Optic Neuritis
Optic neuritis is the term for an inflammation of the optic nerve. This results in various symptoms like pain and blurred vision. This disease shows a strong association with other autoimmune diseases as well as chronic conditions like multiple sclerosis. Optic neuritis may be lessened or prevented, and more serious long-term effects may be avoided, with early detection and care.
What is an Optic Nerve? Anatomy and its Function
The optic nerve, which consists of millions of nerve fibers, transmits visual impulses to the brain to enable vision. An optic nerve at the rear of each eye is directly linked to your brain.
The nerve fiber bundle known as the optic nerve acts as a communication link between your brain and eyes. A special covering known as myelin covers the nerve fibers.
Optic Nerve Anatomy
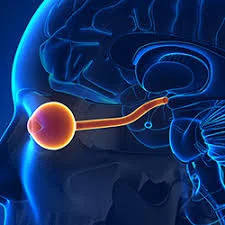
The second of the twelve cranial nerves is the optic nerve. Every eye has one optic nerve.
- The optic disk, a collection of cells in the retinal tissue at the back of the eye, is where the optic nerve begins.
- It enters your skull through the optic canal, a bony notch.
- When it meets the opposite optic nerve, it forms the optic chiasm, an X-shaped structure.
- Generates routes known as the optic radiations (ORs), both lower and upper.
- Nerve signals are sent to the visual cortex, a region of your brain, via the OR pathways. For vision, sensory data is processed by the visual cortex.
Optic Nerve Branches
There are branches on each optic nerve that either go to your brain or combine with other fibers. Half of the nerve fibers from your left eye proceed to:
- The left side of your brain is at the optic chiasm, where the two optic nerves intersect.
- The right side of your brain is connected to half of the nerve fibers in your right eye.
- The nerve fibers that remain united. To produce a coherent visual image, your brain processes information simultaneously from both eyes (binocular vision).
Optic Nerve Function
- Your vision is greatly dependent on the optic nerve. It is an expansion of your spine and brain’s central nervous system.
- Electrical impulses from your eyes are carried to your brain via the optic nerve. Your brain processes this sensory information to enable vision.
What is Optic Neuritis?
- Optic neuritis (ON) is one type of neuropathy, or nerve disease, that can cause vision loss or vision changes. It occurs when signals passing through your optic nerve, the nerve that connects your eyes and brain are impacted by inflammation.
- Your optic nerve cells are covered in a fatty substance known as the myelin sheath. The sheath weakens when you have ON. The covering offers protection. The nerve cells can’t send impulses correctly without it. Because of this, this illness often appears as several types of vision loss.
- Optic neuritis symptoms and signs might appear later on in the course of multiple sclerosis (MS) or they can be the initial sign of MS. The illness known as multiple sclerosis (MS) results in inflammation and harm to both the optic and brain nerves.
- Optic nerve inflammation is not limited to MS; it can also result from infections or immunological disorders like lupus. In rare cases, inflammation of the spinal cord and the optic nerve is caused by a different illness known as neuromyelitis optical.
- Once optic neuritis has crashed, most people recover their eyesight on their own without any medical intervention. Steroid drugs can occasionally speed the visual recovery process following optic neuritis.
Types of the Optic Neuritis
Optic neuritis comes in three primary forms:
- Typical. When left untreated, this variety often only affects one eye, and most patients recover in a few days. (However, for other reasons, specialists continue to strongly advise therapy.)
- Atypical. People with this type typically don’t recover quickly, and it frequently affects both eyes. There is evidence that it is related to several other important neurological disorders that impact the nervous system.
- Pediatric. This is optic neuritis in its juvenile stage. There are some major differences, even though they are similar to the other two categories. Overall, this kind typically has a better prognosis.
Causes of the Optic Neuritis
It is unknown exactly what causes optic neuritis. It is believed that it occurs when your immune system unintentionally attacks the substance that covers your optic nerve, causing inflammation and myelin damage. Electrical impulses normally flow quickly from the eye to the brain, where they are translated into visual information, thanks to the myelin sheath. This mechanism is disturbed by optic neuritis, which impairs vision.
That inflammation could have various causes including:
- Conditions that are inflammatory and autoimmune.
- Infections.
