Multiple Sclerosis (MS)
What is a Multiple Sclerosis?
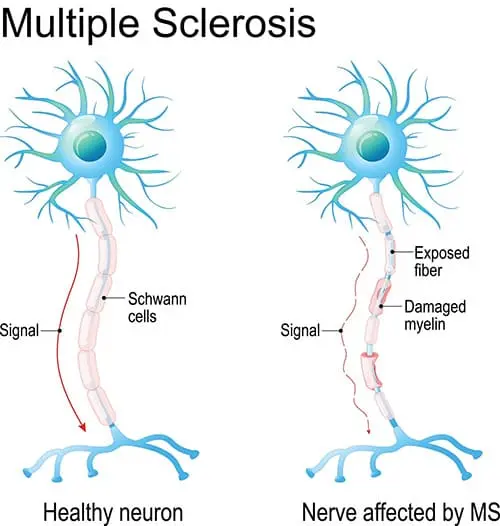
Multiple sclerosis (MS) is a chronic neurological condition affecting the central nervous system (CNS), including the brain and spinal cord. It is characterized by the immune system attacking the protective covering of nerve fibers called myelin, leading to inflammation, damage, and disruption in nerve signal transmission.
- It is believed to be autoimmune. disorder, a state in which the body unintentionally targets itself.
- Certain MS individuals may only exhibit mild symptoms. Others could become unable to write, speak, walk, or see well when There is a breakdown in the flow of information between the brain and other bodily components.
Definition of multiple sclerosis:
- An autoimmune condition known as multiple sclerosis (MS) is typified by gliosis, selective demyelination, and inflammation. It may result in both immediate and long-term effects, which can lead to serious impairment and a lower standard of living.
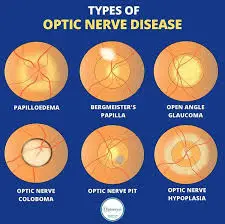
- A chronic condition that targets the central nervous system, including the brain, spinal cord, and optic nerve, is multiple sclerosis.
Causes of multiple sclerosis:
- It is uncertain what causes multiple sclerosis. It is classified as an autoimmune illness since the immune system of the body targets its tissues. The fatty material known as myelin, which covers and shields nerve fibers in the brain and spinal cord, is destroyed in multiple sclerosis cases due to immune system malfunctions.
- Myelin is comparable to the insulating layer that covers electrical cablesThe insulating layer that surrounds electrical lines is analogous to myelin. The messages that pass down a nerve may be delayed or inhibited when the protective myelin covering is broken and the nerve fiber becomes visible. There’s also a chance of nerve injury.
- Autoimmune response: Multiple sclerosis (MS) is considered an autoimmune disease, meaning that the immune system of the patient mistakenly targets the central nervous system, particularly the myelin coating that protects and coats the nerve fibers in the brain and spinal cord. Demyelination, or the loss of myelin, is the cause of neurological symptoms and decreased nerve transmission.
- Hereditary predisposition: Research indicates that genetic factors may impact a person’s susceptibility to multiple sclerosis. Certain genetic variations have been connected to an increased risk of the illness.
- Environmental elements Geographical location, the amount of vitamin D obtained from sunshine, and viral infections are a few environmental elements that have been linked to an increase farther from the equator, where there is less exposure to the sun and, consequently, less synthesis of vitamin D. Furthermore, a few viral infections have been studied in connection with multiple sclerosis, however, no obvious causal connection has been discovered.
- Smoking: It has been shown that smoking increases the chance of acquiring multiple sclerosis (MS) by exposure to several environmental factors.
Pathophysiology of multiple sclerosis:
- Immunological cells that penetrate the blood-brain barriers become activated in MS patients as a result of the immunological response. cause “AUTO-IMMUNE CYTOTOXIC EFFECTS” in the central nervous system by activating the autoantigens. demyelination slows down neuronal transmission and hastens the wear and tear of neurons.
- Demyelinated regions ultimately go through a process known as “GLIOSIS” in which fibrous astrocytes fill the space of cells.
Disease course:
- The majority of MS patients experience relapsing-remitting symptoms. Develop over a few days or weeks, and they often get better entirely or in part. There are peaceful intervals of illness in between these relapses. remission lasting many months or possibly a few years. Although little increases in body temperature might momentarily exacerbate MS signs and symptoms, they are not diseases.
