Phelps Approach
Introduction
The Phelps Approach refers to a comprehensive treatment strategy developed by orthopedic physician W.M. Phelps, primarily aimed at addressing the needs of individuals with cerebral palsy.
One of the first people to treat cerebral palsy was the orthopedic physician W.M. Phelps of Baltimore. (Phelps 1949, 1952; Slominski 1984) He promoted the formation of rehabilitation teams of physiotherapists, occupational therapists, and speech therapists. Phelps’ treatment strategy was centered around the following essential components:
A detailed diagnostic categorization of every child to as certain the best course of action. Phelps classified cerebral palsy into five main categories and several subcategories.
Fifteen modalities are used, with particular combinations chosen based on the kind of cerebral palsy. The following were the modalities:
- Massage for hypotonic muscles; nevertheless, it is not advised for kids with athetoid and spasticity.
- Joint mobilization and demonstration of the required movement by passive motion across the joint range. The kind of cerebral palsy affects how quickly a person moves.
- Motion with active assistance.
- Forceful motion.
- With the child’s ability, to resist movement.
- Conditioned motion, which uses the same song or jingle for the same movement modality and involves a regimen for infants, young children, and mentally impaired children (2–5).
- Confused motion, also known as synergistic motion, is when a muscle group is resistant to another to activate the inactive muscle group simultaneously. Typically, mass motions like the flexion withdrawal reflex or the extensor thrust were employed.
- Combined motion, which uses modalities 2, 3, 4, and 5 to teach the motion of several joints, such as the flexion of the elbow and shoulder.
- Relaxation methods include tensing and relaxing different bodily regions, as well as consciously “letting go” of the body and its components (Levitt 1962). Athetoids are the primary target of these techniques.
- Movement from relaxation, which involves conscious control of movements once relaxation is attained. Most often, children use it to control erratic movements consciously.
- Rest: Athetoids and kids with spasticity should take breaks from activity.
- Reciprocation is the practice of training one leg after the other in a cycling rhythm while knee walking, stepping, crawling, or lying down.
- Practice your balance when standing and sitting while wearing braces.
- The hand function is trained by the use of reach, grab, and release.
- Daily living abilities include grooming, eating, bathing, and restroom use. Occupational therapists provide a lot of assistance.
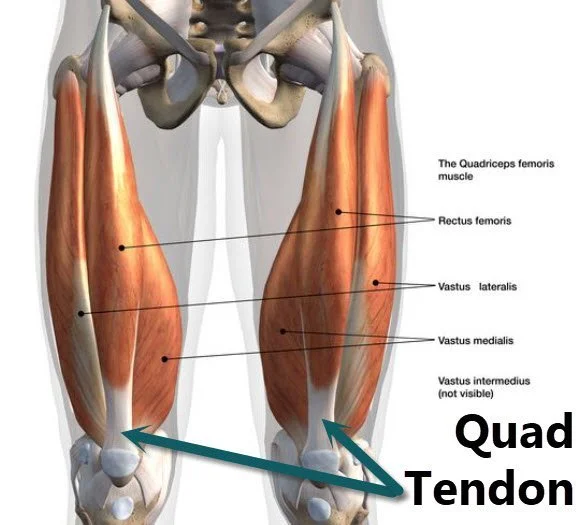
Muscle education, which involves analyzing whether muscles are spastic, weak, normal, or zero cerebral – being unable to act. Muscles antagonistic to spastic muscles are activated to obtain muscle balance between spastic muscles and their weak antagonists. Athetoids were trained to control simple joint motion and did not have muscle education. Weak muscular areas might benefit from strengthening activities for ataxics.
Using calipers or braces with Phelps’s design to control athetosis, correct abnormalities, and provide a straight posture. The bracing is significant and has been used for a long time. Youngsters wearing lengthy leg braces with pelvic bands back support, and occasionally spinal braces are taught how to stand and walk. As they advance, the pelvic band back supports, and below-knee braces are removed. With the locking joints at the hip and knee of the full-length brace, control may be taught with them locked or released.
Other scholars have also created theories on muscle education, such as Rood (1962) and Tardieu et al. (1982). Both spastic and antagonistic muscles should be strengthened, according to Plum and Molhave (1956). However, because spastic muscles are often shorter, they should be worked in their outer ranges, whereas antagonistic muscles should be exercised in their middle and inner ranges. Tabary et al. (1981), in a ‘factorial analysis’, identified the specific problem in the muscles which gives rise to abnormalities and deformities, and treatment is given where indicated. Alcohol injections were used to diminish spasticity, but neurologists no longer recommend this due to side effects. Other drugs are used by them.
Studies by Tabary et al. (1972), Tardieu et al. (1982), and Dietz (1992) have shown specific changes in muscle length (hyperextensibility) of spastic muscles and also changes in the muscle structures, which are quoted in current therapy literature. Tardieu et al. (1988) suggest prolonged passive stretch for 5–7 hours to obtain a change in length helps used braces for treatment, but nowadays, lighter and better-designed orthoses are available.
The equipment that therapists in Phelps’ center recommended is still in use in occupational and physiotherapy, and it has been improved over time along with the creation of new aids. For instance, there used to be an upright standing frame, but it has been enhanced and replaced with various adjustable designs that aid in weight-bearing to prevent hip dislocation. Phelps suggested weight-bearing as a way to prevent hip subluxation, but modern standing frames are now used to promote early weight-bearing and hip joint development.
Phelps recommended using resisted motion to build strength in cerebral palsy patients, and studies by Damiano and others have confirmed the effectiveness of such exercises. However, Damiano acknowledges that some children with spasticity have issues with poor isolation of muscle control, which Phelps called ‘confused motion.’ Therapists have since discouraged confused motion and instead focus on training selective motion of particular muscle groups as part of motor development.
Phelps’ approach to treatments centers around five main modalities:
- Massage: This was used for hypotonia but not recommended for spasticity and athetosis patients.
- Passive motion: Passive movements were used to mobilize joints, maintain soft tissue length, and demonstrate the required movement.
- Active assisted movements: Active and resisted movements were given according to the patient’s needs and ability.
- Conditioned and synergistic motion: Conditioning and synergistic motion involve resistance to one muscle group to facilitate the contraction of an inactive muscle group in the same synergy, which is a familiar concept in PNF.
- Rest: Rest periods were also included, and their beneficial effects should not be neglected in more recent approaches.
Phelps described fifteen modalities, and specific combinations were used for each type of cerebral palsy. Reciprocation, balance, reach, grasp, release, and daily living skills training are some of the other modalities that Phelps’s approach includes.
Phelps’s approach also incorporated the use of braces and calipers as a modality…
The purpose of using braces and calipers was to correct deformity, obtain the upright position, and control athetosis. They were worn extensively for many years, and as the child progressed, the support was gradually removed until only below-knee irons and boots were used.
According to many experts, the use of bracing and splinting is now considered effective as long as it is carefully designed for a specific individual and a particular purpose.
References
- Phelps Approach – Mobile Physiotherapy Clinic. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/phelps-approach/#google_vignette
- Why Choose the Phelps Center? (n.d.). Kennedy Krieger Institute. https://www.kennedykrieger.org/patient-care/centers-and-programs/cerebral-palsy-and-neurodevelopmental-medicine/why-phelps
- Outline of treatment approaches. Musculoskeletal Key.