Introduction
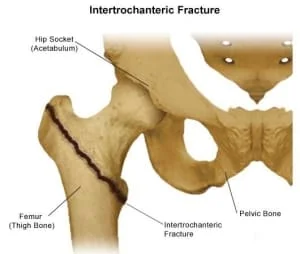
Intertrochanteric fractures are those that occur between the greater and lesser trochanters of the proximal femur outside the capsule. The dense trabecular bone that makes up the intertrochanteric portion of the femur is situated between the greater and lesser trochanters.
The greater trochanter is where the gluteus medius, gluteus minimus, obturator internus, and piriformis insert, as well as where the vastus lateralis originates. The lesser trochanter acts as an insertion point for the iliacus and psoas major, known as the iliopsoas.
The calcar femoral is a solid bone wall that runs vertically from the femur shaft’s posteromedial part to the femoral neck’s posterior region. This structure is critical because it determines whether a fracture is stable. The wide metaphyseal region has a more abundant blood supply, resulting in a higher union rate and less osteonecrosis than femoral neck fractures.
Anatomy
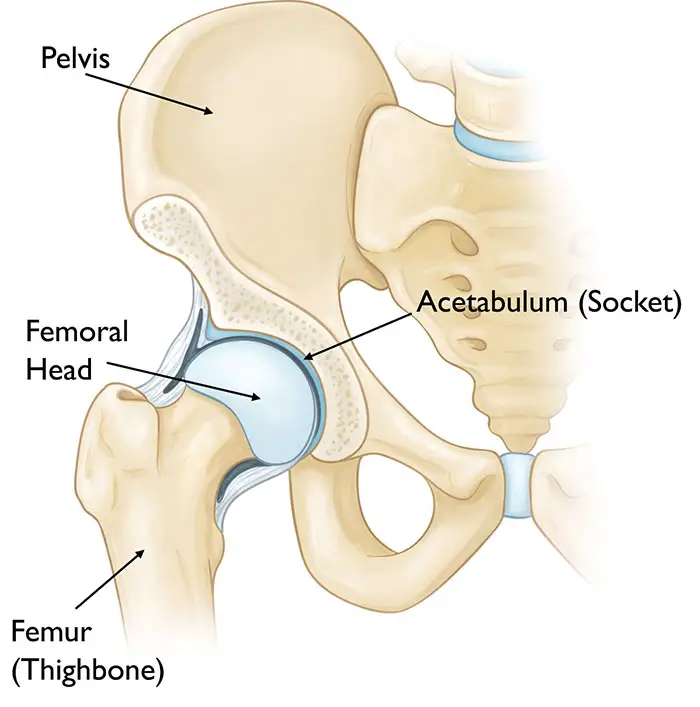
A ball-and-socket joint makes up the hip. The top portion of the thighbone, or the head of the femur, is the ball. The acetabulum is the name of the socket. The acetabulum is one part of the pelvic bone. The femoral head is accommodated by its rounded contour.
Hip Capsule
The transverse acetabular ligament and the acetabulum’s edge are where the hip capsule is proximally joined. Distally, to the femoral neck (1/2 inch from the trochanteric crest), to the bases of the greater and lesser trochanters, and to the intertrochanteric line. There are the retinal vessels, which are important for the blood supply to the femoral head.
