What is a Degenerative Disc Disease?
Degenerative disc disease (DDD) is a common condition that happens when one or more of the discs between the vertebrae of the spinal column deteriorate or break down over time. The spinal discs act as cushions between the vertebrae and allow flexibility and movement of the spine.
The spine’s discs become less elastic, flexible, and shock-absorbing as we get older. The outer layer of the discs called the annulus fibrosus may develop small tears or cracks. The jelly-like interior of the discs called the nucleus pulposus may extrude or slip out through these tears. This natural aging and wear and tear of the spinal discs is the most common cause of degenerative disc disease.
Many people with DDD do not have noticeable symptoms, especially in the early stages. Symptoms tend to develop slowly over time as more wear and tear occurs and spinal discs lose more structural integrity. Common symptoms include:
- Lower back pain that may radiate to the buttocks, hips, and legs
- Stiffness and decreased flexibility in the back
- Pain that worsens with bending, lifting, standing, or walking
- Sensations such as tingling, numbness, or weakness in the legs
DDD is often diagnosed with medical imaging tests such as MRIs which allow detailed views of the spinal discs and can detect bulging or herniated discs. Treatment focuses on managing pain and symptoms and preventing further deterioration. This typically involves medications, injections, physical therapy, exercise, massage, gentle stretching, etc. Surgery like spinal fusion may be an option for advanced cases that do not find relief from more conservative treatments.
There are steps you can take to preserve spinal health and possibly slow the progression of DDD such as maintaining proper posture and weight, exercising regularly, lifting properly, and avoiding smoking. While DDD is likely to worsen to some degree over time, symptoms can often be managed with conservative treatments. Taking steps to care for your back and spine can help improve your quality of life.
Clinically Relevant Anatomy
The Spine
The spine is made up of 33 vertebrae or spinal bones divided into sections – cervical (neck), thoracic (mid-back), lumbar (lower back), sacrum, and coccyx (tailbone). These bones provide structure, protect the spinal cord, and enable flexible movement.
Intervertebral Discs
Between vertebrae are rubbery, shock-absorbing pads called intervertebral discs that cushion and stabilize the spine. Each disc has a tough outer layer (annulus fibrosus) surrounding an inner jelly-like core (nucleus pulposus) which helps distribute pressure.
Spinal Cord and Nerves
Running through the bony vertebral column is the spinal cord, a bundle of nerves that relay signals between the brain and body. Spinal nerves exit through spaces between vertebrae on their way to various body parts.
IVDs of the Lumbar Spine
The lumbar spine bears the most body weight and is the most common site of DDD. This can lead to lower back pain, sciatica, numbness/tingling, and weakness if deteriorated lumbar discs press on spinal nerves.
Facet joints
These are pairs of joints located behind vertebrae that provide stability and guide motion. In the lower spine, facet joint arthritis often accompanies DDD causing added low back pain.
Muscles and Ligaments
Muscles and ligaments surround the spine to facilitate movement and provide extra stability. Weak core muscles coupled with strained ligaments from injury or poor posture worsen spinal issues.
Understanding the anatomy of how the healthy spine is structured and functions is key to recognizing what goes wrong in degenerative disc disease. This overview of clinically relevant spinal anatomy and commonly affected areas lays the groundwork for a more in-depth analysis of DDD.
Pathology associated with degenerative disc disease
Degenerative Disc Disease involves progressive structural and functional changes in the intervertebral discs of the spine. As part of normal aging, biochemical changes occur in discs causing disorganization and breakdown of key components in the annulus fibrosus and nucleus pulposus layers.
Annulus Fibrosis
- Fibers weaken leading to microtears and fissures
- Diminished elastic capability causes discs to be stiffer and less flexible
- Tears allow nucleus material to protrude and cause painful bulging discs/herniations
Nucleus Pulposus
- Loss of hydration and reduced proteoglycan content decrease shock absorption
- Disc tissue can calcify and form bony spurs or osteophytes
Other Age-Related Changes
- The growth of brittle bone spurs affects joint mobility
- Ligaments may thicken and calcify decreasing flexibility
- Spinal facet joints develop osteoarthritis worsening inflammation
This gradual desiccation process reduces disc height and the ability to handle mechanical stress effectively. Physical demands like bending, lifting, and trauma hasten degenerative changes. As disc integrity fails, segments of the spine become unstable and bones may rub together causing inflammation, nerve irritation, and significant pain. Disease progression varies based on factors like genetics, lifestyle, and environment.
Causes of degenerative disc disease:
Aging
The natural process of growing older causes gradual biochemical changes and the breakdown of spinal discs. As discs dehydrate, and lose flexibility and shock-absorption capacity, back pain often emerges.
Genetics
A family history of intervertebral disc degeneration increases DDD risk. Gene variations affecting collagen structure and other disc components are passed down and determine disc vulnerability and rate of decline.
Lifestyle Factors
- Improper lifting/bending – Places excessive strain on spinal discs that cumulatively take a toll
- Being overweight/obese – Excess weight compressing discs speed up wear and tear
- Smoking – Chemicals in smoke negatively impact disc nutrition accelerating degeneration
- Manual labor jobs – Occupations with repetitive lifting, vibration, and bending daily hasten DDD
Injuries/Trauma
Both sudden traumatic events and repetitive microtrauma that place excessive strain on the spine can initiate or accelerate disc degeneration.
- Herniated Discs – Occur when the nucleus pulposus ruptures through the outer wall. Chemical inflammation can lead to nerves being compressed.
- Bulging Discs – Repeated injury causes nuclear material to bulge placing pressure on nerve roots.
- Lumbar Strains – Overstretching of tendons, muscles, or discs themselves from improper lifting.
- Fractures – Vertebral fractures from high-impact falls or accidents contribute to disc deterioration.
- Whiplash – Forces delivered to the spine during car accidents often affect cervical and upper thoracic discs.
Diseases & Disorders
- Scoliosis – Abnormal sideways spinal curvature adds uneven mechanical stress leading to early DDD.
- Spinal Stenosis – Abnormal narrowing of the spinal canal damages nearby discs due to bone overgrowth.
- Spondylolisthesis – Vertebral slippage condition strains sections of the spine and discs.
- Fibromyalgia – Chronic widespread pain and tender point syndrome advance spinal disc breakdown.
- Diabetes – High blood glucose stiffens collagen fibers in discs accelerating dehydration.
