Peripheral Neuropathy
Peripheral neuropathy is the term for any disease that affects nerves other than those in the brain or spinal cord. Peripheral neuropathy is the term used to describe the malfunction or death of these nerves. They might not alert you when you’re in danger, or they might alert you for no apparent reason at all.
Numerous factors, including hereditary diseases, infections, and trauma, can cause this. There are also a lot of possible symptoms. The numerous indicators, underlying causes, and symptoms of this illness can have widely different treatment options.
What is Peripheral Neuropathy?
- Peripheral neuropathy is caused by injury to the peripheral nerves, which are located outside of the brain and spinal cord. This condition often causes pain, numbness, and weakness, usually in the hands and feet. It might also affect other body systems and functions, such as digestion and urine.
- The peripheral nervous system, which includes the brain and spinal cord, is responsible for sending information from the central nervous system to the rest of the body through motor nerves. Through sensory nerves, peripheral nerves also transmit sensory data to the central nervous system.
- Peripheral neuropathy can be brought on by several illnesses, including traumatic injuries, infections, metabolic disorders, genetic causes, and exposure to chemicals. Neuropathy is frequently caused by diabetes.
- Peripheral neuropathy patients typically report their discomfort as tingling, burning, or stabbing. Occasionally, symptoms improve, particularly when they are brought on by a treatable illness. Medication can help control pain associated with peripheral neuropathy.
What does this name mean?
The term “peripheral” derives from the Greek word for “around.” In this usage, “peripheral” refers to something that is not part of the “central” nervous system. The term neuropathy combines two terms whose origins back to ancient Greek:
Neuro: From the Greek word “neuron,” which means “nerve.”
Pathy comes from the Greek word “pathos,” which means “affliction” or “condition.”
Peripheral neuropathy can refer to any disorder that affects the peripheral nerves. The terms “neuropathy” and “polyneuropathy,” which translate to “disease of many nerves,” are commonly used interchangeably with “peripheral neuropathy” by medical professionals. Because peripheral nerves are the furthest from the central nervous system, these disorders often manifest in them at the earliest and most severe stages.
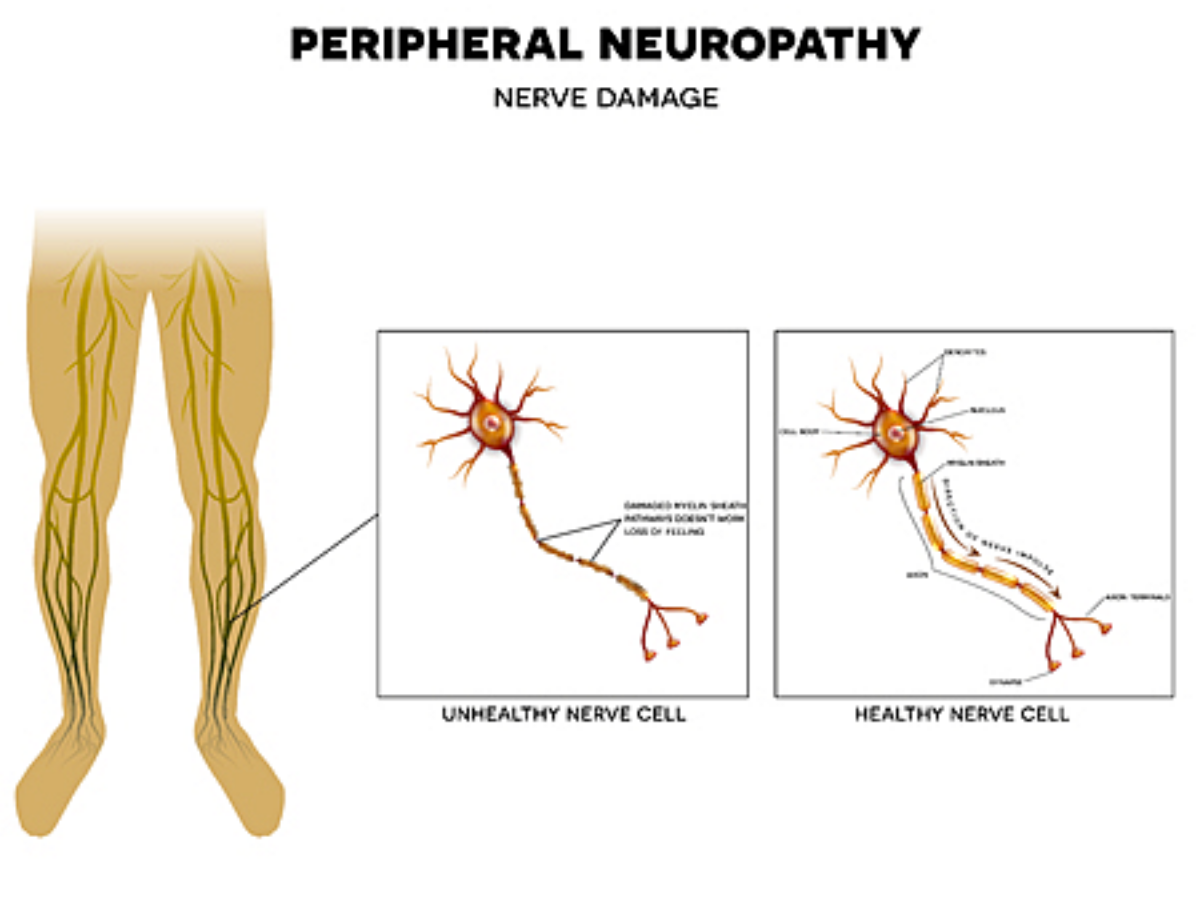
Anatomy and Physiology of the Neuron
To understand how peripheral neuropathy impacts your body, you should first grasp the anatomy of neurons, which are the main cells that make up your nerves. Neurons transmit and distribute electrical and chemical information throughout your nervous system. Each neuron contains the following:
The cell body is the cell’s primary structure.
