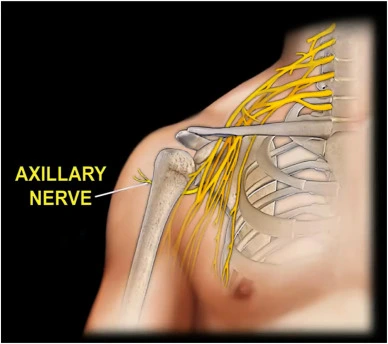
Axillary Nerve Injury
Axillary nerve injury results in a condition that occurs when the axillary nerve is damaged. The axillary nerve is a nerve that runs from the upper back down the arm to the shoulder. The axillary nerve originates in the shoulder region from the brachial plexus.
It supplies sensation to the skin across the shoulder and upper arm and motor function to the deltoid muscle, the rounded muscle on top of the shoulder, and the teres minor, the smaller muscle beneath the deltoid.
The axillary nerve, which runs from your neck to your shoulder, can sustain damage that could be dangerous. Overstretching the nerve is often the cause of them. An injury or compression of the axillary nerve commonly results in pain and weakness in the arm or shoulder. Most of these injuries heal on their own or with the help of conservative treatments like physical therapy and medication.
What Is the Axillary Nerve? Anatomy and its Function
The brachial plexus, a network of nerves that extends from your neck and upper torso to your shoulders and arms, includes the axillary nerve as a branch. Since these nerves are not part of your brain or spinal cord, they are referred to as peripheral nerves.
The C5 and C6 vertebrae in your neck are the source of the axillary nerve, which runs into your shoulder. It facilitates shoulder rotation and raises your arm off your body.
Overview
- Spinal roots: C5 and C6 are the spinal roots.
- Sensory functions: Originates the upper lateral cutaneous nerve of the arm, innervating the skin over the region known as the “regimental badge area” over the lower deltoid.
- Motor functions: Innervates the minor deltoid and teres muscles, among other motor tasks.
Anatomical Route
- Within the upper limb’s axilla, the axillary nerve develops. It has fibers from the C5 and C6 nerve roots since it is a direct continuation of the posterior cord from the brachial plexus.
- The axillary nerve is situated in the axilla anterior to the subscapularis muscle and posterior to the axillary artery.
- It leaves the axilla through the quadrangular space at the inferior border of the subscapularis, frequently with the posterior circumflex humeral artery and vein accompanying him. After that, the axillary nerve travels medially to the humerus’ surgical neck, where it splits into three terminal branches:
- Anterior terminal branch: The anterior side of the deltoid muscle receives motor innervation from the anterior terminal branch, which encircles the humeral surgical neck. It ends with cutaneous branches that go to the shoulder’s anterior and anterolateral regions.
- Posterior terminal branch: The posterior aspect of the deltoid muscle and the teres minor receive motor innervation from the posterior terminal branch. As the upper lateral cutaneous nerve of the arm, it also innervates the skin across the inferior portion of the deltoid.
- Articular branch: The glenohumeral joint is supplied by the articular branch.
Motor Function
Both the teres minor and deltoid muscles are innervated by the axillary nerve.
- Teres Minor: A portion of the rotator cuff muscles that stabilize the glenohumeral joint is called the teres minor. It is innervated by the axillary nerve’s posterior terminal branch and serves to rotate the shoulder joint externally.
- Deltoid: located at the shoulder’s superior aspect. It is supplied by the axillary nerve’s anterior terminal branch and performs the glenohumeral joint abduction of the upper limb.
Sensory Function
- The axillary nerve’s posterior terminal branch delivers the sensory component. The posterior terminal branch of the axillary nerve, which also continues as the upper lateral cutaneous nerve of the arm, serves the teres minor. The “regimental badge area” is the inferior part of the deltoids innervated by it.
- Sensation at the regimental badge location may be absent or diminished in a patient with axillary nerve injury. Additionally, the patient may experience paraesthesia (pins and needles) in the axillary nerve distribution.
Clinical Significance: Damage to the Axillary Nerve
Trauma to the shoulder girdle or proximal humerus can injure the axillary nerve. Injuries to the brachial plexus are frequently observed. Shoulder dislocation, accidental harm during shoulder surgery, and fracture of the humeral surgical neck are common sources of injury.
- Motor functions: The patient will not be able to abduct the affected limb beyond 15 degrees due to motor function impairments affecting the deltoid and teres minor muscles.