- Most people with relapsing-remitting multiple sclerosis (MS) eventually develop secondary-progressive MS, which is characterized by a continuous onset of symptoms with or without periods of remission.
Symptoms often intensify and cause issues with movement and gait. Individuals with secondary-progressive MS have a wide range of disease progression rates. - There are some MS patients whose symptoms appear gradually at first and then steadily worsen over time without ever relapsing. We refer to this as primary-progressive MS.
Types of multiple sclerosis:
MS comes in four varieties:
- Symptoms of the clinically isolated syndrome (CIS): it must continue for at least twenty-four hours and is limited to a single episode.
- Relapse-remitting MS (RRMS): This is the most prevalent kind, accounting for around 85% of cases with MS. It involves episodes of fresh or worsening symptoms.
- Primary progressive MS (PPMS): Without early relapses or remissions, symptoms steadily increase. Approximately 15% of cases involve PPMS.
- SPMS, or secondary progressive MS: The condition worsens after the early bouts of relapse and remission. following variables may make you more susceptible to multiple sclerosis:
Risk factors of multiple sclerosis:
- The following variables may make you more susceptible to multiple sclerosis:
- Years old: Although MS can strike anybody at any age, it most frequently strikes those in the 15–60 age range.
- Sexual: MS affects women around twice as frequently as it does males.
- background in the family: You have an increased chance of getting MS if any of your parents or siblings have had the condition.
- certain infections: Numerous viruses, including Epstein-Barr, the virus that causes infectious mononucleosis, have been connected to multiple sclerosis.
- Race: White people are more at risk of acquiring MS, especially those descended from Northern Europe. The least at-risk group is made up of people who are Asian, African, or Native American.
- Weather: In temperate areas, such as those in Canada, the northern United States, New Zealand, southeast Australia, and Europe, MS is significantly more prevalent.
- certain autoimmune conditions: If you have inflammatory bowel disease, type 1 diabetes, or thyroid illness, your chance of having MS is somewhat increased.
- smoking: Smokers have a higher chance than nonsmokers of developing a second event that verifies relapsing-remitting MS after they first encounter symptoms that might indicate the disease.
Symptoms of multiple sclerosis:
Early symptoms of multiple sclerosis:
- Among MS’s most typical symptoms are:
- Muscle weakness: People may suffer from weak muscles as a result of nerve damage, inactivity, or lack of stimulation.
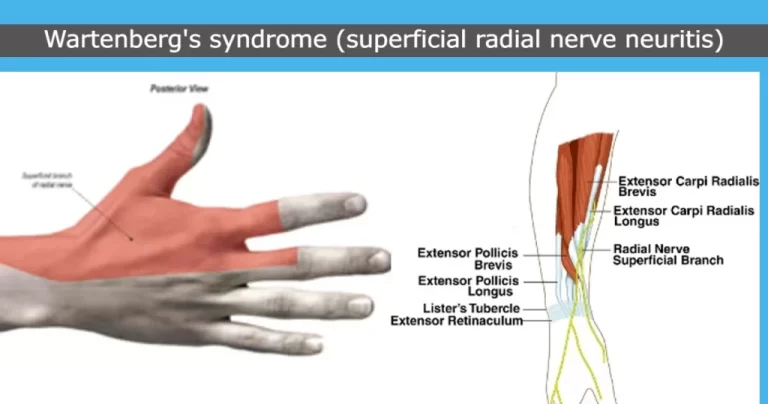
- Numbness and tingling: One of the first signs of multiple sclerosis (MS) is a sensation akin to pins and needles that can affect the arms, legs, face, and torso.
- Lhermitte’s sign: When someone moves their neck, they may feel as though they are receiving an electric shock.
- Urge incontinence: is the term for bladder issues where a person finds it difficult to empty their bladder or has to urinate frequently or unexpectedly. A symptom of MS early on is loss of bladder control.
- Bowel problems: Constipation-induced faecal impaction can lead to bowel incontinence.
- Fatigue: is one of the most prevalent symptoms of multiple sclerosis (MS) and can make it difficult for a person to operate at home or work.Along with balance and coordination impairments, dizziness and vertigo are frequent disorders.
- Sexual dysfunction: Losing interest in sex can happen to men and women equally.
- Muscle spasms and spasticity: are early indicators of multiple sclerosis. Neural fiber damage in the brain and spinal cord can result in excruciating spasms of the muscles, especially the legs.
