Olecranon Bursitis
What is Olecranon Bursitis?
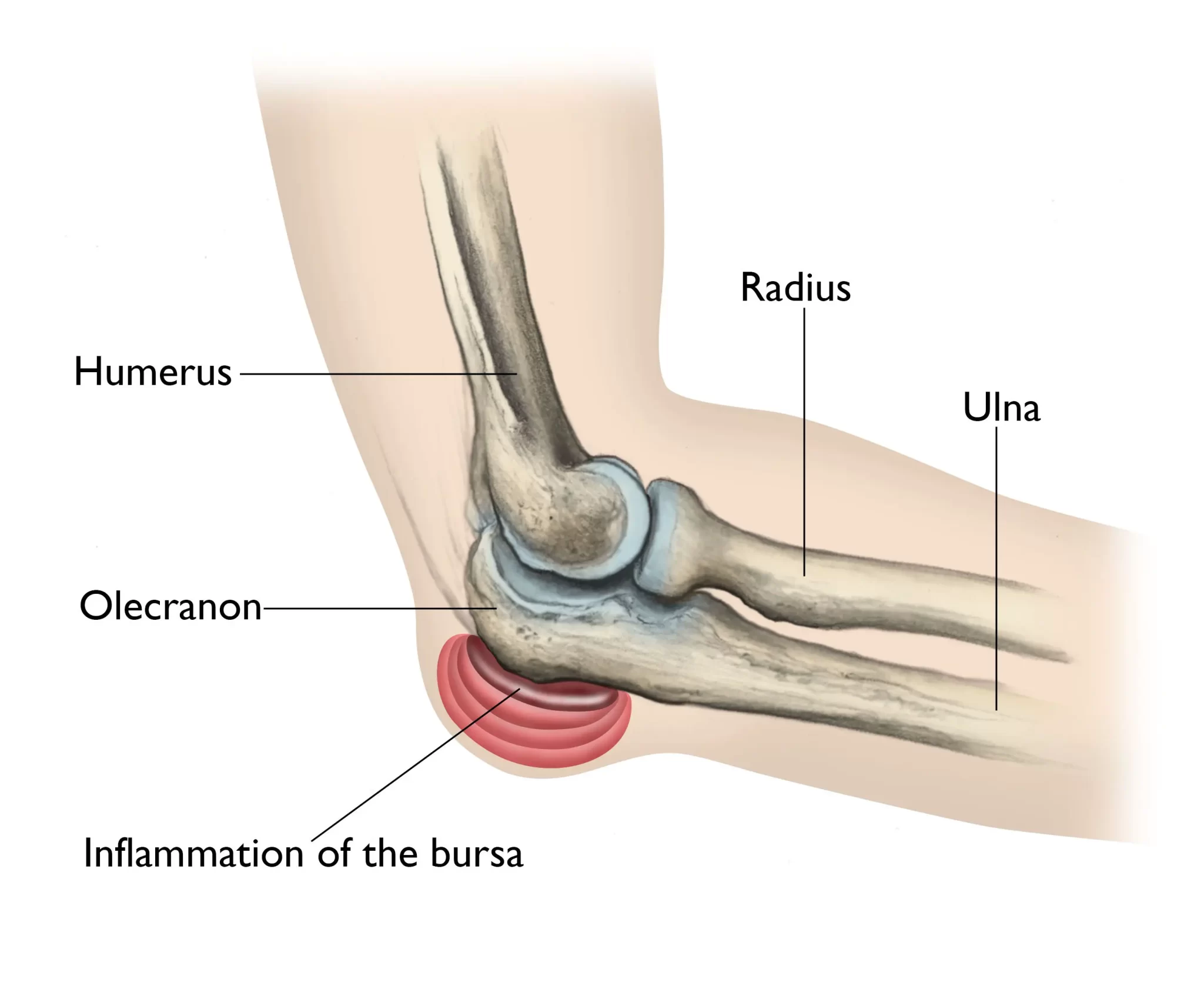
The olecranon bursa, a small pouch filled with fluid at the end of the elbow, becomes inflamed when an individual has olecranon bursitis. The elbow joint can move smoothly because of the olecranon bursa, which serves as a cushion between the skin and the bony prominence of the ulna. Olecranon bursitis can result from this bursa becoming inflamed or irritated, usually as a result of trauma, infection, or repeated friction.