Blood Supply
The femoral head collects blood from three different areas:
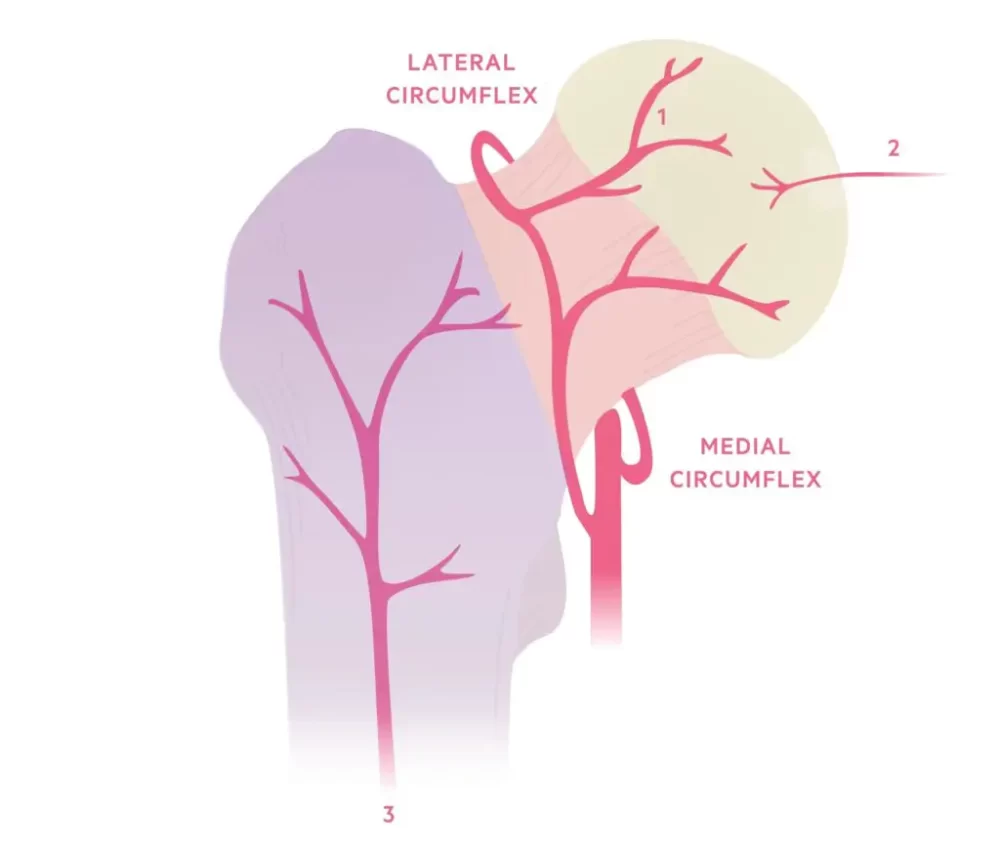
- The primary blood supply is the retinal vessels. is the result of an extra-capsular arterial ring that is reinforced by the superior and inferior gluteal arteries of the internal iliac arteries and supplied by the medial and lateral circumflex vessels (profundal femoris A).
- One minor source is the foveal artery. gives the epiphysis a small amount of blood during the skeleton’s growth. thought to vanish as an adult (ligamentum teres).
- Metaphyseal vessels: not a significant supply. After skeletal maturity, the femoral head receives blood flow from metaphysical arteries.
Epidemiology of Intertrochanteric Fractures
Incidence is increasing as the proportion of the older population in various nations rises 4. Femoral neck and intertrochanteric fractures are about equally common in people aged 65 to 99.
Causes of Intertrochanteric Fractures
Those 65 years of age and older are most likely to suffer these fractures, which are typically the result of falls. Your bones naturally weaken and degrade with age, even from small falls. Hip fractures in children and young adults are primarily caused by sports-related injuries, automobile collisions, and bicycle accidents.
Other things that can shatter your hip consist of:
- Being born as a female.
- Your genetic makeup: are you tall or slim, and do you have any ancestors who experienced fractures later in life?
- You’re not receiving enough calcium and vitamin D to maintain strong bones.
- Staying inactive. Walking and other weight-bearing workouts keep bones robust.
- Smoking history.
- Osteoarthritis, for example, might prevent smooth and safe movement, as can diseases that cause vertigo or balance problems.
- Taking some drugs, such as long-term steroid treatments for COPD or asthma.
Risk Factors of Intertrochanteric Fractures
Age and Sex
As people age, their bone density and muscle mass decline. In addition to eyesight and balance concerns, older persons may have a higher risk of falling.
Intertrochanteric Fractures occur approximately three times more frequently in women than in males. Because menopause reduces estrogen levels, which accelerates bone loss, women lose bone density faster than males. However, men can also have dangerously poor bone density.
