Peroneal Nerve Injury
Peroneal nerve injury affects the peroneal nerve, which runs through the front of your legs and into your foot and toes. This nerve and its branches sense the tips of your feet and the sides and fronts of your legs. You can also point your toes upward and gain control over the muscles in your front and outside thighs.
This common nerve can be injured suddenly, gradually through compression, or as a result of complications from other diseases like diabetes or delivery. Peroneal nerve dysfunction is frequently caused by damage to the nerve that impairs movement or sensation in the foot and leg. This condition is also known as common fibular nerve dysfunction.
The most typical damage symptom is the inability to raise your toes with strength. The underlying cause determines the course of treatment, however, it may involve surgery or physical therapy. This article discusses peroneal nerve injuries, including their causes, risks, and available treatments.
What is the Peroneal Nerve?
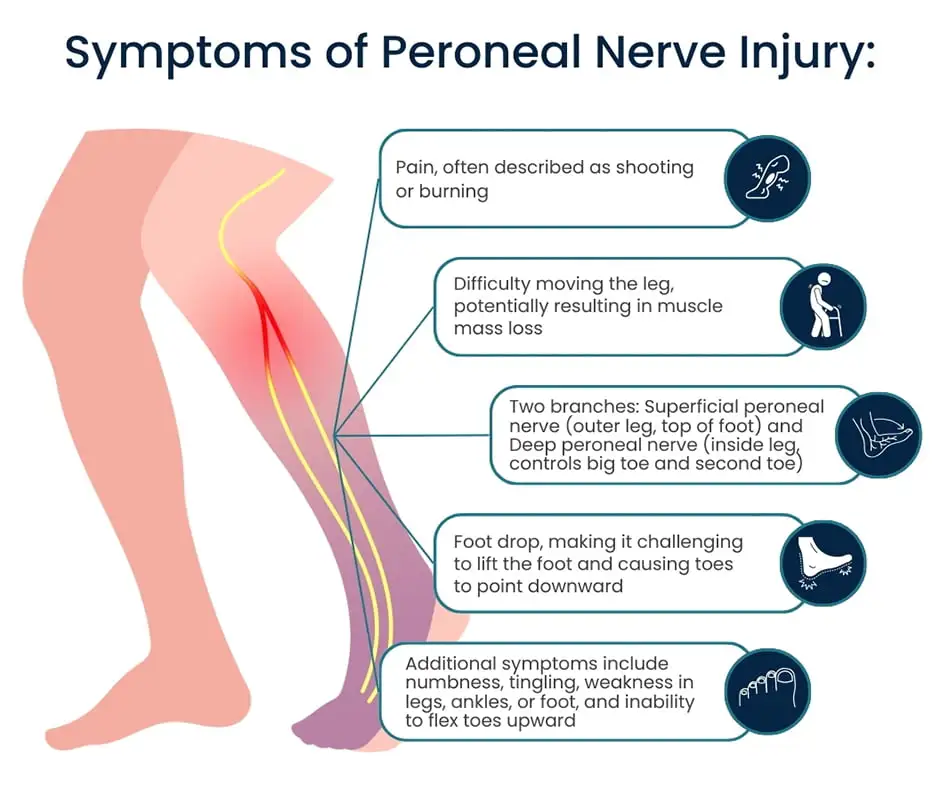
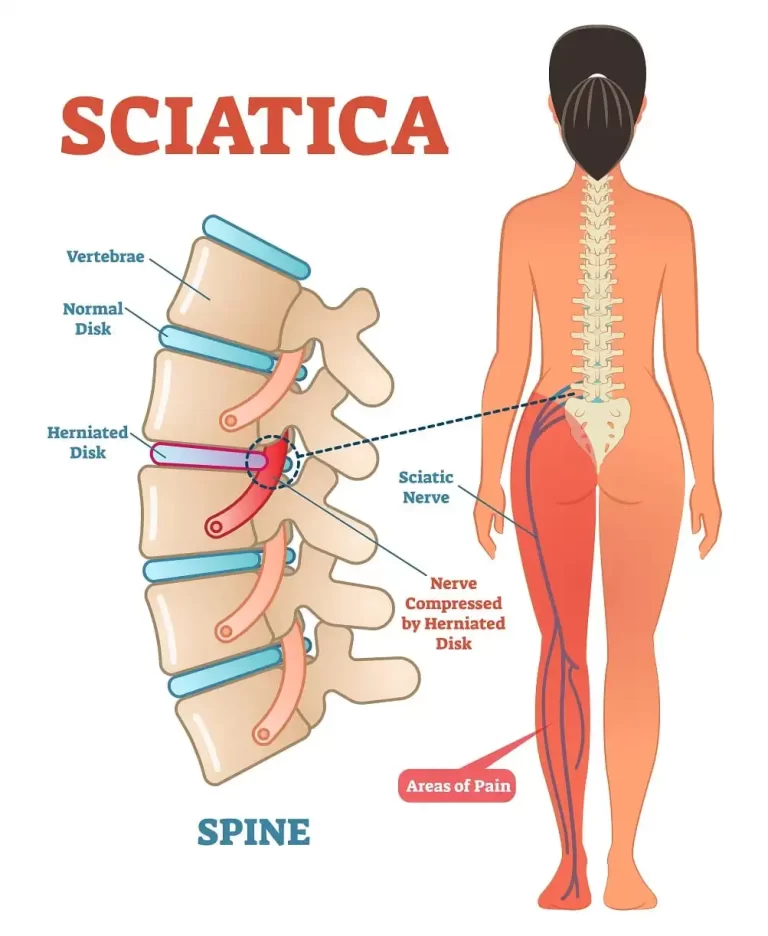
- The peroneal nerve, a crucial nerve in the rear of the thigh, divides from the sciatic nerve. The two smaller nerves that split off as the peroneal nerve travels down the leg are the superficial and deep peroneal nerves.
