What is a Sprengel’s Shoulder Deformity?
Sprengel’s shoulder deformity, also known as congenital high scapula or congenital elevated scapula, is a rare musculoskeletal anomaly characterized by an abnormally high-positioned shoulder blade (scapula) on one side of the body.
It is a rare congenital disorder that affects how the shoulder blade (scapula) develops and is positioned in the early stages of fetal development. Carl Sprengel, a German physician, is honored to have been the first to describe this disease in 1891.
The scapula fails to drop from its original high position in the developing baby in Sprengel’s Shoulder. Here, it lays more superiorly. It is ill-formed and hypoplastic. It is linked to congenital anomalies such as cervical ribs.
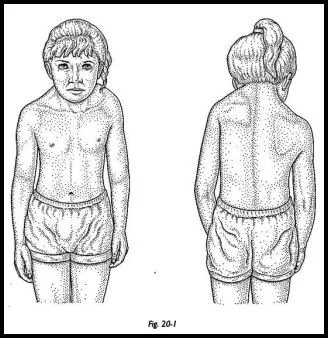
When a person has Sprengel’s shoulder deformity, the affected side of the body has a higher scapula because they are unable to descend to their usual position in the back. Consequently, the scapula may appear atypically small, tilted, and raised in relation to the opposite side. Although it can affect one or both shoulders, the right shoulder is the most frequently affected.
History:
Otto Gerhard Karl Sprengel, a German surgeon who lived from 1852 to 1915, is credited with writing about four instances in 1891.
Anatomy Related to Sprengel’s Shoulder
As part of the relocation operation, significant dissection is necessary, which puts several important tissues at risk. Among these constructions are the following ones:
- Dorsal scapular nerve
- Spinal accessory nerve
- Suprascapular nerve
The dorsal scapular nerve runs along the plane between the erector spinae and the rhomboid muscle, at the superomedial edge of the scapula. The subscapular muscles and serratus anterior continue to be anterior to the dorsal scapular nerve.
When dissecting the periscapular muscles at the superomedial angle of the scapula and when the rhomboid and trapezius muscles are reflected off the spine as a single unit during the Wood operation, there is a chance that the dorsal scapular nerve will be injured (see Treatment). Thus, it is crucial to maintain a subperiosteal position when releasing the periscapular muscles, particularly at the superomedial angle of the scapula.
The spinal accessory nerve is situated between the rhomboid and trapezius muscles, which puts it in danger. However, due to its positioning, the nerve is seldom harmed when the two muscles work together.
When the superior part of the scapula is dissected, the suprascapular nerve, which runs in the suprascapular notch of the scapula, may be damaged if the dissection is prolonged too far laterally. During the process, damage to the nerve can be prevented by positioning oneself at least one centimeter medial to the notch.
Causes of Sprengel’s Shoulder
Although the exact reason for Sprengel’s shoulder deformity is not always known, abnormal development in the early stages of embryogenesis is thought to be the cause. Certain cases could be linked to additional congenital conditions or syndromes, including Klippel-Feil syndrome, which impacts the cervical spine’s development.
A congenital condition known as Sprengel’s Shoulder develops and shows as:
- The early development of the developing baby is affected.
- This might be caused by an extension of muscle that doesn’t develop from the skull to the scapula, or by an incomplete descent of the shoulder girdle by the third month.
- Genetic defect.
- Sprengel’s deformity may be associated with Klippel-Feil syndrome, clavicular abnormalities, rib abnormalities, limb length discrepancy, scoliosis, spina bifida, hemivertebrae, and underdevelopment (hypoplasia) of the shoulder or neck muscles.
Pathology
Because surrounding structures depend on the appropriate growth of the scapula, Sprengel’s deformity often affects them. Raised scapulas are the most common symptom, however, there are other indicators as well, such as weak surrounding muscles. a disruption in the development of bones, cartilage, and muscles.
The trapezius muscle, rhomboids muscle, levator scapulae muscle, pectoralis major muscle, latissimus dorsi muscle, and sternocleidomastoid muscle may be absent or deficient. If the serratus anterior muscle is weak, the scapula may wing.
