Vagus Nerve
Introduction
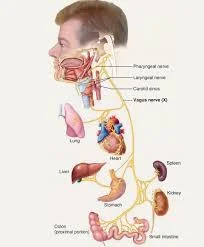
The vagus nerve, also known as the 10th cranial nerve or CN X, is one of the longest and most complex nerves in the human body. It starts in the brainstem, travels through the neck, chest, and abdomen, and branches out to the heart, lungs, digestive tract, and even the tongue and ears.
The longest cranial nerve in the body, the vagus nerve (cranial nerve [CN] X), performs both efferent and afferent motor and sensory functions. The vagus nerve has several clinical correlations because of its widespread distribution throughout the body.
The vagus nerve is the body’s superhighway, carrying information between the brain and the internal organs while also controlling the body’s response during relaxation. The massive nerve starts in the brain and extends to the neck and torso in many different directions. It transfers sensory data from the ear’s skin, regulates the muscles involved in speaking and swallowing, and affects your immune system.
Anatomical Course of the vagus nerve
The vagus nerve is the longest of all the cranial nerves, running from the head to the abdomen. The Latin word “vagary,” which means “wandering,” is the source of its name. Sometimes, it’s referred to as the wandering nerve.
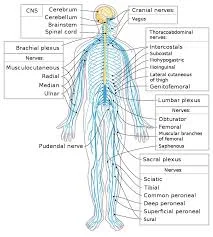
In the Head
The vagus nerve emerges from the medulla of the brainstem. It exits the cranium through the jugular foramen alongside the glossopharyngeal and accessory nerves (CN IX and XI, respectively).
The auricular branch emerges from within the skull. This provides sensation to the posterior portion of the external auditory canal and external ear.
In the Neck
The vagus nerve passes inferiorly beside the internal jugular vein and common carotid artery after entering the carotid sheath of the neck. At the base of the neck, the right and left nerves have distinct pathways:
The subclavian artery and the sternoclavicular joint are the two points on the thorax where the right vagus nerve enters.
The left vagus nerve enters the thorax inferiorly between the left common carotid and left subclavian arteries, just behind the sternoclavicular joint.
Several branches emerge in the neck:
- The pharyngeal branches provide motor innervation to the majority of the pharyngeal and soft palate muscles.
- The superior laryngeal nerve bifurcates into its internal and external branches. The cricothyroid muscle is innervated by the external laryngeal nerve. The internal laryngeal nerve supplies sensory innervation to the laryngopharynx and superior part of the larynx.
- Right recurrent laryngeal nerve – Hooks underneath the right subclavian artery and ascends to the larynx. It innervates the vast majority of the larynx’s intrinsic muscles.
In the thorax
In the thorax, the right vagus nerve forms the posterior vagal trunk, while the left forms the anterior vagal trunk. Branches from the vagal trunks help to form the oesophageal plexus, which innervates the oesophagus’ smooth muscles.
Two other branches emerge in the thorax:
- Most of the laryngeal intrinsic muscles are innervated by the left recurrent laryngeal nerve, which ascends after hooking beneath the aortic arch.
- Cardiac branches give the heart a visceral sensation and regulate heart rate.
- The vagal trunks enter the abdomen through an opening in the diaphragm called the oesophageal hiatus.
In the abdomen.
The vagal trunks in the abdomen divide into branches that supply the oesophagus, stomach, and small and large bowels (up to the splenic flexure).
Functions of Vagus Nerve
The vagus nerve has a very wide distribution.
Sensory: innervates laryngopharynx and larynx inner surfaces, and the skin of the external acoustic meatus. gives the heart and the viscera of the abdomen a visceral sensation.
Special Sensory: Gives taste sensation to the epiglottis and root of the tongue.
Motor: Innervates the majority of pharyngeal, soft palate, and laryngeal muscles.
Parasympathetic: Controls heart rhythm and innervates smooth muscle in the trachea, bronchi, and gastrointestinal tract. Its cardiac branches slow the heartbeat; its bronchial branches constrict the bronchi; and its oesophagal branches regulate involuntary muscles in the oesophagus, stomach, gallbladder, pancreas, and small intestine, stimulating peristalsis and gastrointestinal secretions.