The synovial membrane known as the olecranon bursa is situated just behind the elbow’s olecranon bone. The bursa’s job is to facilitate the bony olecranon’s seamless transition between flexion and extension of the elbow over the surrounding tissues. The term “olecranon bursitis” describes bursa inflammation.
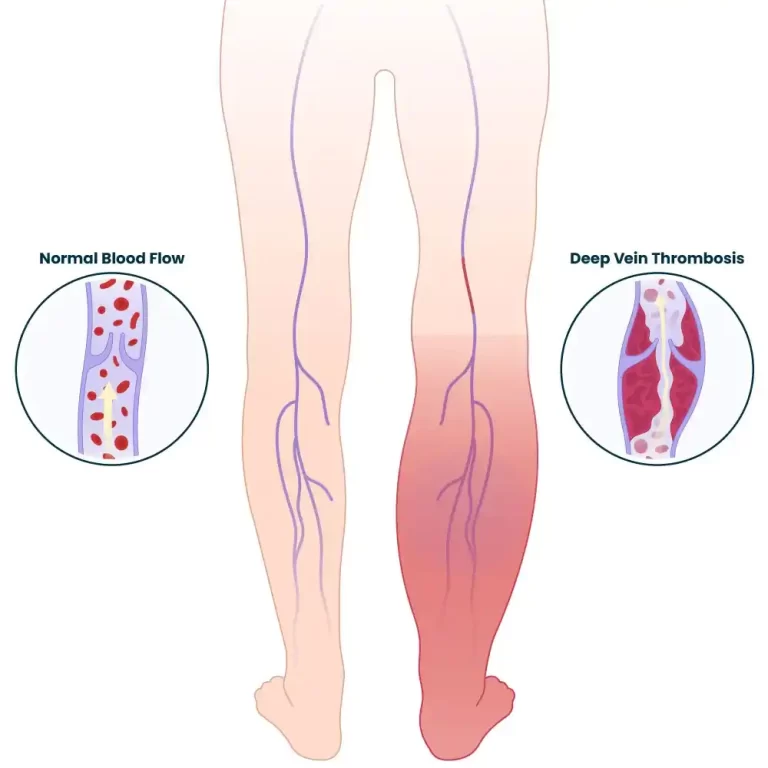
The bursa is vulnerable to damage and infection due to its shallow placement and restricted vascularity. Without the assistance of reliable diagnostic tests, the diagnosis of olecranon bursitis is frequently determined solely only on clinical examination. But when you include the possibility of a different diagnosis or the existence of an illness, diagnostic testing becomes crucial.
Olecranon bursitis commonly manifests as back swelling, soreness, and elbow pain. Occasionally, the skin above the inflammatory area may become hot and red. While olecranon bursitis is often caused by small injuries or overuse, infectious bursitis can potentially be caused by bacteria entering the bursa.
The treatment plan for olecranon bursitis is based on its underlying cause. Non-infectious cases can be treated with anti-inflammatory medications and the rest, ice, compression, and elevation (RICE) protocol. Infectious bursitis may require the use of antibiotics. In more severe or persistent cases, aspiration of fluid from the bursa or other medical procedures might be investigated.
It’s imperative to consult a healthcare professional for a precise diagnosis and customized treatment plan. Appropriate and prompt therapy can help prevent issues and lessen symptoms.
What is a Bursa?
A bursa is a small pouch that holds a tiny volume of liquid. The fluid resembles synovial fluid, which is found in joints. The body contains a number of bursae, one of which is located directly above the olecranon. Bursae facilitate smooth transitions between “stick-out” bones and the skin above them.
The pointy bone at the end of the elbow is called the olecranon (oh-LEH-cruh-nahn). A bursa is a little fluid-filled sac that lies between the skin and its bony point. It facilitates the skin’s easy glide over the bone. In its normal state, this sac lies flat and contains very little fluid.