Epidemiology
According to most research in the field of medicine, women are three times more likely than men to have Sprengel deformity. Other research indicated that men and women may be equally affected by the illness.
Associated Conditions
Most of the time, additional congenital abnormalities—particularly those affecting the ribs and vertebrae—coexist with Sprengel’s Shoulder. An omovertebral bar, a fibrous, cartilaginous, or osseous connection between the scapula and cervical spine, is frequently present.
Furthermore, it is often associated with hypoplasia or atrophy of the surrounding muscles, which can result in greater shoulder misalignment and limited shoulder mobility.
Patients with Sprengel deformity commonly have the following conditions and abnormalities:
- Klippel-Feil syndrome
- Kyphoscoliosis,
- Torticollis,
- Spina bifida,
- Underdevelopment of the humerus or clavicle
It is necessary to assess each patient who presents with a Sprengel deformity for these possible co-existing disorders.
Symptoms of Sprengel’s Shoulder Deformity
The severity of the symptoms associated with Sprengel’s shoulder deformity and any underlying abnormalities might vary.
- An abnormal posture of the shoulders.
- The scapula is 2–10 cm high.
- An elevated shoulder blade can cause a hump at the base of the neck.
- Adjacent undeveloped muscles.
- limited shoulder and arm range of motion (ROM) on the affected side.
- limitation on the abduction and elevation of the shoulders.
- There is restricted or limited cervical spine motion.
- From mild torticollis to severe spine abnormalities like kyphoscoliosis, there are many different types of neck deformities.
- There might be spina and cranial bifida.
Depending on the severity of the condition and the presence of additional skeletal or muscular abnormalities, the signs and symptoms of Sprengel’s deformity might vary. It could not exhibit any obvious symptoms or indicators in certain individuals. The deformity is usually minor and affects just one side, although reports of bilateral occurrences exist as well. In these circumstances, the deformity is functionally incapacitating but far more acceptable in terms of appearance.
In addition to creating an uneven position of the shoulder, a raised shoulder blade can result in a lump at the back of the base of the neck, undeveloped or incomplete muscles nearby, and a limited range of motion on the side with the affected shoulder and arm. Between the shoulder blade and the next vertebrae in certain people, there is bone, cartilage, or fiber-like tissue.
Several typical characteristics linked to Sprengel’s deformity consist of:
- Klippen Feil syndrome
- scoliosis
- disparity in limb length, undeveloped vertebrae (backbone), and additional, fused, or absent cervical ribs
- deformities of the chest, collarbone, or bodily organs misplaced to the other side (liver on the left, heart on the right, for example).
- spina bifida occulta
- cleft palate
Classification
The Sprengel’s Shoulder Deformity is graded using the Cavendish classification system:
Grade Level of Sprengel’s Shoulder Deformity
- grade 1 Very mild deformity
The deformity is nearly undetectable when clothes are worn. - grade 2 Although still deformity is still small, the abnormality is visible as a bump.
The superomedial portion of the high scapula is convex and has a hump on it. - grade 3 moderate Sprengel’s Shoulder deformity with 2–5 cm of apparent shoulder elevation.
- grade 4 significant abnormalities with neck webbing and >5 cm elevation of the affected shoulder.
Diagnosis
Imaging tests, a physical examination, and a medical history are usually used to diagnose Sprengel’s shoulder deformity.
Medical history: The physician will begin by obtaining a history of the patient’s diseases, taking into account any family history of congenital disorders or syndromes that may be connected to the deformity of Sprengel’s shoulder.
Physical examination: The patient’s shoulder and upper back will be evaluated during a comprehensive physical examination. The physician will be on the lookout for any related anomalies or physical characteristics, improper scapula position, limits in shoulder range of motion, and indicators of asymmetry.
The diagnosis of Sprengel deformity involves a number of specialized diagnostic procedures, including sophisticated imaging scans, a thorough clinical examination, and the determination of certain symptoms.