- Toxins and drugs.
- Other conditions.
Inflammatory and autoimmune diseases:
- Multiple sclerosis: When you have multiple sclerosis, your immune system targets the protective sheath that surrounds your brain’s nerve fibers. After one episode of optic neuritis, a person with optic neuritis has a 50% lifetime chance of acquiring multiple sclerosis. If an MRI scan reveals brain lesions, you are at an even higher risk of developing multiple sclerosis after optic neuritis.
- Optic neuromyelitis: Inflammation affects the spinal cord and optic nerve in this disorder. While neuromyelitis optica and multiple sclerosis are comparable conditions, neuromyelitis optica rarely damages the brain’s nerves. Nevertheless, compared to MS, neuromyelitis optica is more severe and frequently results in a slower recovery following an incident.
- Myelin oligodendrocyte glycoprotein (MOG) antibody disorder: This illness may result from inflammation of the brain, spinal cord, or optic nerve. Recurrent episodes of inflammation can happen, just like in MS and neuromyelitis optica. It is generally better to recover from myelin oligodendrocyte glycoprotein (MOG) attacks than from neuromyelitis optica.
Infections
Your optic nerve is not an exception to the rule that infections can harm your nerves (neuropathy). Pediatric ocular neuritis frequently develops as a result of infections. Infections can result from four primary types of pathogens:
Viral Infection
Optic neuritis is frequently caused by viral infections, particularly in the case of juvenile cases. There are various examples of these viruses, including the one that causes:
- Shingles and chickenpox, are called Varicella.
- Type 1 and type 2 herpes simplex virus.
- Cytomegalovirus.
- HIV.
- Viruses are transmitted by mosquitoes.
- Such as measles viruses in children.
Bacterial Infection
Humans typically contract optic neuritis from animals or insects that carry the bacteria. Bacteria or bacterial illnesses include, for example,
- Cat scratch fever.
- Disease carried by ticks, Lyme.
- Tuberculosis
- Syphilis.
Fungal Infection
Optic neuritis can be caused by fungi such as
- Cryptococcus neoformans, or cryptococcosis.
- Different species of candida (candidiasis).
- Histoplasmosis caused by Histoplasma capsulatum.
- Aspergillus (aspergillosis) in several forms.
Parasitic Condition
Pets, particularly cats and dogs, are common carriers of parasitic diseases that can lead to ocular neuritis in people. As an example, consider:
- Toxoplasmosis caused by Toxoplasma gondii in cats.
- Dogs that have toxocariasis, or Toxcocara canis.
Toxins and drugs
Optic neuropathy is occasionally caused by both prescription and over-the-counter pharmaceuticals (nerve injury). Toxins and medications that can cause this most frequently include:
- Drugs used to treat infections, such as sulfa-type antibiotics, isoniazid, chloramphenicol, and ethambutol.
- Drugs for arrhythmias, such as digoxin or amiodarone.
- Drugs for malaria of the quinine class, such as hydroxychloroquine and chloroquine.
- Drugs that treat cancer, such as tamoxifen, vincristine, and methotrexate.
- Nicotine and tobacco products.
- Methanol is frequently referred to as “wood alcohol,” or alcohol.
Other causes
Optic neuropathy can also be caused by several different disorders. Among them are:
- Blood flow is decreased (ischemia). Your optic nerve may become damaged if there is insufficient blood supply to it, as this can cause malfunctioning of its cells.
- Vitamins deficiencies. Low levels of B vitamins, particularly vitamin B12, can seriously and permanently harm nerves.
- Compression of the nerves. This is the result of anything pressing on one or more of your optic nerves, inflaming and damaging them. Tumors and disorders can convey it on like hydrocephalus.
- Metabolic diseases such as diabetes type 2. As diabetes worsens, there is a greater chance of optic nerve injury. Higher blood sugar levels further increase the risk.
Symptoms Of Optic Neuritis
Usually, optic neuritis affects just one eye. A few possible symptoms include:
- Pain. When moving their eyes, the majority of people with optic neuritis suffer worsening eye pain.
- loss of vision in one eye. The degree of temporary vision loss varies, but most patients experience some reduction in vision. A few hours or days usually pass after significant vision loss, and it usually improves over a few weeks or months. There are situations where vision loss cannot be reversed.
