Cervical Radiculopathy
Cervical radiculopathy refers to a condition where a nerve root in the cervical spine (neck region) is compressed or irritated, leading to symptoms such as pain, numbness, tingling, or weakness that radiates down to one’s shoulder, arm, or hand. It’s often caused by conditions like herniated discs, bone spurs, or degenerative changes in the spine.
Definition
Cervical radiculopathy, sometimes known as a “pressed nerve,” is a condition that happens when a nerve in the neck becomes compressed or inflamed where it branches out from the spinal cord. This can lead to discomfort spreading into the shoulder and/or arm, as well as muscular weakening and numbness.
Cervical radiculopathy is typically caused by age-related “tear and damage” alterations in the spine, such as arthritis (Degeneration). In younger people, the most common cause is a sudden accident that results in a herniated disc. However, in certain situations, the start of symptoms is related to a traumatic problem.
Anatomy
Your spine is made up of 24 vertebrae, which are placed on top of one another. These bones form a canal that protects the spinal cord.
The cervical spine is made up of seven tiny vertebrae that connect the base of the head to the neck.
Spinal cord and nerves: Your spine also contains the spinal cord and nerves. These “electrical cables” transmit information from your brain to your muscles as they pass through the spinal canal. Nerve roots arise from the spinal cord through vertebral holes (foramen)
Intervertebral disks. Intervertebral discs are flexible structures that sit between your vertebrae. They function as shock absorbers when you walk or run.
Intervertebral discs are flat and circular, roughly half an inch thick. They are comprised of two components:
- Annulus fibrosus. This is the disk’s strong, flexible outer ring.
- Nucleus pulposus. The center of the disc is spongy and jelly-like.
- Cervical spinal nerves extend to the
- shoulders.
- Arms.
- Chest.
- Upper back.
As a result, the neurological symptoms of cervical radiculopathy might spread down from your neck to any of these body areas, depending on which nerve root are suffering. Cervical radiculopathy often affects only one side of the body, such as the right arm, rather than both.
Cervical radiculopathy can cause neurological symptoms such as pain, which can spread down the neck.
- Numbness.
- tingling or a “pins and needles” sensation.
- Muscular weakness.
- Weakened reflexes.
- Cervical radiculopathy affects individuals differently. You may have any of the neurological symptoms listed above, or simply one
Causes of Cervical Radiculopathy
Any condition that pinches or irritates a cervical nerve root might result in cervical radiculopathy. Cervical radiculopathy can affect anybody, however, it tends to be more frequent in adults.
Cervical radiculopathy can be caused by various factors, including:
- Herniated Discs: A disc herniates when the jelly-like structure in the center (nucleus) presses against the outer ring (annulus). If the disc is severely torn or damaged, the nucleus may squeeze out. When a herniated disc bulges out towards the spinal canal, it produces pressure on the sensitive nerve root, resulting in discomfort, pain, and weakness in the area supplied by the nerve. Lifting, pulling bending, or twisting are common causes of herniated discs. Cervical radiculopathy caused by a herniated disc is more frequent in adults under the age of 50.
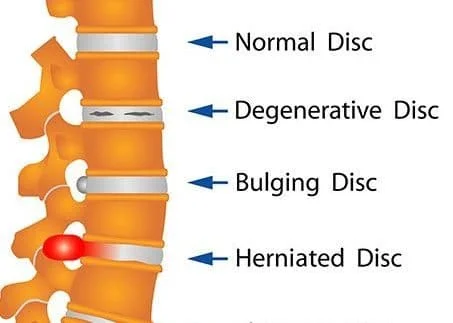
- Degenerative Disc Disease: Wear and tear on the discs in the cervical spine can lead to narrowing of the space between vertebrae, potentially causing compression of nerve roots. People in their 70s and older are more likely to develop cervical radiculopathy due to foraminal constriction caused by arthritis. The foramen is a bone hollow opening between vertebrae through which spinal nerve roots pass.
