What is an Ankylosing Spondylitis?
Ankylosing Spondylitis (AS) is a chronic inflammatory condition primarily affecting the spine, characterized by inflammation of the spinal joints, leading to pain, stiffness, and potentially spinal fusion. It falls under the category of spondyloarthritis, a group of rheumatic diseases that share common clinical features.
AS typically begins in the sacroiliac joints, causing lower back pain and stiffness, and can progress to involve other parts of the spine and even peripheral joints.
AS frequently causes reduced spinal motion and might result in postural problems. Patients may also have buttock and hip pain. Peripheral arthritis, enthesitis, and dactylitis (“sausage digits”) are all caused by AS.
In addition to skeletal involvement, AS can affect organs other than the joints. Extraarticular symptoms of AS include inflammatory bowel disease (affecting up to 50% of people), acute anterior uveitis (seen in 25%-35% of patients), and psoriasis (around 10% of cases).
AS is also associated with an increased risk of cardiovascular disease, which is thought to be caused by the systemic inflammation found in people with AS. Pulmonary issues have been connected to since decreased chest wall expansion and reduced spinal motion can predispose people to a restrictive pulmonary pattern.
Finally, those with AS are at least twice as likely to develop vertebral fragility fractures. Furthermore, patients have an increased risk of atlantoaxial subluxation, spinal cord damage, and, occasionally, cauda equina syndrome.
Who Develops Ankylosing Spondylitis?
Ankylosing spondylitis can affect anyone; however, several risk factors can improve your chances of having the disease. These factors include:
- Family history and genetics. If you have a family history of ankylosing spondylitis, you are more prone to acquire the condition.
- Age. Most people experience symptoms of ankylosing spondylitis before the age of 45. However, some people develop the condition as children or teenagers.
- Other conditions. People with Crohn’s disease, ulcerative colitis, or psoriasis may be more predisposed to developing the disease.
Epidemiology
Ankylosing spondylitis (AS) most typically affects people under the age of 40, with over 80% of patients experiencing their first symptoms before the age of 30. After age 45, less than 5% of cases are diagnosed. AS is additional common in men than in women. Furthermore, there is an elevated chance of getting AS in families of affected patients.
Pathophysiology
Ankylosing spondylitis (AS) is a chronic inflammatory disease that usually develops gradually and without noticeable early signs. The condition can be identified by increasing musculoskeletal, and sometimes extraskeletal, indications and symptoms. Each person experiences disease progression at a different rate.
The major pathophysiology of spondyloarthropathies, including AS, is enthesitis. CD4 and CD8 T lymphocytes, as well as macrophages, are among the immune cells that penetrate during chronic inflammation. Cytokines, including TNF-α and TGF-β, play an important function in inflammation. They contribute to inflammation, fibrosis, and ossification in areas affected by enthesitis.
Causes of Ankylosing Spondylitis:
Ankylosing spondylitis’s cause is unknown to researchers. However, research indicates that both genes and environmental factors may contribute to the disease’s development. Researchers know that the HLA-B27 gene raises the likelihood of developing ankylosing spondylitis, but having the gene does not guarantee you will acquire the condition. Many people carry the gene yet do not get ankylosing spondylitis, indicating that environmental variables may play a role.
Researchers are still discovering many more gene changes that may cause the disease; nevertheless, HLA-B27 is the key gene known to raise the risk of getting ankylosing spondylitis.
Symptoms Of Ankylosing Spondylitis
The most common symptom of ankylosing spondylitis is pain and stiffness in the lower back and/or hip. Over time, the symptoms may spread to other parts of the spine or body. The pain usually increases during periods of rest or inactivity, so some people may feel more pain in the middle of the night or after extended sitting. Typically, moving and exercising can help relieve discomfort.
Some people experience intermittent mild pain, but others experience chronic, severe pain. Ankylosing spondylitis symptoms, minor or severe, can worsen in “flares” and improve during remission.
Because the disease can affect other sections of the body, other symptoms may occur, such as:
- Pain, stiffness, and inflammation in other joints, including the ribs, shoulders, knees, and ankles.
- Difficulty breathing deeply if the rib joints are compromised.
- Uveitis, an inflammatory condition of the eye, causes vision abnormalities and pain.