- Sensory functions: Sensation over the inferior deltoid (also known as the “regimental badge area”) will be lost due to damage to the upper lateral cutaneous nerve of the arm.
- External rotation slowness and deltoid extension delays are two examples of clinical examinations. Muscle atrophy, neuropathic discomfort, and persistent numbness at the lateral shoulder region can all be caused by long-term axillary nerve lesions.
Causes of the Axillary Nerve Injury
Axillary nerve dysfunction can result from several factors, such as:
- Trauma to the shoulder, such as a fracture, dislocation, or crush injury.
- Entrapment of the nerve by adjacent tissues, including hematomas, tumors, or swollen lymph nodes.
- Nerve inflammation, such as that caused by an autoimmune condition or a virus.
- Iatrogenic factors include radiation treatment or surgery for the shoulder.
- Repetitive shoulder motions, such as those used in weightlifting or throwing.
- Heavy items are carried for extended lengths of time on one shoulder.
- Sleeping for extended lengths of time on one arm.
Symptoms of the Axillary Nerve Injury
The following are signs of dysfunction of the axillary nerve:
- Shoulder Pain mainly in the upper arm or shoulder
- Shoulder weakness that makes it challenging to raise the arm When attempting to elevate the arm away from the body, as in brushing your hair or reaching for something on a high shelf, this weakness is most apparent.
- The skin above the shoulder and upper arm feels numb or tingly. The outer part of the upper arm, over the deltoid muscle, is usually where this numbness is felt.
- The degree of nerve damage can affect how severe these symptoms are. Some people may only feel slight weakness or pain in certain situations.
- In other situations, weakness and intense discomfort could make things challenging to perform everyday actions.
Risk Factors of the Axillary Nerve Dysfunction
The following are risk factors for dysfunction of the axillary nerve:
- Trauma to the shoulder: The most frequent cause of dysfunction in the axillary nerve is trauma to the shoulder. Fractures, dislocations, and penetrating injuries to the shoulder are examples of trauma. This may occur from falls, contact sports, or other mishaps.
- Compression of the nerve in the armpit: Hemostasis (blood clots) in the armpit, swollen lymph nodes, or tumors can all contribute to nerve compression there. Compressing the nerve can also occur with prolonged use of backpacks with extremely tight straps.
- Repetitive overhead movements: Athletes who engage in activities like baseball, tennis, and weightlifting, which require repetitive overhead motions, are frequently at risk for this. Repeated movements might cause inflammation by causing nerve irritation.
- Overuse of slings or crutches: Inappropriate usage of crutches or a sling might cause harm by applying pressure on the axillary nerve.
- specific medical disorders: The wide name for nerve damage that can affect the axillary nerve is neuropathy, and conditions like diabetes and obesity can make you more likely to get it.
- Previous shoulder surgery: There is a little chance that the axillary nerve may be harmed if you have had shoulder surgery.
- It’s crucial to remember that not everyone who has these risk factors will experience dysfunction of the axillary nerve. Nonetheless, you can take precautions to safeguard your shoulders and lower your risk of getting the condition if you are aware of these hazards.
Diagnosis for the Axillary Nerve Dysfunction
A combination of a physical examination and nerve function tests is usually used to diagnose axillary nerve impairment.
Physical Examination
Your doctor will question you about your symptoms during a physical examination, including:
- When did your symptoms start?
- How bad your suffering is
- Any shoulder trauma in the past?
- Whether your arm is weak or numb in any way
- In addition, your physician will examine your shoulder to check for atrophy, weakness, and soreness over the axillary nerve in the deltoid muscle.
- Your shoulder’s range of motion and your capacity to detect a light touch on the skin of your upper arm and shoulder will also be tested.
Tests
Axillary nerve dysfunction can be diagnosed with several tests, such as:
- EMG, or electromyography: An EMG test is used to evaluate muscular electrical activity. By evaluating the condition of the deltoid muscle, which the axillary nerve regulates, it can be utilized to identify injury to the axillary nerve.
- Nerve Conduction Studies: Studies known as nerve conduction studies (NCS) are used to quantify the strength and speed of signals that pass through nerves. They can be utilized to discover whether the axillary nerve is damaged or blocked.
- Radiography: X-rays can be utilized to rule out arthritis or fractures as other reasons for shoulder pain.
- Other procedures, such as blood testing to look for diseases like diabetes that can cause neuropathy, might be required in certain situations.