- The superficial peroneal nerve senses the skin on the outside of the lower thigh and the top of the foot. It also controls the muscles involved in everting, or turning, your foot outward.
- Because of the deep peroneal nerve, the skin on the top of the foot, between the big and second toes, is sensitive. It also controls the muscles that allow you to elevate your foot, or dorsiflex it.
What is Peroneal Nerve Injury?
- A peroneal nerve injury is a lesion to the nerve that passes through your front legs, reaching your toes and feet. This nerve greatly influences your lower leg and foot’s feeling and movement.
- A significant portion of your lower body’s feeling and movement is controlled by the sciatic nerve, a big nerve that starts in your lower spine. Two branches emerge from your sciatic nerve:
- The common peroneal nerve runs along the back and the outer edge of your lower leg, splitting into the superficial and deep peroneal nerves. The tibial nerve is the largest branch that runs down the back of your leg and ends in your foot.
- Damage to your common peroneal nerve or any of its branches is referred to as a peroneal nerve injury. Where the common peroneal nerve wraps across the top of your fibula is where it is most susceptible.
Causes of The Peroneal Nerve Injury
Traumatic and non-traumatic are the two primary types of causes of peroneal nerve injury.
Traumatic Causes
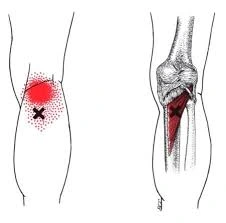
- A knee injury or trauma: One typical cause of damage to the peroneal nerve is this. Peroneal nerve injury can occur in as many as 40% of cases of dislocated knees. The smaller bone on the outside of the lower leg, the fibula, can break, and knee replacement surgery is another injury that can harm the peroneal nerve.
- Fibula injury or direct impact: The peroneal nerve, which circles the head of the fibula, might sustain direct injury from a fall, blow, or other trauma.
Not-Traumatic Causes
- Compression of the nerve: There are several reasons why the peroneal nerve may get compressed, such as:
- Tight splint or cast: An excessively tight splint or cast might injure the nerve by compressing it.
- Prolonged leg crossing: Prolonged leg crossing can put a strain on the peroneal nerve, which is located behind your knee.
- Extended bed rest: Individuals who experience peroneal nerve injury may be at a higher risk of developing this condition.
- Cysts or tumors: Rarely, a cyst or tumor close to the peroneal nerve may compress it and result in damage.
Medical conditions:
Several illnesses have the potential to harm nerves in the body, including the peroneal nerve. Among these prerequisites are:
- Diabetes insufficient in vitamin B12
- Charcot-Marie-Tooth disease: a collection of hereditary illnesses affecting the nervous system
- Lyme disease
- Additional: Peroneal nerve injury can also result from repetitive strain on the nerve, such as from prolonged kneeling or squatting.
Symptoms of The Peroneal Nerve Injury
Foot drop is the most typical sign of peroneal nerve damage. It is challenging to elevate the front of your foot off the ground when you have this ailment. Individuals who have foot drop may have a slapping gait, in which they elevate their knee over their normal walking height to clear the ground.
Additional signs of damage to the peroneal nerve can be:
- Discomfort, tingling, or numbness in the toes, top of the foot, or front of the lower leg.
- The foot or ankle weakness.