The term “olecranon” describes the spitzen bone in your elbow. The term “bursitis” describes inflammation of a bursa, a component of your body.
The bursa is normally imperceptible, but when it becomes inflamed, it enlarges and becomes noticeable, causing a soft lump to form over the back of your elbow. Though it can have many forms and sizes, it is sometimes said to have the shape of a goose egg. Bursitis is also frequently seen in the joints close to your:
- hip
- shoulder
- Knee
Olecranon bursitis is sometimes referred to as Popeye’s elbow, Baker’s elbow, Elbow bursitis, and student’s elbow.
Olecranon Bursa Anatomy
Situated between the skin, the bony tip of the elbow, and the olecranon process is a small sac filled with fluid called the olecranon bursa. It serves as a cushion and lessens the force exerted by the skin and bone.
The bursa’s roof is in contact with the surrounding subcutaneous tissue, while the bursa’s floor is supported by the olecranon and triceps brachii tendon. It is a sac lined with synovium that usually contains very little fluid and a thin wall.
Development
This bursa, which develops between the ages of 7 and 10, serves to allow mobility without friction when the elbow is flexed due to the deep attachment of the olecranon process and triceps brachii tendon.
Epidemiology
Olecranon bursitis occurs somewhat frequently. There is no connection between this condition and death. Posterior elbow pain can cause morbidity and limit one’s activities. Usually, men in their 30s to 60s are impacted.
- In two-thirds of nonseptic cases, sports injuries or repeated trauma cause bursa bleeding or the release of inflammatory mediators.
- Neither a sexual nor racial inclination exists.
- Children and adults can both suffer from olecranon bursitis.
- Prolonged hemodialysis treatment, uremia, or a mechanical component can all contribute to inflammation.
- Technicians who crawl on their knees and rely on their elbows in cramped spaces are particularly at risk.
Inflammation can also be caused by a systemic inflammatory disease like rheumatoid arthritis or a crystal deposition condition like gout or pseudogout. This condition can occur as a side effect of sunitinib, a drug used to treat renal cell cancer.
Pathophysiology
Reactive inflammation occurs in the bursa in reaction to the triggering event, which might be the introduction of an infectious pathogen or trauma. The inflammatory process causes extravasation of protein and synovial fluid into the bursa. The outcome is the recognizable circular swelling associated with the condition.
Types of olecranon buesitis
Olecranon bursitis comes in two varieties:
- Septic or infected
- Not infected (aseptic)
Causes of Olecranon Bursitis:
Olecranon bursitis typically develops as a result of an infection, underlying inflammatory disease, or trauma. An injury may cause internal bleeding in the bursa and produce inflammatory mediators that increase the risk of recurrence.
It may also be linked to long-term health issues like diabetes, alcoholism, or HIV, as well as inflammatory diseases including gout, psoriatic arthritis, and rheumatoid arthritis. It is believed that infection occurs transcutaneously rather than hematogenous because of the low vascularity. Since infection is typically the result of moderate trauma or direct inoculation, it typically involves the normal skin flora.
Football, hockey, basketball, and volleyball players have frequently been reported to have olecranon bursitis as a result of trauma, such as elbow strikes or falls on the back of the elbow.
The majority of patients experience the condition as a result of frequent elbow flexion-extension motions that irritate the bursa. For instance, weightlifters or athletes who play sports where throwing requires raising the arm above the head, like baseball or cricket players who throw javelins.
Over time, people who repeatedly rest their elbows on hard surfaces may experience this issue. Those who work with their elbows frequently, such as air conditioning and plumbing technicians, are more susceptible to this. It is known as “student’s elbow” when it affects persons who lean on their elbows on a desk to study. When a job requires a lot of crawling with elbows, other terms for it include “plumber’s elbow,” “miner’s elbow,” etc.
This condition can be more common in people with rheumatoid arthritis, gout, or kidney failure requiring dialysis.
