De Quervain’s Tenosynovitis
What is a De Quervain’s Tenosynovitis?
De Quervain’s Tenosynovitis is a painful condition that affects the tendons in the wrist and base of the thumb. It takes the name Fritz de Quervain in honor of the Swiss surgeon who discovered the condition in 1895.
Overview
Definition: De Quervain’s tenosynovitis is a type of tendon injury characterized by inflammation of the sheath or covering around the tendons that control movement of the thumb. Specifically, it involves swelling of the tendon sheath surrounding the abductor pollicis longus and extensor pollicis brevis tendons as they travel through a tunnel on the thumb side of the wrist.
The exact cause is often unknown, but it is associated with repetitive hand or wrist motions, such as wringing out towels or other forceful grasping. It can also occur during pregnancy, likely due to swelling and fluid retention, or after a direct injury to the wrist or thumb area.
Diagnosis involves a physical exam to check for tenderness and perform maneuvers that reproduce the pain. Imaging tests like X-rays may rule out other conditions.
Treatment typically starts with resting the thumb/wrist, anti-inflammatory medications, a splint or brace, and modifying activities. Steroid injections or surgery may be recommended if symptoms persist.
Causes of De Quervain’s Tenosynovitis
The exact cause of De Quervain’s tenosynovitis is often unknown, but it is typically associated with overuse or repetitive movements that put strain on the tendons around the base of the thumb. Several potential contributing factors and causes have been identified:
Overuse Injury: With repeated use, the synovial sheath surrounding injured tendons may become irritated and inflamed, particularly when vigorous movement or wringing motions are performed. This is common in jobs or activities that involve:
- Repetitive hand-twisting motions
- Frequent lifting or carrying of babies/young children
- Sports that require a firm grip like golf, tennis, rowing
- Frequent usage of instruments that need a firm grip
Direct Injury: A direct blow, trauma, or injury to the wrist or base of the thumb can also trigger the inflammatory process in the tendon sheath.
Fluid Retention: For women, increased fluid retention during pregnancy or hormonal changes can cause swelling that compresses the tendon sheath.
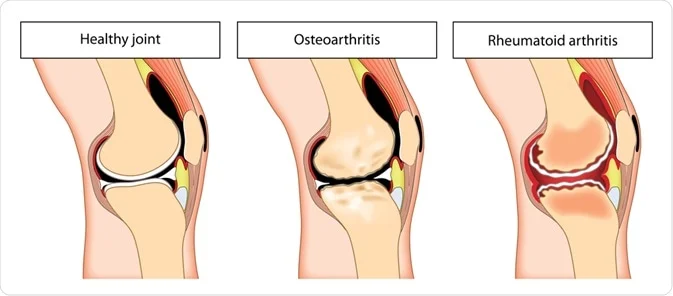
Arthritis: In some cases, rheumatoid arthritis or other types of arthritis may contribute to tendon inflammation.
Anatomical Factors: Occasionally, an anatomical abnormality like a small tumor, cyst, or irregularity in the wrist bones or musculature can affect the tendons and tendon sheath.
While overuse is the most common underlying cause, an exact inciting event or repetitive motion is not always identified. The condition can sometimes occur spontaneously without any obvious trigger.
Proper diagnosis of any potential causes, as well as the location and extent of inflammation, is important to determine the best course of treatment.
Clinically Relevant Anatomy
De Quervain’s tenosynovitis affects two key tendons in the wrist and thumb area – the extensor pollicis brevis (EPB) and the abductor pollicis longus (APL).
