Shoulder Pain
What is a Shoulder Pain?
Shoulder pain is an exceedingly common complaint that affects people of all ages. The shoulder joint has the greatest range of motion of any joint in the body, allowing movement in nearly every plane. This also makes it susceptible to various injuries and conditions that can cause significant pain and disability.
The onset of shoulder pain can be insidious or sudden and acute. It may arise from injury or trauma to the shoulder region, repetitive overuse, degenerative and arthritic conditions, strains and sprains of muscles and tendons around the shoulder, or neurological irritations that manifest as shoulder pain. Regardless of the cause, shoulder pain can severely impact one’s quality of life and ability to carry out activities of daily living and work-related tasks.
The anatomy of the shoulder is complex, involving bones, muscles, tendons, ligaments, bursae, and nerves that allow coordinated movement and provide mobility, as well as stability. Structures most commonly implicated in shoulder pain include the rotator cuff muscles and tendons, subacromial bursa, glenohumeral joint capsule, acromioclavicular joint, biceps tendon, and labrum. Pain-sensing nerves in these areas can become compressed or irritated, leading to significant and often disabling pain.
Due to the complexity of the shoulder anatomy and the diversity of potential causes for pain, achieving an accurate diagnosis is highly important when evaluating shoulder pain. A detailed history, physical exam, and in some cases, imaging studies facilitate diagnosis and allow for targeted treatments addressing the underlying pathology. Early and aggressive interventions are crucial to restoring function and providing pain relief. The longer shoulder pathology persists without appropriate care, the more difficult it may become to achieve full recovery.
With the right interventions, however, outcomes for shoulder pain sufferers are often excellent. Home-based care, physical therapy, medical treatments, and in more severe cases, surgery, can help most shoulder problems and let patients regain mobility and quality of life. An understanding of the intricacies of the shoulder joint and mechanics is fundamental to optimizing these interventions and outcomes.
Shoulder Anatomy and Function
The shoulder is made up of three main bones – the humerus, scapula, and clavicle. These bones articulate to form three main joints:
Glenohumeral Joint
- formed by the humeral head’s articulation with the scapula’s glenoid fossa
- A ball-and-socket type synovial joint that permits circular arm rotation
- Relies on surrounding rotator cuff muscles, joint capsule, and ligaments to provide stability
Acromioclavicular Joint
- Articulation between the outer end of the clavicle and the acromion process of the scapula
- Plane-type synovial joint with upward/downward gliding motions
- Stabilized by acromioclavicular ligaments and capsule
Sternoclavicular Joint
- Articulation between the manubrium of the sternum and the medial end of the clavicle
- The axial skeleton and upper limb are only attached by bone.
- Allows side-to-side and front-to-back motions of the shoulder
- Four muscles arising from the scapula and inserted onto the humeral head (supraspinatus, infraspinatus, teres minor, subscapularis)
- Functions in shoulder stability and rotation
Bursae
- Fibrous sacs with lubricating fluid that prevent friction between adjacent structures
- The subacromial bursa allows smooth gliding between the acromion and structures below
Labrum
- The fibrocartilagenous ring that lines and deepens the glenoid fossa
- Provides stability and deepens the socket for the humeral head
The shoulder muscles provide the dynamic stability and strength required for shoulder function. The rotator cuff is the most important group of muscles and tendons that surround the shoulder helping initiate movement and providing ongoing stability. The muscles of the upper arm, chest, and back also contribute to overall shoulder mobility.
This complex anatomy allows the shoulder to have tremendous mobility. The ball and socket glenohumeral joint affords movement in all planes and positions. This allows us to reach overhead and complete activities requiring rotation, extension, and flexion of the shoulder joint.
Causes and Risk Factors of Shoulder Pain
Rotator Cuff Injuries
The four muscles that make up the rotator cuff are the teres minor, subscapularis, supraspinatus, and infraspinatus. These muscles originate from the scapula and insert into the humeral head, covering the glenohumeral joint.