Medical conditions
The following conditions:
- Osteoporosis: Bones weakened by this condition are more likely to break.
Thyroid issues. An overactive thyroid may cause fragile bones. - Intestinal problems: Conditions that limit vitamin D and calcium absorption can also lead to weaker bones.
- Problems with balance: Peripheral neuropathy, Parkinson’s disease, and stroke can all increase the risk of falling. Low blood pressure and blood sugar levels may increase the risk of falling.
Medications
Long-term usage of corticosteroid drugs, such as prednisone, can damage bones. Some drugs, whether alone or in combination, can cause dizziness, increasing the risk of falling. Sedatives, antipsychotics, and sleep aids are the medicines most commonly associated with falls.
Nutritional Problems
When young people do not consume enough calcium and vitamin D, their peak bone mass decreases and their risk of fractures increases later in life. To preserve bone density as you age, it’s also important to eat enough calcium and vitamin D. Underweight people are also more likely to lose bone mass.
Lifestyle Choices
Lack of regular weight-bearing activity, such as walking, weakens bones and muscles, increasing the risk of fractures and falls.
Alcohol and tobacco can hinder the normal mechanisms that form and maintain bone, resulting in bone loss.
Symptoms of Intertrochanteric Fractures
Intertrochanteric fracture symptoms typically appear suddenly. They may, however, begin gradually and intensify with time. Hip fracture symptoms include:
- Pain: Hip pain is typically strong and intense. However, it can be achy or mild. The majority of persons report pain in their groin, pelvis, outer hip, and thigh. Sciatica can cause discomfort that spreads from your buttocks to your legs. You can also have knee pain.
- Limited mobility: Most hip fracture patients are unable to walk or stand. Walking may be possible at times, but bearing weight on one leg produces agonizing pain.
- Physical changes: You may have a bruised hip. You can have a leg that appears shorter than the other. The hip may appear out of position, twisted, or rotated.
Diagnosis of Intertrochanteric Fractures
Physical Examination
A physician examines your hip and pelvis to assess discomfort, bruising, and swelling. He or she inquires about the location and severity of your pain. Your doctor will promptly diagnose an open fracture (a fracture in which a bone protrudes through the skin) and, in most cases, perform surgery right away.
Radiography
Radiography involves X-ray images. Use electromagnetic radiation to identify a fractured bone in the hip or pelvis. They also let your doctor determine whether a bone has many fractures and whether any of the fractured bone parts have been relocated.
CT Scans
Your doctor may order a CT scan to look into a potential fracture pattern or to establish the extent of hip joint injury. A CT scan uses X-rays and a computer to create two- and three-dimensional images of the hip and pelvic bones, allowing medical personnel to see a fracture from various angles. Small bone fragments that could become stuck in the hip joint and require surgical removal may also be discovered during this examination.
After reassembling a shattered bone, clinicians use CT scans to ensure that the pieces fit properly.
MRI Scans
Your doctor may recommend an MRI if they feel you have a stress fracture in your hip or pelvis that is not evident on an X-ray, or if your symptoms indicate further damage to your blood vessels, ligaments, tendons, or nerves. This test uses radio waves and a magnetic field to create digital, three-dimensional pictures of the soft tissues surrounding the joint.
An MRI may reveal strained or torn tendons, ligaments, or a bone fragment pressing on a nerve. If an X-ray reveals no signs of trauma but your symptoms suggest a fracture, doctors may order an MRI.
An MRI may be recommended if your doctor suspects a stress fracture in your hip or pelvis, or if your symptoms indicate additional damage to your blood vessels, ligaments, tendons, or nerves. This test creates computerized, three-dimensional images of the soft tissues surrounding the joint using radio waves and a magnetic field. An MRI may reveal strained or torn tendons, ligaments, or a bone fragment pressing against a nerve.
Bone Scans
If you experience pain and swelling from a fracture but cannot get an MRI owing to an implanted pacemaker or other medical devices, your doctor may recommend a bone scan.