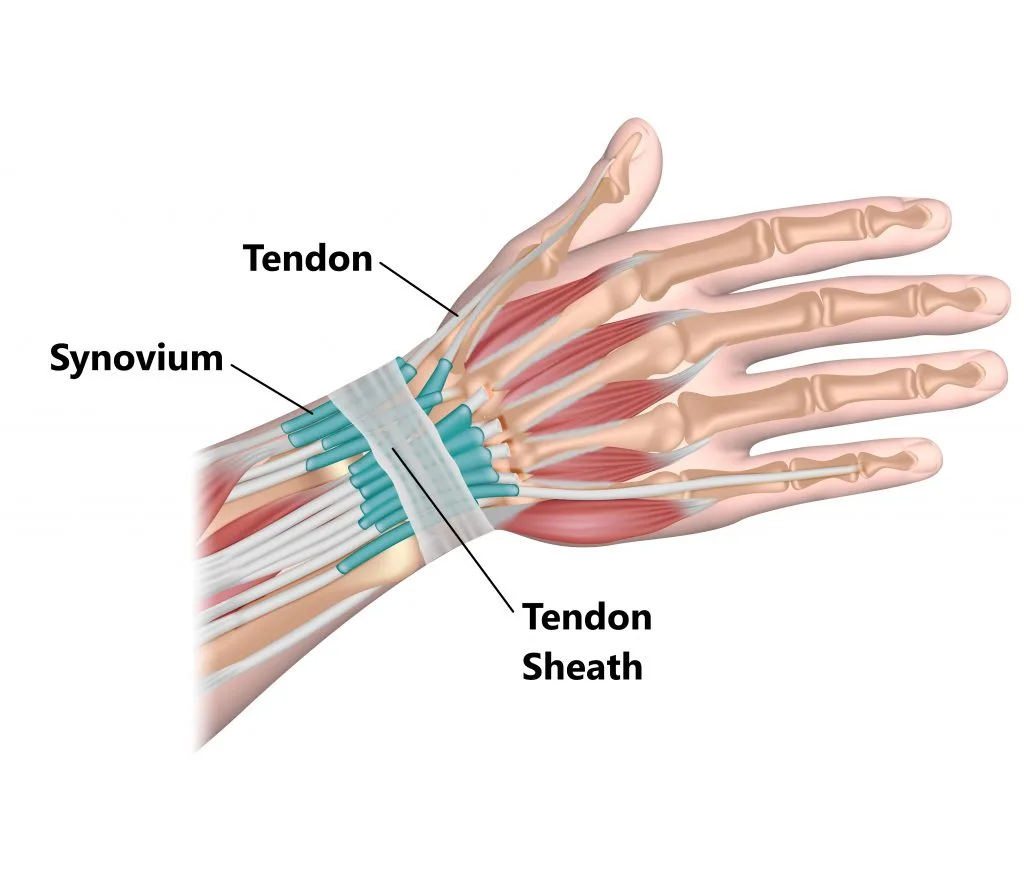
Extensor Pollicis Brevis (EPB)
- Originates from the dorsal side of the radius and interosseous membrane in the forearm
- Inserts at the base of the thumb’s
- Functions to extend the thumb and radially abduct the wrist
- Innervated by the radial nerve’s posterior interosseous branch
- Blood supply from the posterior interosseous artery
Abductor Pollicis Longus (APL)
- Originates from the dorsal sides of the radius, ulna, and interosseous membrane
- Attaches itself to the first metacarpal bone’s base.
- Functions to abduct the thumb and radially abduct the wrist
- Also innervated by the posterior interosseous branch of the radial nerve
- Blood supply from the posterior interosseous artery
Both the EPB and APL tendons travel through a fibro-osseous tunnel formed by the radius styloid process and the extensor retinaculum at the wrist as they course toward their thumb insertions.
In De Quervain’s tenosynovitis, this compartment containing the two tendons becomes inflamed and stenotic, limiting the gliding motion of the tendons. This leads to pain, swelling, and difficulty abducting or extending the thumb.
Proper functioning of the EPB and APL tendons is critical for normal thumb movements required for gripping, grasping, and pinching activities. Understanding this anatomical region is key for diagnosing and treating De Quervain’s tenosynovitis.
Epidemiology
De Quervain’s tenosynovitis is a relatively common condition, especially among certain demographic groups. Several studies have estimated its prevalence:
Overall Prevalence:
- One study found a prevalence of 0.5% in men and 1.3% in women
- Another study determined a 0.36% prevalence in women and 0.13% in men
Peak Age:
- The condition tends to peak in prevalence among individuals in their 40s and 50s
Gender Differences:
- De Quervain’s occurs more frequently in women compared to men across multiple studies
Risk Populations:
- Those with a prior history of medial or lateral epicondylitis (tennis/golfer’s elbow) may have an increased risk
- New mothers and childcare providers are a classic risk group due to repetitive wrist motions when lifting children
- Bilateral cases are common, often resolving when child-lifting becomes less frequent
Risk Factors:
- Pregnancy is considered a significant risk factor, likely due to fluid retention
- Manual labor and occupations involving repetitive hand motions are another major risk factor
While not prevalent in the general population, De Quervain’s can be more common among certain age groups, genders, and occupations that predispose the wrist tendons to overuse injuries. Early recognition in high-risk groups is important.