Infection: A cut, scrape, or insect bite can infect your bursa, causing the sac to swell, fill with excess fluid, and turn red.
Idiopathic: The cause is frequently unknown.
Signs and Symptoms
- stiffness in the elbows
- Tenderness: Sensitivity in the elbow region and achy sensation with pressure or movement are further indicators.
- It’s possible that gradual elbow swelling goes unnoticed at first. Sometimes, the swelling appears suddenly.
- The most common symptom of bursal inflammation is swelling near the back of the elbow. This swelling above the olecranon process looks like a goose egg, which makes it easy to identify. The swelling at the elbow tip may get so bad that it resembles a soft golf ball.
- When olecranon bursitis occurs, pain is typically not experienced.
- An infection of the bursa may result in warmth, redness, or pain in the affected region, along with a possible fever.
- Since the joint capsule is not affected, range of motion is often maintained with little pain, unless the movement is at its most extreme.
- Pus may leak out of an infected bursa by breaking open.
- Make careful to check the joints above and below the elbow, as well as the contralateral elbow joint.
Differential Diagnosis
- Rheumatoid arthritis
- Forearm and elbow overuse injuries
- Pseudogout and gout
- fractures of the olecranon
- Avulsion of the triceps tendon
- The cellulitis
- Septic arthritis Ruptures in the ligaments
- Neoplasm
- hematoma
Diagnosis
In individuals who have experienced elbow bursitis repeatedly, your doctor may perform an x-ray to check for a fractured bone, bone spur, or calcium deposit at the elbow in order to identify olecranon bursitis.
A needle may be used to extract some fluid from the bursa and send it for analysis. There is an infection in the bursa if pus is the fluid within. When uncertainty persists following a clinical examination, laboratory testing is necessary to distinguish between septic and non-septic bursitis; hence, the aspirate should be submitted for microscopy and culture.
Generally, blood tests are not useful. Until culture results are obtained, therapy for a suspected septic case should be administered if the diagnosis is unclear.
History and Physical Examination:
Swelling that covers the olecranon process is the first sign of olecranon bursitis. As the edema increases, elbow mobility may become limited. Elbow mobility is unrestricted in the early stages, which sets it apart from elbow joint edema. Bursitis is characterized by a rounded or “golf ball”-shaped appearance due to the fluid’s confinement within the bursa.
When an underlying infection is the cause of bursitis, erythema, and pain are typically present. Additionally, it may be linked to systemic symptoms including fever and malaise. It should be highlighted that only around 70% of cases of septic bursitis have a fever; as a result, in cases when a patient has a fever, an infectious cause may not always be definitively ruled out.
Assessment:
The diagnosis is often made by a skilled medical professional using only the physical examination and history. It is critical to take the possibility of septic bursitis into account while diagnosing. Without objective diagnostic testing, the average physician is unable to accurately distinguish between mildly infected bursitis and non-infectious bursa due to the presence of both overlapping and variable signs and symptoms. Therefore, one must weigh the advantages and disadvantages of the minimally invasive bursa aspiration procedure needed for conclusive testing.
The gold standard for diagnosis is thought to be bursal aspiration and analysis. This is especially crucial when thinking about an underlying infection. Fluid should be submitted for a cell count, Gram stain, culture, sensitivity tests, and crystal inspection when assessing to rule out infection.
Additionally, there has been some opinion that in septic cases, changes in serum/bursal fluid glucose concentrations are noticeably more substantial. This hasn’t been confirmed, yet. In addition to closely examining vital signs to rule out systemic sepsis, a practitioner investigating septic bursitis must also consider reviewing serum lab tests when appropriate.
Treatment of Olecranon Bursitis:
With basic treatment, including resting the elbow, minimizing pressure, and using ice packs, olecranon bursitis often resolves on its own. Certain individuals discover that applying a compression bandage to their elbow enhances comfort. Most occurrences of olecranon bursitis eventually resolve on their own, provided there is no infection.