Any condition that allows abnormal motion, misalignment, or asymmetry in the spine will contribute to uneven wear and tear leading to disc issues. Catching developing problems early and correcting them with physical therapy or bracing may help slow future degeneration.
While disc degeneration is inevitable to some degree with age, genetics, and lifestyle choices determine the rate of progression. Understanding DDD risk factors like family history, smoking, obesity or high-impact activities enables prevention efforts before significant pain and disability occur.
Common symptoms associated with degenerative disc disease:
Most people with DDD experience mild to severe pain in the lumbar region that may come and go or be constant. It typically worsens with standing, bending, lifting, or sitting for long periods. Twisting motions often provoke pain.
Sciatica
Many people with DDD develop sciatica or radiating pain that runs from the lower back down through the buttocks and legs. This occurs when inflamed nerve roots become compressed causing burning, tingling, or numbness along the sciatic nerve pathways.
Stiffness & Reduced Flexibility
As spinal discs degenerate and lose flexibility, the range of motion decreases. Activities requiring flexibility like looking over the shoulder become more challenging. Muscle tension and joint stiffness especially after long periods of stillness are common.
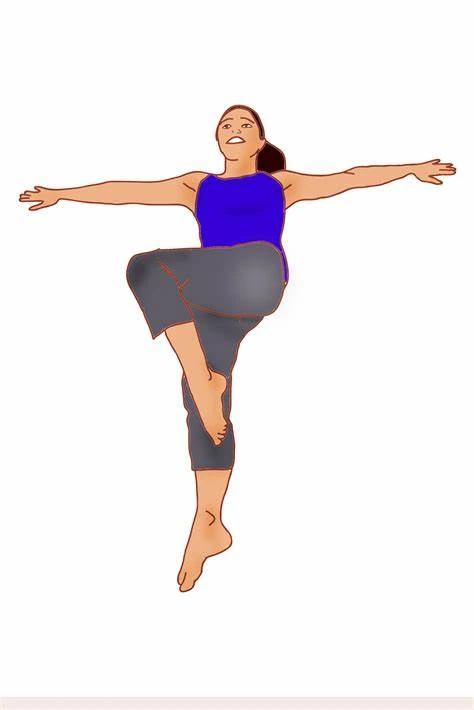
Abnormal Gait & Balance
Altered biomechanics from degenerative structural changes can disrupt normal walking patterns. Shifting weight to reduce painful pressure points leads to limping, swaying, or stooped posture making balance and coordination more difficult.
Leg Numbness or Weakness
Advanced DDD can cause discs to bulge or bone spurs to develop which narrows the spinal canal. This exerts pressure on the spinal cord and nerve roots leading to sensations of tingling, prickling, or numbness down the legs. Atrophy and loss of leg muscle control may also occur.
Catching degenerative disc problems early when symptoms first manifest enables patients to seek treatment regimens that manage pain and inflammation while restoring strength, flexibility, and spinal stability. This helps slow the disease course avoiding disability.
How degenerative disc disease is typically diagnosed
Medical History
A doctor will ask about symptoms, pain locations/severity, injury history, and daily activities to assess environmental and genetic factors contributing to possible DDD. Family history will also be reviewed.
Physical Exam
Pressing along the spine to replicate pain, assessing range of motion, reflex testing, balance/coordination checks, and muscle strength tests help determine affected areas and nerve involvement severity.
Initial Interview
The physical therapist will start by asking questions about the patient’s symptoms, daily activities, pain triggers, injury history, progression timeline, and past treatments tried. This helps direct the exam.
Postural Assessment
Standing, sitting, and walking postures are observed to check for muscular imbalances, gait abnormalities, spine curvature, pelvic tilts, or poor biomechanics exacerbating DDD.
Range of Motion Testing
The therapist manually or with instruments measures the ability to bend/twist the spine and hips. Reduced flexibility signifies strained tissues that may need targeted stretching.
Manual Muscle Testing
Key muscles like the core, glutes, hamstrings, and quadriceps are tested for strength deficits or atrophy which contribute to instability and back strain.
Orthopedic Tests
Specialized tests like the straight leg raise check for nerve root compression. Others assess facet joints or sacroiliac dysfunction which worsens back pain.
Functional Movement Screening
Patients perform activities similar to daily tasks such as squatting, lifting, and carrying to assess how DDD impacts mobility and function.
Pain Mapping
Patients rate pain levels on a scale when pressure is applied to different spinal points. This identifies tender tissues and guides treatment.
Imaging Tests
Magnetic Resonance Imaging (MRI) Scans
- Allows detailed views of soft tissues – ideal for assessing spinal discs, nerve roots, and cord
- Can detect bulging, herniated, or torn discs
- Shows loss of disc height and fluid
- May require contrast dye to improve visualization
Computed Tomography (CT) Scans
- Provides images of bone for clear views of the bony spine anatomy
- Detects bone spurs, cysts, fractures, stenosis or deformities
- Useful to inspect spinal facet joints or areas of narrowing
- Shows calcification patterns indicating advanced disc degeneration
X-Rays
- Cost-effective first-line imaging test
- Reveals disc space narrowing suggesting loss of disc padding
- Identifies bone changes like excessive growths or spurs
- Limited utility for visualizing soft tissues
Discograms
- Contrast dye injected right into spinal discs
- Helps determine if discs are the main pain generator
- Provocative testing isolates the culpable degenerated disc level
- Improves surgical intervention planning
Advanced imaging like MRI and CT scans offer the best assessment of degenerating spinal discs. While X-rays have utility for initial DDD screening, they have limitations in distinguishing the often complex structural failures underlying recurrent back pain.
Blood Work
Tests checking for inflammatory markers, vitamin deficiencies, blood sugar, genetics, etc. help uncover underlying contributors to early onset DDD.
Formal diagnosis of degenerative disc disease first involves a medical history and physical. Then if DDD is suspected, doctors will order spine imaging scans such as MRI or CT tests which offer the best visualization of deterioration within soft and hard spinal tissues.
Differential Diagnosis
It’s important to rule out other potential causes when evaluating chronic back pain. Degenerative disc disease shares symptoms with several spinal conditions.
Spinal Stenosis
Narrowing of spaces around the spinal cord or nerve roots also causes pain and numbness in the back and legs. Stenosis can accompany DDD but also occurs alone from arthritis or injury.