- Having trouble everting (or turning outward) the foot.
- loss of lower limb muscle mass.
The degree of nerve injury will determine how severe the symptoms are. Some people may only feel a slight tingling or numbness in certain situations. In other situations, they could be unable to raise their foot at all and have a total foot drop.
Risk Factors of The Peroneal Nerve Injury
Several things can make you more susceptible to peroneal nerve damage. These can be broadly divided into two groups: actions that compress the nerve and underlying conditions.
Conditions That Predispose
Age: Older persons are more likely to sustain peroneal nerve damage. This is most likely caused by several things, such as aging-related neuropathy (nerve damage) and decreasing muscle mass.
Medical conditions: Several illnesses have the potential to harm nerves in the body, including the peroneal nerve. As an example, consider:
- Diabetes: Nerve damage, or neuropathy, can be brought on by diabetes. The possibility of peroneal nerve damage may rise as a result.
- Vitamin B12 deficiency: The health of your nerves depends on vitamin B12. Neuropathy and an elevated risk of peroneal nerve damage can result from a deficit.
- Charcot-Marie-Tooth disease: A collection of hereditary conditions known as Charcot-Marie-Tooth disease impacts the nerves. Peroneal nerve damage is more common in those with Charcot-Marie-Tooth illness.
- Lyme disease: This disease spread by ticks can result in neuropathy, which can harm the peroneal nerve.
Anatomical factors: In certain individuals, the peroneal nerve is located in greater proximity to the surface of the fibula, which is a tiny bone located on the outside of the lower leg. This may increase the nerve’s susceptibility to damage.
Activities that Cause Nerve Compression
- Trauma or injury to the knee: One of the most prevalent causes of peroneal nerve injury is trauma or injury to the knee. Peroneal nerve injury can occur in as many as 40% of cases of dislocated knees. Knee replacement surgery and fibula fractures are two other knee injuries that might harm the peroneal nerve.
- Tight splint or cast: An excessively tight splint or cast might injure the nerve by compressing it.
- Legs crossed for extended periods: The peroneal nerve behind your knee may become compressed if you sit with your legs crossed for extended periods.
- Longer bed rest: Individuals who experience peroneal nerve injury may be at a higher risk of developing this condition.
- Repetitive strain: Long-term kneeling or squatting can cause repetitive tension on the nerve, which can lead to peroneal nerve damage.
Diagnosis of The Peroneal Nerve Injury
A physical examination by a medical practitioner and particular tests to evaluate nerve function are usually used in the diagnosis of peroneal nerve damage. The technique is separated in the following way:
Physical Examination:
Your physician will probably start by asking you about your symptoms, including when they started, how bad they were, and whether there was anything that might have caused them, like an injury, an accident, or a pre-existing condition. The physical examination of your foot and leg will then be conducted, with special attention to:
- Muscle strength: Your ability to evert (turn your foot outward) and dorsiflex (raise it upward) your foot will be evaluated. Peroneal nerve involvement is suggested by weakness in these movements.
- Sensation: The top of your foot and the outer portion of your lower leg, which are supplied by the peroneal nerve, will be tested for feeling. In certain regions, numbness or tingling may be a sign of nerve injury.
- Gait: Your physician may watch you walk to see whether you have foot drop, a condition in which you are unable to raise your foot off the ground, causing your toes to drag.
Tests for Nerve Function:
Although a physical examination might offer important hints, specialized testing is frequently required to identify a peroneal nerve injury and determine its extent. These examinations could consist of:
- EMG, or electromyography: Your muscles’ electrical activity is measured by this test. A tiny needle electrode is put into your leg muscles to record an EMG. When a small electrical current activates the muscles, the electrode records the electrical signals that the muscles create. Damage to the nerves can be indicated by abnormal EMG readings in the muscles supplied by the peroneal nerve.
- Nerve Conduction Study (NCS): This examination assesses the efficiency with which electrical signals pass through your nerves. The peroneal nerve and the muscles it regulates are covered with tiny electrodes that are applied to your skin. By passing electrical pulses into the nerve, the physician can gauge the signal’s strength and speed. Signals that are absent or sluggish indicate neural pathway impairment.
- Imaging Tests: X-rays, CT scans, and MRIs can sometimes be performed to rule out alternative explanations of your symptoms, like fractures or bone spurs that could be compressing a nerve.
Additional tests might be required in certain circumstances, including:
Magnetic Resonance Neurography (MRN): The location and degree of nerve damage can be determined with the use of magnetic resonance neurography (MRN). This specialized MRI scan offers a more detailed picture of your nerves.