- Fatigue, or feeling extremely fatigued.
- Loss of appetite and weight loss.
- Skin rashes, specifically psoriasis.
- Abdominal pain and loose bowel motions.
Diagnosis
History and Physical
Because of the disease’s systemic nature and probable involvement in numerous organ systems, a thorough examination of the entire body is required in possible cases of AS. Back discomfort is a typical complaint from patients. The typical back pain in AS is “inflammatory” in nature.
The presence of inflammatory back pain is defined by at least four of the following five characteristics: commencement of symptoms before the age of 40, gradual and insidious onset, reduction with exercise, lack of improvement with rest, and nocturnal pain that improves upon awakening. Additionally, spinal stiffness, reduced mobility, and postural abnormalities, particularly hyperkyphosis, are commonly reported.
AS can cause axial and peripheral musculoskeletal symptoms as well as extraarticular characteristics, thus the patient’s history and physical examination should cover all body systems. A thorough medical history should be collected to detect or rule out associated illnesses such as psoriasis, inflammatory bowel disease, and uveitis, among others, which may be related to AS.
Evaluation
In cases of ankylosing spondylitis (AS), laboratory results are frequently unclear but may provide evidence to support a diagnosis. Approximately 50% to 70% of patients with active AS have higher levels of acute phase reactants including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). However, normal ESR and CRP levels should not be used to rule out the potential of AS.
Several imaging abnormalities, particularly those involving the spine and sacroiliac joints, are linked to AS. The Assessment of Spondyloarthritis International Society (ASAS) axial spondyloarthritis criteria include evidence of sacroiliitis on imaging, whether radiographic or magnetic resonance imaging (MRI).
There is a standardized plain radiography grading system for sacroiliitis. This scale extends from normal (0) to the most severe (IV), as explained below.
- 0: Normal SI joint width with acute joint borders.
- I: suspicious.
- II: Sclerosis and some erosions.
- III: Severe erosions, pseudo-expanding joint space, and partial ankylosis.
- IV: Complete ankylosis
Plain radiographic alterations in the SI joints can be inconspicuous in the early stages of AS; however, these changes usually become more visible throughout the first decade of the disease. The most visible abnormalities on radiographs are subchondral erosions, sclerosis, and joint fusion. These changes are usually symmetrical, affecting both sides of the SI joints equally.
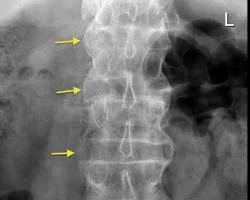
Throughout AS, some different radiographic abnormalities might gradually occur. In the early stages, a noticeable indication is the “squaring” of vertebral bodies, which is best seen on lateral X-rays. This squaring is caused by inflammation and bone deposition, leading to the lack of normal concavity along the anterior and posterior borders of the vertebral body. In addition, early-stage radiographs may reveal Romanus lesions, commonly known as “shiny corner signs,” which are characterized by small erosions and reactive sclerosis at the vertebral body corners.
Late-stage radiographic abnormalities include ankylosis (fusion) of the spine’s facet joints, syndesmophytes, and calcification of the anterior longitudinal ligament, supraspinous ligaments, and interspinous ligaments. This calcification appears as the “dagger sign,” a single, vertically arranged radiodense line down the spine, on frontal radiographs.
The “bamboo spine sign,” or vertebral body fusion by syndesmophytes, is a common radiographic finding in late-stage AS. The bamboo spine usually affects the thoracolumbar or lumbosacral joints. This spinal fusion increases the patient’s risk of developing progressive back stiffness.
While plain radiography is the primary imaging modality in AS, further imaging with MRI may be required to detect more subtle abnormalities, such as fatty or inflammatory alterations. MRI can detect current inflammatory lesions in the SI joints. These show up as bone marrow swelling (BME) on short tau inversion recovery (STIR) and T2-weighted imaging with fat suppression.
Differential Diagnosis
Certain diseases and conditions may look like ankylosing spondylitis (AS) and must be ruled out.
This includes but is not limited to:
- Mechanical lower back pain.
- Lumbar spinal stenosis.
- Rheumatoid arthritis.
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Each of these illnesses shares similarities with AS, but their differences must be checked for a correct diagnosis.