- Axon: An axon is a long structure that projects from the cell body and resembles an arm. At the end of the axon are numerous finger-like extensions that convert the electrical signal in the neuron into a chemical signal. These extensions, known as synapses, connect adjacent nerve cells.
- Dendrites are tiny branch-like extensions of the cell body (the term originates from a Latin word meaning “tree-like”). Dendrites receive chemical signals from the synapses of adjacent neurons.
- A thin layer of fatty chemical components makes up myelin. Myelin covers and protects the axons of numerous neurons.
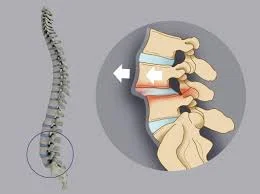
- Your nervous system consists of two parts the central nervous system and the peripheral nervous system. Your central nervous system consists of two components: your brain and your spinal cord. The peripheral nervous system is made up of all of your body’s nerves. It also comprises nerves that branch out from your spinal cord and brain to supply your face and the rest of your body.
How does Peripheral Neuropathy impact your body?
- Peripheral neuropathy is a term used to describe a variety of disorders involving injury to the peripheral nervous system, it serves as a massive communications network between the body’s remaining systems and the central nervous system, which includes the brain and spinal cord.
- Peripheral nerves convey a variety of sensory information to the central nervous system (CNS), including the message that your feet are chilly. They also transmit messages from the CNS to the rest of the body. The most well-known signals are those that tell our muscles to contract, which allows us to move. However, other types of signals also assist control our immune system, blood vessels, bones, digestion, urination, and sexual function.
- More than 20 million people in the United States are thought to have some kind of peripheral neuropathy, while this figure might be much higher because not all persons with neuropathy symptoms get tested for the condition, and current diagnostics do not screen for all types of neuropathy.
Nerve signal disruption
Peripheral nerves function similarly to wires that link various computer components or connect to the Internet. When they fail, complicated processes might come to a standstill.
Nerve signaling in neuropathy is interrupted in three ways:
- Signal loss.
- Inappropriate signaling can occur.
- Errors that affect communications are being transmitted.
Some types of neuropathy cause damage to just one nerve (mononeuropathy). Multiple mononeuropathy, or mononeuropathy multiplex, refers to neuropathy that affects two or more nerves in distinct regions. More commonly, several or all of the nerves are damaged (polyneuropathy).
Peripheral Neuropathy Types
According to structure Peripheral neuropathy develops in two primary ways:
- Demyelinating neuropathy: It occurs when the myelin covering on the axon deteriorates or does not develop properly. This influences the way messages pass through the neuron.