Differential Diagnosis of The Peroneal Nerve Injury
A differential diagnosis is essential to guarantee appropriate treatment because many illnesses might resemble the symptoms of peroneal nerve damage. The following ailments are among those that are part of the peroneal nerve injury differential diagnosis:
- Traumatic injuries: The peroneal nerve can be harmed by fractures, dislocations, and other traumas to the knee or ankle.
- Compressive neuropathies: The peroneal nerve may be compressed by Tarsal tunnel syndrome and other compressive neuropathies, resulting in symptoms.
- Systemic or inflammatory conditions: The peroneal nerve can be harmed by diabetes, alcoholism, and autoimmune illnesses such as rheumatoid arthritis.
- Nutritional deficits: Nerve injury can result from shortages in vitamin B12 and other nutrients.
- Toxic neuropathies: Nerve injury can result from exposure to specific poisons, including heavy metals and chemotherapy medicines.
- Neurological disorders: The nerves that regulate the muscles of the lower leg and foot can be impacted by ALS, multiple sclerosis, and other neurological disorders.
Treatment of The Peroneal Nerve Injury
The extent and location of the damage determine the treatment plan for a peroneal nerve injury. Physicians will typically start with non-surgical methods. Here is a summary of available therapies and care plans:
Non-surgical interventions:
- Rest and steer clear of stressful situations: This stops additional injury and gives the nerve time to regenerate.
- Orthotics, also known as ankle-foot orthoses, or AFOs: By making up for foot drop, a brace or splint can assist hold the foot high and enhance stride.
- Physical therapy: Regaining mobility in the injured leg requires exercises that increase strength, range of motion, and balance. You can also receive gait retraining to improve your ability to walk safely and without tripping.
- Medication: To lessen pain and inflammation, doctors may prescribe anti-inflammatory drugs.
- Surgical treatments: Surgery may be considered if conservative approaches are not successful in improving symptoms within a realistic time frame. The following are a few surgical options:
- Surgery for decompression: By eliminating any structures that are compressing the nerve, this surgery releases pressure on the nerve.
- Nerve repair or grafting: Surgeons may try to sew the severed ends together (repair) or use a nerve graft from a different area of the body to fill the gap in a serious injury.
- Tendon transfer: Surgeons may use tendons from other muscles to replace the weaker peroneal muscles if nerve damage is irreversible and muscular function cannot be recovered.
Physical Therapy of The Peroneal Nerve Injury
Recovering from a peroneal nerve injury requires physical therapy. What a physical therapist might perform for your recovery program is broken down here:
Physical therapy’s goals are:
- Enhance your muscle strength, especially in the peroneal muscles, which are responsible for lifting and extending the foot.
- Increase the range of motion in the ankle joint and calf muscles to avoid tightness that could further compress the nerve.
- To avoid falls and enhance gait, work on improving your balance and proprioception, or your body’s knowledge of its position in space.
- Depending on your situation, use techniques like electrical stimulation or ultrasound to reduce discomfort and inflammation.
Elements of Physical Rehabilitation:
- Exercises for strengthening: To increase general stability and function, these will concentrate on the calf, peroneal, and other muscles in the lower leg and foot. Resistance bands, weights, or your body weight may be used in exercises.
- Exercises for stretching: Mild stretches for the Achilles tendon and calf muscles can assist increase the ankle range of motion and lessen the chance that tightness will pinch a nerve.
- Training for proprioception and balance: Exercises involving single-leg stances, wobble boards, and agility drills can help retrain your nervous system and enhance balance, which lowers your chance of falling.
- Gait retraining: The therapist will assist you in learning how to walk correctly again if you suffer foot drop as a result of the nerve injury. This could entail training strategies to compensate for weakness and starting with an AFO brace.
- Nerve glides: These are soft motions that mobilize and stretch the nerve, possibly encouraging nerve regeneration.
- Manual therapy: Methods such as joint mobilization or massage can help lessen discomfort and increase flexibility.
- Modalities: In some situations, ultrasound or electrical stimulation may be utilized to lessen pain and inflammation and encourage tissue repair.
Treatment Progression:
The physical therapy program will be customized to meet your requirements and advance with time. Pain and inflammation management may take preference at first, then gradually progress to balance and strengthening exercises. The program will probably go on to more difficult exercises as you get stronger to restore complete function.
Complications of The Peroneal Nerve Injury
If peroneal nerve damage is severe or is treated poorly, it may result in some consequences. A few potential issues are below:
- Foot drop: The most frequent side effect of peroneal nerve damage is foot drop. It happens when the muscles that elevate the front of the foot weaken, which makes regular walking challenging. When walking, people with foot drop may drag their toes on the ground and may need to raise their knees higher than normal to clear the ground.