Pathophysiology
The first dorsal compartment of the wrist, containing the synovial sheath-lined abductor pollicis longus and extensor pollicis brevis tendons, is affected by De Quervain’s tenosynovitis.
The first dorsal compartment is separated from the other five dorsal wrist compartments by the extensor retinaculum. Under this circumstance, the two tendons cross the radial styloid process and go beneath the extensor retinaculum’s transverse fibers, passing through a roughly 2-centimeter fibrous tunnel.
This anatomical region puts the tendons at risk for entrapment, particularly with acute trauma or repetitive motion causing inflammation and swelling.
The pathologic process begins with the thickening of the tendon sheath in the first compartment due to increased mechanical stress and irritation. This leads to a “stenosing” (narrowing) tenosynovitis as the sheath thickens and the compartment shrinks around the tendons.
Several key changes occur:
- Formation of fibrocartilage within the tendon sheaths in response to increased stress
- Thickening of the tendon sheaths
- Neovascularization (new blood vessel formation) in the affected sheaths
- Myxoid degeneration within the tendons themselves
Additionally, a septum (dividing wall) is often present between the two tendons in the first compartment. This further reduces the compartment volume and complicates both non-operative and surgical treatment approaches.
The narrowing of the first dorsal compartment due to the sheath thickening and potential septum entrap restricts the gliding motion of the APL and EPB tendons. With wrist and thumb motions, this results in pain, edema, and restricted thumb mobility.
Risk Factors
While overuse is the main underlying cause, certain groups are at higher risk of developing De Quervain’s:
- Women and those assigned female at birth
- People over the age of 40
- Childcare workers
- Parents of young children
- Manual laborers and those with hand-intensive jobs
- Athletes, especially those playing racquet sports
The increased risk is likely due to a combination of anatomical factors, hormonal influences, and the repetitive wrist/thumb motions required in childcare, manual labor, and many athletic activities.
Early recognition of risk factors and modifying aggravating activities are important for the prevention and treatment of this common condition.
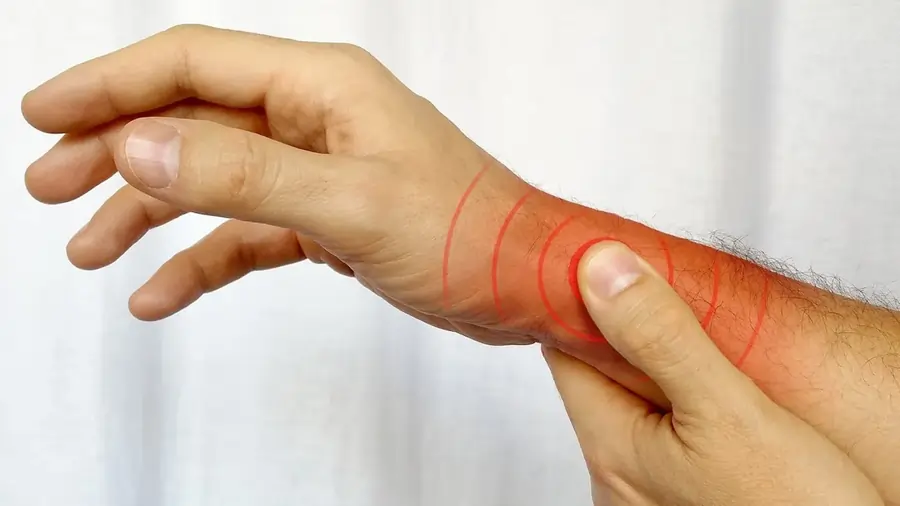
Symptoms of De Quervain’s Tenosynovitis
- Pain near the base of the thumb
- Swelling around the base of the thumb
- Having trouble extending the thumb and wrist to squeeze or grip
- A “sticking” or “catching” sensation in the thumb with movement
- In extreme situations, the pain might radiate farther into the forearm or thumb.
As the condition progresses without treatment, thumb and wrist mobility becomes more limited and painful.