Herniated Disc
While DDD weakens discs over time, sudden disc herniations are often traumatic tears. Both elicit pain through inflammation and nerve compression. MRIs can differentiate.
Spinal Osteoarthritis
Thinning of cartilage around facet joints of the spine mimics DDD pain patterns. It also contributes to loss of joint mobility as arthritis worsens.
Spondylolysis/Spondylolisthesis
Stress reactions or small fractures in vertebrae that cause slippage are other sources of mechanical back pain and tightness.
Skeletal Irregularities
Existing spinal curvatures like scoliosis or kyphosis which distort posture exacerbate disc strain and degeneration.
The diagnostic process includes patient history, physical examinations, imaging tests, and often trials of anti-inflammatory medications. Since many spinal abnormalities share symptoms, differential diagnosis aims to isolate the precise interrelated biomechanical dysfunction and nerve aggravation underlying patient pain. This informs effective management.
Risk factors
- Age: Discs naturally lose flexibility and elasticity over time as part of the aging process. DDD is more common in middle-aged and older adults.
- Genetics: Some people inherit genes from their parents that make them predisposed to early disc degeneration and related problems.
- Weight: Excess body weight, especially around the abdomen, puts increased force and strain on the spine, accelerating wear and tear.
- Lifestyle: Those with sedentary jobs or activities have a higher risk as inactivity leads to weaker back muscles and poor flexibility. Regular heavy lifting without safe technique also strains discs over time.
- Trauma: Prior back injuries like fractures, disc tears, or muscle strains make one more prone to developing degenerative changes like disc bulging or herniation earlier. Auto accidents can also initiate disc issues.
- Diseases: Having diabetes, arthritis, bone density loss, and other systemic diseases negatively impact spinal health and accelerate disc degeneration. Smoking also impedes nutrient flow to discs.
- Posture & Alignment: Poor posture habits like slouching as well as structural misalignments or leg length inequality increase mechanical stress on the back and discs contributing to breakdown over the long term.
Medical treatments
Medications
- Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen reduce spinal inflammation and provide pain relief. Stronger prescription NSAIDs may be used for severe pain.
- Muscle relaxants ease muscle tension and spasms that accompany DDD. Medications like cyclobenzaprine or tizanidine minimize pain from stiffness.
- Nerve pain medications such as gabapentin or certain antidepressants can alleviate numbness, burning sensations, or nerve sensitivity associated with DDD.
Epidural steroid injections
- Anti-inflammatory corticosteroid injections are administered intraperitoneally (i.e., into the area between the spinal nerve roots) via epidural injections.
- Steroids reduce inflammation caused by a bulging, herniated, or degenerative disc pressing on nerve roots. This can temporarily relieve associated pain and neurological symptoms.
- The injection is administered in the doctor’s clinic as an outpatient procedure. The area on the back is sterilized and local anesthetic is used to numb before inserting the needle into the epidural space under imaging guidance.
- Corticosteroid medications like triamcinolone, methylprednisolone, or betamethasone are commonly injected along with some local anesthetics like lidocaine.
- Patients may feel some temporary pressure or cramping as medication goes in. The procedure itself is minimally painful due to anesthetic medicines.
- If successful, pain relief starts within 2 weeks, reducing leg/back pain by reducing impinged nerve inflammation and improving mobility and quality of life.
- Side effects are rare but may include infection, nerve injury, bleeding and leakage of spinal fluid, worsened pain, etc if the procedure is not done properly.
- Effects last a few months typically before nerves get compressed again. The injection can be repeated up to 3-4 times a year if it provides good symptomatic relief.
So in summary, epidural steroid shots are a safe and effective non-surgical treatment for degenerative disc problems when performed by an experienced doctor. It provides moderate to significant pain alleviation for many patients.
Alternative Therapies
- Acupuncture, massage, gentle chiropractic care, physical therapy, electrical nerve stimulation, ultrasound therapy, and low-impact aerobic exercise may supplement medical treatments.
Surgical Treatment
Discectomy
This procedure removes a damaged portion of a herniated or bulging disc that is putting pressure on a nerve root. It alleviates pain and numbness caused by inflammation and irritation of the nerve.
Laminectomy
This surgery eliminates bone overgrowths, such as bone spurs, by trimming away a section of the bony lamina to relieve pinched nerves. Widening the space relieves pressure.
Spinal Fusion
Fusion surgery stabilizes the spine by permanently joining two or more vertebrae together using bone grafts and metal implants. Eliminating motion between vertebrae reduces inflammation and irritation.
Artificial Disc Replacement
This removes the damaged disc and inserts a prosthesis device meant to maintain spine flexibility and motion, unlike stiff spinal fusion. The artificial disc aims to mimic healthy disc function.
Minimally Invasive Surgeries
Advanced procedures utilize tubular instruments aided by microscopic cameras. These approaches minimize incision size and collateral damage to muscles allowing quicker recovery periods.
Surgery is typically an option reserved for serious cases after more conservative medical therapies have failed and functional loss persists. Consulting multiple specialists helps determine the optimal surgical approach to address an individual’s distinct spinal instability and nerve compression issues.
A multi-modal non-surgical treatment approach focused on reducing inflammation and muscle tension while improving stability, posture and spinal flexibility serves as the first-line therapy. Surgery is considered for severe, refractory cases.
Physical Therapy Treatment
Spinal Manipulation Therapy
- Hands-on technique where a practitioner or device applies controlled force to joints/tissues to improve mobility
- Commonly associated with chiropractic care but also used by physical therapists, osteopaths
Goals in DDD Treatment
- Mobilize stiff spinal segments to increase the range of motion
- Loosen tight surrounding musculature pulling vertebrae out of alignment
- Create space between vertebrae to take pressure off nerve roots
Considerations in DDD
- Gentle mobilizations are appropriate but high-velocity thrusts are too risky
- Target areas of fixation but avoid direct force on unstable segments
- Monitor disc condition closely avoiding techniques that could worsen herniations
Benefits
- Shown to increase spinal flexibility and relieve associated headaches
- Relax back spasms/muscle tension contributing to pain
- Joint noise release provides short-term relief lasting hours to days
Spinal manipulation can provide pain relief in DDD cases early on. However, benefits remain limited as structural instabilities advance. Therapists constantly evaluate risks since discs prone to herniations require conservative care. Monitoring for red flags before attempting mobilization is key.
Stretching
Quadriceps Stretch

- Stand upright next to a wall for support, feet shoulder-width apart.