The particular tests that are ordered will be determined by your specific situation.
Differential Diagnosis for the Axillary Nerve Injury
To determine the exact cause of the symptoms in the case of axillary nerve dysfunction, a differential diagnosis is essential. When making an axillary nerve dysfunction diagnosis, a physician may take into account the following conditions:
- Cervical Radiculopathy: This disorder results from a neck nerve root being irritated or compressed. While it can produce symptoms akin to numbness, weakness, and shoulder pain, it frequently travels down the arm along a particular nerve pathway.
- Thoracic Outlet Syndrome: Compression of blood arteries, nerves, or muscles in the upper chest can result in thoracic outlet syndrome. It can show tingling in the fingers and hand, but it can also mimic axillary nerve dysfunction with pain, weakness, and numbness in the arm and shoulder.
- Rotator Cuff Tear: Shoulder pain and weakness may result from a tear in the rotator cuff tendons, which stabilize the shoulder joint. Large tears can occasionally impinge on the axillary nerve, producing weakness in abduction the ability to move the arm away from the body even though they do not directly impact the nerve.
- Brachial Plexopathy: More serious damage known as brachial plexopathy affects the entire network of nerves (brachial plexus) that supplies the hand, arm, and shoulder. To distinguish it from isolated axillary nerve failure, it can result in extensive discomfort, weakness, and sensory loss throughout the arm.
- Quadrilateral Space Syndrome: This less prevalent ailment is characterized by compression of the axillary nerve inside a particular armpit compartment. Though there may be a palpable mass under the armpit and a more concentrated area of weakness, the symptoms are similar to those of axillary nerve dysfunction.
- Brachial Neuritis: Usually brought on by a viral infection, this condition is an inflammation of the brachial plexus nerves. Though the shoulder and arm may experience abrupt onset discomfort, weakness, and numbness, it usually gets better faster than axillary nerve dysfunction.
- Glenohumeral Joint Fracture/Dislocation: Shoulder joint fractures or dislocations can occasionally cause axillary nerve damage. This would manifest as a combination of the fracture/dislocation symptoms and possible malfunction of the axillary nerve, such as weakness.
- Subacromial Impingement Syndrome: Tendons under the shoulder acromion bone can get pinched in subacromial impingement syndrome. Although its main effect is pain, it can occasionally irritate surrounding nerves, resulting in some weakening and numbness that could be mistaken for malfunction of the axillary nerves.
- Herpes Zoster (Shingles): Anywhere on the body, including the nerves in the shoulder, can get infected with this virus. Shingles can be differentiated from axillary nerve dysfunction by its characteristic rash and burning pain.
Treatment for the Axillary Nerve Injury
The underlying cause and extent of the nerve injury determine the treatment plan for axillary nerve dysfunction. The following is a summary of possible treatment choices:
Non-surgical methods:
- Rest and Activities modification: Resting the shoulder and avoiding activities that exacerbate the pain will often allow the nerve to recover on its own, especially for minor injuries. To prevent undue strain, this may need wearing a sling for brief periods.
- Physical Medicine: Regaining the shoulder’s strength, flexibility, and range of motion requires physical therapy. A therapist can create a customized workout plan to enhance muscular performance and stop weakness-related muscle atrophy.
- Medication: Pain and inflammation can be managed with the aid of medications. Choices consist of:
- Painkillers are available over-the-counter: These can be used to treat mild to moderate pain. Acetaminophen and ibuprofen are two examples.
- Prescription painkillers: More potent drugs may be recommended for cases of extreme pain.
- Anti-inflammatory drugs: Drugs such as corticosteroids can aid in the healing process by lowering inflammation surrounding the nerve.
- Electrical Stimulation: Pain management and improved muscular function can occasionally be achieved with methods such as transcutaneous electrical nerve stimulation (TENS).
Surgical intervention:
Generally, non-surgical therapy is tried for a considerable amount of time before considering surgery (generally 6-12 months). The following are a few possible surgical options:
- Nerve decompression: Surgery may be necessary to remove the source of compression and release the nerve if it is being compressed by tumors, scar tissue, or swollen lymph nodes.
- Nerve grafting or repair: Surgeons may choose to replace a damaged nerve with a healthy one from another area of the body to bridge the gap and encourage regeneration in cases of severe nerve damage.