Embryology
The pharyngeal and laryngeal muscles, laryngeal cartilages, aortic arch, and subclavian arteries are all developed by the vagus nerve, which arises from the fourth branchial arch.
Blood Supply and Lymphatic
The middle meningeal artery provides intracranial blood supply to the vagus nerve. The extracranial blood supply is provided by the common carotid artery, internal carotid artery, inferior thyroid artery, external carotid artery, posterior meningeal artery, internal thoracic arteries, bronchial arteries, and oesophagal arteries.
The vagal system regulates the contraction of lymphatic cells (which contain actin).
Nerves
The pharyngeal, superior laryngeal, recurrent laryngeal, and superior cardiac nerves are among the vagus nerve’s branches in the neck. The structure and function of these nerves have been described previously.
Muscles of the vagus nerve
The vagus nerve contains several fibres that innervate the striated muscles of the larynx and pharynx, with two exceptions: the stylopharyngeus muscle (CNIX) and the tensor veli palatini muscle (V3).
- The vagus nerve innervates the palatoglossus muscle, which elevates the posterior portion of the tongue.
- The cricothyroid muscle is supplied by the superior laryngeal nerve’s external branch.
- The vagus has pharyngeal branches that supply the levator veli palatini, salpingopharyngeus, palatopharyngeus, and uvula.
- The intrinsic muscles of the larynx are innervated by recurrent laryngeal nerves, except for the cricothyroid muscle.
Vagus Nerve Testing
- A physician may use the gag reflex to test the vagus nerve. During this part of the exam, the doctor may use a soft cotton swab to tickle the back of the throat on both sides. This should cause the individual to gag.
- If the patient does not gag, there might be a vagus nerve issue, which might point to a brain stem function issue.
- According to recent research, physicians may also assess vagal nerve function when diagnosing cardiovascular disease. Damage to the vagal nerve can cause problems with the cardiovascular system.
- Measuring heart rate, blood pressure, and cardiovascular response to exercise can reveal information about how your vagal nerve interacts with your cardiovascular system, a process known as cardiovagal tone. It can provide clues about your cardiovascular health.
Conditions Affect the Vagus Nerve
Your vagus nerve is responsible for many bodily functions, so its malfunction can result in a variety of conditions. Scientists are still investigating how it may impact mental health, chronic headaches, and even Alzheimer’s.
Other related conditions are:
Gastroparesis. As a result of this condition, food cannot pass through your digestive system. A compromised vagus nerve as a consequence of diabetes, surgery, infection, or an autoimmune disease can result in gastroparesis in certain cases.
Vasovagal syncope. If you have this condition, you are more likely to faint in hot weather, when you are hungry or anxious, or under other stressful conditions. The vagus nerve overreacts to these situations, causing your blood pressure to drop dramatically, making you dizzy, or causing a fainting spell.
Vagus nerve pathology
The autonomic nervous system (ANS)’s sympathetic and parasympathetic components control and regulate the function of various organs, glands, and involuntary muscles throughout the body (for example, vocalisation, swallowing, heart rate, respiration, gastric secretion, and intestinal motility).
As a result, aside from vocalisation, the majority of the signs and symptoms of vagus nerve dysfunction are ambiguous and nonspecific. Laryngeal nerve palsy causes paralysis of the ipsilateral vocal cord and is used to diagnose diseases affecting the vagus nerve from its origin to the end of its branch of the laryngeal nerve.
Sensory neuropathy.
Refractory or idiopathic cough results from vagal afferent nerve hypersensitivity.
Arnold’s nerve ear-cough reflex, while uncommon, is a symptom of vagal sensory neuropathy and is the cause of a refractory chronic cough that can be treated with gabapentin. Mechanical stimulation of the external auditory meatus causes coughing, which is accompanied by other neuropathic features such as throat irritation (laryngeal paresthesia) and coughing in response to nontussive triggers such as cold air and eating (allotussia). These characteristics suggest that the cough has a neuropathic origin.