Diagnosis
Examination
History:
- Report of wrist/thumb pain, either from overuse/repetitive motions or acute trauma
- Description of radiating pain up the forearm with grasping/thumb extension
- Pain aggravated by lifting, gripping, twisting motions
- Note if pregnant/postpartum, hand dominance, occupation/activities
Physical Exam Findings:
- Tenderness over the base of the thumb and first dorsal compartment near the radial styloid
- Swelling in the anatomical snuffbox area
- Decreased range of motion in thumb carpometacarpal abduction
- Potential thickening of extensor tendon sheaths and crepitus with gliding
- Weakness or paresthesia in the hand
Special Tests:
- Finkelstein test is commonly positive
- The patient makes a fist over the thumb, then the ulnar deviates from the wrist
- Reproduces sharp pain over the first dorsal compartment
Additional tests are often performed to confirm the diagnosis and rule out other conditions.
Diagnostic Tests
- Radiographs (x-rays) to evaluate for anatomic abnormalities or other causes
- Ultrasound or MRI may show tendon sheath thickening and inflammation
The group of symptoms, physical exam findings, and positive special tests in the appropriate clinical context can reliably diagnose De Quervain’s tenosynovitis. Imaging is sometimes used to confirm the diagnosis or investigate other potential pathologies.
Differential Diagnosis
Conditions that can imitate or present similarly to De Quervain’s include:
- Osteoarthritis of the first carpometacarpal (CMC) joint
- Scaphoid fracture
- Radial styloid fracture
- Sensory branch of radial nerve neuritis (Wartenberg’s syndrome)
- Intersection syndrome
- Trigger thumb
- Other forms of tendinitis like intersection syndrome
A careful history, physical exam, and potential imaging are required to differentiate De Quervain’s from these alternative diagnoses.
Treatment of De Quervain’s Tenosynovitis
De Querv’s treatment options are typically divided into three:
- Tier 1: Non-invasive approaches such as splinting, Physical Therapy- ultrasound, multimodal hand therapy, and modifying activities.
- Tier 2: Using corticosteroid injections.
- Tier 3: Surgical intervention.
Combining Tiers 1 and 2 may be considered based on the patient’s condition and their consent to receive corticosteroid injections.
Medical Treatment
A healthcare provider will typically recommend treatments for de Quervain’s tenosynovitis that address your symptoms while promoting healing in your thumb tendons and sheaths. Common treatments may include the following:
- Utilizing a splint or brace: This device will stabilize your wrist and thumb, reducing pressure on the affected tendons.
- Applying ice to your wrist: Using ice packs wrapped in a thin towel can help decrease swelling and alleviate pain. Apply them to your wrist for 20-minute intervals multiple times a day.
- Resting: It is advisable to minimize the use of your affected wrist. Avoid engaging in sports or repetitive activities, especially those that triggered de Quervain’s tenosynovitis.
- Taking NSAIDs: Non-prescription NSAIDs can lessen inflammation and pain. However, do not exceed 10 consecutive days of NSAID use without consulting your healthcare provider.
The main of non-surgical is to lessen pain and reduce swelling. Strategies may involve:
- Educating patients about avoiding repetitive or aggravating movements
- Using non-steroidal anti-inflammatory drugs (NSAIDs)
- Applying ice/heat packs
- Engaging in physical therapy
- Participating in occupational therapy
- Wearing a thumb splint
De Quervain’s Splint
Research backs the use of a forearm brace that includes the thumb to minimize ulnar deviation and thumb motion. There is a difference among healthcare providers on how often and for how long the splint should be worn; some suggest continuous wearing for four to six weeks, while others recommend using it only as necessary for pain relief.
Studies have shown a 19% improvement with splint use, but coupling it with NSAIDs resulted in a 57% enhancement. Combining an orthosis with corticosteroid injections has shown greater efficacy than either treatment alone for de Quervain’s condition.
Ultrasound for Treatment
- Therapeutic ultrasound: Can effectively manage pain, although findings from studies are varied and may have limited sample sizes and outcome measures.
- Ultrasound-guided injections: Have been found beneficial for De Quervain’s tenosynovitis, outperforming previous reports, and showing no adverse effects.
- Ultrasound-guided injections targeting specific areas have been more effective than manual injections.
Corticosteroids Injections
Corticosteroid injections have proven to be effective, typically requiring one or two injections for pain relief. If symptoms do not significantly improve after two injections, surgical intervention may be considered, often in an outpatient setting and using local, regional, or general anesthesia.
Patients with moderate to severe symptoms usually need a combination of cortisone injections and splinting.