Additional issues to think about:
- Treating the underlying causes: Managing an underlying medical condition, such as diabetes, is essential for the best possible recovery if nerve damage is being caused by it.
- Steroid injections: Although their usage is restricted owing to possible adverse effects, steroid injections may be used in some circumstances to lessen inflammation surrounding the nerve.
- Prognosis: Depending on the extent of the injury, healing times for axillary nerve dysfunction vary. With the right care, a full recovery may happen in a few months in certain situations. But in extreme circumstances, there can be some residual lifelong paralysis or numbness.
A vital part of treating axillary nerve dysfunction is physical therapy. Its main goals are to increase the range of motion, strength, and flexibility in the shoulder joint with the ultimate goal of reducing discomfort and restoring function.
Physical Therapy for the Axillary Nerve Injury
A physical therapist will create a customized exercise plan for you depending on how severe your ailment is and how you’re doing over time. What to anticipate from physical therapy for axillary nerve dysfunction is outlined below in general terms:
Early Stage:
- Pain Management: To reduce pain and inflammation, try cold therapy, electrical stimulation (TENS), and ultrasound.
- Posture Correction: The therapist will examine your posture and provide you with exercises to strengthen and correct your shoulders, which can help your nerves repair more indirectly.
- Mild Range-of-Motion Exercises: These will assist in preserving and progressively enhancing your shoulder joint’s range of motion, hence reducing stiffness.
Progressive Stages:
- Strengthening Exercises: The therapist will start you on exercises to strengthen the muscles surrounding your shoulder, especially the deltoid muscle, which is mostly controlled by the axillary nerve, as soon as the pain goes away and you can move around a bit. This enhances the shoulder’s stability and functionality.
- Neuromuscular Re-education: By retraining the muscles to react more favorably to nerve signals, methods such as neuromuscular electrical stimulation (NMES) can enhance muscular control.
- Stretching Exercises: By extending the range of motion and improving flexibility, stretching exercises for the shoulder and chest muscles can aid in promoting more comfortable movement.
Functional Education:
- Progressive The Return of Activities: To assist you in safely returning to your routine, the therapist will progressively include exercises that replicate your everyday activities or your sports-related movements.
- Exercises for Balance and Proprioception: You can strengthen and stabilize your shoulder by performing exercises that test your body’s awareness of its position in space and balance.
Home Exercise Programme: To sustain the gains acquired during therapy sessions and to continue strengthening the shoulder, the therapist will prescribe you a customized home exercise program to follow daily
Additional Things to Consider:
- Patient Education: The therapist will instruct you on how to prevent further injury, the significance of using the correct form during workouts, and axillary nerve dysfunction.
- Communication: Having open lines of communication with your therapist is essential during treatment. Tell them if you feel any pain or discomfort when performing the exercises so they can modify the program.
Recall that you and your therapist work together throughout physical therapy. You can greatly increase your chances of restoring shoulder strength, flexibility, and function by consistently carrying out the prescribed exercises as well as by routinely attending therapy sessions.
Complications for the Axillary Nerve Injury
Dysfunction of the axillary nerve can result in several consequences, such as:
- Sensory loss: This can make it harder to detect pain or temperature changes, resulting in numbness or tingling in the upper arm and shoulder.
- Muscle weakness can make moving objects or elevating the arm overhead challenging. The primary muscle responsible for raising the arm, the deltoid, may become paralyzed in extreme circumstances.
- Persistent pain: This could be an aching or burning sensation in the arm and shoulder. It may result from misuse of other muscles due to muscle weakening or damage to the nerve itself.
- A frozen shoulder is a painful and stiff ailment affecting the shoulder joint. The inability to move the shoulder joint due to weakness in the deltoid muscle might be a consequence of malfunction of the axillary nerve.
- Skin issues: An axillary nerve injury may also result in excessive perspiration, dryness, or trouble healing from wounds in the armpit area. This is due to the nerve’s role in regulating local blood flow and sweat gland activity.
Prevention for the Axillary Nerve Injury
Although axillary nerve dysfunction cannot be completely prevented, several tactics can greatly lower your risk:
- Keep your posture straight: Maintaining good posture helps to soothe your nerves and keeps your shoulders in alignment. Try not to slouch by keeping your shoulders relaxed and back.
- Exercise with correct form: Pay attention to your form when lifting weights, throwing, and performing other shoulder-related exercises. A licensed physical therapist or trainer can advise you on the appropriate form.