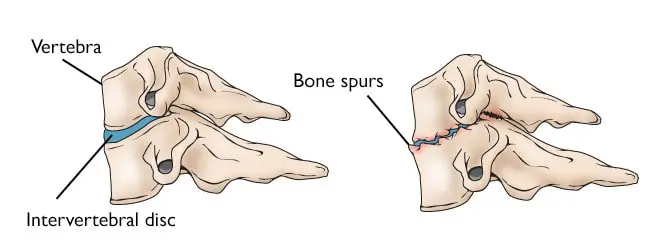
- Bone Spurs: Also known as osteophytes, these bony growths can develop on the edges of vertebrae due to aging or degenerative conditions, potentially compressing nearby nerve roots.
- Spinal Stenosis: Narrowing of the spinal canal, often due to bone overgrowth or thickened ligaments, can put pressure on nerve roots.
- Trauma or Injury: Such as whiplash from a car accident, which can damage spinal discs or structures and lead to nerve compression.
- Degenerative Changes: Degenerative changes in the disks are often called arthritis or spondylosis. Arthritis or spondylosis can cause changes in the spine that contribute to nerve compression. Cervical radiculopathy caused by disc degeneration is more frequent in adults aged 50 and 60.
- Tumors: Rarely, tumors in the spine can compress nerve roots and lead to radiculopathy.
- Infections or Inflammation: Conditions like spinal infections or inflammatory disorders can affect nerve roots in the cervical spine.
Symptoms of Cervical Radiculopathy
The symptoms of cervical radiculopathy can vary depending on which nerve root is affected and the severity of the compression or irritation. Common symptoms include:
- Neck Pain: Pain in the neck is often a primary symptom, which may be localized or radiate to the shoulders and upper back.
- Arm Pain: Pain that radiates from the neck down into one arm, often following a specific nerve pathway. The pain can range from mild to severe and may worsen with certain movements or positions.
- Shoulder Pain: Pain in the shoulder region, sometimes extending down the arm. This pain may be sharp or dull and can be accompanied by muscle spasms.
- Numbness and Tingling: A sensation of numbness, tingling, or pins-and-needles in the neck, shoulder, arm, or hand. This can occur along specific nerve pathways corresponding to the affected nerve root.
- Weakness: Muscle weakness in the arm, hand, or fingers on the affected side. This weakness may make it difficult to grip objects, lift items, or perform fine motor tasks.
- Changes in Reflexes: Diminished or exaggerated reflexes in the affected arm or hand may be observed during a physical examination.
- Radiating Pain: Pain that travels down the arm in a specific pattern, such as following the path of the affected nerve root. This discomfort can get worse with specific motions or activities.
- Difficulty with Fine Motor Skills: In some cases, cervical radiculopathy can lead to difficulty with tasks that require precise movements, such as buttoning a shirt or writing.
Diagnosis
Physical Examination
Physical examination for cervical radiculopathy typically involves several components to assess nerve function, muscle strength, reflexes, and range of motion. Here are key aspects of the physical examination for cervical radiculopathy:
- Medical History: The physical therapist will start by gathering information about your symptoms, including neck pain, shoulder pain, arm pain, numbness, tingling, weakness, and any factors that worsen or improve your symptoms. They will also inquire about your medical history, previous neck injuries or conditions, and any relevant family history.
- Neck Examination:
- Range of Motion: The provider will assess your ability to move your neck in different directions, such as flexion (forward bending), extension (backward bending), lateral bending (side-to-side), and rotation (turning the head). Restricted range of motion or pain during movement may indicate cervical spine issues.
- Tenderness: The healthcare provider may palpate the neck area to identify areas of tenderness or localized pain, which can help localize the source of symptoms.
- Upper Extremity Examination:
- Muscle Strength: The provider will evaluate muscle strength in your shoulders, arms, and hands by asking you to perform specific movements against resistance. Weakness or decreased strength in certain muscle groups may indicate nerve compression.
- Reflexes: Reflexes in the arms and hands, such as the biceps reflex (C5-C6), triceps reflex (C7-C8), and finger flexor reflex (C8-T1), will be tested using a reflex hammer. Abnormal reflexes, such as hyperreflexia (exaggerated reflexes) or hyporeflexia (diminished reflexes), can indicate nerve root involvement.
- Sensory Testing: The provider may assess sensation in the arms, hands, and fingers by using light touch, pinprick, or temperature stimuli. Changes in sensation, such as numbness, tingling, or altered perception, may suggest nerve root compression.