Various factors distinguish mechanical back pain from AS. The beginning of symptoms is a major distinguishing aspect, as mechanical back pain can develop at any age, whereas AS usually appears before the age of 40. Morning stiffness is mild and transient; in contrast to AS, mechanical back pain gets better with rest. Mechanical back pain is not associated with peripheral arthritis or other extraskeletal symptoms typical in AS.
Lumbar spinal stenosis (LSS) is a disorder characterized by a narrowing of the spinal canal, which causes spinal cord compression. Like AS, it can cause chronic back pain and morning stiffness. LSS, unlike AS, typically affects people above the age of 60 and does not come with peripheral arthritis or extraskeletal characteristics. The reaction to NSAIDs in LSS varies among people.
Rheumatoid arthritis (RA) is another chronic inflammatory illness of the joints that, like AS, causes progressive back pain and morning stiffness in persons aged 40 and younger. However, peripheral arthritis is extremely common in RA but not in AS.
Diffuse idiopathic skeletal hyperostosis (DISH) is a degenerative condition that causes ossification in the spine, particularly in the anterior longitudinal ligament, paravertebral tissues, and the peripheral side of the annulus fibrosus. DISH, like AS, may present with postural abnormalities and back pain. DISH, unlike AS, is not an inflammatory disease and does not display inflammatory symptoms such as morning stiffness or improvement with activity but not rest. DISH also shows no indication of sacroiliitis on radiographic imaging.
Treatment of Ankylosing Spondylitis
The treatment aims for AS are to reduce pain and stiffness, maintain axial spine mobility and functional capacity, and avoid spinal problems. Non-pharmacological therapies should include frequent exercise, posture training, and physical therapy.
First-line pharmacological therapy involves the long-term use of nonsteroidal anti-inflammatory medications (NSAIDs). If NSAIDs do not give significant relief, they can be combined with or replaced with tumor necrosis factor inhibitors (TNF-Is) such as adalimumab, infliximab, or etanercept. The response to NSAIDs should be monitored 4 to 6 weeks after beginning, but the response to TNF-Is should be tested 12 weeks later.
Systemic glucocorticoids are not indicated for treating AS, however local steroid injections may be used in specific cases. Specialist referrals may be required based on the patient’s clinical presentation, probable consequences, and extra-articular symptoms of the disease. Rheumatologists can help with the official diagnosis, care, and monitoring of AS, whereas dermatologists, ophthalmologists, and gastroenterologists can help with the disease’s non-musculoskeletal presentations.
Physiotherapy Treatment
Physiotherapy as an Effective Treatment for Spondylitis Ankylosing
An important part of treating Ankylosing Spondylitis (AS) and its symptoms is physiotherapy (PT). It can raise your standard of living through:
- Reducing stiffness and pain: Joint mobilization, strengthening, and stretching activities can help reduce stiffness and pain.
- Preventing spinal fusion and preserving mobility: Frequent movement lowers the chance of spinal fusion (ankylosis) and preserves joint mobility.
- Developing proper posture and core strength: Strong core muscles and proper posture can support your spine and reduce pain.
- Boosting cardiovascular health: For those with chronic conditions like AS, aerobic activity can help you feel better about yourself generally and with your heart.
- Getting regular exercise and using stress reduction strategies will help you sleep better and feel less fatigued.
- Promoting self-management: Acquiring workouts that you can perform at home gives you the ability to properly maintain your health.
The following are the components of a typical AS physiotherapy program:
- Exercises to correct your posture and avoid slouching, which may aggravate pain, are known as posture training.
- Exercises for range of motion: Mild stretches to keep your spine and other joints flexible.
- Exercises to strengthen your back, core, and other muscle groups that support your spine are referred to as strengthening exercises.
- Cardiovascular exercise: Low-impact exercises to strengthen your heart and increase your general fitness, such as riding, walking, or swimming.
- Hydrotherapy: Activities performed in warm water are beneficial for reducing pain and increasing range of motion.
- Manual therapy: Light touch methods to increase the range of motion in joints and reduce discomfort.
- Education and self-care: Acquiring knowledge about AS and knowing how to control your symptoms at home.