A technician will inject a small amount of dye into a vein in your arm to perform this test. This dye, known as a tracer, travels through the bloodstream and collects in locations where your tissues and cells are healing.
A radiologist uses a specialized camera to photograph the tracer while scanning your body after it has been in your bloodstream for one or two hours. A fracture may occur if it gathers more in some parts of the hip or pelvis than in others.
Treatment of Intertrochanteric Fractures
The goal of conservative treatment is to alleviate hip pain symptoms. When compared to surgical treatment, functional outcomes are frequently not significantly different.
Intertrochanteric fracture treatment typically includes surgery, rehabilitation, and medication.
In most other cases, surgery will be required to repair the shattered hip. For an aged patient who is functionally healthy, doctors will most likely recommend surgery to speed up healing and recovery. Intertrochanteric fractures are often treated with surgery, medicine, and post-surgical rehabilitation.
Medical treatment of Intertrochanteric Fractures
Up to 10% of persons 65 and older who have had a hip fracture will have another one within two years. Bisphosphonates and other osteoporosis treatments may help lower the risk of a subsequent Intertrochanteric fracture. To avoid side effects that may make oral bisphosphonates difficult to tolerate, your doctor may consider intravenous (IV) administration.
Bisphosphonates are generally not suggested for those who have kidney issues. Long-term bisphosphonate therapy may occasionally result in jaw pain and swelling, eyesight issues, or an unusual Intertrochanteric fracture.
Rehabilitation of Intertrochanteric Fractures
Your care staff will most likely get you out of bed and moving on the first day following surgery. Physical therapy will first concentrate on range-of-motion and strength exercises. Depending on the sort of surgery you had and whether you have help at home, you may need to transition from the hospital to an extended care facility.
In extended care and at home, you may work with an occupational therapist to master daily independent skills such as toileting, bathing, dressing, and cooking. Your occupational therapist will assess whether a walker or wheelchair can help you regain mobility and independence.
Nonsurgical Treatment of Intertrochanteric Fractures
Perhaps you do not need surgery for your shattered hip. If you’ve had a fracture for a while and only saw your doctor when it started to mend, you won’t need surgery. Nonetheless, it is not advisable to disregard a hip fracture. It could lead to severe and long-term impairment.
Furthermore, some individuals may decline to have surgery. This is the role of conservative therapy. These include specific treatments and technologies that help to alleviate pain or discomfort while also preventing further harm.
Assistive devices
Take it easy for at least six weeks after sustaining a hip fracture. Until it recovers, you should avoid strenuous activity and bearing weight on the injured hip.
This does not indicate that you have to stay in bed all day. Moving around would help to prevent deep vein thrombosis and blood clots caused by immobility. You can get around for the time being using assistive devices such as a walker, crutches, or a cane. These technologies allow you to move around without straining your hips.
Electronic and Ultrasonic Bone Stimulation
Bone stimulation is used to treat newly fractured, nonunion, or improperly fused bones. A device can provide extracorporeal shock waves, low-intensity ultrasound, or a low-electric current to your bones. It is said to speed up the healing process for hip fractures.
Despite the promise of pain relief and improved function, a study of the experiment found no significant benefits for bone repair. Further research is required to confirm the effectiveness of this medication.
There are no known negative effects from bone stimulators. Doctors advise against the treatment for youngsters and pregnant women, citing the need for more clinical research to demonstrate bone stimulation’s safety and effectiveness in these populations.
Physical therapy (PT)
Before and after surgery, your doctor may prescribe that you consult a physical therapist. Exercise helps your broken bone repair faster by feeding it with nutrients and oxygenated blood.
Your doctor and physical therapist may periodically recommend bed rest in conjunction with weight-bearing activities. Your physical therapist can teach you how to perform basic range of motion and stretching exercises.
There are three ways you can benefit from physical therapy. It prevents the muscles from deteriorating in the first place. It also increases your flexibility. Third, it increases your range of motion. Your condition will dictate the duration and frequency of your physical therapy sessions. A physical therapist can help your hip fracture heal and maintain muscle strength.