Exercises for De Quervain’s Tenosynovitis
Your healthcare provider might recommend various stretches and exercises to enhance the strength and flexibility of your wrist if you have De Quervain’s tenosynovitis. One common exercise involves lightly squeezing a tennis ball:
- Gently hold a tennis ball for a few minutes.
- Take a short break.
- If you don’t experience any pain, repeat the squeezing motion with slightly more pressure.
The Advantages of Exercise for People with de Quervain’s Tenosynovitis
Exercise plays a crucial role in the comprehensive treatment approach for de Quervain’s tenosynovitis, often in conjunction with other therapies such as anti-inflammatory medications, cortisone injections for pain relief, splinting, and modifications in daily activities. Physical or occupational therapy is usually started early in the course of treatment.
Throughout the rehabilitation process, your therapist will instruct you on specific methods aimed at enhancing the mobility of the affected tendons in your thumb, namely the abductor pollicis longus and extensor pollicis brevis. Initially, pain-free exercises focusing on the thumb and wrist range of motion are performed to enhance tendon movement within the sheaths. Subsequently, strengthening exercises may be incorporated to facilitate a return to your usual activities.
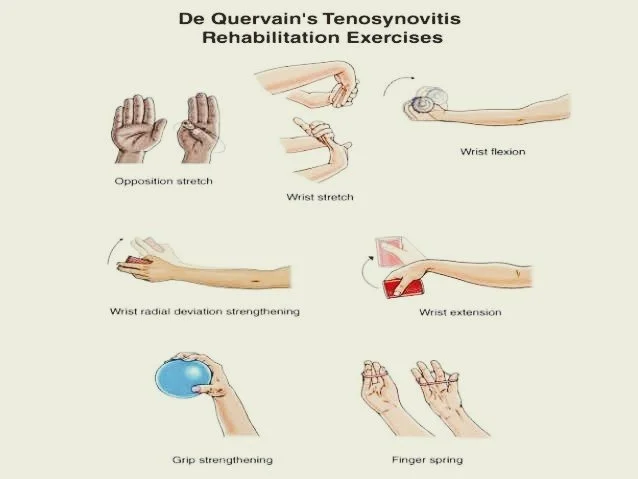
Common Exercises for a Particular Diagnosis
- Thumb Opposition Stretch: Pointing your palm toward a table. Slowly move your thumb across your hand towards your pinkie finger. Hold this position for six seconds once they touch. Repeat 10 times daily.
- Wrist Extension Stretch: With your arm straight and palm down, stretch your arm in front of you. Use your other hand to pull the affected hand’s palm upward until you feel a stretch. Hold for 15–30 seconds, repeating two to three times daily.
- Wrist Flexion Stretch: Keep your arms in the same posture as you did during the wrist extension stretch, but push your hand’s top down. Hold for 15–30 seconds, performing this stretch two to three times daily.
- Strengthening Wrist Radial Deviation: With your thumb pointed upward, hold a lightweight and hang your hand off a table. Raise and lower your wrist without raising your forearm. Every day, perform two sets of fifteen reps.
- Strengthening Wrist Extension: Hold one end of a resistance band and hang your wrist off a table, palm down. As the tension in the band grows, raise your wrist. Perform three sets of fifteen repetitions each day.
- Wrist Flexion Strengthening: Holding a secured resistance band, raise your hand towards the ceiling with the palm facing up. Repeat the exercise 15 times, completing two sets each day.
- Grip Strengthening: Squeeze a squishy ball or putty tightly, holding for five seconds. Perform two sets of 15 repetitions daily.
- Finger Spring: Wrap a rubber band around your thumb and fingers, spreading them as wide as you can. Hold for one or two seconds, and repeat this 15 times, twice daily.
- Thumb Lifts: Rest your hand on a table and lift your thumb in an arc motion away from it. Hold for six seconds, repeating eight to 12 times.
- Thumb Flexion: Use the thumb lift position and gently push the thumb down towards the palm with your other hand. Hold for 15–30 seconds, completing two to four repetitions daily.
- Finkelstein Stretch: Make a fist around the affected thumb and extend your arm, palm inward. Use the other hand to push down on the fist, holding for 15–30 seconds. Repeat two to four times daily.
Surgical Treatment
Most individuals do not have surgery as a treatment for de Querv’s tenosynovitis. However, surgical intervention may be suggested if other remedies do not alleviate the symptoms, especially in more severe cases.