- Axonal degeneration: This causes the axon to degenerate and eventually perish. The longer a neuron is the more severe the impact. That is why axonal degeneration problems most commonly affect your legs and feet, which are the furthest away from your spinal cord and rely on connections made with longer axons. Axonal degeneration is the most prevalent feature of peripheral neuropathy.
According to Symptoms Peripheral Neuropathy Types:
Peripheral neuropathy comes in over a hundred different varieties, each with a distinct set of symptoms and a distinctive prognosis. To assist clinicians in classifying them, they are frequently divided into the following categories:
- Motor neuropathy. This is a nerve injury that affects muscles and movement in the body, such as moving your hands and arms or speaking.
- Sensory Neuropathy. Sensory nerves regulate how you feel, such as pain, warmth, or a gentle touch. Sensory neuropathy affects these nerves.
- Autonomic nerve neuropathy. Autonomic nerves regulate functions that you are unaware of, such as breathing and heartbeat. Damage to these nerves can be severe.
- Combination neuropathies. You might have a combination of two or three additional forms of neuropathies, such as sensory-motor neuropathy.
Causes of the Peripheral Neuropathy
Peripheral neuropathy can develop for several causes. This includes:
- Type 2 diabetes. Unmanaged type 2 diabetes is the most prevalent cause of peripheral neuropathy. When your blood sugar levels remain too high for an extended period, your peripheral nerves suffer harm. This is why persons with type 2 diabetes may lose sensation in their feet and lower legs.
- Alcohol use disorder. Excessive alcohol use, particularly over lengthy periods, can harm nerves. Alcohol use disorder is a major cause of peripheral neuropathy, and it can also contribute to vitamin deficiencies that lead to the condition.
- Vitamin and mineral deficiencies. People who are deficient in some vitamins may experience nerve injury. Copper deficiencies, as well as vitamins B1, B6, B9, B12, folic acid (B9), and E, are the most common causes. This can also be caused by a high intake of vitamin B6.
- Autoimmune and inflammatory disorders. Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy (CIDP) can result in significant weakness. They are also very curable. Lupus, rheumatoid arthritis, Sjögren syndrome, vasculitis, and other conditions can all cause neuropathy.
- Medications and poisons. Chemotherapy and some other drugs (antibiotics, as well as treatments for arrhythmia and gout) can produce peripheral neuropathy. It can also be brought on by exposure to certain heavy metals and industrial pollutants.
- Tumors. Tumors, both malignant (cancerous) and benign (noncancerous), can damage your peripheral nervous system.
- Genetic conditions. Genetic illnesses can be passed down from one or both parents. Amyloidosis, Fabry disease, and Charcot-Marie-Tooth disease are some of the conditions that can cause peripheral neuropathy. There are therapies available for hereditary amyloidosis and Fabry disease.
- Infections. Infections that harm nerves can be brought on by bacteria like Borrelia burgdorferi, which causes Lyme disease, or viruses like HIV. Another prominent example is getting shingles, which can cause persistent nerve discomfort.
- Hansen illness (sometimes known as leprosy). While the symptoms of this condition, which is uncommon in industrialized nations, are most obvious on the skin, it also affects your peripheral nerves. It is a highly prevalent cause of peripheral neuropathy in underdeveloped countries. worldwide
- Trauma and surgery. Direct nerve injuries and damage can occur as a result of trauma or medical operations. Swelling and stretching can also cause nerve injury. This type of injury generally only occurs in one spot. It might even be permanent in the long run.
- Vascular diseases are circulatory issues. Peripheral neuropathy can develop due to a lack of blood supply. A harmless, transient type of this occurs when you sit or lay in a specific position and one arm or leg falls asleep. This goes away soon if you adjust your posture sufficiently for circulation to resume. More severe circulation issues might result in significant and irreversible nerve injury.
- Idiopathic neuropathy. Peripheral neuropathy is frequent and can occur for unexplained reasons. This form of neuropathy is called “idiopathic” or “cryptogenic” (meaning “hidden or unknown cause”).
Symptoms of the Peripheral Neuropathy
There are several signs of peripheral neuropathy. This illness can affect a single nerve, a group of related nerves, or a large number of nerves located throughout your body. The symptoms are also determined by the kind of nerve signal damaged; many signal types may be implicated.
The symptom types (with additional details below) are:
- Motor.
- Sensory and pain.
- Autonomic.