- Avoid repetitive overhead motions: These movements, which are typical in various occupations and sports, might aggravate the axillary nerve. To lessen tension, take frequent pauses, stretch frequently, and think about other methods.
- Keep your weight in check: Being overweight raises your risk of experiencing compression on any nerve in your body, including the axillary nerve.
- Make sure you use slings and backpacks appropriately. If you’re using a backpack, make sure the straps are adjusted to maintain a balanced distribution of weight and to keep your armpits free from excessive tightness. To avoid putting pressure on the nerves following surgery, sling use should be done as directed by a medical specialist.
- Treat underlying problems: If you have diabetes or other disorders that make you more susceptible to neuropathy, taking good care of them can lower your risk of developing nerve damage, including damage to the axillary nerve.
- Exercise caution when participating in contact sports: Wear the necessary protective gear and use proper tackling or blocking methods to reduce the chance of fractures or dislocations that could injure the nerve.
- Exercise before and after warming up and cooling down: Warming up properly improves blood flow to your muscles and gets them ready for action while cooling down lowers the chance of injury and helps you avoid stiffness.
- Pay attention to your body. Be mindful of any shoulder soreness or discomfort. Put an end to painful activities and seek medical attention if symptoms don’t go away.
- Sustain appropriate blood sugar regulation: Those who have diabetes may be able to avoid peripheral neuropathy by keeping their blood sugar levels in check.
Summary
The axillary nerve is attached to your shoulder. It allows you to rotate and extend your arm and provides you with feeling. Damage to the axillary nerve can occur for a variety of reasons. They could cause issues like paralysis in the arms.
You can prevent some injuries by using safety equipment and using extra caution to prevent falls. If you have a shoulder injury or other problems, don’t be afraid to get in touch with your doctor.
FAQs
How is dysfunction of the axillary nerve treated?
If a trapped nerve is the source of your symptoms, surgery to release the nerve may make you feel better. Physical therapy can help maintain muscle strength. Other forms of therapy, such as muscle retraining or job adjustments, could be suggested.
What occurs when the axillary nerve is injured?
What occurs when the axillary nerve is injured?
The lateral shoulder region is permanently numb due to chronic axillary nerve lesions, the deltoid and teres minor muscle atrophy, and probably persistent neuropathic discomfort.
How Is an Axillary Nerve Injury Treated?
Steroids to reduce swelling.
NSAIDs, or non-steroidal anti-inflammatory Medicines, reduce pain and inflammation.
Painkillers.
Physical treatment to increase the flexibility and strength of muscles.
Workouts involving shoulder rotation.
Arm and shoulder stretches.
Is it possible to treat nerve dysfunction?
Is it possible to treat nerve dysfunction?
There are several cases when nerve injury is incurable. However, several therapies can lessen your symptoms. Nerve damage usually gets worse with time, so it’s important to visit a doctor as soon as symptoms arise. In this manner, you can lessen the possibility of long-term harm.
How much time does the axillary nerve take to heal?
In 6 to 12 months, full healing happens 85–100% of the time under conservative care. As the tissues from the shoulder dislocation heal muscle weakness brought on by the axillary nerve lesion may go away on its own.
When you have axillary nerve discomfort, how do you sleep?
If you have pinched nerves in your shoulder or arm, it’s recommended that you sleep on your side. To alleviate your problems, you must sleep on the side without the pinched nerve. Sleep on your back with your arms straight if it affects both of your arms.
References
- Axillary nerve dysfunction. (n.d.). Mount Sinai Health System. https://www.mountsinai.org/health-library/diseases-conditions/axillary-nerve-dysfunction#:~:text=Axillary%20nerve%20dysfunction%20is%20a,axillary%20nerve%2C%20is%20called%20mononeuropathy.
- Tessler, J., & Talati, R. (2023, August 14). Axillary nerve injury. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK539895/
- Axillary nerve injury. (n.d.). Physiopedia. https://www.physio-pedia.com/Axillary_Nerve_Injury
- Whitten, C. (2021, December 16). What to know about an axillary nerve injury. WebMD. https://www.webmd.com/pain-management/what-to-know-about-axillary-nerve-injury
- Phillips, N. (2018, September 29). Isolated nerve dysfunction. Healthline. https://www.healthline.com/health/isolated-nerve-dysfunction
- Professional, C. C. M. (n.d.-a). Axillary nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22264-axillary-nerve