Exercise for Ankylosing Spondylitis (AS)
Several workouts that are suggested for AS include:
- Exercises for flexibility:
Gentle stretches: Pay particular attention to stretches that work your shoulders, chest, hips, and spine. Arm circles, neck rolls, and cat-cow stretches are a few examples.
Pilates or yoga: These mind-body therapies, which include breathing exercises, mild stretches, and strengthening activities, may be helpful for those with AS.
- Exercises for strengthening:
- Core strengthening: To develop your core muscles, which support your spine and improve posture, try exercises like planks, bird dogs, and bridges.
- Low-impact strength training: You may build your primary muscle groups without overstressing your joints by performing exercises with low weights or resistance bands.
3. Exercises for the aerobic system:
- Low-impact exercises: Go for joint-friendly activities like swimming, walking, cycling, or water aerobics.
- Extra factors to think about:
- Warm-up and cool-down: Before working out, always warm up with mild aerobic stretches, then cool down with static stretches.
- Pay attention to your body: As you gain strength, progressively increase the duration and intensity of your workouts. Start cautiously. Keep an eye on your pain threshold and quit if you start to feel uncomfortable.
- Maintain good form: To prevent injuries, perform workouts with perfect form. For advice on the correct technique, speak with a certified physical therapist or other healthcare provider.
Prognosis
Individuals with an earlier onset of ankylosing spondylitis (AS) have poorer functional outcomes. However, it is worth noting that significant physical disability is quite uncommon with AS. Most patients can maintain an acceptable level of physical function and live active, satisfying lives.
Patients with severe and long-standing diseases have a higher chance of death than the general population. The higher mortality is mostly due to cardiovascular problems.
Complications
Ankylosing spondylitis (AS) causes both articular and extra-articular problems. This includes:
- Chronic Pain and Disability
- Aortic regurgitation
- Possible diagnoses include pulmonary fibrosis and cauda equina syndrome.
- Mood Disorders
- Spinal fusion: The most common AS effect occurs when the bones of the spine fuse together, keeping the spine hard and inflexible. This might cause pain, stiffness, and trouble moving.
- Difficulty breathing: Rib cage stiffness can make deep breathing difficult, resulting in shortness of breath and weariness.
- Heart problems: AS-related inflammation can damage the heart and blood vessels, increasing the risk of a heart attack, stroke, and other cardiovascular issues.
- Osteoporosis: AS can raise the risk of osteoporosis, which weakens bones and increases their susceptibility to fracture.
- Eye difficulties: People with AS are more prone to eye problems such as uveitis, an inflammation of the eye’s central layer.
- AS can also cause gastrointestinal difficulties, such as inflammatory bowel disease (IBD).
- Amyloidosis is an uncommon side effect of AS that can harm the kidneys, liver, and other organs.
Post-operative and rehabilitation care
Exercise programs have shown considerable benefits in controlling ankylosing spondylitis by improving pain management, flexibility, mobility, and general function. While no single protocol is universally suggested for AS management, numerous studies have found advantages across a variety of exercise programs, including home exercise programs and group therapy.
Hydrotherapy is a popular treatment option for people with AS due to its cardiovascular advantages and pain relief effects. Respiratory and postural exercises are vital in AS since the illness process can affect proper respiratory mechanics and posture.
Deterrence and Patient Education
Patient education is important in the treatment of ankylosing spondylitis (AS). The chronic nature of the illness, the drugs used to treat it, and any possible adverse effects should all be explained to patients.
There should be a focus on regular exercise programs that relieve symptoms. Physical therapy, such as water therapy and swimming, can be extremely effective in terms of symptom reduction, functional improvement, and general fitness.
Given the risk of pulmonary involvement in AS, we must highlight the need to quit smoking.
Pearls and Other Issues
Patients with AS should be closely watched for vertebral fractures, especially in the event of minimal trauma. Individuals with AS have an increased risk of vertebral fracture and subluxation, particularly in the cervical spine. As a result, these patients are more likely to experience neurologic complications.
Exercise, physical therapy, targeted pharmaceutical medication, and regular follow-up meetings with doctors can all help to reduce disease morbidity.
Improving Healthcare Team Outcomes
Ankylosing spondylitis (AS) is a systemic disease that affects several organ systems. As a result, an interprofessional team approach is advised for reducing morbidity and providing complete treatment to people with AS. An effective interprofessional team can include healthcare experts such as the following:
- Rheumatologists are often at the forefront of AS treatment, offering diagnosis, disease monitoring, and medication management advice.