- The visual field is lost. Loss of side vision can occur from any pattern, including loss of peripheral or central vision.
- loss of eyesight in color. Color perception is commonly affected by optic neuritis. Colors may seem less vibrant than usual.
- lights that flash. Some patients with optic neuritis claim to have seen lights flicker or flash when they move their eyes.
Risk Factors Of Optic Neuritis
Optic neuritis is more likely to occur in certain situations. Among them are:
- Gender. The development of typical ocular neuritis is more common in women and individuals assigned as female at birth (AFAB) than in men and individuals assigned as male at birth (AMAB). The AFAB-to-AMAB ratio can range from 3 to 2 to 5 to 1, according to research. Atypical optic neuritis is the exception, and it seems to affect individuals with AMAB more frequently.
- Ages. The age range between 20 and 40 is the most common for typical optic neuritis cases. It is more common for atypical optic neuritis to occur after age 50 or before age 18. Optic neuritis in children typically develops before the age of ten.
- Race. It is more common for White people to get optic neuritis. If someone has optic neuritis and then gets MS, race may also be a factor. Asians had a significantly lower risk of developing multiple sclerosis (MS) following optic neuritis, according to research.
- Location. Your chance of acquiring MS may vary depending on where you reside. Living away from the equator increases one’s chance of developing it by a small amount. Experts believe that vitamin D levels and/or sun exposure are related to this.
- Having an additional autoimmune condition. Optic neuritis is more common in people with autoimmune diseases such as sarcoidosis, Behçet’s illness, and lupus erythematosus.
Diagnosis of Optic Neuritis
For a diagnosis, which is typically based on your medical history and an examination, you’ll probably consult an ophthalmologist. The following eye tests are likely to be carried out by the ophthalmologist:
- A regular eye examination. Your eye doctor will measure your peripheral (side) vision as well as examine your eyesight and color perception.
- Ophthalmoscopy. Your doctor will examine the structures at the back of your eye by shining a strong light on it during this examination. The optic disk, which is where the optic nerve enters the retina of your eye, is assessed during this eye exam. About one-third of those who have optic neuritis experience swelling of the optic disk.
- Test for Pupillary Light Reaction. Your physician may use a flashlight to test your pupils’ reaction to intense light by moving it in front of your eyes. When exposed to light, the pupils in your optic neuritis will not contract as much as those in your healthy eyes.
Additional examinations to identify optic neuritis could be:
- MRI stands for magnetic resonance imaging. A magnetic field and radio wave energy pulses are used in a magnetic resonance imaging (MRI) scan to create images of your body. You may be given a contrast injection during an MRI to check for optic neuritis to enhance the visibility of your optic nerve and other brain regions.
- To find out if your brain has any lesions, or damaged areas, an MRI is crucial. These lesions are indicative of a significant risk of MS development. An MRI can also rule out a tumor or other potential causes of vision loss.
- Blood examinations. It is possible to have a blood test performed to look for certain antibodies or illnesses. An antibody that results in severe optic neuritis is connected to neuromyelitis optica symptoms. This test can be used to assess the risk of neuromyelitis optica in patients with severe optic neuritis. Blood testing for MOG antibodies may also be performed for unusual occurrences of optic neuritis.
- OCT, or Optical coherence tomography. This examination gauges the thickness of the retinal nerve fiber layer in the eye, which is frequently reduced due to optic neuritis.
- Visual field exam. To find out if there is any vision loss, this test evaluates each eye’s peripheral vision. Visual field loss can occur in any pattern due to optic neuritis.
- Evoked visual reaction. You will be seated in front of a screen with an alternating checkerboard pattern during this test. Your head is fitted with tiny patch wires that capture your brain’s reactions to the images on the screen. This kind of test informs your doctor if damage to your optic nerve is causing your brain’s electrical signals to travel more slowly than usual.
To confirm the diagnosis of optic neuritis, your doctor may urge you to come in for follow-up examinations two to four weeks after your symptoms start.
Treatment for Optic Neuritis
Optic neuritis frequently passes quickly and goes away on its own in four to twelve weeks without the need for medication.