- Bending one knee, raise your heel to your buttocks. Using the hand on the same side, grasp your ankle.
- Keep your knees aligned and pointing straight ahead. Avoid letting your knee drop inward.
- Gently pull your ankle towards your body until you feel a stretch in the front of your thigh and hip.
- Keep your torso upright and your knees together. Don’t arch your lower back.
- For a deeper stretch, press your hip forward while continuing to pull the ankle back.
- Hold the stretched position for 30 seconds, breathing slowly and deeply.
- Release and repeat on the opposite leg, performing 2-4 rounds per side.
- Ensure you maintain good spinal alignment throughout the stretch. Don’t bounce or force the stretch.
- If needed, place your free hand against the wall for extra balance support.
Hip Flexor Stretch

- Start in a half-kneeling lunge position, with one knee bent at 90 degrees and the other knee on the floor behind you.
- Keep your torso upright and engage your core by gently drawing your belly button in towards your spine.
- Shift your body weight forward until you feel a stretch in the front of the hip and thigh of your back leg.
- For a deeper stretch, raise the arm on the same side as your back leg up towards the ceiling.
- To increase the stretch further, lean your torso slightly backward while keeping your core engaged.
- While holding the stretch for 30 seconds, take deep breaths.
- Switch legs, bringing the other knee forward into the half-kneeling lunge to stretch the opposite hip flexor.
- Repeat 2-3 times per side.
- Ensure your front knee remains at a 90-degree angle and does not extend past your toes.
- Keep your front knee directly over your ankle to avoid excessive strain.
Adductor Stretch
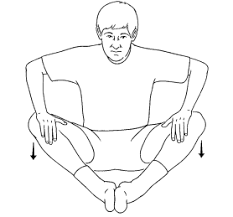
The adductors are inner thigh muscles that pull the legs inward. Tight adductors rotate the pelvis and hips putting uneven strain on the lumbar discs.
- With your legs out in front of you and your back straight, take a seat on the floor.
- Bring the soles of your feet together, allowing your knees to drop out towards the sides in a butterfly position.
- Grasp your ankles or the outsides of your feet with your hands.
- Keeping your back straight, gently press your knees down towards the floor with your elbows.
- You should feel a stretch along the inner thighs and groin area.
- Avoid rounding your back or hunching forward. Keep your chest upright.
- While holding the stretch for 30 seconds, take deep breaths.
- For a deeper stretch, walk your hands forward slightly while continuing to press your knees toward the floor.
- Release the stretch by slowly bringing your knees back together.
- Repeat 2-3 times, holding each for 30 seconds.
Hamstring Stretch
The hamstrings span the back of the thigh attaching to the pelvis. Short hamstrings tilt the pelvis back increasing low back pressure.

- Extend both legs out in front of you while lying flat on your back.
- To engage your core, pull your belly button in the direction of your spine.
- Raise one leg towards the ceiling, keeping the knee straight.
- Use a strap or your hands to grip behind the thigh and gently pull the raised leg towards your body.
- You should feel a stretch down the back of your thigh and knee.
- Keep your other leg flat on the floor to prevent arching the lower back.
- Breathe deeply while you hold the stretch for thirty seconds.
- Release and switch legs, stretching the opposite hamstring.
- Perform 2-3 sets per leg, holding each for 30 seconds.
- Avoid rounding or arching your back. Keep it pressed into the floor.
lying iliotibial band (IT band) Stretch

- Lie on your side with both legs straight out
- Bend the top hip and knee bringing the foot in front of your lower leg
- Brace your upper body on your forearm and elbow so your neck is aligned with the spine
- Avoid rolling your torso forward or backward as you rest your head on your lower hand
- With the opposite hand, grasp the ankle of the lower leg below the knee then gently pull the heel toward the buttocks
- Slowly lift the lower leg while slightly internally rotating the hip to increase tension on the outer hip/thigh
- Continue raising your leg while pressing the hip bone down into the surface below you
- Hold the stretch for 30 seconds when mild tension/discomfort is felt in the IT band
- Repeat lift 3-4 times then reverse positions lying on opposite side
- Perform the stretch 1-2 times per day, especially after long sitting periods
Glute Stretch

- Position yourself on your back, legs bent, and feet flat on the ground.
- Cross one leg placing the ankle above the opposite knee
- Thread hands through the triangular space between thighs
- Grasp the back of the thigh just behind the bent knee
- Pull the bent leg diagonally across the body until the stretch felt in the buttock
- Keep shoulders, and head relaxed and pressed into the floor
- After 30 seconds, hold each side twice or thrice.
Cat and Camel
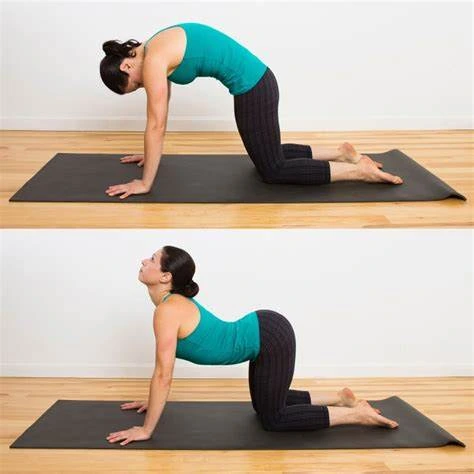
- Place your hands directly under your shoulders and your knees under your hips to begin on your hands and knees.
- The floor should be parallel to your back.
- As you exhale, gently arch your back towards the ceiling and let your head drop (camel position). Hold for 2-3 seconds.
- As you inhale, slowly drop your belly towards the floor and lift your head and tailbone towards the ceiling (cat position). Hold for 2-3 seconds.
- Continue flowing between the two positions, moving with your breath – arching the spine on the exhale (camel) and rounding the spine on the inhale (cat).
- Perform 5-10 slow, controlled repetitions between cat and camel, synchronizing your movements with your breathing pattern.
- In the camel position, avoid overarching by keeping your shoulders away from your ears.
- In the cat position, imagine lengthening the space between each vertebra as you round your spine.
- Keep your abdominal muscles engaged throughout the movement to provide stability for your spine.