- Tremor: Involuntary trembling motions might occur in certain MS patients.
- Vision issues: Some persons may have blurry or double vision, as well as partial or complete blindness. This usually only has an effect on one eye at a time. Pain when moving the eye might be a symptom of optic nerve inflammation. Low vision is a precursor of multiple sclerosis.
- Alterations in gait and mobility: MS patients may have alterations in their gait owing to muscular weakness, balance issues, weariness, and dizziness.
- Depression and emotional changes: Demyelination and damage to nerve fibers in the brain can cause emotional alterations.
- Memory and learning issues: These might interfere with one’s ability to focus, organize, learn, set priorities, and multitask.
- Suffering: Suffering is a typical MS symptom. Localized pain might be caused by muscular stiffness or spasticity, but neuropathic pain is directly related to multiple sclerosis.
Less frequent symptoms consist of:
- Headaches
- Loss of hearing
- Scratching breathing issues or respiratory issues
- Seizures
- Speech problems
- Swallowing issues
Additionally, there’s a greater chance of decreased activity, loss of mobility, and urinary tract infections. These may affect a person’s career and social life. - Later on, individuals may have cognitive and perceptual abnormalities, as well as increased heat sensitivity.
- Everybody is affected by MS differently. Some people begin with a few subtle years. Sometimes, within weeks or months, symptoms get worse quickly.
- Some will only show minor symptoms, while others will develop major abnormalities that become incapacitating. There can be occasions when a person’s symptoms go worse before getting better.
How to diagnose multiple sclerosis?
- A physical examination looks for abnormalities or deficiencies in your sensibility, balance, leg or hand coordination, eye movements, and equilibrium. verbal or automatic. Even though a neurologist may have a high suspicion of MS at this point, a diagnosis won’t be made until more test results are validated in the ms.
- MRIs, or magnetic resonance imaging.
- A powerful magnetic field is used by an MRI scanner to provide an intricate picture of the interior of your brain and spinal cord. It’s quite precise and can precisely locate and measure any damage, inflammation, or scarring (lesions). More than 90% of MS patients get an MRI to confirm their diagnosis.
- An individual must lie down and pass through a little tunnel in the middle of the MRI scanner to have a picture of their brain and spinal cord taken. It is a painless procedure that takes anywhere from 10 to 60 minutes, of scanning. In a video, the Newcastle Upon Tyne Hospitals NHS Foundation Trust describes what to anticipate when you obtain an MRI.
Tests for evoked potentials
- The goal of this painless test is to time how long it takes for your electrodes to be put on your head. These test the brain’s response to sounds perceived through headphones and patterns shown on a screen or feelings that are experienced by your skin.
- If MS has destroyed the myelin layer in your brain, messages will travel through it more slowly. brain to process information from your skin, hearing, and eyes.
Puncture of the lumbar region
- This is known as a spinal tap sometimes. This is done by inserting a needle into your local anesthetic. To check for MS symptoms, a little sample of the fluid around your spinal cord is obtained. Individuals suffering from MS.
- frequently have antibodies in this fluid. Antibodies indicate that the immune system is functioning in the brain and spinal cord. This is an item. that non-MS patients do not exhibit. After a lumbar puncture, headaches are common. You should get management advice from the medical personnel.
- The usage of punctures has decreased with the widespread adoption of MRI scans. lower back, into the region around your spinal nerve.
Medication for attack by multiple sclerosis:
- Corticosteroids are used to lessen neuropathy, Insomnia, elevated blood pressure, mood fluctuations, and fluid retention are possible side effects. The exchange of plasma (plasmapheresis). Your blood is extracted, and the liquid component known as plasma is separated from the rest of your blood
- Cells: Your body reintroduces the blood cells after they have been mixed with albumin, a protein solution.
- Exchange of plasma is possible. if your symptoms are brand-new, severe, and unresponsive to steroid treatment.
- Symptom: Paresthesias, or sensory symptoms.
Pins and needles, tingling, irritation, and numbness.
Handling:
- Treatment is not essential unless it interferes with function; if so, medication may be prescribed; if not, PT/OT referral may be necessary.