X-Ray
An accurate method of identifying Sprengel deformity is by a chest radiograph, sometimes referred to as an anteroposterior chest x-ray. The phrase “anteroposterior” means “front to back.” The patient is positioned with their back to the film plate and the X-ray in front of them throughout this examination. The scapula that is affected exhibits elevation and rotation, with the inferior angle pointing laterally.
CT Scan
A CT scan with 3D reconstruction is used to evaluate the omovertebral connection, scapula dysplasia, and malpositioning. For preoperative planning, it is beneficial.
Computed tomography (CT) scans are two sophisticated imaging modalities that are commonly utilized to confirm a diagnosis of Sprengel deformity. X-rays and a computer are used during a CT scan to create a film that displays cross-sectional images of certain tissue characteristics.
Magnetic resonance imaging (MRI)
Magnetic field waves are used in magnetic resonance imaging (MRI) to produce cross-sectional images of bodily tissues. These tests have the ability to reveal an omovertebral bone. The application of cutting-edge imaging techniques can also help with surgical procedure planning and oversight.
In imaging studies, it is sometimes difficult to recognize an omovertebral bone due to the likelihood of overlay bones.
Treatment of Sprengel’s Shoulder Deformity
A multidisciplinary approach is usually used to treat Sprengel’s shoulder deformity, with advice from orthopedic surgeons, physical therapists, and other experts. Enhancing the affected shoulder’s functional capacities and range of motion is the main objective of therapy. Physical therapy is one form of conservative treatment that can help with posture and shoulder strength.
Surgical intervention may be considered in more severe situations or when conservative approaches prove to be ineffective. Repositioning the scapula, removing soft tissue attachments that impede mobility, and treating any related abnormalities are all possible surgical treatments.
Physical Therapy Treatment
An important part of treating Sprengel’s shoulder malformation is physical therapy. For this condition, improving shoulder function, range of motion, muscular strength, and posture are the main objectives of physical therapy. The particular course of therapy will depend on the requirements of each patient and the severity of their disease.
The following are a few typical physical therapy techniques for treating Sprengel’s shoulder deformity:
- Exercises to increase the affected shoulder’s range of motion are created by physical therapists. Shoulder flexion, abduction, external and internal rotation, and scapular motions are a few such workouts.
- Exercises for strengthening the muscles: Improving stability and function requires strengthening the muscles surrounding the shoulder and scapula. The deltoids, rotator cuff muscles, and scapular stabilizers will all be targeted by particular workouts.
- Training for posture: Managing Sprengel’s shoulder malformation requires proper posture. Physical therapists will help patients align their posture correctly and will give them exercises to build stronger muscles that support healthy posture.
- Stretching: Performing stretches can assist to increase flexibility and lengthen tense muscles. Improving general shoulder mobility may be facilitated by focusing on tense muscles in the upper back and shoulder region.
- Manual therapy: Physical therapists may employ hands-on methods to manipulate and move the soft tissues around the shoulder joint in order to enhance joint mobility and lessen muscular tension.
- Assistive equipment: Slings or braces are examples of assistive devices that may be suggested in certain situations to stabilize and support the shoulder while it heals or is being used for a particular activity.
- Functional training: To enhance the patient’s capacity to carry out everyday duties and activities, physical therapists will concentrate on functional exercises that mimic motions seen in real life.
- Patient education is a crucial part of physical therapy treatment. It involves informing the patient and their caregivers about the disease, appropriate body mechanics, and exercises to be done at home.
- Physical therapists will keep an eye on patients’ development during the course of therapy and modify the plan as necessary to achieve the best possible results.
It is significant that the beneficial effect of physical therapy is contingent upon the specific circumstances of each patient as well as their level of adherence to the recommended exercises and treatments. In certain cases of severe Sprengel’s shoulder deformity, surgical intervention may be required, and physical therapy may be part of the recovery process following surgery. As usual, a trained healthcare expert with expertise in orthopedic and musculoskeletal disorders should be consulted in developing the treatment strategy.
