid arthritis – Symptoms and causes – Mayo Clinic. (2023, January 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
- Rheumatoid Arthritis: Symptoms, Diagnosis, and Treatment | Arthritis Foundation. (n.d.). https://www.arthritis.org/diseases/rheumatoid-arthritis






44 Comments