The outpatient surgery involves examining the sheath surrounding the affected tendon or tendons and then opening the sheath to relieve pressure, allowing the tendons to move smoothly.
Following surgery, your healthcare provider will advise you on resting, strengthening, and rehabilitating your body. A physical therapist or occupational therapist may guide new strengthening exercises and help you adjust your daily routine to prevent future issues.
Rehabilitation Management
Using Ice/Heat Packs
Applying heat can assist in relaxing and loosening tight muscles, while ice can help reduce inflammation of the sheath surrounding the muscles.
Strengthening
The exercise regimen should be progressed in the following order:
- Isometric
- Eccentric
- Concentric inner range
- Therapeutic
- Radial nerve glides
Patients can begin strengthening exercises once their pain has reduced to a painless level. The strengthening program should be carefully structured and incremental. Progression through the strengthening program should only occur if patients can endure their current routine for at least a week. It is crucial to advance gradually and ensure that patients strengthen within a pain-free range of motion to prevent exacerbation of symptoms.
Examples of strengthening exercises.
Mobilization
Utilizing movement in therapy has proven effective in reducing pain, enhancing range of motion, and improving the functionality of patients with De Quervain’s tenosynovitis. The patient was advised to do radial abduction-adduction with the thumb after the therapist performed a manual radial glide on the proximal row of carpals.
This mobilization therapy, done in 3 sets of 10 repetitions, followed by eccentric hammer curl exercises using a theraband and high voltage electrical stimulation, demonstrated effectiveness upon a 6-month follow-up.
Studies by Savva et al. have investigated the pain-relieving benefits of joint mobilization in tendinopathy, highlighting the limited data available emphasizing the effectiveness of these techniques in tendinopathies like De Quervain’s, which have only been vaguely reported in a few retrospective case studies.
Taping
Taping is another method that can be employed to alleviate pain and enhance functionality.
Ultrasound
Therapeutic ultrasound has been associated with improved results in pain management and healing processes.
Prognosis
The prognosis for De Quervain’s tenosynovitis is generally very good with proper treatment:
- Most cases are resolved with conservative non-operative management like splinting, injections, activity modification
- Even cases that fail conservative treatment typically improve with surgical release of the first dorsal compartment
- Risk factors for failing non-operative treatment include female sex, hypothyroidism, presence of a compartment septum, psychiatric illness
With timely diagnosis and appropriate treatment, the vast majority of patients achieve complete resolution of symptoms.
Complications
While uncommon, potential complications can occur with both non-operative and surgical management:
Non-operative:
- Skin depigmentation or fat atrophy from corticosteroid injections
Surgical:
- Injury to the superficial radial nerve
- Entrapment or subluxation of the APL/EPB tendons after compartment release
- Scarring and stiffness with delayed recovery
Overall, De Quervain’s tenosynovitis has a favorable outlook when properly identified and managed according to guidelines. Complications are infrequent when treated by an experienced professional.
When to See a Doctor
You should consult a doctor if you experience persistent symptoms of De Quervain’s tenosynovitis that do not improve with initial self-care measures, such as:
- Resting and avoiding use of the affected thumb/wrist
- Applying cold packs to the painful area
- Using over-the-counter pain relievers such as naproxen or ibuprofen
Seek medical evaluation if the pain and dysfunction continue despite taking these conservative steps for a week or two. Early examination can confirm the diagnosis and determine if further treatment is required.
Additionally, seek prompt medical care if:
- The pain becomes severe and unrelenting
- Hand/thumb motions become significantly restricted
- Symptoms do not start improving within a few weeks of self-care
Lifestyle modifications and Home remedies
Lifestyle Modifications:
- Avoid repetitive wrist/thumb motions that aggravate symptoms
- Take breaks from aggravating activities to allow the tendons to rest
- Modify activities/techniques to reduce strain on the affected area
Home Care:
- Wear a thumb spica splint or brace to immobilize and rest the tendons, especially at night
- Apply ice packs to the base of the thumb for 15-20 minutes several times per day to reduce inflammation
- Perform gentle range-of-motion and tendon gliding exercises as tolerated and prescribed
- Utilize assistive devices (key turners, jar openers) for gripping tasks
Other Remedies:
- Take over-the-counter anti-inflammatory medication (NSAIDs) to reduce pain and swelling
- Try alternating heat and cold therapy
- Consider trying nighttime wrist braces or splints in addition to thumb immobilization
- Identify and avoid any activities that consistently cause increased pain, swelling, or numbness
The key is resting and immobilizing the inflamed tendons while avoiding re-aggravation. Simple home treatments combined with activity modification can help resolve milder cases. See a doctor if symptoms persist despite these conservative remedies.