- Symptoms: * Primary pain * Continuous central neuropathic pain (dysesthesias) Medication used for treatment
antiepileptic drugs (pregabalin, gabapentin); tricyclic antidepressants (amitriptyline, nortriptyline, desipramine) - Additional: using capsaicin acid cream topically; practicing behavioral self-management (mindfulness, meditation)
Cognitive behavior therapy and hypnotherapy. - Intermittent central neuropathic pain (trigeminal neuralgia) Medications used for treatment:
- Initially, carbamazepine.
Other choices include baclofen, lamotrigine, and oxcarbazepine.
Other alternatives with less proof include valproic acid, phenytoin, clonazepam, and intranasal lidocaine.
Surgery: glycerol rhizotomy, radiofrequency rhizotomy, and radiofrequency electrocoagulation. - Relevance of psychosocial factors to every pain manifestation:
difficulties balancing, clumsiness, and loss of dexterity due to sensory loss, uncomfortable, occasionally unbearable,
Increased exhaustion brought on by drugs and sleep disturbances. - NOTE: Even though pain is a prevalent, distressing, and incapacitating symptom of multiple sclerosis (MS), many individuals continue to hear from doctors that the disease does not cause pain.
- *Symptom: Musculoskeletal secondary pain
either from incorrect wheelchair use or fitting or from poor posture and balance in people who can walk. - Interventions for treatment: wheelchair/scooter referral to PT; gait and balance training;
Pharmaceuticals: analgesics
evaluation of all seats in the house, car, and workplace.
Physical Therapy Treatment:
- Treatment with a physical therapist might be crucial to maintaining there isn’t a treatment for multiple sclerosis, exercise seems to help on several levels and might play a significant part. can aid in postponing the disease’s detrimental consequences.
MS sufferer who is well and actively involved in the community. - Exercise selection should take one’s skills and shortcomings into account. There is evidence to support the effectiveness of exercise treatment for MS. Its purpose is to determine the ideal ‘dosage’ (intensity, frequency, and duration) of treatment to maximize the positive benefits of therapy on participation and activities for MS patients. There was no proof of any negative consequences for MS patients who engage in exercise treatment. Exercise is thought to be a safe and effective kind of recuperation.
- PT assessments should concentrate on posture, mobility, and function, giving careful thought to how a patient’s limitations in terms of pain, exhaustion, or other conditions may affect their ability to perform. By analyzing these outcomes, the physiotherapist will be able to create a customized program. It is necessary to configure this program such that it can be carried out at home. To help patients manage their programs as autonomously as possible, education is also crucial.
Positive outcomes from multidisciplinary treatment for MS patients are possible. - Patients may have only minor deficits in the EARLY STAGE of MS. The physical therapist may now concentrate on teaching the patient, their family, and carers about the course of the illness and energy-saving compensatory techniques.
- To benefit directly from sunlight in MS, emphasize moving outside, especially in the sunshine. The most current research indicates that regardless of race or ethnicity, lifetime sun exposure appears to lower the incidence of multiple sclerosis. Research shows that Sun exposure’s protective effects in MS are most likely mediated by immunomodulatory pathways.
Multiple sclerosis exercise:
- Exercises that are either passive, active, or aided (done with a partner or using the Bobath approach, Vojtas, and Proprioceptive Neuromuscular Techniques); when done consistently and intensely enough, show signs of improvement in MS patients with the use of tools like elastic bands.
- Osteoporosis and pathological fractures can result from the use of therapeutic corticosteroids and inactivity brought on by weakness and exhaustion. Aerobic training appears to have a beneficial impact, and weight-bearing workouts can slow down the loss of suggested for preserving bone and muscle. Training in aerobic exercise at a low to moderate intensity can enhance aerobic capacity and lessen fatigue.
- Exercise for balance can help with balance: The risk of falls is increased by poor postural control. Patients with MS have a diminished capacity to produce falls, delayed postural disturbances, and greater sway in silent standing. The majority of gait studies show reduced joint mobility, cadence, stride length, and speed. MS, To help MS patients avoid falls, the therapist has to pinpoint several potentially intervention-friendly circumstances.
- Improvements in balance deficits can be facilitated by comprehensive exercise programs. Exercises for functional balance can profoundly affect an adult’s quality of life, balance, and physical activity due to multiple sclerosis.
approach the boundaries of stability. These deficiencies most certainly - In neuro-rehabilitation, MOTOR IMAGERY: is being used more and more to improve motor function. MS patients can benefit from motor imagery and rhythmic auditory stimulation for walking rehabilitation. Significant improvements in walking distance, pace, perception, and quality of life were seen in a randomized control experiment examining motor imagery.