Strengthening Exercises
Abdominal draw-in
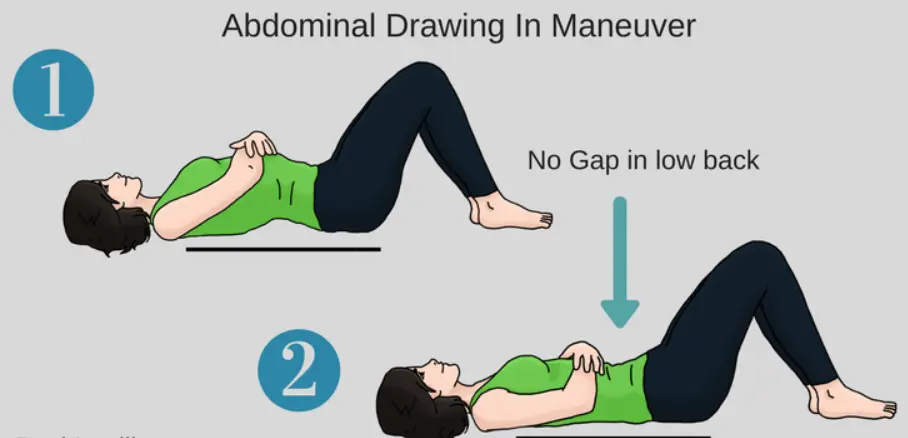
- Lay on your back with your feet flat on the ground and your knees bent.
- Activate the core by gently drawing the lower abdomen inwards away from the waist
- Maintain abdominal contraction as you slowly extend one leg straight out
- Keep opposite knee bent with the foot planted while straightening leg hovers just above the floor
- Slowly pull the bent knee towards the chest until a mild stretch is felt in the lower back
- Continue holding abdominal activation throughout motion ensuring the spine stays relaxed on the floor
- Hold knee to chest for 10-15 seconds then slowly lower foot back to start position
- Repeat the exercise bringing the opposite knee to the chest and completing 2-4 reps per side
This core strengthening progression incorporates hip flexor engagement simultaneous to stabilizing the spine for greater muscle coordination. The knee to chest mobilizes the lower back while the abdominal draw-in provides gentle traction and segmental control.
Abdominal draw-in exercise with heel slides

- Lie on your back with knees bent, feet flat about hip-width apart
- Activate core muscles by gently drawing the lower abdomen inwards
- Keeping spine stationary, slowly slide one heel out along the floor emphasizing control
- Make sure hips stay squared as the leg straightens then pull back in
- Repeat sliding the same heel out and in for 10 repetitions
- Switch to sliding the opposite heel out and in for 10 reps
- Work up to holding the abdominal contraction continuously while alternating sliding heels out
- Progress by straightening the sliding leg higher off the floor adding resistance
- Maintain stable neutral spine positioning throughout the slides
This core control sequence trains spinal stability while moving the legs. The abdominal draw-in maneuver engages the deep stabilizers providing segmental control. Heel slides strengthen hip mobility needed for transitional movements with spinal protection.
Double knee to chest
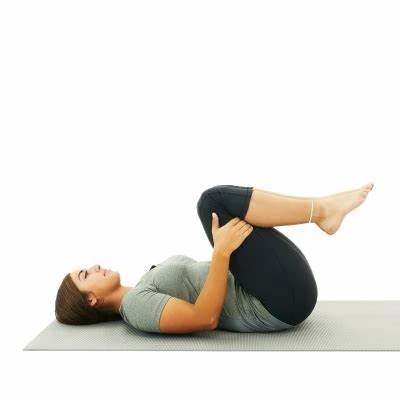
- With your arms at your sides and your legs outstretched, lie flat on your back.
- Activate the core by gently squeezing the abdominals inward
- Keeping spine stationary, bend both knees slowly pulling them vertically toward the chest
- Grasp under thighs below knees to hold legs in place
- With controlled movement, pull thighs closer to the body until moderate stretch felt in the lower back
- Maintain abdominal contraction keeping the spine relaxed into the floor
- Hold the double knee-to-chest position for 15-20 seconds breathing slowly
- Slowly lower both feet back to start position
Repeat the sequence 2-4 times engaging the deep core throughout the motion. Drawing abdominals inward while pulling knees to the chest provides spine decompression with stability – improving mobility and reducing pressure on degenerative discs.
Supine twist
- With your knees bent and your feet flat on the ground, lie on your back.
- Extend arms out to sides so they form a ‘T’ shape, palms facing up
- Keeping shoulders down, gently drop both knees slowly over to one side
- Rotate the head and upper back in opposite directions to create a twist
- Continue controlled twisting motion until stretch is felt through the spine
- Hold the stretch for 30 seconds being careful not to overrotate
- Slowly bring your legs back to the center then repeat the same stretch sequence to the opposite side
- Complete 2-4 repetitions stretching evenly to both sides
Remember to move slowly with control through the rotation. Do not force the range of motion or brace into discomfort which risks injury. This supine rotation loosens tight vertebrae and their connective tissues alleviating stiffness caused by degenerative disc compression and muscle tension.
Squats

- Place your feet shoulder-width apart and point your toes slightly outward while standing. Keep your spine in a neutral position.
- Inhale as you bend your knees and hips, sitting your hips back like you’re sitting in a chair. Keep your knees aligned over your ankles – do not let them cave inward.
- Descend until your thighs are parallel to the floor. Your knees should not pass far over your toes. Maintain weight in your heels.
- Engage your core by pulling your belly button toward your spine to keep your back straight. Avoid hunching or arched backs.
- Exhale then drive through your heels back to the starting position, squeezing your glutes at the top. Fully straighten your hips and knees at the top.
- Repeat for 10-15 controlled reps with proper form. Squats should be smooth and controlled on both the descent and ascent.
- If holding weights: Hold dumbbells at your sides or a barbell across your upper back. The weights should not cause you to lean forward. If so, decrease weight.
- Modify depth or use assistance if needed, but maintain proper alignment and hip/knee extension at the top.
Focus on proper technique over using heavy weight to maximize benefits and reduce injury risk. Start with body weight or light loads to master the movement pattern before increasing intensity.
Prone bridging exercise

- Lie face down supported by forearms and elbows
- Tighten abdominal muscles gently drawing the belly button up away from the floor
- Keep neck in line with spine, relax shoulders away from ears
- Exhale and slowly extend one leg behind you keeping hips level
- Hold bridge position for 5 seconds before lowering the leg and switching sides
- Build to holding the prone bridge on alternating legs for 30 seconds
- Progress by straightening both legs behind you supporting your torso only with elbows/toes
This core and back strengthening sequence trains essential stabilization needed for protecting vulnerable spine segments prone to excessive motion. Adjust hand placement closer or wider to scale difficulty. Always maintain neutral alignment without an overarching low back.