Prevention Strategies
- Learn and use proper technique for sports, work tasks, and physical activities involving the wrists/thumbs
- Wear proper protective equipment like braces or splints if recommended
- Gradually ease into new exercises or activities to allow the tendons to adapt
- Take frequent breaks from repetitive hand motions or gripping tasks
- Avoid pushing through wrist/thumb pain during activities – this can worsen injury
- Allow time for rest and recovery after intense hand/wrist use
- Consider using ergonomic tools/equipment to reduce strain on the hands
Summary
De Quervain’s tenosynovitis is a painful condition affecting the tendons that control thumb movement. It involves inflammation and swelling of the tendon sheath surrounding the abductor pollicis longus and extensor pollicis brevis tendons as they pass through a tunnel at the base of the thumb.
The most common cause is repetitive hand/wrist motions from occupations or activities requiring frequent gripping, grasping, or twisting. New mothers are a classic risk group due to repetitive wrist motions when lifting babies. The condition leads to pain, swelling, and difficulty moving the thumb, particularly with grasping.
Diagnosis is made through the clinical presentation of tenderness at the base of the thumb, a positive Finkelstein test, and limited thumb mobility. Imaging like ultrasound may aid in visualizing tendon sheath thickening.
Initial treatment is conservative, focusing on immobilizing the thumb, oral anti-inflammatories, and modifying aggravating activities. Splinting and steroid injections into the tendon sheath are commonly utilized. If symptoms persist after several weeks/months of conservative care, surgery to release the thickened tendon sheath may be recommended.
FAQs
What is De Quervain’s tenosynovitis?
De Quervain’s tenosynovitis is a condition where the tendons around the base of the thumb become inflamed and swollen, making thumb movement painful.
What causes De Quervain’s?
It is most commonly caused by repetitive hand/wrist motions from activities like gardening, playing sports, lifting children, or jobs requiring frequent gripping.
What are the symptoms?
The main symptoms include pain and swelling at the base of the thumb, difficulty moving the thumb, and a “catching” sensation with thumb motions.
How is it diagnosed?
Diagnosis is made through a physical exam checking for tenderness, swelling, and limited motion, and by performing the Finkelstein test. Imaging like ultrasound may be used.
What is the Finkelstein test?
The patient makes a fist over the thumb and then ulnarly deviates the wrist. Reproducing pain at the base of the thumb indicates a positive test.
How is De Quervain treated?
Initial treatment involves immobilizing the thumb with a splint, oral anti-inflammatories, activity modification, and sometimes steroid injections. Surgery may be needed for persistent cases.
Can De Quervain’s be prevented?
Using proper techniques, taking breaks from repetitive activities, wearing braces during risky activities, and allowing rest can help prevent it.
What is the recovery time?
Most cases resolve within 4-6 weeks of conservative treatment, but severe or chronic cases can take several months to fully recover from, even after surgery.
References
- Satteson, E., & Tannan, S. C. (2023, November 22). De Quervain Tenosynovitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK442005/
- De Quervain’s Tenosynovitis. (n.d.). Physiopedia. https://www.physio-pedia.com/De_Quervain%27s_Tenosynovitis
- Professional, C. C. M. (n.d.). De Quervain’s Tendinosis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/10915-de-quervains-tendinosis#living-with
- de Quervain’s Tenosynovitis: Causes & Treatment – familydoctor.org. (2024, January 3). familydoctor.org. https://familydoctor.org/condition/de-quervains-tenosynovitis/
- De Quervain tenosynovitis – Diagnosis and treatment – Mayo Clinic. (2022, August 4). https://www.mayoclinic.org/diseases-conditions/de-quervain-tenosynovitis/diagnosis-treatment/drc-20371337
- De Quervain’s Tenosynovitis Symptoms and Treatment – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/de-quervains-tendinosis/
- Ocs, T. P. D. (2022, February 17). 11 Exercises to Reduce de Quervain’s Tenosynovitis. Verywell Health. https://www.verywellhealth.com/de-quervains-tenosynovitis-exercises-5217358




One Comment