Whether bursitis is infectious or not has a significant impact on how it is treated. Acute noninfectious bursitis resolves on its own. Conservative treatment options include rest, ice, and NSAID usage. It has also been demonstrated that using elastic bandages can aid in preventing edema. Corticosteroid injections may be able to reduce olecranon bursitis symptoms early, according to certain studies; nevertheless, there is a 10% chance of iatrogenic infection with this therapy.
At eight weeks, up to 25% of patients treated with aspiration may still have edema or recurrence, and at six months, up to 10% may still experience persistent symptoms. When an event occurs repeatedly, bursectomy may be an option. An underlying bone spur indicates a higher chance of recurrent episodes. Therefore, surgical removal of the problematic spur should be considered for patients with a known spur and many recurrences. Surgical excision of the bursa may be beneficial in cases of persistently reoccurring bursitis without the presence of a spur.
Antibiotics are necessary for the treatment of infectious bursitis, especially those that target streptococcal and staphylococcal bacteria. It is strongly advised to aspirate and drain, being sure to disturb any existing locations. Antibiotics used orally are enough, and there is no evidence of any benefit from intravenous (IV) doses. There is no proof that prolonged durations of therapy reduce recurrence, thus a 7-day prescription of oral antibiotics is sufficient.
Patients who experience recurring infections or who do not improve clinically after trying alternative therapies may be candidates for a bursectomy. More assessment of severe sepsis or septic shock with the current suitable therapy for either condition should be considered evidence of systemic infection.
Medical Treatment
In certain situations, additional therapies suggested are:
Anti-inflammatory drugs (such as diclofenac, ibuprofen, naproxen, etc.) could be administered to treat swelling and inflammation. Another choice if the elbow hurts is paracetamol.
If a lot of fluid accumulates, a medical practitioner can drain the fluid (aspiration) using a sterile needle and syringe. But after the fluid is emptied, it usually starts to accumulate again. In order to keep the fluid from re-accumulating, you might be instructed to wear a tight-pressure bandage for a period after it has been drained.
A bursa steroid injection might solve the issue. It is effective for steroids to lower inflammation. Nevertheless, bursa infections can occasionally result after steroid injections.
If none of the foregoing remedies work, surgery to remove the bursa may be necessary.
In the event that an infection is the bursitis’s etiology, antibiotics are required. Typically, an antibiotic, like erythromycin or flucloxacillin, is administered while waiting for the aspirated fluid test results. The treatment plan can then be modified as needed to target the specific bacteria (germs) causing the infection. The most prevalent kinds of bacteria that cause olecranon bursitis are treated with erythromycin and flucloxacillin.
Surgical Treatment
Treatment for an Infected Bursa
Surgery to remove the whole bursa may be required if the infection does not resolve with medications or by draining fluid from the elbow. Since this is frequently an inpatient operation, you will have to spend the night in the medical facility. This procedure can be combined with further intravenous or oral antibiotic use.
Usually, the bursa regenerates over many months as a typically functioning, non-inflammatory bursa.
Non-Infected Bursa Surgery
Surgery can still be required if nonsurgical therapy for elbow bursitis is ineffective if the condition is not caused by an infection. In this instance, the bursa removal operation is often done as an outpatient treatment. Not a single muscle, ligament, or joint structure is affected by the procedure.
You normally don’t require formal physical therapy following surgery, but there are activities you may do to increase your range of motion. Usually, they are approved a few days after the procedure.
Physical Therapy for Olecranon Bursitis
The following actions may be taken at home to aid in the healing of your bursitis:
Rest:
Resting the joint is an excellent place to start if you’re seeking to treat your bursitis.
Joints that are subjected to repeated actions on a regular basis are susceptible to bursitis. Sports like tennis or golf might lead you to acquire this illness.
Long durations of elbow bending or trauma such as falling on your elbow can also result in elbow bursitis.
The best course of action is to refrain from the activity or regular action that is causing your inflammation. Bursitis frequently resolves on its own if you can prevent aggravating the bursa.
Ice
For the first 48 hours following the onset of symptoms, icing the elbow can help minimize swelling.