Superman’s exercise

- Lie face down on the floor or on an exercise mat with your arms extended straight out in front of you and your legs straight behind you.
- Keep your head, arms, chest, and legs relaxed on the floor to start. Engage your core by tightening your abdominal muscles.
- Inhale slowly then exhale as you simultaneously lift your arms, legs, and chest off the floor. Extend your arms straight out, reaching along with your fingers. Lift your legs straight back, squeezing your glutes and thighs together.
- Hold this contracted position, keeping your body in a straight line parallel to the floor for 2-3 seconds. You should feel the effort in your lower back, glutes, and hamstrings during this phase.
- Inhale again then slowly exhale as you lower back down, returning your arms, legs, and torso to the starting position on the mat.
- Repeat for 10-15 repetitions, taking breaks as needed between sets to reset proper form. Focus on controlled motions rather than speed.
- Breathe naturally throughout the exercise, exhaling as you contract and lift, and inhaling as you lower. Do not hold your breath.
Make sure to keep your abdominal muscles tightened and, your spine neutrally aligned without sagging hips or straining neck. Start with smaller sets and gradually increase reps over time for best results.
Quadruped opposite arm/leg exercise
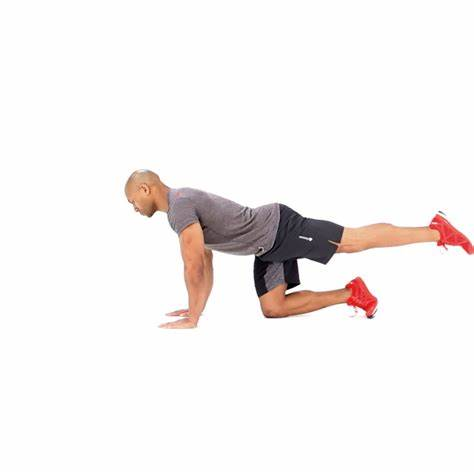
- Take a tabletop position and begin on your hands and knees. Immediately place your wrists under your shoulders and your knees under your hips.
- Pull your belly button in the direction of your spine to activate your core muscles. Throughout the exercise, maintain tensed abdominal muscles.
- Lift and extend your left arm forward in front of you while simultaneously extending your right leg straight back behind you. Reach your arm and leg as long as possible, keeping them as straight as you comfortably can.
- Hold this extended arm/leg position for 2-3 seconds, feeling the contraction in your back, abdominals, and glutes.
- Exhale and slowly lower your right knee and left hand back down to the starting position, maintaining stability in your core.
- Repeat the same motion on the opposite side, reaching forward with your right arm as you simultaneously kick back with your left leg.
- Continue alternating sides in a controlled manner. Move slowly rather than quickly.
- Complete 10-15 controlled repetitions on each side. Maintain level hips and a straight back throughout.
- Breathe naturally throughout the exercise without holding your breath. Keep your abdominal muscles engaged for core stability.
Make sure to keep the proper form to avoid straining your back. Start slowly and build on your endurance over time.
Press-ups

- Lie face down with palms flat under shoulders, legs straight behind
- Engage abdominal muscles by pulling the belly button up away from the floor
- Inhale then exhale pressing into palms to straighten your arms and lifting your chest
- Keep hip bones pressed down, and spine neutral without overarching low back
- Hold the top press-up position for 2 counts before slowly bending elbows to lower back down
- Progress by adding lower body movement – As the press upstarts, simultaneously pull one knee in towards the chest
- Alternate drawing knees in while performing press-up repetitions
- Start with 3 sets of 5-8 reps, resting and repeating sequence 2-3x weekly
This exercise strengthens arms, shoulders, spine extensors, and abdominals simultaneously. The controlled motion challenges the core stability required for protecting vulnerable lower back segments. Master form without compromising posture before advancing the degree of difficulty.
Prone cobra exercises

- Lie face down with palms flat under shoulders, legs straight behind
- Engage the core by gently drawing the lower abdomen up away from the floor
- On exhale, press into palms lifting your chest slowly off the floor
- Continue raising the torso while keeping the pelvis stationary and legs relaxed
- Lift chest only as high as comfortably possible avoiding overarching low back
- Hold the top of the cobra pose for 5 seconds breathing deeply
- On inhale, slowly return the chest to the floor then repeat
- Complete 10-12 reps, 3 sets resting between sets
This spinal extension exercise strengthens erector spinae muscles running parallel along the spine. Building extensor endurance better supports upright posture reducing compression through damaged lumbar discs. Move carefully within a non-painful range of motion.
Braces/Supports
- Custom-fitted rigid or flexible devices that restrict spine movement
- Limit painful motion segments allowing inflamed nerves and discs to heal
- Useful for unstable spines until core/back strengthening takes effect
- Help correct postural deviations and improper biomechanics
- Models available for lumbar, thoracic, and cervical regions
- May incorporate hot/cold therapy for additional pain relief
TENS Units
- TENS stands for transcutaneous electrical nerve stimulation
- Low voltage current interrupts pain signals reducing spinal and extremity pain
- Portable units are available allowing home use for consistent pain control
- Electrodes placed near nerves/tissues causing discomfort
- Various settings modulate frequency and intensity
- Can be used for 20-30 minute sessions 1-3 times per day
While effectiveness research varies, TENS risks are low making it a reasonable non-pharmacological treatment option. The devices can be combined with activity modification, manual therapy, and therapeutic exercise for DDD pain management.
Core Stability Exercise
Purpose
Core exercises strengthen the intricate web of muscles supporting the spine to improve stability and prevent excessive motion that further strains deteriorating discs.
Key Muscles Targeted
- Transversus abdominis
- Multifidus
- Pelvic floor
- Diaphragm
- Internal and external obliques
Goals
- Improve control of neutral spine posture
- Optimize alignment and weight distribution
- Develop muscle tension transfer for stability
- Decrease reliance on passive structures
- Gradually progress to functional movements
Approach
- Begin simple then make progressively more challenging
- Ensure proper breath training integrated
- Advance from isolation to integrated exercises
- Monitor for overexertion flare-ups
- Make specific daily life demands
Benefits
- Reduced recurrent injuries
- Less acute pain flare-ups
- Improved capacity for daily movements
- Enhanced spine and pelvis stabilization long-term
A tailored therapeutic program activating and strengthening core musculature offers lumbar spine decompression along with dynamic support reducing strain on damaged discs. The careful balance between rest and active recovery is key for long-term outcomes.