Traction
Your surgeon can use pulleys and weights to stretch the muscles around your shattered hip. When you are in the hospital, they are fitted and secured to your leg. Traction keeps your muscles in position while the fracture heals. This type of non-surgical fracture treatment is useful in certain situations, such as intertrochanteric fractures.
Surgical Treatment of Intertrochanteric Fractures
The type of surgery you have is generally determined by the position and severity of the fracture if the shattered bones are improperly aligned (displaced fracture), your age, and any underlying health concerns. Options include:
Internal repair with screws: Metal screws are put into the bone to keep it together when the fracture heals. Sometimes screws are fastened to a metal plate that runs down the femur.
Total hip replacement: Prostheses replace your upper femur and pelvic socket. Total hip replacement is becoming more cost-effective and associated with better long-term outcomes in otherwise healthy persons who live independently. Total hip replacement is the preferred method for treating hip fractures in otherwise healthy, self-sufficient people.
Partial hip replacement: If the ends of the shattered bone are dislocated or damaged, your surgeon may remove the femur’s head and neck and replace it with a metal prosthesis. Adults with various health issues or cognitive impairment, as well as those who can no longer live independently, may benefit from partial hip replacement.
If the blood supply to the ball of your hip joint was compromised during the fracture, your doctor may propose a partial or total hip replacement. This type of injury, which is most common in older adults with femoral neck fractures, makes the bone less likely to mend properly.
Physiotherapy Treatment
Rehabilitation begins quickly.
Two to three days post-operative
- Instruct the patient in deep breathing and coughing. Goal: Avoid postoperative pneumonia and atelectasis.
- Start isometrics and ankle pumps with the involved extremity. Goal: Prepare the patient for an active exercise program.
- Begin bedside sitting after the physician has cleared the patient for this activity. Goal: Prepare the patient to begin the transfer and progressive gait training programs.
Three to five days postoperative
- Gait train the patient while using weight-bearing precautions. Transition to a walker or crutches. Goal: Develop an independent gait using an assistance device, employing the optimal gait pattern on all surfaces and stairs.
- Begin training in activities of daily life, such as bed mobility and transfers to and from the toilet. Goal: Achieve independence in all transfers.
- Start an active range of motion/strengthening program. Individualize workout plans based on each patient’s needs, but generally include the following. Goals: Increase the strength of the concerned extremity and increase independence through an exercise program. Supine: hip abduction and adduction, gluteal and quadriceps sets, straight leg raise, hip and knee flexion, short arc quadriceps, and internal and external rotation. Sitting: Long-arc quadriceps, hip flexion, and ankle pumping
- When internal fixation is performed, partial weight-bearing is recommended for 8-10 weeks (based on radiological examination of fracture healing), with full weight-bearing allowed after 3 months.
- Following the surgeon’s instructions, the patient can begin strengthening activities.
- Patients should also receive balance and proprioceptive rehabilitation, as these abilities quickly deteriorate with inactivity. Balance and fall prevention classes should be considered.
Weight-bearing exercises are essential for mobility, balance, everyday activities, and quality of life. Examples include stepping in different directions, standing up and sitting down, tapping the foot, and stepping onto and off a block.
Patients who undergo a prosthetic replacement must avoid the following for roughly 12 weeks.
- Hip flexion > 70-90°
- External rotation of the leg
- Adduction of the leg from the midline
- Should not bend forward from the waist by more than 90°.
Post-Operative Treatment
Post-operative evaluation
Two to three days post-operative
- Evaluate gross muscular strength and range of motion in the other extremities.
- Assess the gross muscular strength of the affected extremity using isometric muscle contractions.
- Evaluate the feeling of the concerned extremity.
- Evaluate the range of motion of the affected hip within the limits of pain.
Three to five days postoperative
- Assess gait pattern using an assistive device.
- Assess functional abilities concerning transfers and bed mobility.