- Primary care physicians play an important role in evaluating overall health, coordinating care, and managing comorbid conditions.
- Gastroenterologists test for inflammatory bowel disease.
- Ophthalmologists evaluate for anterior uveitis.
- Cardiologists evaluate for heart block and valve involvement.
- Physical and occupational therapists collaborate to create exercise programs, provide pain management measures, and increase mobility and functionality.
- Neurologists look for nerve compression syndromes.
- Pharmacists keep track of medication interactions and analgesic dependence.
- Nurses provide continuing support, education for patients, and care coordination.
- Several papers have presented data supporting the effectiveness of an interprofessional approach in addressing ankylosing spondylitis, which leads to functional improvement, pain reduction, and improved quality of life.
Risk factors
While the specific origin of Ankylosing Spondylitis (AS) is unknown, there are various risk factors related to its development. These can be classified as genetic and environmental.
Genetic Factors:
The HLA-B27 gene is the best-known genetic risk factor for AS. This gene is carried by around 90% of persons with AS; however, not everyone with the gene develops the condition. It is crucial to keep in mind that carrying the gene does not guarantee that you will get AS, and many people who carry the gene never experience symptoms.
Other genes: Researchers are looking into other genes that may play a role in AS development, although their specific role is still unknown.
Environmental Factors:
Age: AS commonly begins between the ages of 17 and 45.
Sex: Men are approximately twice as likely as women to get AS.
Family history: Having a close family member with AS raises your risk.
Several infections: While the specific link is unknown, some studies suggest that some bacterial infections may cause AS in people with a genetic vulnerability.
Gut microbiome: A recent study indicates that alterations in the gut’s bacteria may be connected with AS development, although further research is needed to prove this link.
It is crucial to remember that these are only risk factors, and not everyone with them will get AS. Conversely, someone with no recognized risk factors may nevertheless get the condition.
Prevention
However, there is no known technique to prevent Ankylosing Spondylitis (AS) fully. This is because the specific etiology of the condition is unknown, but it is thought to entail a complex interaction of hereditary and environmental variables.
However, there are certain things you can do to minimize your risk of having AS or limit its advancement if you already have it.
Lifestyle modifications:
- Exercise regularly: Low-impact exercises like swimming, yoga, or Pilates can help preserve joint flexibility and mobility, thereby lowering stiffness and pain.
- Maintain a healthy weight: Excess weight can strain your joints, so eating a well-balanced diet and exercising regularly will help.
- Quit smoking: Smoking increases the chance of developing and worsening AS. Quitting smoking can drastically lower inflammation and improve overall health.
- Set goals for excellent posture: Maintaining proper posture while sitting, standing, and sleeping will assist in preventing pressure on your spine and joints.
- Early diagnosis and treatment:
- Seek medical help right away: If you have persistent back pain, stiffness, or other symptoms of AS, see a doctor as soon as possible. Early detection and therapy can dramatically improve outcomes while perhaps slowing disease development.
- Follow the treatment plan: Following your doctor’s recommended treatment plan, which may include medications, physical therapy, and lifestyle changes, is important for symptom management and reducing disease progression.
Additional considerations:
- Genetic testing: While not a preventive measure, genetic testing for the HLA-B27 gene can assist in identifying those who are more likely to develop AS, allowing for earlier monitoring and management. It is important to realize, however, that carrying the gene does not guarantee that you will get AS, and many people who carry the gene never experience symptoms.
- Stay informed and connected. AS research is continuous, with new advances being made all the time. Stay up to date on the newest advancements by engaging with patient support groups and organizations such as the Spondylitis Association of America (SAA).
Conclusion
Ankylosing spondylitis (AS) is a chronic and progressive disease with no single, definitive cure. However, here are a few important considerations to consider:
Overall:
- AS is a lifelong condition that can be managed effectively to allow for a full and active life. Early diagnosis and treatment are important.
- Symptom management is important: While there is no cure, a variety of treatments can considerably reduce pain and inflammation while improving mobility.
- The prognosis varies: some people endure limited progression, while others have more severe symptoms and may require spinal fusion.