- Steroid drugs are occasionally used to treat optic nerve irritation. A steroid treatment’s possible adverse effects include mood swings, weight gain, flushing of the face, upset stomach, and insomnia.
- The usual method of administering steroid therapy is intravenously. Intravenous steroid therapy appears to have little effect on the quantity of vision recovery for typical optic neuritis, but it does speed up the process.
- Plasma Exchange Therapy. Some patients may be able to regain their eyesight with plasma exchange therapy if steroid medication is ineffective and their severe visual loss does not improve. Studies have not yet established the effectiveness of plasma exchange treatment for treating optic neuritis.
- Keeping multiple sclerosis (MS) from occurring. Multiple sclerosis drugs, such as interferon beta-1a or interferon beta-1b, may help postpone or prevent multiple sclerosis (MS) if you have optic neuritis and two or more brain lesions that are visible on MRI scans. Those who have a high risk of acquiring MS are treated with these injectable medicines. Depression, irritability at the injection site, and flu-like symptoms are possible side effects.
Surgical Treatment
- Endoscopic Nerve Decompression: By removing a piece of the bony optic canal, endoscopic optic nerve decompression is a minimally invasive surgery used to stabilize or improve eyesight by relieving some of the pressure on the optic nerve.
- Vitrectomy procedure: A vitrectomy is a common procedure used to repair a macular hole. A macular hole is a tiny opening in the macula, the region of the retina that lies in the center of the retina. In almost nine out of ten cases, the hole is successfully closed after the operation if the patient has had it for less than six months. The success percentage will be lower if the hole has been there for a year or more.
Physical-Therapy for Optic Neuritis
One useful element of the recovery process for optic neuritis is physical therapy. Physical therapists can help optic neuritis patients improve their overall health and functional vision.
- Electric stimulating: The therapeutic technique known as neuromuscular electrical stimulation uses electrical currents to activate muscles. It strengthens muscles that are impaired by optic neuritis or other conditions.
- Exercises for eye movement: These can help you become easier at moving your eyes smoothly and effectively. Keep your finger at arm’s length and concentrate on it briefly. Then gradually move your finger towards your nose until it’s about an inch away, and concentrate on it for a few seconds. Repeat this movement a few times.
- Eye rolling: For a few seconds, slowly roll your eyes clockwise; then, reverse the motion.
- Palming: To generate warmth, rub your palms together. Next, lightly cover up your hands over your closed eyes, careful not to press. Cut off all lights and take a thirty to one-minute break to stay calm.
- Increasing daily living activities while having low vision: People who suffer from optic neuritis may find it difficult to visually scan their surroundings, which can make daily tasks difficult. Physical therapists can help patients with optic neuritis by teaching them techniques to maximize their remaining vision and do everyday activities.
- Vestibular rehabilitation: Optical neuritis can sometimes affect the vestibular system, which is responsible for maintaining balance. Exercises for coordination and balance that are utilized in vestibular rehabilitation help improve balance. These can assist you in improving your ability to walk on uneven surfaces, maintain balance when standing on one leg, and avoid falls.
- Gait training: Creating a safe and efficient workout schedule along with a physical therapist is the usual approach to gait training. Exercises that enhance coordination, strength, and balance may be part of the training. A cane or other assistive equipment is used by physical therapists to help patients walk with better balance.
Prognosis
- Six months after an optic neuritis episode, most patients regain near-normal vision. Individuals who experience a recurrence of optic neuritis are more susceptible to developing myelin oligodendrocyte glycoprotein (MOG) antibody-related disease, neuromyelitis optica, or multiple sclerosis.
- People without underlying medical disorders are more likely to experience a recurrence of optic neuritis and have a better long-term prognosis for their vision than individuals who have neuromyelitis optica or multiple sclerosis.
Complications of Optic Neuritis
Among the potential complications of optic neuritis are:
- Damage to the optic nerve. After an episode of optic neuritis, most patients have some lasting damage to their optic nerves, yet the damage may not result in long-term symptoms.
- A decline in visual clarity. Within a few months, most people’s eyesight returns to normal or almost normal, while some people may always have partial loss of color discrimination. There are many who never fully regain their vision.
- Adverse effects of the medication. The steroid drugs that treat optic neuritis suppress your immune system, making your body more vulnerable to infections. Increased weight and mood swings are two more adverse consequences.