The main functions of rotator cuff muscles are:
- Provide dynamic stability to the shoulder joint
- Keep the humeral head centered in the glenoid fossa with arm movements
- Generate and control rotation and elevation of the arm
Rotator Cuff Tears
- Result from injury or trauma to the tendon that is severe enough to cause tissue damage
- Can range from partial thickness tear involving some tendon fibers to full thickness tear with complete discontinuity
- Most commonly affects the supraspinatus tendon at its insertion on the greater tuberosity
- associated with older age, repetitive overhead activities, degeneration
- Present with pain, weakness in the shoulder, decreased mobility
- Tend to progressively worsen over time without treatment
- Require rest, physical therapy, and possible surgical repair based on severity
Rotator Cuff Tendinitis
- Caused by repetitive overuse of the shoulder leading to inflammation
- Most commonly affects supraspinatus, and can involve other RC tendons
- Repeated microtrauma leads to irritation, inflammation, swelling
- Presents with pain when reaching overhead or behind the back, night pain
- Diagnosed based on physical exam, may have positive impingement signs
- Treated by rest, NSAIDs, physical therapy for tendon gliding exercises
Impingement Syndrome
- Compression of rotator cuff tendons between the humeral head and undersurface of the acromion
- Can cause irritation, inflammation, and tearing of the rotator cuff over time
- Intrinsic factors like acromial shape, and bone spurs can contribute
- Also caused by muscle imbalance, weakness, impaired scapular mechanics
- Pain when reaching overhead is typical
- The goals of treatment are resolving inflammation and removing pressure
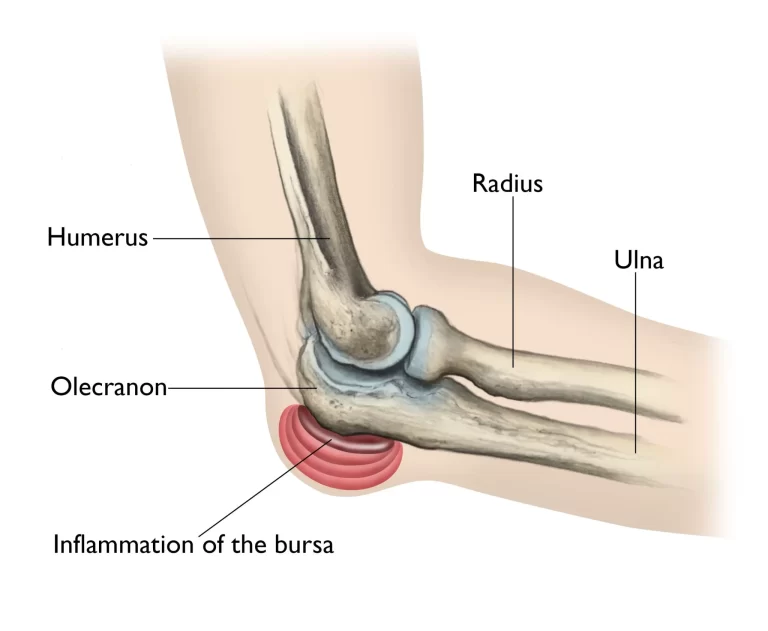
Bursitis
- Inflammation of one of the bursae sacs that protect tissues around the shoulder joint
- Most commonly affects the subacromial bursa under the acromion bone
- Caused by repetitive overhead motions, injury, pinching of structures
- Also associated with rotator cuff tears, impingement
- Presents with pain and tenderness on top of the shoulder that gets worse with overhead motions
- Diagnosed based on clinical exam, may involve ultrasound or MRI
- Treatment involves rest, NSAIDs, physical therapy, injections, addressing underlying causes
Adhesive Capsulitis (Frozen Shoulder)
- Characterized by thickening and contraction of the glenohumeral joint capsule
- This leads to a severe loss of both the active and passive range of shoulder motion
- Occurs in three stages: freezing (increasing pain and stiffness), frozen (plateau of symptoms), and thawing (gradual resolution)
- More common in ages 40-60, diabetes, hypo/hyperthyroidism, cardiovascular disease
- The exact cause is unknown, may be due to an inflammatory response or scarring after injury
- Diagnosed based on a limited range of motion on the exam without changes in imaging
- Treatment tailored to the stage – NSAIDs, PT, steroids injections, manipulation under anesthesia
Dislocations
- When the humeral head is completely displaced from the glenoid socket
- Most often anterior direction due to mechanisms of injury
- Acute dislocations cause tears in the labrum and/or capsule of the shoulder joint
- Makes shoulder prone to recurrent instability and dislocations
- Presents with severe pain and deformity after a traumatic event
- Requires prompt closed reduction to relocate the humerus
- Follow-up imaging to assess for lesions, SLAP tears
- Later treatment may involve surgery to repair damaged tissues
Osteoarthritis
- Degenerative joint disease is marked by progressive loss of cartilage in the joint
- The humeral head and/or glenoid socket become rough, irregular surfaces
- Bony growths, osteophytes, appear as joint space narrows
- Causes gradual onset of pain, stiffness, and decreased mobility over time
- Diagnosed on x-ray showing joint space narrowing, bone spur changes
- Initial treatment conservative – rest, NSAIDs, PT, injections if needed
- The later stage may require shoulder arthroplasty (joint replacement)
- Autoimmune inflammatory disease causing swollen, painful joints
- Can affect the glenohumeral joint or acromioclavicular joint
- Leads to synovitis – inflammation of joint linings
- Causes cartilage and bone erosion over time
- Presents with pain, stiffness, decreased shoulder mobility
- Diagnosed via blood tests (for RA markers like RF and anti-CCP antibodies) and radiographic changes
- Treated with DMARDs, biologics, and steroids to reduce inflammation
- Physical therapy helps maintain range of motion and function
Injuries – fractures, sprains, strains
- Fractures occur when trauma causes the bone to break
- Common shoulder fractures include clavicle, proximal humerus, scapula
- Causes acute pain, swelling, and bruising after injury
- Diagnosed via x-ray, reduced range of motion on exam
- Requires immobilization, possible surgery depending on type/severity of fracture
- Sprains refer to stretched or torn ligaments, often acromioclavicular joint