Motor neuropathy.
Pathology of the vagus nerve proximal to the laryngeal nerve is typically characterised by hoarseness of voice and paralysis of the vocal cords. Although idiopathic vocal cord palsy accounts for the majority of these, tumours, particularly lung cancers, are the next most common cause. The most common oncological causes of vocal cord palsy are tumours in the right lung’s apex and the left lung’s hilum. Thyroid and proximal oesophagal cancers are less common causes of vocal cord palsy.
Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) is a procedure that involves inserting a device into the body to stimulate the nerve with electrical impulses. It is used to treat certain types of epilepsy and depression that do not respond to other medications.
Experts believe the vagus nerve may be linked to depression, metabolic disease, and heart disease. If research confirms this, researchers believe VNS could help with a variety of health issues.
Usually positioned under the skin of the chest, the device is attached to the left vagus nerve by a wire. When the gadget is turned on, signals are sent to your brainstem via the vagus nerve and then to your brain.
A neurologist usually programmes the device, but people are often given a handheld magnet that they can use to control the device themselves.
In the future, VNS may be used to treat a variety of other illnesses, such as cluster headaches, Alzheimer’s disease, posterior autoimmune uveitis, and multiple sclerosis.
Symptoms of vagus nerve
Symptoms of vagus nerve conditions vary depending on the cause and affected part of the nerve.
You might experience:
- Stomach pain and bloating.
- Acid reflux (GERD).
- Variations in heart rate, blood pressure, or blood sugar.
- Swallowing problems or a loss of gag reflex.
- Feeling dizzy or faint.
- Loss of voice, wheezing, or hoarseness.
- Loss of appetite, sudden feeling full, or unexplained weight loss.
- Nausea and vomiting.
Diagnosis
If you have a vagal nerve disorder, your doctor might prescribe one of the following tests:
- CT scan or MRI to detect intestinal blockages.
- The echocardiogram is a tool used to evaluate heart health.
- Gastric emptying solid study or smart pill (a swallowable electronic gadget) to measure the amount of time food takes to move from your stomach into your intestines.
- An examination of the upper digestive tract is done through an upper endoscopy procedure.
Treatment
Treatment options for gastroparesis include:
Dietary changes.
Medicines to relieve nausea and abdominal pain, control blood sugar, and improve stomach emptying.
Feeding tubes are used to deliver nutrition to the bloodstream.
Gastrostomy is a procedure that creates an opening in your stomach to relieve pressure.
Similar to VNS, gastric electrical stimulation stimulates the muscles and nerves in the stomach to move food through the intestines.
Treatment options for vasovagal syncope include:
Consuming a salt-rich diet.
Stop taking blood pressure-lowering medications, such as diuretics.
taking drugs to increase blood pressure, sodium, and fluid levels or to reduce nervous system reactions.
Put on compression stockings to keep your legs from becoming swollen with blood.
Prevention of vagus nerve
Many of the same precautions you would take for general health also apply to maintaining the health of your vagus nerve. Consume a diet rich in fresh fruits and vegetables and well-balanced. Several times a week, spend at least 30 minutes exercising. Control long-term health issues like diabetes and high blood pressure. Furthermore, practising mindfulness, meditation, or yoga can help to keep your vagus nerve healthy by relaxing your nervous system.
Experts believe there is a strong link between the gut biome and a healthy vagus nerve because bacteria in our guts can produce neurotransmitters like dopamine, so they recommend taking prebiotics and probiotics to maintain a healthy gut biome.
Singing may also stimulate your vagus nerve, keeping it healthy, because vibrations stimulate the vagus nerve in the back of your throat. If you don’t enjoy singing, gargling has the same effect.
Summary
The body’s longest cranial nerve, the vagus nerve, performs both afferent and efferent motor and sensory functions. It runs from the head to the abdomen and is responsible for carrying sensory information, controlling swallowing and speaking muscles, and influencing the immune system. The nerve has several branches in the neck, including the pharyngeal, superior laryngeal, recurrent laryngeal, and superior cardiac nerves. It has a wide distribution and functions, including sensing, sensory, motor, and parasympathetic control.