Prevention for Optic Neuritis
Nerve injury and optic neuritis typically occur for various reasons. While it is not possible to prevent every potential cause, there are steps you may take to reduce your risk.
Some of the things you can achieve are as follows:
- Stay Away or give up using tobacco products (smokeless and vaping included).
- Treat infections early on to stop them from damaging your visual nerves.
- Follow the directions on prescription drugs and avoid using over-the-counter drugs.
- Prioritize your diet to prevent vitamin shortages.
- When it comes to alcohol use, exercise moderation and stay away from poisons like methanol.
- Control autoimmune or inflammatory diseases that are already present.
Summary
Optic neuritis is a disorder that can cause discomfort and irritation. Fortunately, extensive research conducted in the past few decades has improved the ability of eye care doctors and other healthcare professionals to treat the illness. As soon as you notice any symptoms of optic neuritis, you should consult an ophthalmologist.
Your chances of a successful outcome increase with the timing of your diagnosis and course of therapy. Early diagnosis and treatment can also be beneficial if you have a chronic condition such as multiple sclerosis, neuromyelitis optica spectrum disorder, or MOG-antibody-associated disease that is linked to your optic neuritis. Treatments exist for these disorders that can assist slow down their progression and improve your day-to-day activities both now and in the days to come.
FAQs
What is optic neuritis’ primary cause?
Herpes, Lyme disease, CMV, and multiple sclerosis frequently cause optic neuritis. Optic neuritis frequently has a brief course and goes away on its own in four to twelve weeks without any medical intervention
Does blindness result from optic neuropathy?
The symptoms of optic neuropathy should be seen by a specialist as soon as possible because they have the potential to cause blindness. A patient suffering from optic neuropathy may have pain when moving their eyes as well as momentary blindness.
What signs of neuritis are present?
Typical symptoms include pain and soreness in the area of the inflamed nerve or nerves, irregular circulation, decreased sweating ability, and impaired strength and reflexes. The impaired feeling is frequently accompanied by numbness or hypersensitivity.
How severe is optic neuritis pain?
Pain is a common sign of optic neuritis in over 90% of cases, and it frequently gets worse when you move your eyes. However, atypical optic neuritis may not even hurt in certain situations. reduction in vision acuity. This indicates that your vision is not as sharp or clear.
Which kind of action is appropriate for damaged optic nerves?
Gradual vision loss or progressive visual deterioration is the most typical sign of optic nerve compression. The most popular method of treating optic nerve compression is surgery. At UPMC, the Endoscopic Endonasal Approach (EEA) is the recommended surgical procedure for treating optic nerve compression.
How can one diagnose optic neuritis?
Optic neuritis can be diagnosed by your healthcare practitioner using the following procedures: Medical exam. Analyze how your eyes react to intense direct light. Check your visual acuity by using the letter chart to measure your visual acuity.
Which deficiency leads to neuritis?
Alcohol exposure, thiamine insufficiency, niacin deficit, pyridoxine excess and deficiency, cyanocobalamin deficiency, pantothenic acid deficiency, alpha-tocopherol deficiency, celiac disease, and multifactorial processes are among the causes of nutritional neuropathies.
References
- Professional, C. C. M. (n.d.-h). Optic Neuritis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14256-optic-neuritis
- Optic neuritis Diagnosis & treatment Mayo Clinic. (2021, September 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/optic-neuritis/diagnosis-treatment/drc-20354958
- Optic Neuritis. (2024, March 22). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/optic-neuritis
- Krause, L. (2022, May 30). Optic Neuritis. Healthline. https://www.healthline.com/health/optic-neuritis#outlook
- Ponsford, S. (2017, December 25). What is optic neuritis? https://www.medicalnewstoday.com/articles/320414#recovery-time
- Knobbe, C. A., MD. (2019, March 4). Optic neuritis and neuropathy: Symptoms, causes, treatments. All About Vision. https://www.allaboutvision.com/conditions/optic-neuritis.htm
- Professional, C. C. M. (n.d.-h). Optic nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22261-optic-nerve
- Image- Star Health – Your Health Insurance Specialists. (n.d.). Star Health. https://blog.starhealth.in/blog/optic-neuritis/