Surgical Treatment of Sprengel’s Shoulder Deformity
Several surgical procedures are utilized to address the deformities produced by Sprengel’s shoulder. The methods derived from the Woodward operation and modified Green scapuloplasty are the most often employed ones. These procedures entail extracting the omovertebral bone and the projecting portion of the scapula, as well as translating the scapula inferiorly to a more caudal position. To avoid harm to the brachial plexus, clavicle osteotomies can also be done.
Choosing the surgical procedure in close collaboration with the patient’s family, physicians, and other healthcare providers is the best course of action. The specifics of the patient’s condition, a full analysis of the risks and benefits, including any possible long-term consequences, and other pertinent factors should all be taken into account when making decisions.
Operative Procedures
- Woodward procedure
In order for the scapula to rotate into enhanced shoulder abduction and move inferiorly, the medial parascapular muscles near the root of the spinous processes are cut off and then rejoined.
Surgical descent together with the removal of the upper medial edge of the scapula characterize Modified Woodward.
- Schrock, Green procedure
Extraperiosteal separation of the paraspinal muscles occurs at the scapular insertion and reinsertion following the inferior movement of the scapula using traction cables.
- osteotomy of the clavicles
in conjunction with the aforementioned surgical procedures carried out prior to scapula movement in situations of severe deformity in order to avoid harm to the brachial plexus.
- Bony resection
For cosmetic purposes, extraperiosteal excision of the proximal scapular prominence can be performed either on its own or in combination with other procedures.
- The results
Up to 40–50 degrees can be improved by the Woodward, Schrock, and Green procedures.
Rehabilitation Following Surgery
After surgery, the patient’s shoulder was immobilized to promote recovery and reduce any possible pain.
Reducing deformity and allowing the shoulder to move normally are the objectives of physical therapy.
- TENS stands for transcutaneous electrical nerve stimulation.
Transcutaneous electrical nerve stimulation, which can be set off by stretching exercises, relieves pain.
Ultrasound may readily break down adhesions.
- Thermodynamic treatment:
Using thermotherapy, muscles are relaxed before starting an activity program.
- Mobilization:
Six weeks later, passive and active range-of-motion exercises will be the focus of physiotherapy. Gradually relaxing and passively mobilizing the shoulder and scapula is done to enhance the shoulder’s range of motion and flexibility. early mobilization of the shoulder and scapula, including abduction and elevation movements.
Strengthening exercises
All exercises that target specific muscle groups aid in strengthening the weaker muscles. The shoulder girdle muscles can be strengthened by isometric and isotonic exercises including bridging, arm supports, forearm supports, shoulder shrugs, and pushups.
- Exercises for stretching the upper trapezius muscle:
The child settles into a comfortable chair. He puts his right hand just below her crotch. The therapist supports the child’s shoulder by holding onto the lateral border and acromion of the scapula. The youngster then flexes his neck and twists it to the left. And with that, the child places her left hand right below her knees. The therapist supports the child’s shoulder by holding onto the lateral border and acromion of the scapula. The child then flexes his neck and twists it to the right. The child keeps these neck positions for ten seconds while stretching.
- Scapula protraction exercise:
As it is, the child is supine. with her right shoulder flexed ninety degrees and her elbow fully extended. The child then uses all of his effort to propel his right elbow forward. The therapist holds the acromion and grasps the scapula to prevent the child’s scapula from rising and their trunk from turning.
- Posterior tilt exercise for scapula:
With the humerus above, the shoulder abducted to 130° to 145°, and the forearm neutral, the infant is lying on his back. The child then gently puts the dorsum of her left palm on her forehead, placing it beneath her brow. When the patient extends her right arm with his elbow extended, the therapist stops her from elevating her shoulder blade.
Family Education
It is advised that parents supervise their children throughout every exercise session. When exercising at home, parents should keep an eye on their kids to maintain proper scapular mobility and prevent scapular elevation. If the superior border of the scapula slips upward, the activity should be stopped and the kid should try it again.
Prognosis
For those with Sprengel’s shoulder deformity, the prognosis might change depending on how severe the problem is and how well therapy works. Better results and enhanced shoulder function can result from early diagnosis and management.