Motor symptoms
Your peripheral nervous system transmits motor impulses, which are directives from your brain to your muscles. These signals allow you to move around. To be healthy and functional, your muscles require nerve connections to the brain.
- Motor symptoms include muscle weakness and paralysis. Peripheral neuropathy causes nerve degeneration, which weakens the surrounding muscles. This can produce paralysis, resulting in difficulties moving the toes, foot drop, and hand weakness. Weakness can impact muscles in the thighs, arms, and other areas.
- Muscular atrophy. Loss of nerve connectivity can cause muscles to shrink and weaken. This is especially true in the feet, lower legs, and hands of those suffering from peripheral neuropathy. Muscle loss may lead to deformities in the hands and feet.
- Uncontrolled muscular motions. Nerves that lose their connection to the brain due to peripheral neuropathy can become overactive on their own, resulting in cramping.
Sensory symptoms.
Your peripheral nerves translate information from the outer environment into nerve impulses. These impulses then travel to your brain, where they are processed into what you see as your perception of the world. Peripheral neuropathy can impair your sense’s capacity to see the outside environment and interact with your brain. The sensory signs of peripheral neuropathy are:
- Tingling. This occurs when there is an issue with the nerves that transmit messages to your brain. This is similar to radio static, which you hear when you are too far away from a broadcasting station.
- Numbness. This occurs when nerves fail to send or relay sensory impulses, resulting in the loss of some types of feelings. For example, picking up a cold pop can but not experiencing its smoothness or coolness, or not being able to feel the texture of carpet or the temperature of the floor through your feet.
- Imbalance and clumsiness. Nerves also transport sensations, which your brain utilizes to track the placement of your hands and feet. You are not consciously aware of these feelings, yet they are essential for balance and coordination. Without these sensations, you may lose balance, particularly in the dark, and become clumsy with your hands.
- Pain. Nerve damage from peripheral neuropathy can create faults in how and when nerves deliver pain signals, making them more powerful (hyperalgesia) or occurring too frequently (anesthesia). It can even lead nerves to spontaneously produce pain impulses. This is referred to as “neuropathic” pain, and it is the most prominent and disruptive sign of peripheral neuropathy.
Autonomic symptoms.
Your body has several autonomic processes. These are your body’s autonomic operations that occur without your conscious thought or awareness. They include sweating, digestion, blood pressure management, and so forth.
Autonomic nerve fibers transmit autonomic impulses. Disruptions in autonomic signals mean that your body’s automatic systems cannot function properly. Some may operate intermittently, while others may never work. Autonomic signs of peripheral neuropathy may include:
- Blood pressure varies. Your body normally regulates blood pressure, but peripheral nerve injury can interrupt this process. This might result in rapid decreases in blood pressure or rises in heart rate, particularly while standing up.
- Sweating excessively or not enough. Your body unconsciously regulates its interior temperature by sweating to release heat. If you have peripheral nerve damage, you may sweat too much or not enough. This might cause dry skin and scaling on your feet, as well as excessive perspiration after eating.
- Bowel and bladder issues. Your bowel and bladder are controlled by autonomic impulses that you are unaware of. Nerve fiber disruption can alter bowel motions (constipation or diarrhea) and, on occasion, bladder control.
- Sexual dysfunction. Your autonomic nerve system regulates sexual arousal. This is why autonomic issues can lead to sexual dysfunction.
- Other symptoms. Autonomic alterations caused by peripheral neuropathy can also result in skin color changes, edema, pupil changes, and blurred vision.
How fast does Peripheral Neuropathy develop?
The development of peripheral neuropathy, particularly the rate of its progression, is heavily influenced by the underlying etiology. Injuries can cause it to develop immediately, within minutes, or hours. Some toxic and inflammation-based types of peripheral neuropathy can develop quickly in days or weeks, but the majority of other disorders take months, years, or even decades to develop.
Who is affected by Peripheral Neuropathy?
Peripheral neuropathy can affect anybody, regardless of age, gender, color or ethnicity, personal circumstances, or medical history. However, certain people are more susceptible to certain forms of peripheral neuropathy.
Peripheral neuropathy is also commonly associated with certain age-related disorders. As you become older, your chance of having peripheral neuropathy increases.
How prevalent is Peripheral Neuropathy?
Peripheral neuropathy is prevalent because it encompasses a wide range of disorders. Globally, around 2.4% of individuals suffer from some kind of peripheral neuropathy. This figure jumps to between 5% and 7% among adults aged 45 and above.