By lowering blood flow to the region, the cold helps to alleviate inflammation. Additionally, by lowering nerve activity, cold treatment can assist in providing momentary pain relief.
Avoid putting ice directly on your elbow as this may lead to skin damage. Try covering the ice in a towel instead. To avoid damage to the nerves, apply ice to the skin for brief intervals of 15 to 20 minutes.
Heat
Try heating up something or having a warm bath. Increased circulation from heat can aid in reducing stiffness. Another effective remedy for your pain is heated.
To reduce the risk of burns, it’s crucial that your heat therapy be warm rather than hot.
Bursitis and many other forms of inflammation can be effectively treated with heat and cold therapy. On the other hand, discontinue the medication right once if it either increases your pain or swelling.
Changes in activity
It’s best to stay away from activities that put strain or pressure on the elbow, such as heavy lifting, workout sports, and some contact sports.
Try your best to refrain from doing whatever prompted your flare-up if it is a recurring action. Try scheduling frequent relaxation periods or rotating that activity with others if you must. See your doctor about substitutes that you might try.
Elbow Pad
To protect your elbows whether you sit, work, or sleep, use an elbow pad.
The cushioning envelops the region surrounding the elbow in addition to helping you avoid striking it.
The covering retains heat and compresses. Warmth and compression can both aid in reducing stiffness and edema.
Exercises
To lessen pain and stop issues down the road, certain workouts can help strengthen the muscles that surround the elbow.
Pain reduction techniques: Physical therapy techniques have the potential to be beneficial in lowering pain and inflammation. For instance, electrical stimulation and phonophoresis. However such methods aren’t always necessary for the majority of people with olecranon bursitis. In addition, the physical therapist can educate the patient and provide compensatory techniques for upper extremity rest during the healing process.
Prior to attempting elbow rehabilitation activities, get medical advice. If you are in pain, you should also start off slowly and reduce the amount of activity you undertake.
Common stretches include
- Flexion stretch
Raise the aching arm and bend it at the elbow.
Turn your palm in your direction.
Apply a little pressure on the back of the affected forearm with your other hand.
You should feel a stretch in your upper arm as you press your hand toward your shoulder.
After holding for 15 to 30 seconds, repeat a few times.
- Extension stretch
With your palm facing away, extend the affected arm in front of you.
With your fingers pointing above, bend your wrist back.
Gently bend your wrist farther with your other hand until your forearm starts to lengthen.
Hold for a few repetitions of 15 to 30 seconds each time.
Follow the same instructions, except this time, point your finger downward.
- Pronation and supination stretch
Make a fist with the affected elbow at your side, bent at a 90-degree angle.
Turn your forearm back and forth slowly in each direction, rotating it such that your hand faces up and down.
Take six seconds to hold each posture, and then ten seconds of relaxation in between.
Do this eight to twelve times.
- Hand flips
With your palm facing down, rest your hand and forearm on your thigh while seated.
Turn your hand over so that the palm is facing up while keeping your forearm on your thigh.
Do this eight to twelve times.
Complications
Persistent pain and the resulting diminished functional use of the affected upper extremity are complications of the illness process.
The following are possible aspiration or injection complications:
Swelling: This might happen again, especially if the patient doesn’t keep the area adequately pressured or iced, or if there was an infection at the time of the first aspiration.
Virus Infection
Continuous outflow via the injection channel
Ulnar nerve injury: If the aspiration or injection is done via a medial route, this might potentially happen.
Prevention
Although you cannot avoid all cases of bursitis, you can lessen its severity. It is also possible to reduce the likelihood of recurrences.
Try to avoid lifting large objects and limit the amount of strain on your joints. Nevertheless, developing muscle and exercising might help ward off more injuries.
Stretching and warming up before engaging in any exercise or activity that might put stress on the joint is important if you have bursitis or are prone to it. If you’re unsure about the kinds of workouts to perform, see a fitness expert.
Prognosis
If there are no significant medical co-morbidities, particularly if there are immunosuppressive diseases, olecranon bursitis is usually benign. There is very little possibility that an infected bursa may lead to a systemic infection in a typically healthy patient. Actually, the young, healthy patient may be more likely to experience spontaneous remission without treatment than to get ill with a systemic condition.