- Atrophy and weakening of muscles: In addition, weakness and atrophy (wasting) of the muscles in the foot and lower leg can result from peroneal nerve injury. Walking, standing, and climbing stairs may become challenging as a result.
- Chronic pain: Peroneal nerve damage patients may have persistent pain in their legs or feet. This discomfort may be severe, tingly, or burning
- Complex regional pain syndrome (CRPS): Following a nerve injury, CRPS is a chronic pain disorder. Severe pain, edema, and stiffness in the affected limb are possible outcomes.
- Skin issues: Foot skin issues like tingling, numbness, and trouble sweating can also result from peroneal nerve damage. The likelihood of skin infections may rise as a result.
- Balance issues: It can be challenging to maintain balance when experiencing weakness or loss of sensation in the foot, which raises the possibility of falling. These consequences can be avoided by treating peroneal nerve damage as soon as possible.
Prevention of The Peroneal Nerve Injury
Although there is no certain method for preventing peroneal nerve damage, you can lower your risk by adhering to these easy guidelines:
- Don’t spend a lot of time sitting with your legs crossed. The peroneal nerve behind your knee may be compressed as a result.
- Lessen the amount of activities that strain your knees, particularly the back or outside. This involves doing repetitive stress exercises on the knees, such as several martial arts, as well as prolonged lengths of time spent kneeling on hard surfaces and performing improper squats.
- Keep your posture straight. This relieves strain on your nerves and maintains the alignment of your spine.
- Put on appropriate footwear. Put on supportive and well-fitting shoes. Steer clear of shoes that are excessively tight or have high heels.
- Before exercising, warm up, and after, chill down. This can lessen the risk of injury and enhance blood flow to your muscles and nerves.
- Regular stretching. Stretching can help you become more flexible and lower your chance of getting hurt.
- Pay attention to the pain and stay mindful of your body. Stop the exercise and consult a doctor if you feel pain in your leg or knee. Nerve damage can be avoided by treating leg injuries as soon as possible.
- Sustain a healthy weight. Obesity and excess weight can place additional strain on your nerves and joints.
It’s critical to properly treat any conditions that raise your risk of nerve compression, such as diabetes, to lower your chance of peroneal nerve injury.
FAQs
What is a typical malfunction of the peroneal nerve?
A condition known as common peroneal nerve dysfunction is characterized by a lack of feeling or movement in the leg and foot as a result of peroneal nerve injury.
What signs indicate injury to the peroneal nerve?
Reduced sensations in the outside part of the upper or lower leg or the top of the foot, as well as tingling or numbness.
Foot dropping (inability to keep the foot up) “Slapping” gait (a manner of walking where the sound of each step is similar to a slapping one)
Walking causes toes to drag.
Issues with walking.
weakness in the feet or ankles.
How much time does peroneal nerve palsy take to heal?
Your recovery period will vary depending on your age, underlying medical conditions, and the degree of your common peroneal nerve palsy. Although nerve injury heals gradually, symptoms go immediately. Up to six months may pass before full recovery occurs.
Can someone who has damaged peroneal nerves walk?
Your toes may drag while you walk if this nerve is pinched, making it difficult to elevate the front portion of the foot. Additional signs of foot drop include walking with your knees raised above your hips to elevate your foot. weakening of the affected leg’s muscles.
What is the most effective peroneal nerve treatment?
You can experience numbness in your foot or lower leg if you have damage to your peroneal nerve. A foot drop is a common condition. For peroneal nerve injuries, gait training, physical therapy, and shoe inserts are common therapies. Nonsurgical treatment often alleviates or eliminates symptoms.
References
- Peroneal nerve injury. (2023, October 30). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/peroneal-nerve-injury
- Professional, C. C. M. (n.d.-f). Peroneal nerve injury. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24263-peroneal-nerve-injury
- Lezak, B., Massel, D. H., & Varacallo, M. (2022, November 14). Peroneal nerve injury. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK549859/
- Common peroneal nerve dysfunction. (n.d.). Mount Sinai Health System. https://www.mountsinai.org/health-library/diseases-conditions/common-peroneal-nerve-dysfunction
- Yetman, D. (2022, December 22). Peroneal nerve injury in the leg: What you should know. Healthline. https://www.healthline.com/health/peroneal-nerve-injury#about-peroneal-nerve-injury
- Sissons, B. (2023, March 16). What causes peroneal nerve pain? https://www.medicalnewstoday.com/articles/peroneal-nerve-pain#symptoms