Diagnosis of Peripheral Neuropathy
Peripheral neuropathy is typically diagnosed using a variety of techniques. These consist of medical history and symptoms. Your medical history, current symptoms, and any changes you’ve experienced will probably be topics of inquiry for your healthcare professional. They might also inquire about your diet, lifestyle, habits, and any medical illnesses and issues, such as type 2 diabetes.
Neurological and Physical examinations. These entail a medical professional searching for outward manifestations of peripheral neuropathy, such as altered sensory perception, weakened muscles, altered reflexes, or difficulties with walking and balance.
Diagnostic, imaging, and laboratory tests. Peripheral neuropathy can be diagnosed with the aid of many tests. The following are the most typical diagnostics for peripheral neuropathy, which are performed to either confirm the diagnosis or rule out other conditions:
- Blood tests: these can identify a wide range of issues, including poisons and toxins, particularly metals like lead or mercury, as well as immune system issues.
- EMG/NCV: These examinations monitor the electrical activity in your muscles and nerves to assist in identifying the extent and location of nerve injury.
- Ultrasonography of the nerves. A noninvasive experimental method called muscle and nerve ultrasonography is used to image muscles and nerves to check for injuries like severed or compressed nerves. Muscle or nerve disorders may be linked to anomalies found during ultrasound imaging of the muscles. Muscle ultrasonography reveals distinctive patterns in a few hereditary muscular diseases.
- Biopsy of the nerve. In an attempt to identify the source of the neuropathy, a tiny section of a nerve, typically a sensory nerve, is removed in this procedure.
- Biopsy of the skin. To count the number of nerve endings, a tiny piece of skin is excised.
- Genetic examination. Certain hereditary neuropathies can be tested for using genes.
- Imaging tests like MRIs, CT scans, or X-rays may occasionally be performed to rule out alternative reasons for your symptoms, like tumors or nerve compression.
Management and Treatment of Peripheral Neuropathy
Peripheral neuropathy can have a wide range of treatments depending on what causes it. Treatment may also be impacted by other variables, such as your personal preferences, medical history, and more. The best person to advise you on treatment(s) and the anticipated time frame for recovery is your healthcare professional. For peripheral neuropathy, the following treatment approaches are generally more popular:
Medication
Many medications can be used to treat problems with the peripheral nervous system. These can be administered intravenously, orally, as oral pills, topically applied patches, slow-release pharmaceuticals, and more.
For the treatment of moderate pain, over-the-counter (OTC) oral pain relievers such as acetaminophen (Tylenol) and nonsteroidal anti-inflammatory medicines (NSAIDs) like ibuprofen and aspirin can be very beneficial.
These medications can impair the function of your stomach or liver if you take them in excess. It’s crucial to refrain from utilizing them for an extended length of time, particularly if you often consume alcohol.
A list of additional over-the-counter topical drugs that you might want to try is provided by the Foundation for Peripheral Neuropathy. Among them are:
- Absorbine Jr., This mixture of herbs and menthol helps relieve aches and pains in the muscles. Some creams with menthol in them might also be helpful. These consist of Vicks VapoRub, Flex-All, Flexgen, and Tiger Balm.
- capsaicin cream. Some patients find that the heating action of the chili pepper oils in this cream helps to relieve their discomfort. Brands and formulas exist.
- Neuragen PN. This lotion, which is made of plant oils, is intended especially for treating nerve pain in the hands and feet.
- No More Sore. This is an additional herbal anesthetic that might help ease the pain associated with neuropathic pain.
This condition’s pain can also be managed with the aid of numerous prescribed painkillers. Narcotics, several antiepileptic drugs, and certain antidepressants are among them. Other useful prescription drugs consist of:
- Apply a patch of lidocaine to the injured region.
- Pregabalin, a drug that treats epilepsy
- The antidepressant duloxetine
- Anesthetics and steroids
Occasionally, pain specialists may recommend alternative treatments including acupuncture, transcutaneous electrical nerve stimulation, injections, or surgery to implant a spinal cord stimulator if normal medications are ineffective in treating your pain from peripheral neuropathy or nerve injury.
- Physical therapy. This might lessen pain symptoms or aid in your recovery from surgeries or injuries. Additionally, it can help you improve your balance and avoid falls while you adjust to changes in your neurological system.