The vagal system also develops pharyngeal and laryngeal muscles, laryngeal cartilage, aortic arch, and subclavian arteries. Testing the vagus nerve can reveal information about its interaction with the cardiovascular system, known as cardiovagal tone. Damage to the vagus nerve can result in various conditions, including mental health issues, chronic headaches, Alzheimer’s, and gastroparesis.
Vagus nerve pathology is a complex condition affecting the autonomic nervous system, affecting organs, glands, and muscles. Symptoms include laryngeal nerve palsy, sensory neuropathy, and motor neuropathy. Vagus nerve stimulation (VNS) is a procedure that stimulates the nerve with electrical impulses, used to treat certain epilepsy and depression. It may be linked to depression, metabolic disease, and heart disease.
Symptoms include stomach pain, acid reflux, heart rate, blood pressure, swallowing problems, dizziness, loss of voice, loss of appetite, and nausea. Diagnosis involves tests like CT scans, MRIs, echocardiograms, gastric emptying devices, and upper endoscopy. Treatment options include diet changes, medications, feeding tubes, and gastomy. Preventing vagus nerve health includes a balanced diet, regular exercise, controlling long-term health issues, practising mindfulness, meditation, yoga, and taking prebiotics and probiotics.
FAQs
What’s a different term for the vagus nerve?
The longest cranial nerve in the body, the vagus nerve (cranial nerve [CN] X), performs both efferent and afferent motor and sensory functions.
What appears if the vagus nerve is oversensitive?
Vasovagal syncope occurs when the vagus nerve to your heart overreacts to stimuli such as extreme heat, anxiety, hunger, pain, or stress. Blood pressure drops rapidly (orthostatic hypotension), causing you to feel dizzy or faint.
The vagal nerve is located where?
The vagus nerve travels from the brain to the abdomen via the thorax and face. travels laterally out of the skull through the jugular foramen after leaving the brain via the medulla oblongata of the brainstem.
What is the vagus nerve’s motor function?
The muscles in the pharynx, larynx, and soft palate—the fleshy region close to the back of the roof of the mouth—are among the motor functions of the vagus nerve. stimulating the heart’s muscles, which lowers the heart rate at rest.
What are the vagus nerve disorders?
Damage or dysfunction of the vagus nerves can result in disorders such as gastroparesis. Food does not pass through the stomach and into the intestines properly in this condition.
Vasovagal syncope. In this disorder, sudden drops in blood pressure cause dizziness or fainting.
Why is the vagus nerve special?
The vagus nerve, also known as the vagal nerve, is the primary nerve of the parasympathetic nervous system. This system regulates specific bodily functions like digestion, heart rate, and immune system. Because they are involuntary, you are unable to control them consciously.
How should the vagus nerve be evaluated?
The physician may tickle the back of the throat on both sides during this portion of the examination with a soft cotton swab. The person should gag as a result of this. If the patient does not gag, there might be a vagus nerve issue, which might point to a brain stem function issue.
References:
- Segal, D. (2022, October 6). Vagus Nerve: What to Know. WebMD. https://www.webmd.com/brain/vagus-nerve-what-to-know
- Vagus Nerve. (n.d.). Physiopedia. https://www.physio-pedia.com/Vagus_Nerve
- Seladi-Schulman, J. (2023, February 14). What is the Vagus Nerve? Healthline. https://www.healthline.com/human-body-maps/vagus-nerve
- Professional, C. C. M. (n.d.). Vagus Nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22279-vagus-nerve
- The Vagus Nerve (CN X) – Course – Functions – TeachMeAnatomy. (2023, October 7). TeachMeAnatomy. https://teachmeanatomy.info/head/cranial-nerves/vagus-nerve-cn-x/
- Kenny, B. J., & Bordoni, B. (2022, November 7). Neuroanatomy, Cranial Nerve 10 (Vagus Nerve). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537171/


2 Comments