- Individuals with multiple sclerosis benefit from hippotherapy, which also improves their quality of life and balance. In people with neuromotor development and physical impairments, horseback riding has both physical and emotional benefits, according to a systematic review and meta-analysis of the therapeutic efficacy of the intervention.
- MS patients who are ambulatory reported improved balance and gait when riding horses. Hippotherapy benefits the horse by offering efficient rhythmic anterior and posterior swinging motion combined with sensory stimulation. It motivates the cyclist to have good posture and equilibrium.
- People with progressing multiple sclerosis may benefit from the AQUATIC EXERCISE program. Individuals with progressive multiple sclerosis benefit from interventions that bolster overall health, increase energy, and enhance mental impairment. Due to the diminished influence of gravity. Through training, patients can complete activities including standing and moving, even if they have significant lower extremity paresis.
Cognitive behavioral therapy(CBT):
- In MS patients, CBT has a somewhat beneficial impact on tiredness. Nevertheless, this impact diminishes when medication is stopped. There is a long-term impact of these short-term effects because CBT has a good short-term effect on tiredness associated with multiple sclerosis. It is best to send the patient to a CBT specialist to get positive outcomes.
- CBT can potentially be a useful short-term therapeutic for MS patients to reduce mild depression, which may help increase the patient’s standard of living.
PT can provide psychological support to patients and their families/caregivers at any point in the MS journey. - PT Interventions for Frequently Experienced MS Symptoms:
- Pain: MS patients frequently suffer pain that is either a direct result of the illness, a side effect of medicine or other symptoms, or the result of something else different. PT uses hydrotherapy to aid with pain relief.
- Sensory deficits: During resistance training and exercise, tapping and spoken signals can help restore proprioception deficits. Double or fuzzy vision are frequent visual issue among MS patients. PT may provide safety tips and methods for enhancing balance and coordination in low-light conditions. Interventions in physical therapy for reduced feeling incorporate instruction on awareness, safety, and self-care to help desensitize body areas to light contact. Devices that relieve pressure are a key preventive measure that should be used in conjunction with appropriate transfer methods and frequent skin examinations to preserve skin integrity.
- Tiredness: A significant proportion of MS patients report experiencing tiredness, one of the disease’s most incapacitating symptoms. PT techniques to assist patients in overcoming sensations of extreme fatigue include energy conservation, pacing, and aerobic activity. A PT constantly monitors aerobic exercise routines to make sure a patient doesn’t overheat and can continue working on boosting their potential for endurance, which will enable them to work better all day. PTs can impart energy by reducing weariness, conservation techniques, and activity pacing can assist someone in continuing their regular activities.
- Spasticity: Spasticity causes a range of impairments, such as contractures, postural deformities, decubitus ulcers, and more. It also leads to physical and functional limits. electrical stimulation, range-of-motion exercises, therapeutic exercise, and posture training. A mix of the paths pursued is frequently treated.
- Postural impairments, coordination, and balance: Deficits in balance and coordination can be caused by ataxia, postural instability, muscular spasms, and generalized muscle weakness. PT methods for resistance training, water treatment, proprioceptive loading, static/dynamic balance training, and rhythmic stabilization instruction treat these problems, such as core exercises and posture.
- Problems with Mobility: Among other deficiencies, weakness, especially in the lower extremities, fatigue, poor posture, contractures, loss of sensation, heat intolerance, and other deficiencies can make it difficult for a physical therapist (PT) to help a patient overcome their mobility limitations through locomotor and functional training.
- Walking is a key component of locomotor exercise, which also trains posture and balance. Thigh and hip strength are increased. As needed, orthotics and assistive technology are incorporated. Functional training includes transfers, bed mobility, and collaborating with the patient to design safety measures for moving about the house and the neighborhood.
Medication alteration:
- Nutrition is a major factor in health. According to research, including items that reduce inflammation in the diet may help manage chronic inflammation.
- Numerous variables, including a shortage of vitamin D and gluten and dairy products, may contribute to inflammation. It is strongly advised to follow a diet high in whole, fresh foods and low in dairy, sugar, excessive salt, and processed foods.
- To enhance lifestyle, several researchers are investigating nutritional intervention strategies for MS. An Iranian research found that probiotics may benefit MS patients’ health by lowering disability and enhancing inflammatory and metabolic markers.