- Strains are stretched or torn muscles or tendons, like biceps tendon
- Cause acute pain, weakness, and reduced shoulder function after the event
- Treated with rest, ice, NSAIDs, and rehabilitation exercises
Overuse
- Repetitive shoulder motions through extreme ranges of motion
- Common in overhead throwing athletes (pitchers), swimmers, weightlifters
- This leads to inflammation, microtears, impingement, tendinitis
- Presents as gradual onset pain with activities, loss of flexibility
- Requires activity modification, physical therapy, correcting mechanics
Age
- Degenerative changes like arthritis increase with older age
- Rotator cuff tears are closely associated with aging
- Prevalence of adhesive capsulitis peaks at ages 40-60 years old
- Older adults are more prone to injuries like fractures with falls
- Age impacts tissue quality – poorer healing, slower recovery
Sports with Repetitive Shoulder Motions
- Swimming – high volume of shoulder rotations during strokes
- Baseball pitchers – extreme shoulder rotation/acceleration with throwing
- Tennis players – repetitive overhead motions with serves, smashes
- Volleyball – repetitive overhead swinging for spiking
- Weightlifting – pressing, snatching, jerking place demand on shoulders
Occupations with Repetitive Motions
- Hammering, lifting materials overhead
- Using vibrating power tools
- This leads to rotator cuff tendinitis, tears
- Bursitis under acromion
Common Shoulder Pain Symptoms
Pain
- The most common shoulder pain symptom
- Pain can vary substantially depending on the underlying condition
- May be described as sharp, stabbing, dull, achy, throbbing
- Usually worsens with movement and may disrupt sleep
- Specific patterns can help indicate the cause:
- Anterior shoulder pain – often indicates an issue with rotator cuff tendons or bursitis
- Lateral/side shoulder pain – suggests involvement of acromioclavicular joint
- Posterior shoulder pain – commonly seen with dislocations or labral tears
- Important aspects include location, severity, duration, timing, precipitating factors
Joint Stiffness
- Many shoulder conditions limit normal mobility of the shoulder joint
- The capsular pattern of restriction distinguishes intrinsic conditions of the shoulder from referred pain
- Significant stiffness and loss of motion occur with adhesive capsulitis
- Shoulder osteoarthritis also greatly reduces the range of motion over time
Swelling
- Accumulation of fluid around shoulder structures
- Associated with acute injuries (sprains, fractures)
- Also present with bursitis, tendinitis as inflammatory response kicks in
- The glenohumeral joint effusion may cause diffuse shoulder swelling
- Localized soft tissue swelling over affected structure (e.g. acromioclavicular joint)
Tenderness
- Exquisite pain and discomfort with palpation over the affected structure
- Suggests inflammation, injury, and degeneration in that area
- Assessing the precise location of maximal tenderness aids diagnosis
Muscle Weakness
- Pain, swelling, and stiffness inhibit the ability to generate normal muscle strength
- Direct trauma to muscles/tendons reduces power
- Dynamic stabilizers like rotator cuff weakened with tendinosis
- Atrophy can develop in muscles if disuse/immobility
Crepitus
- Grating, crackling, and popping sensations in the shoulder
- Due to irregular joint surfaces rubbing together
- Common with osteoarthritis and other degenerative processes
Diagnosis and Testing
Medical History
- A key part of shoulder evaluation, provided by the patient
- Helps determine the onset, duration, severity, and location of pain
- Identifies inciting events or injuries
- Questions about specific aggravating/easing factors
- Prior treatments tried and related diagnoses
- Relevant medical issues, medications, imaging reports
- Thorough history guides diagnosis and treatment plan
Physical Exam
Range of Motion Assessment
- Active and passive ranges of motion measured
- Full arc typically is 0-180 degrees of forward flexion/abduction
- External rotation normally ~90 degrees
- Loss of motion suggests reduced joint mobility or pain inhibition
Strength Testing
- Manual muscle testing of rotator cuff and scapular muscles
- Ratings of normal, good, fair poor are based on the ability to resist
- Weakness signifies injury, disuse, imbalance, nerve issues
Palpation
- Shoulder structures palpated for point tenderness
- Most commonly anterior structures like bicipital groove, rotator cuff tendons
- Acromioclavicular joint tenderness suggests pathology there
- Pain out of proportion to the exam suggests alternate conditions
Special Tests
Rotator Cuff Tears
Drop Arm Test
- The patient asked to slowly lower the arm from a fully abducted position
- The inability to smoothly lower the arm suggests a rotator cuff tear
External Rotation Lag Sign
- Tests infraspinatus/teres minor strength
- Resistance is applied as the patient externally rotates
- Lag = possible posterior cuff tear
Adhesive Capsulitis
Passive Range of Motion Assessment