Postural Training
Postural Training Goals
- Learn and reinforce neutral spine alignment
- Strengthen core and back muscles to support good posture
- Increase body awareness to correct postural faults
- Practice posture in different positions – sitting, standing, lying down
- Integrate good posture habits into daily activities
Sitting Posture
- Keep ears, shoulders, and hips aligned vertically
- Engage core muscles to maintain a slight inward curve of the lower back
- Use a small towel roll or lumbar support at the lower back
- Keep feet flat and avoid crossing your legs
- Take frequent posture breaks to reduce prolonged loading
Standing Posture
- Distribute weight evenly on both feet
- Pull shoulders back slightly and keep the chin tucked
- Engage abdominal muscles to avoid swayback
- When standing for long periods, prop one foot up slightly
Sleeping Posture
- Sleep on a supportive mattress, may need a pillow under your knees
- Those with DDD often prefer sleeping on their side with a pillow between their knees
Regular practice of corrective exercises, stretches, and activities that remind proper spine alignment help ingrain postural habits. Good posture alleviates strain and allows the back to heal.
Prevention strategies for degenerative disc disease:
- Maintain proper posture and body mechanics: Poor posture puts more stress and strain on the back and discs. Make sure to stand up straight, avoid slouching or hunching over, and use good body mechanics when bending, lifting, sitting, etc. This helps reduce excessive forces on the discs.
- Lose weight if overweight: Extra body weight puts more pressure on the spine and discs. Losing weight minimizes stress on the back and reduces the risk of disc issues. Even losing 5-10 lbs can make a difference. Follow a healthy diet and exercise plan for weight management.
- Exercise regularly: Low-impact aerobic exercises like walking, swimming, and cycling along with core strengthening and gentle stretching help nourish discs through improved blood flow. They also strengthen back muscles providing more support to the spine. On most days of the week, aim for 30 minutes of moderate activity.
- Practice stress management: Emotional and physical stress causes muscle tension affecting back support and straining discs over time. Try relaxation techniques, meditation, yoga, massage, etc. to keep stress in check. Maintaining a work-life balance also helps manage stress.
- Avoid activities that strain the back: Use proper techniques when lifting heavy objects. Avoid sudden twisting movements. Be careful with high-impact exercises and sports that jar the spine repeatedly. Make modifications when needed.
- Quit smoking: Smoking impedes blood flow denying nutrition to discs and other structures. It also leads to chronic cough causing intradiscal pressure and injuring discs over time. Quitting protects spine health.
- Address other medical conditions: Managing diseases like obesity, osteoporosis, arthritis, etc. reduces the risk of related spinal problems including disc degeneration as it minimizes mechanical wear and tear.
Home remedies that can help with degenerative disc disease
- Apply heat and cold therapy: Apply a heating pad or warm compress to the back for 15 minutes to relax muscles and increase blood flow. Follow with a cold pack for 10 minutes to reduce inflammation. Do this several times a day. You can also alternate hot and cold showers.
- Try topical pain relievers: Menthol, camphor, eucalyptus oil, capsaicin creams and gels provide cooling or warming sensations that help temporarily reduce back pain. Massage these over the sore area 2-3 times per day.
- Consider over-the-counter pain medications: Oral NSAIDs like ibuprofen, naproxen or diclofenac tablets can alleviate swelling and discomfort associated with disc issues when taken as directed. Acetaminophen also eases general aches.
- Practice spinal stretches and exercises at home: Simple stretches like knee to chest, cat-cow pose, child’s pose, and spine twists along with low-impact exercises like walking help strengthen the core and relax tight muscles. Do them daily.
- Use supportive devices: Lumbar cushions, orthopedic seat cushions, back braces, and shoe insoles to help decompress the spine and improve posture reducing strain on compromised discs.
- Get adequate rest: Rest allows time for damaged tissues to heal. Set aside time to put your feet up and relax your back throughout the day. Sleeping on a firm mattress also helps support the spine overnight.
- Consider supplements: Anti-inflammatory herbs like turmeric, celery seed, Boswellia, and ginger help ease swelling and discomfort. Glucosamine and MSM provide building blocks for repair.
With a combination of conventional medical treatments and these home remedies, degenerative disc problems can be better managed.
Ergonomic and posture tips
Maintain good sitting posture
- Keep your head level, balanced straight over your torso – avoid poking your head forward or craning your neck which strains muscles.
- Shoulders should be relaxed, not elevated up near your ears. Draw them down and slightly back.
- Do not round your upper back – keep your chest lifted to support the upper/mid back curve.
- Support your lower back curve with a small pillow or roll up a towel if your chair does not provide lumbar support.
- Hips and knees should be at 90-degree angles. If your feet do not lie flat on the ground, use a footrest.
- Thighs should be parallel to the floor – avoid sitting with knees below your hip level.
- Maintain a neutral pelvis without tilting forward/back. Do not cross your legs which causes asymmetry and twisting.
Adjust your workstation setup
- Your screen should be an arm’s length away, placed directly in front of you at eye level.
- Use a document holder next to the screen at the same level if frequently looking from screen to paper.
- Push items you use most close to you to avoid overreaching.
- Elbows should form 90-100-degree angles when typing. Adjust seat height or use a wrist rest accordingly.
- Thighs should have clearance space between the chair front and the underside of the desk to prevent circulatory issues.
Lift properly
- Stand close to the load with a wide balanced stance with one foot slightly ahead for stability.
- Bend at hips and knees and tighten core muscles as you squat down keeping your back straight to pick up objects. Do not bend forward from the waist only.
- Let your strong leg muscles do the work. Use smooth motions avoiding any jerky twisting.
- Hold loads as close as possible to your body at belly button level to minimize lower back strain.
- Modified lifting options include getting help lifting heavy loads or using carts/dollies to roll items to avoid carrying the entire weight yourself.
- When placing items down, use the same technique in reverse, using leg strength to lift back up to standing.
Wear supportive shoes
- Choose quality athletic shoes for exercise/sports with proper arch support and cushioning in heel/forefoot areas. Stable tennis shoes are a good option.