Conclusion
In conclusion, inflammation of the bursa near the elbow’s tip is a sign of olecranon bursitis. Efficient and suitable treatment is essential, regardless of the underlying cause—trauma, abuse, or illness.
The treatment of olecranon bursitis may frequently be relieving, and problems can be avoided, with a mix of rest, medicine, and sometimes medical treatments. Seeking early medical care guarantees a more customized and efficient treatment for this elbow-related condition.
FAQs
How is bursitis of the olecranon treated?
If there is no illness of the olecranon bursa, the initial course of treatment is to avoid activities that provide direct pressure on the elbow. Reduce the swelling by using a compression sleeve or wrap to apply pressure and icing the elbow for 15 to 20 minutes twice a day.
Why does elbow bursitis occur?
Bursitis is most commonly caused by repetitive motions or postures that put pressure on the bursae around a joint. Two examples include tossing a baseball or constantly raising something over your head. Reaching out and placing your arm on your elbows.
Is surgery necessary for olecranon bursitis?
Rest, corticosteroid injections, anti-inflammatory drugs, and fluid drainage are the usual treatments for elbow bursitis or inflammation of the bursa. Elbow surgery may be necessary if the bursa becomes infected and does not improve after fluid evacuation or antibiotic treatment.
Which three bursitis symptoms are present?
Bursitis is most commonly characterized by pain, swelling, and pain around a joint. Anti-inflammatory drugs and rest are effective treatments for bursitis.
Is bursitis of the olecranon serious?
Olecranon bursitis is not that uncommon. There is no connection between this condition and death. Posterior elbow pain can cause morbidity and limit one’s activities. Usually, men in their 30s to 60s are impacted.
Is bursitis of the olecranon painful?
Some people with elbow bursitis may not even have any swelling at first, nor do they ever experience any pain. However, when the olecranon bursa grows larger, it may cause pain or pain, particularly while bending or straightening.
Olcranon bursitis is treated by whom?
Physicians who treat elbow bursitis include orthopedic surgeons, physical therapists, sports medicine specialists, and primary care physicians.
What causes olecranon bursitis the most frequently?
Trauma, such as striking the elbow on a hard surface or falling on it, is a typical cause of olecranon bursitis. Players who play football, hockey, basketball, and volleyball frequently suffer from elbow falls, which can occur at any sporting event.
Which three bursitis symptoms occur?
The most common signs of bursitis are pain, edema, and soreness around a joint. Anti-inflammatory drugs and rest are effective treatments for bursitis.
Which antibiotic works best for bursitis?
Patients with septic bursitis are given antibiotics. Tablets or capsules containing antibiotics, such as erythromycin, clarithromycin, and flucloxacillin, are taken two to four times daily.
Does heat help with bursitis?
Use heat before engaging in any activity if you have a persistent bursa injury that doesn’t seem to go away. This will help to loosen up the soft tissue in the joint and increase its flexibility.
Is surgery required for bursitis?
The RICE (rest, ice, compression, and elevation) approach is one kind of early therapy; however, surgery may be required if the symptoms persist and the enlarged bursa gets infected. Because the infection can spread throughout the body, an inflamed elbow bursa poses a serious risk to life.
What might happen if you didn’t treat bursitis?
Chronic discomfort: If bursitis is left untreated, the bursa may thicken or grow permanently, resulting in persistent inflammation and pain. Muscle
atrophy: Loss of surrounding muscle and a prolonged reduction in joint usage might result in a decrease in physical activity.
References
- Physiotherapist, N. P. (2023, December 13). Olecranon Bursitis: Causes, Symptoms, Diagnosis & Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/olecranon-bursitis/
- Professional, C. C. M. (n.d.). Elbow (Olecranon) Bursitis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22553-elbow-olecranon-bursitis
- Physiotherapist, N. P. (2023, August 31). Olecranon Bursa – Anatomy, Development, Location. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/olecranon-bursa/