- Equipment and wearable Technology. These consist of prescription footwear, and medical equipment like canes, walkers, and braces, among other things. While they might not cure peripheral neuropathy directly, these can lessen its consequences. A good example would be specific footwear for those with type 2 diabetes-related peripheral neuropathy.
- Foot care and Pedicure. Often, peripheral neuropathy affects the feet. This, especially in those with type 2 diabetes, can result in alterations to the soft tissue and bone, causing ulcers and infections. Many peripheral neuropathy sufferers require the care of a specialist (expert in feet).
Physical Therapy of Peripheral Neuropathy
When it comes to controlling peripheral neuropathy symptoms and enhancing your quality of life, physical therapy can be an invaluable resource. Even though it cannot reverse the underlying nerve damage, it can:
- Minimise pain and suffering: Massage, ultrasound, electrical stimulation, and other methods are only a few of the ways therapists can control pain (TENS).
- Enhance muscular function and strength: Exercise regimens customized for you will help build stronger muscles and better coordination, which will make it easier to carry out daily tasks.
- Improve balance and prevent falls: People with peripheral neuropathy often worry about falling, so balancing exercises can help you become more stable and less likely to do so.
- Prevent stiffness in your joints by stretching and doing other exercises. This will help you maintain your range of motion and flexibility.
- Teach you to take care of your health: Physical therapists can provide you with the knowledge and tools you need to comprehend your condition and actively participate in your care.
The following are a few typical physical therapy treatments for peripheral neuropathy:
- Aerobic exercise: Engaging in regular low-impact aerobic activities, such as swimming, cycling, or walking, can enhance general fitness, lessen pain, and improve circulation.
- Strength training: Moderate strength training exercises will assist in increasing the function and strength of your muscles, which will make it easier for you to carry out everyday tasks.
- Balance training: You can lessen your chance of falling and increase your stability with balance exercises.
- Exercises for flexibility: You can prevent stiffness in your joints by doing stretches and other exercises.
- Manual therapy: Methods like massage and joint mobilization can aid in enhancing range of motion, lowering pain, and improving circulation.
- Neuromodulatory techniques: These methods, which include therapeutic ultrasonography and transcutaneous electrical nerve stimulation (TENS), can assist in lowering pain and enhancing function.
It’s critical to remember that physical therapy is a customized treatment plan. Together, you and your physical therapist will create a customized treatment plan that addresses your unique requirements and objectives. Make sure the therapist you choose has experience treating peripheral neuropathy if you are thinking about doing physical therapy for it.
- Talk kindly about your aims and symptoms with your therapist.
- Tell the truth about your limits and any discomfort you feel while exercising.
- Pay close attention to the advice given by your therapist and show up for all of your appointments.
- It could take some time to notice the effects, so have patience.
- At home, keep up with the exercises you learn in physical therapy.
Complications of Peripheral Neuropathy
- Foot ulcers and infections: Peripheral neuropathy can produce a lack of sensation in the feet, making it harder to detect injuries. This can result in ulcers, which are open sores that can get infected.
- Charcot foot: This is a medical condition in which the bones of the foot weaken and distort. It can cause discomfort, edema, and difficulty walking.
- Digestive issues: Peripheral neuropathy can impair the nerves that govern digestion, causing constipation, diarrhea, and other disorders.
- Urinary problems: Peripheral neuropathy can affect the nerves that regulate urine, causing difficulties emptying the bladder or incontinence.
- Cardiovascular problems: In some circumstances, peripheral neuropathy can affect the nerves that control the heart and blood pressure, resulting in arrhythmia (irregular heartbeat) and excessive blood pressure.
It is crucial to remember that not everyone who has peripheral neuropathy will have all of these symptoms and problems. The severity of the symptoms will vary according to the underlying cause and degree of nerve injury.
Prevention of Peripheral Neuropathy
Some potential causes of peripheral neuropathy are avoidable. You can also reduce your risk of having it by avoiding or postponing certain circumstances. In general, the best preventative or precautionary measures you may take are:
- Eating a balanced diet. Certain vitamin deficiencies, particularly vitamin B12 deficiency, can harm your neurological system and create serious difficulties. Other vitamins, particularly B6, are hazardous and can induce peripheral neuropathy at large doses.