- Provocative Maneuvers:
- Spurling’s Test: This maneuver involves extending, rotating, and tilting the head to one side while applying gentle downward pressure. It can reproduce or exacerbate symptoms of cervical radiculopathy, such as shooting pain or tingling down the arm.
- Shoulder Abduction Test: The provider may ask you to raise your arms to the sides and hold them in an abducted position (above shoulder level) to elicit or worsen radicular symptoms.
- Special Tests:
- Upper Limb Tension Test (ULTT): This test involves a series of movements and positions to assess the mobility and tension of nerves in the upper limb. It can help identify nerve compression or irritation in cervical radiculopathy.
- Cervical Compression and Distraction Tests: These tests involve applying pressure or traction to the cervical spine to reproduce or alleviate radicular symptoms, aiding in the diagnosis of nerve root compression.
Imaging Studies
Depending on the findings from the physical examination and your medical history, your doctor may order imaging tests such as X-rays, MRI, or CT scans to get a detailed view of the cervical spine and to identify any structural abnormalities or nerve compression.
- X-rays: These capture photos of thick structures like bone. An X-ray can show the arrangement of bones in your neck. It can also identify whether the foramen is narrowing or if the discs have been damaged.
- Magnetic resonance imaging (MRI) scans: These investigations give clearer pictures of the body’s soft tissues. An MRI of the neck can reveal if nerve compression is the result of soft tissue injury, such as a bulging or herniated disc. It can also help your doctor identify if your spinal cord or nerve roots have been damaged.
- Other Tests: In some cases, nerve conduction studies (electromyography or EMG) may be ordered to assess nerve function and to determine the extent of nerve damage.
Treatment of Cervical Radiculopathy
Nonsurgical Treatment
Conservative treatment for cervical radiculopathy, consisting of medication and physical therapy, is effective in most cases.
The initial therapy for cervical radiculopathy is nonsurgical. Nonsurgical therapy alternatives include:
Medications
Medication can play a significant role in managing the symptoms of cervical radiculopathy, particularly in reducing pain and inflammation. Here are some commonly used medications for this condition:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Drugs like ibuprofen (Advil, Motrin) or naproxen (Aleve) can help reduce pain and inflammation, which are common symptoms of cervical radiculopathy. These drugs are frequently used as the initial form of therapy.
- Acetaminophen: This medication (e.g., Tylenol) can help relieve pain, although it doesn’t have the anti-inflammatory effects of NSAIDs.
- Muscle Relaxants: If muscle spasms are contributing to your symptoms, your doctor may prescribe a muscle relaxant such as cyclobenzaprine (Flexeril) or tizanidine (Zanaflex) to help reduce muscle tension and improve comfort.
- Corticosteroids: These medications can be prescribed in different forms:
- Oral Steroids: A short course of oral corticosteroids, such as prednisone, may be prescribed to reduce inflammation and pain.
- Steroid Injections: Corticosteroid injections directly into the affected area of the spine can provide targeted relief by reducing inflammation around the compressed nerve.
- Neuropathic Pain Medications: If you experience neuropathic pain (nerve pain), medications such as gabapentin (Neurontin) or pregabalin (Lyrica) may be prescribed to help alleviate this type of pain.
- Topical Analgesics: creams, gels, or patches that include drugs such as lidocaine or capsaicin that can be applied directly to the painful spot to offer localized pain relief.
- Opioid Pain Medications: These are generally reserved for severe cases of pain that are not adequately managed with other medications, and their use is carefully monitored due to the risk of dependence and side effects.
Physiotherapy Management
Pain Management:
- Modalities such as heat therapy, cold therapy, ultrasound, or electrical stimulation may be used initially to help reduce pain and inflammation.
- Manual therapy techniques, including soft tissue mobilization and massage, can also help alleviate muscle tension and discomfort.
- This technique involves gently stretching the neck to relieve pressure on the spinal discs and nerves. It can be done manually by a physical therapist or using mechanical devices.
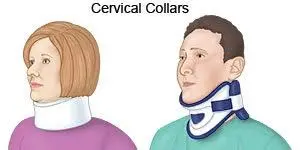
Soft cervical collar.