It is crucial to remember that Sprengel’s shoulder deformity is a complicated disease and that each instance will present differently and react differently to therapy. It is imperative that you get medical examination and management from trained healthcare experts if you believe you or someone you know is impacted by this condition.
Summary
One shoulder blade is unusually elevated on the back in a rare congenital disease known as Sprengel’s shoulder deformity. Asymmetry, restricted shoulder mobility, and related abnormalities may result from it. A diagnosis is based on a combination of imaging, physical examination, and medical history. The goals of physical therapy are to enhance posture, range of motion, and shoulder function. In more severe situations, surgery could be recommended. Early diagnosis and care are critical for better outcomes.
FAQs
What causes Sprengel’s deformity?
Although the precise source of Sprengel’s shoulder deformity is not always known, aberrant development in the early stages of embryogenesis is thought to be the cause. Certain cases could be linked to additional congenital conditions or syndromes, including Klippel-Feil syndrome, which impacts the cervical spine’s development.
How is Sprengel’s shoulder taken care of?
A multidisciplinary approach is usually used to treat Sprengel’s shoulder deformity, with advice from orthopedic surgeons, physical therapists, and other experts. Enhancing the affected shoulder’s functional capacities and range of motion is the main objective of therapy. Physical therapy is one form of conservative treatment that can help with posture and shoulder strength.
Surgical intervention may be considered in more severe situations or when conservative approaches prove to be ineffective. Repositioning the scapula, removing soft tissue attachments that impede mobility, and treating any related abnormalities are all possible surgical treatments.
What is the scapular malformation caused by Sprengel?
The rare congenital disorder known as Sprengel’s shoulder deformity, sometimes called congenital high scapula or undescended scapula, affects how the shoulder blade (scapula) develops and is positioned in the early stages of fetal development.
This condition also causes localized muscle atrophy or hypoplasia, which causes the shoulder to distort and become less mobile.
What is the process used by Sprengel Woodward?
The Woodward procedure includes extracting the roots of the trapezius and rhomboid muscles from the spinous process and pressing them downward, following the removal of the omovertebral bone and any additional fibrous bands keeping the scapula together.
Does Sprengel’s shoulder provide a challenge?
Congenital elevation of the scapula, or Sprengel’s deformity, is a complex pectoral girdle malformation that impairs function as well as vision.
Where may one observe Sprengel deformity?
The most prevalent congenital shoulder anomaly is the Sprengel deformity, also known as congenital elevation of the scapula. It is a complicated malformation of the shoulder. Radiographs can frequently be used to make an initial diagnosis, but an MRI or CT scan is sometimes required to assess the specifics of the problem.
What differentiates Sprengel from Klippel Feil Syndrome?
A congenital condition known as Klippel-Feil syndrome (KFS) is caused by the fusion of cervical vertebral bodies as a result of signaling pathway dysregulation during somite development. It is frequently associated with Sprengel deformity and scoliosis.
What is the syndrome of Sprengel’s deformity?
The displacement of the shoulder blade is estimated to be between 2 and 10 cm or around 0.5 and 4 inches. The primary indications of Sprengel deformity include restricted or limited mobility of the cervical spine, arm, and shoulder blade on the affected side.
How is the Sprengel deformity surgically treated?
It has been suggested that older children should have an omovertebral bone, the superomedial piece of the scapula, or both removed. In addition to improving shoulder function and appearance, this procedure is safe and technically simple.
Is Sprengel’s deformity an impairment?
Congenital elevation of the scapula, also known as Sprengel’s deformity, is a complicated pectoral girdle abnormality that causes cosmetic and functional handicaps.
References
- Physiotherapist, N. P. (2023, December 13). Sprengel’s Shoulder Deformity: Cause, Symptoms, Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/sprengel-shoulder/
- Sprengel’s Deformity of the Shoulder | Best Treatment in Bangalore. (2022, October 4). Bangalore Shoulder Institute. https://bangaloreshoulderinstitute.com/sprengels-deformity-shoulder/