- Continue to assess the gross strength of the afflicted extremity.
Outpatient assessment
- Perform particular muscle testing on each group.
- Range of motion tests for the hip, knee, and ankle.
- Analyze the gait.
- Evaluate functional ability.
- Complete particular assessments, such as the Functional Ambulation Profile and the GetUp and Go Test.
Precautions during evaluation
- The physician must determine the weight-bearing status.
- Determine cardiac status before beginning the evaluation.
Complication
An Intertrochanteric fracture can cause major consequences. Veins can clog with blood, most commonly in the legs. A clot could fracture and end up in a blood artery in your lung. A pulmonary embolism, as this obstruction is termed, is potentially fatal.
Additional difficulties may include:
- Pneumonia
- Muscle atrophy (the loss of muscle tissue)
- Postoperative infection
- Nonunion or incorrect union of your bone
- Mental impairment following surgery in elderly patients
- Bed sores from sitting still and moving very little.
Prevention
- Eating correctly: Calcium and vitamin D-rich diets aid in strengthening bones.
- Getting routine checkups: See your doctor about bone density tests to detect osteoporosis signs. Your doctor may recommend bisphosphonates, a medication that strengthens and slows bone loss.
- To avoid accidents, remove any potential fall hazards from your home, such as throw rugs. Exercise caution when using stairs or walking on icy surfaces. If you have Parkinson’s disease, talk to your doctor about how to keep your body healthy and prevent falls.
- Maintaining health: Avoid smoking, control your weight, and limit your alcohol consumption.
FAQs
Can you walk with an intertrochanteric fracture?
Sciatica can cause pain to spread down your buttocks and into your leg. You may also get pain in your knee. Most persons with hip fractures are unable to stand or walk. Walking is sometimes doable, but putting weight on the leg causes excruciating pain.
How do you fix an intertrochanteric fracture?
The majority of these fractures are treated surgically with a sliding hip screw or an intramedullary hip screw, with arthroplasty being an uncommon choice. Indications for the sliding hip screw include stable fracture patterns and an undamaged lateral wall.
Can intertrochanteric fractures heal without surgery?
Only a small percentage of adult fractured hips require surgery. Isolated greater trochanteric hip fractures are treatable without surgery. When patients are critically ill and have displaced, unstable hip fractures, their families frequently question whether surgery is necessary at all.
What is the goal of treatment for intertrochanteric fracture?
The goal of treating any Intertrochanteric (IT) fracture is to recover early mobility, reducing the risk of medical problems and returning the patient to a pre-operative position.
How long does an intertrochanteric fracture take to heal?
Most people can return to work 4 weeks to 4 months after surgery. However, it may take six months to a year for you to fully recover.
REFERENCES
- Attum, B. (2023, August 8). Intertrochanteric Femur Fracture. StatPearls: NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK493161/#:~:text=Introduction,composed%20of%20dense%20trabecular%20bone.
- Karadsheh, M. (n.d.). Intertrochanteric Fractures, Trauma and Orthobullets: https://www.orthobullets.com/trauma/1038/intertrochanteric-fractures
- Intertrochanteric Fracture. (n.d.). Orthopaedic Trauma Association (OTA). https://ota.org/for-patients/find-info-body-part/3720#/+/0/score,date_na_dt/desc/
- Bandoim, L. (2017, August 3). Intertrochanteric Fractures. Healthline. https://www.healthline.com/health/intertrochanteric-fracture
- Intertrochanteric Fractures | Dr. Roshan Melvani, Dual Fellowship-Trained Orthopaedic Surgeon, Shoulder and Elbow Specialist, Victorville, CA. (n.d.). https://www.drmelvani.com/intertrochanteric-fractures-orthopaedic-surgeon-victorville-ca/
- S. (2019, September 5). Hip Fractures: Intertrochanteric, Subtrochanteric, and Femoral Neck. Louisville Orthopaedic Clinic. https://www.louortho.com/blog/hip-fractures-intertrochanteric-subtrochanteric-and-femoral-neck/