- Measure glenohumeral joint range with examiner moving arm
- A significant reduction in all planes indicates a frozen shoulder
Apprehension Test
- Pain/guarding at end-range on passive stretch signifies capsular tightness
SLAP Tears
O’Brien’s Test
- Pain on resistance during shoulder flexion + internal rotation suggests a labral tear
Crank Test
- The patient elevates the arm to 160 degrees then externally rotates
- Pain = possible SLAP lesion
Acromioclavicular Joint Injuries
Cross Body Adduction Test
- The patient forward flexes the affected shoulder to 90 degrees
- Examiner adducts arm across body
- Pain indicates AC joint pathology
Impingement Syndrome
Neer Impingement Sign
- Forced shoulder flexion with examiner stabilizing scapula
- Pain = positive sign of impingement
Diagnostic Test
X-ray
- First-line imaging modality due to accessibility, low-cost
- Useful for assessing bones, joints, and soft tissues indirectly
- Can detect dislocations, fractures, arthritis, calcific tendinitis
- Limited utility for muscles, tendons, and labrum which require cross-sectional imaging
MRI
- Gold standard imaging technique for shoulder
- Uses radio waves and magnets to produce 3D images with excellent soft tissue contrast
- Visualizes subtle bone marrow lesions, rotator cuff/labral tears, and capsule issues
- Relatively expensive, may require contrast (arthrogram) to enhance
Ultrasound
- Utilizes sound waves to dynamically visualize soft tissue structures
- No radiation exposure, relatively inexpensive
- Excellent for tendons, muscles, and bursae around the shoulder
- Operator-dependent, limited visualizing bones/intra-articular structures
CT Scan
- Uses rotating X-ray beams and detectors to generate cross-sectional images
- Superior bony imaging – fractures, dislocations, bone spurs
- Requires radiation exposure
- Primarily used after surgery or when MRI contraindicated
Choice of imaging guided by suspected pathology based on history, and physical exam. MRI is excellent for soft tissue injuries. X-ray best initial test for fractures, and arthritis. Ultrasound good dynamic study. CT provides a detailed bony assessment.
Treatment of Shoulder Pain
Medical Treatment
Rest & Ice
- Activity modification is essential early in injurious or inflammatory conditions
- Relative rest allows healing by reducing repetitive irritation
- Sling can provide support in cases of instability or after surgery
- Apply ice for 15-20 mins several times per day
- Helps control swelling and secondary hypoxic injury in acute injuries
- Also reduces pain and inflammation in overuse conditions
NSAIDs
- Oral non-steroidal anti-inflammatory drugs
- Help relieve pain stemming from inflammation
- Common options – ibuprofen (Advil), naproxen (Aleve), meloxicam (Mobic)
- The exact mechanism is not fully understood but likely to inhibit COX enzymes
- Can be used alongside other modalities like physical therapy
- Risks include GI upset, bleeding, cardiovascular and kidney injury
The initial treatment focus for most shoulder pain is conservative care with rest, ice, and NSAIDs to calm symptoms and allow healing. Relative rest means avoiding provocative activities but maintaining pain-free mobility exercises. More aggressive treatments may be warranted if there is no improvement or progressive worsening.
Heat Therapy
Heat therapy, also called thermotherapy, can be an effective part of a physical therapy program for treating shoulder pain and injuries. Heat helps in several ways:
- Increases blood flow – The warmth helps dilate blood vessels, increasing blood circulation to the shoulder area. This boosts oxygen and nutrient delivery to the tissues to promote healing.
- Reduces pain – The heat stimulates sensory receptors in the skin, which can decrease pain signals transmitted to the brain. It also increases the pain threshold.
- Relaxes muscles – The warmth relaxes tight, spasmed muscles around the shoulder joint. This reduces muscle tension, spasms, and associated pain.
- Improves flexibility – Warm tissues are more supple. Gentle stretching done with heat therapy can help improve shoulder joint and soft tissue flexibility.
- Reduces stiffness – Heat loosens stiff joints and eases tightness from scar tissue. This improves mobility.
Different heat modalities can be used:
Moist heat packs – Gel or fabric packs that can be heated in the microwave and applied to the shoulder. Provides steady, deep heating.
- Hot packs – Chemical packs that heat up when exposed to air. Easy to apply with adjustable wraps.
- Heating pads – Electric pads that deliver dry heat to the area. Good for home use.
- Hydrotherapy – Warm water immersion or moist hot packs. Provides deep heat with compression.
Proper technique is important. Heat should feel comfortably warm, not hot. Avoid direct contact with the skin. Limit to 15-20 minutes per session. Communicate with the therapist on effectiveness and precautions. Heat therapy, when combined with other treatments like gentle exercises, stretches, and manual therapy, can help provide relief from shoulder pain.