- This is a cushioned ring that fits around the neck and is held in place by Velcro. Your doctor may recommend that you wear a soft cervical collar to relax the muscles in your neck and minimize neck mobility. This can assist reduce the pinching of the nerve roots that occurs while moving the neck. A soft collar should only be worn for a short period since extended use might weaken the neck muscles.
Physical therapy. Neck Range of Motion Exercises:
- Neck Flexion and Extension: Gently lower your chin towards your chest for flexion and then tilt your head back for the extension.
- Neck Side Bending: Tilt your head sideways towards each shoulder to stretch the neck muscles.
- Neck Rotation: Turn your head to the right and left, trying to look over each shoulder.
- Strengthening the muscles around the neck, shoulders, and upper back can help provide support to the spine and reduce strain on the nerves. Examples include:
- Neck Retraction: Gently pull your head backward as if making a double chin, then relax.
- Shoulder Blade Squeezes: Sit or stand with your arms at your sides, then squeeze your shoulder blades together.
- Scapular Stabilization Exercises: These target the muscles that stabilize the shoulder blades and upper back.
Postural Correction:
- Improving posture can help alleviate stress on the cervical spine. Your physical therapist may teach you proper sitting, standing, and sleeping positions.
- Techniques such as massage, mobilization, and manipulation may be used by the physical therapist to reduce muscle tension, improve joint mobility, and relieve pain.
Modalities:
- Your physical therapist may use modalities such as
- heat therapy,
- cold therapy,
- ultrasound,
- traction
- Electrical stimulation, Transcutaneous Electrical Nerve Stimulation (TENS), and Interferential Current Therapy (IFT) to reduce pain and inflammation.
Education and Ergonomic Training:
- Learning about ergonomic principles and how to modify daily activities to reduce strain on the neck can be beneficial. This includes adjusting workstation setups, using proper lifting techniques, and taking frequent breaks from prolonged sitting or computer use.
Functional Training:
- Your physical therapist may incorporate functional activities and exercises that mimic your daily tasks to improve overall function and movement patterns.
Surgical Management
Surgical procedures for cervical radiculopathy are considered when conservative treatments such as medication, physical therapy, and injections fail to relieve symptoms or when there is a progressive neurological deficit. The goals of surgery are to decompress the affected nerve roots, stabilize the cervical spine if necessary, and improve overall function. Here are the common surgical procedures for cervical radiculopathy:
Anterior Cervical Discectomy and Fusion (ACDF):
- Procedure: In ACDF, the surgeon makes an incision in the front of the neck (anterior approach) and removes the damaged or herniated disc that is compressing the nerve root. The space left by the disc removal may be filled with a bone graft or a metal cage, and the adjacent vertebrae are fused using plates and screws.
- Indications: ACDF is often recommended for cervical radiculopathy caused by disc herniation, degenerative disc disease, or spinal cord compression due to bone spurs (osteophytes).
Posterior Cervical Foraminotomy:
- Procedure: This procedure is performed through a small incision in the back of the neck (posterior approach). The surgeon removes a portion of the bone and soft tissue to widen the neural foramen, the opening through which the nerve root exits the spinal canal. This takes away pressure on the nerve roots.
- Indications: Posterior cervical foraminotomy is suitable for cases where the nerve root compression is primarily caused by foraminal stenosis or bone spurs.
Cervical Laminectomy:
- Procedure: In a laminectomy, the surgeon removes part of the lamina (the bony arch at the back of the vertebra) to create more space in the spinal canal and decompress the nerve roots. This procedure is typically done through a posterior approach.
- Indications: Cervical laminectomy is used for cases of severe spinal cord compression or multiple levels of nerve root compression.
Artificial Disc Replacement (ADR):
- Procedure: ADR involves removing the damaged disc and replacing it with an artificial disc implant. This procedure aims to maintain motion at the affected spinal segment while decompressing the nerve root.
- Indications: ADR may be considered for select patients with cervical radiculopathy who desire preservation of neck motion and have specific criteria for disc replacement.
Cervical Corpectomy and Fusion:
- Procedure: In cases of significant spinal cord compression or multi-level disc disease, a corpectomy may be performed. This involves removing a portion of the vertebral body along with the discs above and below it. The remaining vertebrae are fused to stabilize the spine.
- Indications: Cervical corpectomy is indicated when there is severe compression of the spinal cord or nerve roots due to disc herniation, bone spurs, or other structural abnormalities.