- For work settings, wear leather shoes or sneakers with a rigid heel counter and flexible soles in the ball of the foot for ambulating tasks.
- Consider over-the-counter orthotics or custom inserts if you have flat feet, high arches, or other abnormal foot anatomy. Proper alignment helps back.
- Replace exercise/work shoes regularly every 6 months depending on the frequency of use to maintain adequate shock absorption and avoid injury.
- Avoid shoes with little cushioning or support like flat ballet-style slippers or flimsy flip flops to reduce jarring impact to the back.
The prognosis for degenerative disc disease (DDD):
- Symptom severity tends to fluctuate over time. Many people experience intermittent periods of worse pain followed by times when symptoms improve. Only about 10-15% of people have slowly worsening pain.
- With conservative treatment focused on pain relief, exercise, physical therapy, and lifestyle modifications, most people with DDD find their symptoms do not progress rapidly and their condition is maintained over many years.
- There is no cure for degenerative changes in spinal discs themselves. But for disc herniations and related impingement issues, symptoms often dissipate over time as bulging portions may retract or reduce in size through the body’s natural healing processes.
- Younger individuals tend to have better prognosis than older patients as age-related changes to the spine contribute to the degenerative process. People with otherwise good health also respond better to treatment.
- Stopping smoking and managing one’s weight through diet and exercise is extremely helpful for the long-term outlook, as obesity and smoking accelerate deterioration.
- While DDD cannot be reversed once disc tissues lose integrity, the progression of the condition can be slowed significantly when proper self-care strategies are implemented consistently under a doctor’s supervision.
- With treatment, only about 15-20% of degenerative disc patients end up needing surgery. Those who do opt for surgery usually see significant improvement in symptoms.
So in summary, while DDD is a chronic, progressive condition, most patients have a relatively positive prognosis for the management of symptoms and maintenance of function over time.
Summary
Degenerative disc disease (DDD) is an age-related spinal condition causing gradual deterioration of the discs between vertebrae. As the spine’s shock-absorbing pads wear down from natural aging, genetic predispositions, injuries, and lifestyle factors, painful inflammation, numbness, and nerve compression can occur.
Symptoms like chronic back soreness, stiffness, radiating leg pain, and numbness/tingling tend to develop slowly before escalating and impacting mobility. Diagnosis often involves imaging tests like MRI scans best at visualizing disc bulging and nerve inflammation.
Early conservative treatment focuses on pain and inflammation reduction along with gentle stretching and core/back muscle strengthening to stabilize vulnerable sections of the spine. Custom braces may provide external support if instability exists. Surgery like spinal fusion is an option if intractable pain or weakness persists despite exhaustive nonsurgical options.
Prevention plays a key role in mitigating age-related spinal decline. Improvements in posture, lifting mechanics, fitness, nutrition, and lifestyle habits all help maintain back health and stay active despite degenerative changes. Though DDD cannot be cured, symptomatic management helps patients remain productive and fully engaged in life’s activities.
In summary, a multi-disciplinary approach combining targeted exercise, manual therapy, pain medications, bracing, ergonomic education, weight management, and positive lifestyle changes tailored to each patient offers the best long-term outcomes for managing degenerative disc disease.
FAQs
What causes degenerative disc disease?
Factors like aging, genetic predisposition, and repetitive strain or injury to the spine over time can cause the discs between vertebrae to break down, resulting in pain and other problems.
What are the most common symptoms?
Common symptoms include chronic lower back pain that may radiate into the leg, stiffness, muscle spasms, numbness/tingling, and impaired mobility or flexibility in the back. Pain tends to increase with sitting, bending, lifting, etc.
Can DDD be cured?
There is no cure for the degenerative changes to the discs themselves. However, with treatment, most patients achieve good management of pain and maintenance of function over the long run.
What are the treatment options?
Conservative treatment like NSAIDs, heating pads, lumbar support brace, physical therapy, epidural steroid injections, etc can effectively treat degenerative disc problems in over 80% of cases. Surgery like spinal fusion or disc replacement may be an option in severe cases not responsive to other therapies.
What lifestyle modifications help manage DDD?
Losing weight, exercising regularly, practicing good posture, lifting correctly, managing stress, and quitting smoking all help reduce strain and progression of degenerative disc disease.
Does DDD lead to arthritis?
As discs lose cushioning ability, it can cause rubbing of bone surfaces possibly leading to the formation of bony spurs and degenerative arthritis in later stages.
What makes the outlook worse?
Being obese, sedentary lifestyles, structural back problems, occupational overuse, and smoking all negatively impact prognosis and result in faster degeneration of the spine.
Does DDD raise the risk for other conditions?
DDD may increase susceptibility to spinal stenosis, herniated discs, pinched nerves, muscle loss, and even slight spinal instability if degeneration is significant.
References
Professional, C. C. M. (n.d.). Degenerative Disk Disease. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16912-degenerative-disk-disease
Degenerative Disc Disease. (n.d.). Physiopedia. https://www.physio-pedia.com/Degenerative_Disc_Disease
Giorgi, A. (2023, January 25). What Is Degenerative Disc Disease? Verywell Health. https://www.verywellhealth.com/degenerative-disc-disease-7091203
Dhameliya, N. (2021, October 22). DEGENERATIVE DISC DISEASE (DDD) : Physiotherapy Treatment –. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/degenerative-disc-disease-2/
Prajapati, D. (2023, June 28). Best Exercise For Degenrative Disk Disese. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/best-exercise-for-degenrative-disk-disese/
Friedland, D. (2020, February 28). Safeguard Against Degenerative Disc Disease With These 3 Ergonomic Chairs – Welp Magazine. Welp Magazine. https://welpmagazine.com/safeguard-against-degenerative-disc-disease-with-these-3-ergonomic-chairs/#:~:text=Safeguard%20Against%20Degenerative%20Disc%20Disease%20With%20These%203,3%20%233%20Hbada%20Ergonomic%20Office%20Recliner%20Chair%20
Cpt, A. A. (2023, May 16). How Can I Prevent Degenerative Disc Disease From Getting Worse? Verywell Health. https://www.verywellhealth.com/preventing-degenerative-disc-disease-4137233
https://th.bing.com/th/id/OIP.shds8omIsvZDjPupkCVXpwHaDP?rs=1&pid=ImgDetMain


[…] Degenerative disc disease: The progressive degeneration of the spinal discs, which may be a factor in the development of sciatica. […]