Cold Packs
Cold therapy can reduce inflammation, ease pain, and numb deep aches. Cold packs or ice massages for 10-15 minutes at a time can help, especially after activity or for acute injuries.
Manual Therapy
Hands-on techniques like massage, trigger point release, and joint mobilization provided by the physical therapist can help relax muscles, improve motion, mobilize the joint, and reduce pain.
Taping
Athletic tape or kinesiology tape can be used to support injured structures like tendons or muscles around the shoulder. Taping may help improve posture, alignment, and biomechanics to take pressure off the injured area during activity.
Postural Taping
Tape can also be applied to the upper back, neck, and chest to improve posture. Poor posture contributes to shoulder dysfunction. Taping cues proper postural alignment and activates muscles to enhance mechanics.
Electrotherapy Modalities
Laser Therapy
- Uses light energy to encourage healing and increase cellular activity.
- Helps reduce inflammation and swelling, easing pain.
- Improves microcirculation and speeds tissue repair.
- Low-level lasers penetrate deep into tissues.
- Treatment is painless, with no heat or vibration.
- Typically applied to the shoulder for 5-10 minutes per session.
Ultrasound Therapy
- Uses high-frequency sound waves delivered through the skin via a transducer.
- Generates deep heat to relax muscles, improve flexibility, and promote blood flow.
- Has pain-relieving effects and enhances tissue healing.
- The gel is applied to enhance conduction. The transducer is moved in circles over the treatment area.
- Therapy is applied for 5-10 minutes based on the condition, doctor’s orders, and patient feedback.
Shockwave Therapy
- Uses strong, focused acoustic pulses targeting damaged tissues.
- Stimulates inflammation and improves blood flow to deposit healing factors.
- Helps reduce calcifications, scar tissue adhesion, and shoulder capsulitis.
- No need to inject the shoulder. Pulses are focused on affected tissues.
- Sessions last 5-10 minutes and may require anesthetic cream.
TENS (Transcutaneous Electrical Nerve Stimulation)
- Uses mild electric current via surface electrodes placed on the skin.
- Stimulates nerves to block pain signal transmission.
- Provides short-term pain relief.
- Portable units allow for home use.
- Therapy is applied for 15-20 minutes up to multiple times per day.
These modalities are often used along with exercises, mobilization, and other treatments as part of a comprehensive shoulder rehabilitation program.
Physical Therapy Exercise for Shoulder Pain
Pendulum Exercise:

- Helps initiate shoulder joint mobility in a passive, gentle way.
- The patient leans forward at the waist, letting the affected arm hang down.
- Using the torso, the patient swings their arm back and forth and in circles slowly and smoothly.
- Allows gravity and momentum to move shoulder joints without active muscle contraction.
- Performed for 1-2 minutes at a time, 1-2 times per day.
- Helps loosen up joint stiffness and lubricate the shoulder.

Arm Across Chest Stretch:
- Stretches posterior shoulder structures like posterior deltoid
- The patient stands with an affected arm across the front of the chest.
- The other arm reaches across to grasp the affected arm above or below the elbow.
- Pull gently on the affected arm to feel a stretch in the back of the shoulder.
- Hold for 30 seconds, relax, repeat 2-4 times.
Shoulder Stretch:

- Stretches anterior shoulder muscles like pectoralis major.
- The patient stands in the doorway with the affected arm elevated to shoulder height.
- The arm is bent 90 degrees with the hand/forearm resting on the door frame.
- The patient leans forward through the door frame to feel a stretch across the front of the shoulder.
- Hold 30 seconds, relax, and repeat 2-4 times.
- Avoid over-arching low back.

Eagle Arms:
- Stretches upper back and shoulder muscles.
- Bring arms out to sides at shoulder height, elbows bent 90 degrees.
- Cross one arm over the other.
- Hands should be facing forward.
- Draw shoulders back and down, pressing elbows forward.
- Hold for 30 seconds, relax, switch arm positions, repeat 2-4 times.
Spinal Rolls:
- Mobilizes thoracic spine and scapula.
- Sit or stand with knees slightly bent.
- Keep shoulders relaxed and chin tucked slightly.
- Slowly roll shoulders up, back, and down in a smooth motion.
- Focus on controlled movement through full range of motion.
- Repeat 10-15 times. Can do a few sets.