- Keeping physically active and at a healthy weight. This, together with proper nutrition management, can help prevent or delay the onset of type 2 diabetes, which gradually destroys your peripheral nerves.
- Wearing protective equipment as needed. Nerve damage is mostly caused by injuries. Using safety equipment during work and play activities might help you avoid or reduce these accidents.
- You are managing chronic illnesses as advised. If you have a chronic illness that might impact your peripheral nerves, such as type 2 diabetes, you should follow your healthcare provider’s recommendations. This can reduce the severity of the condition’s symptoms or postpone its progression.
- Avoiding excessive alcohol consumption. Excessive alcohol intake is a known cause of peripheral neuropathy. You can lower your risk of neuropathy (and other medical consequences) by avoiding or taking alcohol in moderation.
- Avoid exposure to chemicals, poisons, and heavy metals. Heavy metals such as lead and mercury may be extremely harmful to your neurological system. Mercury exposure is uncommon due to environmental rules, although outdated thermometers and thermostats may still contain it. Older homes may potentially have lead-based paint. Local, state, and national governments may provide resources and services to assist you avoid harmful metals and chemicals. If you operate with such metals and substances, observe all safety precautions and use the suggested or needed protective equipment.
Summary
Peripheral neuropathy occurs when one or more nerve groups are damaged. The effect on your body relies on which nerve units aren’t functioning properly. Potential reasons include injuries, systemic illnesses, and drugs.
By addressing the underlying cause of neuropathy, you can postpone or prevent its progression. Self-care practices, such as daily planning, can help you manage your illness and enhance your quality of life.
FAQs
What’s the primary cause of peripheral neuropathy?
Diabetes is a leading cause of neuropathy. People with peripheral neuropathy typically report their pain as stabbing, burning, or tingling. Symptoms may improve with time, especially if they are caused by a treatable disease. Medicines can help relieve the discomfort of peripheral neuropathy.
What’s the difference between neuropathy and peripheral neuropathy?
Neuropathy, also known as peripheral neuropathy, refers to damage to any component of your peripheral nervous system, which is the enormous message network that sends critical information from your brain and spine (central nervous system) to your body and vice versa.
Is it possible for peripheral neuropathy to disappear?
Peripheral neuropathy is usually incurable, but there are some things you can do to keep it from worsening. If an underlying ailment, such as diabetes, is the cause, Your doctor will address any underlying medical conditions, such as diabetes, before treating your pain and other neuropathy symptoms.
How can I assist with my peripheral neuropathy?
Walking three times a week can help reduce neuropathy discomfort, improve muscle strength, and control blood sugar levels. Gentle activities like yoga and tai chi may also assist. If you have painful neuropathy in your feet, consider pool-based exercise like swimming. Quit smoking.
What is the best vitamin for nerve repair?
Damage and regeneration occur spontaneously in the peripheral nervous system. The neurotropic B vitamins cobalamin (B12), pyridoxine (B6), and thiamine (B1) all play significant roles in preserving the life of neurons in different ways.
What are the symptoms of neuropathy?
Common symptoms include numbness and tingling in the feet or hands.
Burning, stabbing, or shooting pain in the afflicted regions.
Loss of balance and coordination.
Muscle weakness, particularly in the feet.
Is peripheral neuropathy a severe condition?
If you do not address the underlying cause of peripheral neuropathy, you risk getting potentially dangerous consequences, such as an infected foot ulcer. If left untreated, this can progress to gangrene, and in severe cases, the foot may need to be amputated.
Can I lead a normal life with peripheral neuropathy?
Though peripheral neuropathy offers everyday problems, it may not limit the value of life if properly managed. Many people effectively manage their symptoms by devising an effective treatment plan, adopting lifestyle changes, and practicing proactive self-care.
References
- Peripheral neuropathy – Symptoms and causes – Mayo Clinic. (2023b, September 2). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
- Professional, C. C. M. (n.d.-n). Peripheral neuropathy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14737-peripheral-neuropathy
- Peripheral neuropathy. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy
- Carey, E. (2023, February 10). Peripheral neuropathy. Healthline. https://www.healthline.com/health/peripheral-neuropathy#prevention
- Mfsrh, H. W. M. M. (2023, April 19). What is peripheral neuropathy? https://www.medicalnewstoday.com/articles/147963
- Peripheral neuropathy. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-neuropathy



9 Comments