- Supplementing with vitamin D aids in both MS therapy and prevention. Numerous investigations are looking at how well vitamin D treatment works for MS patients.
- Supplementing with fish oil in addition to vitamins and nutritional guidance can help people with recently diagnosed multiple sclerosis achieve better clinical results. Further research is required to assess the effectiveness of omega-3 dietary treatments in MS and their compatibility with MS medications.
- It is believed that a key factor in the process behind the development of demyelinating diseases is mitochondrial dysfunction. Histopathological and animal research findings indicate that defective mitochondria are significant contributors to the impairment and axon and neuronal loss. The connection between MS neurodegeneration and mitochondrial dysfunction is investigated.
Living with multiple sclerosis:
- You must take your medications as prescribed. Taking part in a research study might assist you. When walking becomes more difficult, you can use assistive devices like walkers or canes to help you get around.
- Rehabilitative exercises might also assist you in maintaining or regaining function. You may maintain your independence by rearranging the furniture in your home. Discuss your needs with your family and medical professionals.
Prognosis for multiple sclerosis:
- Multiple sclerosis has no known treatment and is a permanent disease. Nonetheless, there are excellent therapy choices that can help control symptoms and reduce the frequency of flare-ups. Regardless of the course of therapy, multiple sclerosis (MS) can cause impairment and eventually make it impossible to do daily tasks on one’s own. Throughout your MS journey, your care team is here to support you, take preventative measures, and enhance your quality of life.
- Cigarette smoking may hasten the disease’s progression.
- Life span is typically unaffected by multiple sclerosis unless it is severe.
Summary
- Although there is still much to learn about the underlying genetic and environmental variables that cause multiple sclerosis, such as obesity, smoking, and low vitamin D levels, the illness is still difficult to treat and debilitating. When a patient presents with a clinically isolated condition, imaging, and spinal fluid abnormalities are part of the diagnostic criteria that assist an early and correct diagnosis. Crucially, patients with the recurrent remitting type of the illness have access to a wide range of oral and infusion therapies. Selecting the right course of therapy takes careful thought, weighing efficacy against adverse effects, and intensifying when clinically necessary.
- A clinical guideline released in 2018 supports this shift towards more individualized therapy. In conclusion, it is highly advised that all patients with multiple sclerosis implement a complete management program that promotes wellness, addresses aggravating factors, and manages comorbidities to improve health-related quality of life. The creation of therapies combining neuroprotection and remyelination to address and eventually stop the debilitating, progressive forms of multiple sclerosis is the most unmet challenge in the field.
FAQs
Could someone with MS have a regular life?
If you are diagnosed with multiple sclerosis (MS), you may need to modify your daily routine; nevertheless, many individuals may live long, active, and healthy lives if they receive the appropriate support and treatment.
What is the cause of multiple sclerosis?
It is uncertain what causes multiple sclerosis. It is regarded as an immune-mediated illness, meaning that the body’s defense mechanism targets its own tissues. Myelin, the fatty material that covers and shields nerve fibers in the brain and spinal cord, is destroyed in multiple sclerosis cases due to immune system malfunctions.
Can you manage MS without taking medication?
A tiny percentage of MS patients have relatively minor symptoms and recover effectively without medical intervention. However, many worsen over time. Medication can lessen the frequency and intensity of relapsing-remitting MS bouts.
Does multiple sclerosis impact the brain?
An autoimmune condition that affects the brain and spinal cord is called multiple sclerosis (MS) (central nervous system). Comprising the brain and spinal cord, the central nervous system. Every peripheral nerve is a part of the peripheral nervous system.
Could multiple sclerosis be cured?
It is not possible to cure multiple sclerosis. The goals of treatment usually include controlling MS symptoms, minimizing new radiographic and clinical relapses, expediting recovery from attacks, and delaying the disease’s development. Some people’s symptoms are so minor that they don’t require medical attention.
- Multiple sclerosis (MS). (n.d.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/multiple-sclerosis-ms
- Mayo Clinic: Multiple Sclerosis: Symptoms and Causes. (2022, December 24). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
- Professional, C. C. M. (n.d.). Multiple sclerosis (MS). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17248-multiple-sclerosis
- What is MS? (n.d.-b). National Multiple Sclerosis Society. https://www.nationalmssociety.org/What-is-MS.




25 Comments