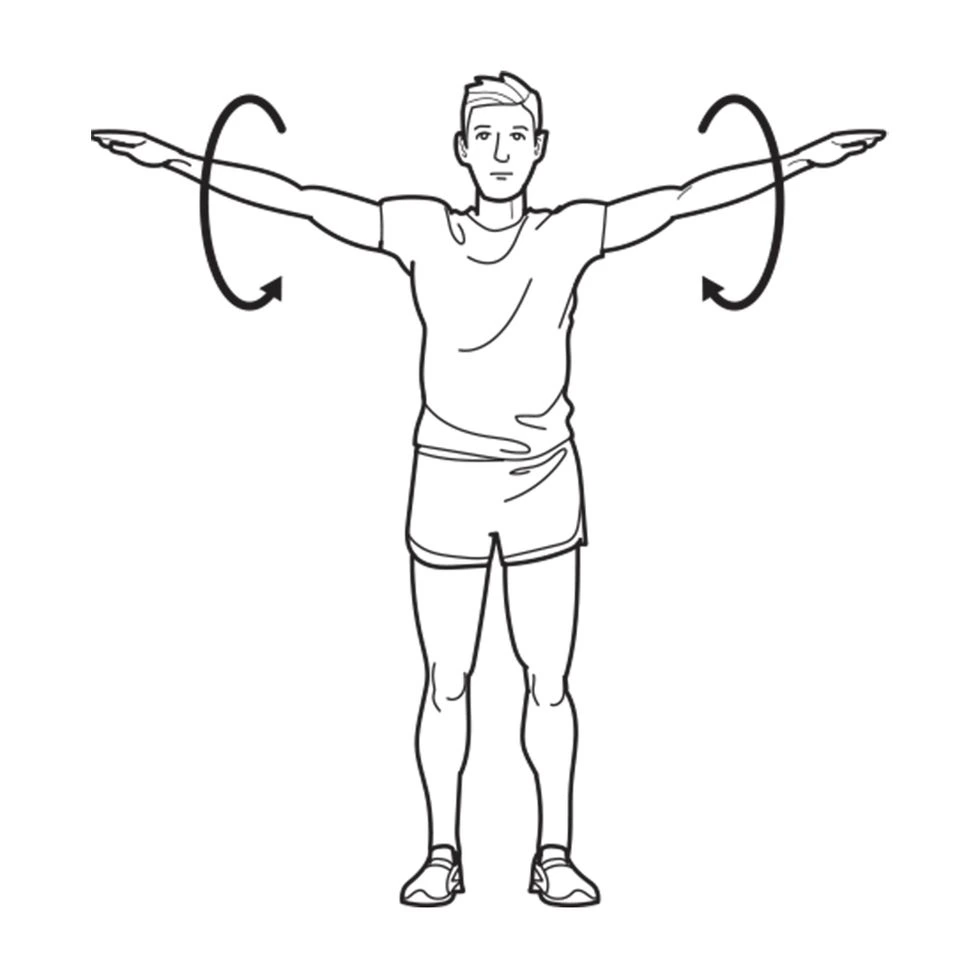
Shoulder Circles:
- Mobilizes shoulder joint through full range of motion.
- Stand or sit tall. Using small, controlled motions:
- Circle shoulders forward 10 times.
- Circle shoulders backward 10 times.
- Make small circles with just the affected shoulder 10 times forward and backward.
- Keep movements slow and controlled.

Doorway Shoulder Stretch:
- Focuses on the chest and front of the shoulder muscles
- Stand in the doorway with the affected arm up, elbow bent 90 degrees.
- Rest forearm on the door frame.
- Slowly lean your body forward through the door frame until a stretch is felt across the front of the shoulder.
- Hold for 30 seconds, relax, repeat 2-4 times.
- Keep your back straight, don’t arch your lower back.
Downward Dog Pose:
- Focuses on posterior shoulder muscles.
- Start on the floor, hands and knees. Hands shoulder-width apart.
- Curl toes under, straighten knees and hips, lifting knees off the floor.
- Press into hands, straighten arms, and press chest back toward thighs.
- Keep shoulders down, and neck relaxed.
- Hold for 30 seconds, repeat 2-4 times.
Child’s Pose:
- Provides gentle shoulder stretch.
- Kneel on the floor with toes together, knees hip-width apart.
- Sit back on your heels, bringing your chest down between thighs.
- Reach arms forward fully, lowering forehead to the floor.
- Hold for 30 seconds, focus on releasing your shoulders down.
- Repeat 2-4 times.

Thread the Needle:
- Targets rotator cuff and posterior shoulder.
- Start on hands and knees on the floor with knees under hips and hands under shoulders.
- Bring right arm under left, rotating right shoulder down and back.
- Palm faces ceiling as right arm threads under the left armpit.
- Feel stretch in the right shoulder. Hold 15-30 seconds. Repeat both sides 2-4 times.
Neck Stretches:

- Stretches neck, upper trapezius, and levator scapulae.
- Sit or stand tall. Look straight ahead.
- Slowly tilt the head to the right, feeling stretch on the left side of the neck. Hold 15 seconds.
- Slowly tilt the head to the left, feeling stretch on the right side of the neck. Hold 15 seconds.
- Repeat 2-4 times per side. Don’t tilt your head back.
Standing Upright Rows:
- Strengthens shoulders and upper back muscles.