- The importance of a holistic approach: Combining medicine, physical therapy, exercise, and lifestyle changes may significantly improve quality of life.
Living with AS:
- Concentrate on treating symptoms. Pain, stiffness, and weariness are frequent, but there are several techniques to help alleviate them.
- Maintain a positive attitude: Keeping active, engaged, and connected to support networks can help relieve the emotional impact.
- Advocate for Yourself: Understand your disease, communicate with your healthcare team, and actively take part in treatment decisions.
FAQs
Is ankylosing spondylitis serious?
Ankylosing spondylitis-related complications
Some people with AS can stay completely self-sufficient or mildly impaired in the long run. However, as a result of injuries to other joints, including the hips or knees, and the bones in their spine fusing in a fixed position, some people eventually become seriously disabled
What triggers ankylosing spondylitis?
Ankylosing spondylitis is a chronic inflammatory illness and an uncommon type of arthritis. Infections (gastrointestinal, urinary tract, and respiratory infections), excessive physical exercise, work stress, emotional stress, and pregnancy can all cause ankylosing spondylitis to aggravate.
Can ankylosing spondylitis be cured?
There is no cure for ankylosing spondylitis (AS), however treatment can help improve symptoms. Treatment can also assist in postponing or preventing the spine from fusing and strengthening. These treatments are also beneficial if you have non-radiographic axial spondyloarthritis.
Can someone live a long life with ankylosing spondylitis?
Ankylosing spondylitis can lead to a long life. People with ankylosing spondylitis have the same life expectancy as the general population, except for individuals with the most severe forms of the disease and those with multiple medical conditions.
Ankylosing spondylitis affects four body parts. What are they?
Ankylosing spondylitis is a kind of arthritis characterized by inflammation of the spine’s joints and ligaments. Peripheral joints like the hips, ankles, and knees may also be impacted. Generally, our ability to move and bend is provided by the joints and ligaments of our spine.
What is the ultimate stage of ankylosing spondylitis?
If you have advanced AS your doctor may inform you that your spine has fused. This occurs when new bone grows between several of the tiny bones that comprise your spine, connecting them. The more frequently this occurs, the less movement you have in your spine.
Is walking dangerous for ankylosing spondylitis?
9 Effective Exercises for People With Ankylosing Spondylitis
Low-impact exercises, such as walking, are appropriate for those who can exercise safely. According to Tehrani, some people may be discouraged from exercising due to joint abnormalities, fused joints, misinformation, or fear of getting hurt, but walking is an excellent way to get into physical activity
Which foods should I stay away from if I have spondylitis?
Foods to Avoid
Sugar, salt, and fat. Inflammation may be caused by highly processed foods, as well as excessive sugar and fat content.
Alcohol. Limit your alcohol consumption or avoid it completely. … NSAIDs. Many arthritis patients take nonsteroidal anti-inflammatory medicines (NSAIDs), which can cause damage to the stomach lining.
What’s the difference between spondylosis and ankylosing spondylitis?
Spondylitis refers to a set of inflammatory disorders that affect the spine’s joints. Spondylosis is caused by wear and tear on the spine, not inflammation. Spondylitis and spondylosis are two diseases that produce arthritis-related pain and stiffness.
How do you sleep with ankylosing spondylitis?
Lying flat on your back with a straight spine may provide more comfort. If you’re lying on your side, avoid curling your legs up into your body; however, you can raise your knees with a pillow. You may also choose to avoid the mattress completely and relax in a recliner or comfortable chair.
What is the recovery time after ankylosing spondylitis?
Depending on the procedure, full recovery time can range from a few weeks to a few months. During this period, your healthcare team will continuously monitor your development. You may require physical treatment to restore movement. Many people may need to wear braces for several weeks.
References
- Ankylosing Spondylitis: Symptoms, Causes, Treatment. (2014, December 7). WebMD. https://www.webmd.com/ankylosing-spondylitis/what-is-ankylosing-spondylitis
- Wenker, K. J. (2023, June 20). Ankylosing Spondylitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470173/
- Branch, N. S. C. A. O. (2023, December 15). Ankylosing Spondylitis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/ankylosing-spondylitis#:~:text=Ankylosing%20spondylitis%20is%20a%20type,help%20us%20move%20and%20bend.