Do’s & Don’ts
Do’s
- Do follow your doctor’s advice: Always adhere to your healthcare provider’s recommendations for treatment, medication, and physical therapy.
- Do gentle exercises: Engage in gentle stretching and strengthening exercises prescribed by your healthcare provider or a physical therapist. These exercises may help you gain flexibility and relieve discomfort.
- Do wear a cervical collar: A cervical collar will support your neck muscle and limit the motion in the cervical region which decreases the pain and inflammation around the neck.
- Do maintain good posture: Keep your neck and spine aligned properly while sitting, standing, and sleeping. Use ergonomic furniture and pillows if needed.
- Do use heat or cold therapy: Applying heat or cold packs can help alleviate pain and reduce inflammation. Follow the recommended duration and frequency for these therapies.
- Do practice relaxation techniques: Stress can exacerbate pain, so try relaxation techniques such as deep breathing, meditation, or yoga to manage stress and promote overall well-being.
Don’ts:
- Don’t ignore symptoms: If you experience worsening pain, numbness, weakness, or other concerning symptoms, don’t ignore them. Contact your healthcare provider promptly.
- Don’t engage in high-impact activities: Avoid activities that put strain on your neck and spine, such as heavy lifting, sudden twisting motions, or contact sports.
- Don’t rely solely on medication: While medication can help manage pain, it should be used in conjunction with other treatment modalities such as physical therapy and lifestyle modifications.
- Don’t smoke: Smoking can impair blood flow and hinder healing. Consider restricting or dropping your smoking habits.
FAQ
What makes radiculopathy worse?
pain, sensation is the most frequent symptom, which is typically a sharp, shooting sensation along the nerve. It might range from a minor discomfort to a severe, heat sensation or severe pain. Sometimes it feels like something shaking or an electric shock. Coughing or sneezing may worsen symptoms, as may prolonged sitting.
How to prevent radiculopathy?
While radiculopathy cannot always be avoided, remaining physically active and maintaining a healthy weight may lower your chance of developing it. Practicing proper posture while sitting, playing sports, exercising, or moving heavy things is also critical for avoiding accidents.
How can I sleep with radiculopathy?
Sleeping on the stomach is not recommended for persons suffering from radiculopathy since it forces them to rotate their necks to rest against the pillow. For people who like to sleep on their stomachs, the ideal option is to use thin pillows or none at all.
How can I fix cervical radiculopathy at home?
You may also perform a few easy things at home to help ease the symptoms of cervical radiculopathy:
Apply hot or cold compresses to minimize swelling.
mild stretching (but check with your doctor)
rest.
Sleep with a customized pillow to keep your neck in position at night.
References
- Professional, C. C. M. (n.d.-d). Cervical radiculopathy (Pinched nerve). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22639-cervical-radiculopathy-pinched-nerve
- Meyler, Z., DO. (n.d.). What is cervical radiculopathy? Spine-health. https://www.spine-health.com/conditions/neck-pain/what-cervical-radiculopathy
- Cervical radiculopathy (Pinched nerve) – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/cervical-radiculopathy-pinched-nerve/
- Cervical radiculopathy. (n.d.). Physiopedia. https://www.physio-pedia.com/Cervical_Radiculopathy
- Cervical radiculopathy. (2022, September 20). WebMD. https://www.webmd.com/pain-management/pain-management-cervical-radiculopathy
- Craig Forsthoefel Illinois Bone & Joint Institute. (n.d.). Cervical radiculopathy – spine – orthobullets. https://www.orthobullets.com/spine/2030/cervical-radiculopathy
- Veritas Health,. (n.d.). Cervical Radiculopathy Interactive Video. Spine-health. https://www.spine-health.com/video/cervical-radiculopathy-interactive-video
- Woods, B. I., & Hilibrand, A. S. (2015). Cervical radiculopathy. Journal of Spinal Disorders & Techniques, 28(5), E251–E259. https://doi.org/10.1097/bsd.0000000000000284
- Complete Physio. (2023, November 21). Cervical Radiculopathy | Complete physio. https://complete-physio.co.uk/cervical-radiculopathy/
- UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-cervical-radiculopathy






3 Comments