- Stand holding dumbbells in front of thighs, palms facing the body.
- Engaging core, pull dumbbells straight up toward chin, elbows out.
- Slowly lower back to start position.
- Repeat 10-15 times, 2-3 sets. Keep elbows above wrists.
Surgical Treatment
Arthroscopic Surgery: This is one of the most common surgeries for shoulder pain. The surgeon makes small incisions and inserts a tiny camera called an arthroscope to see inside the shoulder joint. They can diagnose problems and repair injuries like rotator cuff tears. During arthroscopy, the surgeon may debride damaged tissue, remove bone spurs, or fix labral tears.
Rotator Cuff Repair: This surgery is done to reattach torn tendons in the rotator cuff. The rotator cuff is made up of muscles and tendons that surround the shoulder joint and help stabilize it. Tears are common with age or injuries. In a cuff repair, the surgeon will suture the torn tendon back to the bone. This is often done arthroscopically but may require an open incision.
Shoulder Replacement: Also called shoulder arthroplasty, this surgery replaces the damaged ball and socket of the shoulder joint. The humeral head (ball) and glenoid (socket) are replaced with artificial implants made of metal and plastic. Total shoulder replacement replaces both sides, while partial replacement is just the ball or socket. It’s done when arthritis, fractures, or injury damage the joint extensively.
Acromioplasty: This removes bone from the acromion and creates more space in the subacromial area. The acromion is the bony tip of the shoulder blade that arches over the humerus. Removing a portion can relieve impingement and irritation that causes rotator cuff tears or tendinitis. It’s often done with arthroscopy.
The specific surgical treatment will depend on the underlying cause and severity of the shoulder pain and injury. Non-surgical options like rest, physical therapy, medications, and injections may be tried first. If pain persists and function is limited, surgery like these options could help repair damage and restore mobility.
Shoulder Pain Prevention Strategies:
Rotator Cuff Exercises
- Strengthening rotator cuff muscles critical for injury prevention
- Improves dynamic stabilization of shoulder joint
- Prevents abnormal translations of the humeral head with movement
Basic exercises:
- External and internal rotation with resistance band
- Front and side arm raises
- Shoulder extension, adduction, and retraction motions
Aim for 2-3 sets of 10-15 reps to fatigue for each movement pattern
Proper Overhead Motion Technique
Overhead motions make the shoulder vulnerable to overuse issues
Proper mechanics protect structures:
- Avoid excessive arching of the lower back
- Maintain core engagement and neutral spine posture
- Initiate movement using legs and hips
- Lead motion with elbows vs. opening hands/wrists first
- Control the descent phase rather than letting arms fall
- Stop activity before fatigue/compensation
Taking Breaks
- Frequent short breaks are vital for occupations requiring repetitive motions
- Continuous repetition overworks tissues beyond capacity
- Regularly scheduling brief rest periods can dramatically reduce overuse
- Adequate recovery time allows the restoration of muscle energy stores and tissue resilience
General guidelines:
- Take at least 5-10 mins break after each hour of repetitive work
- Alternate repetitive tasks with other duties
- Avoid repetitive motion again until the shoulder feels fully recovered
Maintaining Appropriate Posture
- Poor posture contributes to shoulder dysfunction and pain
- Slumped posture encourages internal rotation, poor mechanics
- Head forward posture overstretches anterior shoulder structures
- Rounded shoulders cause impaired rotation, nerve compression
- The idea is an upright neutral posture with shoulders back and down
- Can improve posture by stretching tight muscles and strengthening weak ones
- Cueing techniques help train optimal alignment
Home Care Management for Shoulder Pain
Rest
- Take breaks from repetitive, overhead activities as this can further irritate injured structures
- Use a sling for a few days following injury to prevent additional stress on the injured shoulder
- Find alternative options for heavy lifting and chores around the house that aggravate symptoms
Ice
- Apply ice packs wrapped in a towel for 10-15 minutes several times per day
- Most beneficial in the first 72 hours after acute injury to control inflammation and pain
- Can also use ice for symptomatic relief with chronic overuse injuries like tendinitis
Heat
- Apply moist heat pads or take warm showers to improve blood flow and relax muscles
- Best once acute inflammation has settled from the initial injury
- Helps prepare tissues for gentle stretching and exercises
Medications
- Over-the-counter NSAIDs such as ibuprofen and naproxen to relieve pain and inflammation
- Acetaminophen can help shoulder pain without reducing inflammation
- Use oral medicines as directed on the packaging
Correction of Posture/Mechanics
- Ensure proper upright posture especially when performing overhead tasks and activities
- Modify the technique of aggravating motions to reduce overuse
Home Exercise Program
- Targets flexibility, strength, stretching of key shoulder muscles
- A specific program designed by a physical therapist
- Compliance crucial for recovery
Avoiding activities that increase shoulder symptoms and continuing home care under the guidance of a physical therapist facilitates recovery. Close follow-up monitoring of progress is key.
Summary
Shoulder pain is an exceedingly common issue that affects people of all ages. It can severely impact the quality of life and the ability to carry out activities when it arises. The shoulder’s wide mobility makes it prone to injury, overuse, and various pathologies causing pain. Typical symptoms include pain, stiffness, instability, and weakness that can limit shoulder function.
Many factors lead to shoulder issues, most commonly rotator cuff injuries, bursitis, tendinitis, arthritis, and impingement. Repetitive motions in many occupations and sports contribute to overuse. Acute injuries like dislocations also frequently occur. Understanding the intricately complex shoulder anatomy helps distinguish causes of pain for proper diagnosis.
Assessing a patient’s medical history and doing a thorough physical exam helps determine the underlying shoulder problem. Certain tests checking the range of motion, strength, and stability provide valuable clues. Medical imaging like MRI scans can visualize soft tissue lesions often responsible. An accurate diagnosis and prompt intervention are crucial for an optimal outcome.
Many cases of shoulder pain can be treated successfully with conservative measures like rest, ice, medications, corrective exercises, and physical therapy. However, surgical procedures like rotator cuff repair or shoulder replacement may be needed for more severe cases. Preventative steps including technique adjustments, muscle balancing, and taking adequate breaks can also help ward off overuse shoulder injuries. When managed appropriately, shoulder pain generally carries an excellent overall prognosis.
FAQs
What are the most common causes of shoulder pain?
Some of the most common causes of shoulder pain include rotator cuff tears or tendinitis, frozen shoulder, dislocated shoulder, arthritis, fractures, and muscle strains. Overhead motions and repetitive use can also lead to shoulder pain.
When should I see a doctor for shoulder pain?
See your doctor if the shoulder pain comes on suddenly, causes significant loss of function or mobility, follows an injury, persists beyond a few days, or is unrelieved with self-care. Worsening pain and swelling also warrant medical evaluation.
How is the cause of shoulder pain diagnosed?
Your physician will diagnose the cause of shoulder pain based on medical history, description of symptoms, physical examination of the shoulder, and possibly imaging tests like x-ray, MRI, or ultrasound. They may also order blood tests. These provide information to determine the specific tissue involved.
What is the best initial treatment for shoulder pain?
The best initial treatment involves rest, ice packs applied for 15 minutes several times per day, over-the-counter anti-inflammatory medication, and modification of activities that aggravate the pain. See a physical therapist to begin gentle mobility and strength exercises.
When would surgery be necessary for a painful shoulder?
Surgery may be necessary if there is significant damage to tissues like a full-thickness rotator cuff tear, labral tear, recurrent shoulder dislocations, or fractures that have not healed properly with conservative treatment. Severe, debilitating arthritis can also require shoulder replacement.
What prevents developing shoulder pain?
Surgery may be necessary if there is significant damage to tissues like a full-thickness rotator cuff tear, labral tear, recurrent shoulder dislocations, or fractures that have not healed properly with conservative treatment. Severe, debilitating arthritis can also require shoulder replacement.
Once treated, can shoulder pain reoccur?
Yes, shoulder pain can reoccur if underlying causes like poor posture or overuse issues are not corrected. Certain conditions like shoulder instability can lead to recurrent dislocations and pain if not addressed surgically. Complete any recommended rehabilitation program fully to prevent re-injury.
What is the outlook for people with shoulder pain?
With appropriate diagnosis and treatment interventions, whether conservative care or surgical management when necessary, most people with shoulder pain will make a complete recovery and regain good shoulder function over time. Early intervention leads to the best outcomes.
References
Wadehra, S. (2019, January 22). What to know about front shoulder pain. https://www.medicalnewstoday.com/articles/324246
Therapeutic Exercise for the Shoulder. (n.d.). Physiopedia. https://www.physio-pedia.com/Therapeutic_Exercise_for_the_Shoulder
Cronkleton, E. (2023, February 3). Top 10 Exercises to Relieve Shoulder Pain and Tightness. Healthline. https://www.healthline.com/health/shoulder-pain-exercises#prevention
Cronkleton, E. (2023, February 3). Top 10 Exercises to Relieve Shoulder Pain and Tightness. Healthline. https://www.healthline.com/health/shoulder-pain-exercises#prevention
Dhameliya, N. (2023, May 31). Shoulder Pain : Cause, Symptom’s, Physiotherapy Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/shoulder-pain/
Tirgar, P. (2024, February 1). Shoulder Pain: Causes, Diagnosis and Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/shoulder-pain/
Eske, J. (2023, March 3). 10 exercises for shoulder pain. https://www.medicalnewstoday.com/articles/shoulder-pain-exercises#other-treatment-options
https://th.bing.com/th/id/OIP.ubmRe_QJapcmzII4Q1qPYwHaE8?rs=1&pid=ImgDetMain




25 Comments