Cervical Spine
The first seven vertebrae of your spine make up your cervical spine. It supports the weight of your head, covers and protects your spinal cord, and permits a variety of head movements.
This region of your spine is impacted by a number of illnesses, such as stenosis, degenerative bone and disk disease, arthritis, and neck pain. There are numerous alternatives for treatment.
What is the cervical spine?
The cervical spine, or neck region of the spine, is made up of seven vertebrae, which are stacked bones. Your cervical spine’s first two vertebrae are distinct in both form and function. The atlas, or first vertebra (C1), is a ring-shaped bone that starts at the base of your skull.
Atlas, a figure from Greek mythology, is the inspiration behind the name Atlas. Your head is held upright by the atlas. The atlas can hinge against your second vertebra (C2), sometimes referred to as the axis, to enable side-to-side “no” rotation of your head.
Your neck may move forward, backward, and rotate because of a type of joint called a facet joint, which connects your seven cervical vertebrae (C1 to C7) at the back of the bone.
Additionally, tendons, ligaments, muscles, and nerves surround your cervical spine. Intervertebral disks are “shock-absorbing” disks that are positioned in between each vertebra. Your entire spine is centered on your spinal cord. Your brain, which regulates every element of your body’s operations, communicates with your spinal cord.
Functions of Cervical Spine
There are many functions for your cervical spine, such as:
Protecting your spinal cord:
The central vertebrae of your body contain a large opening known as the vertebral foramen, through which the spinal cord’s nerves travel. This opening originates at the base of your skull and continues through the cervical, thoracic, and ends between the first and second lumbar (lower back) vertebrae. Your spinal cord is protected by the protective central canal formed by the overlapping of all the vertebrae in your spine.
Keeping your head supported and enabling movement:
Your head weighs between 10 and 13 pounds on average, and your cervical spine bears this weight. It also permits you to bend your head and neck to one side (ear-to-shoulder; lateral flexion), rotate from side to side, and tilt forward or backward.
Giving the vertebral arteries a secure pathway:
Vertebral arteries supply blood to the brain through tiny openings in cervical spine vertebrae C1 through C6. In the entire spine, this is the sole segment of vertebrae where arteries can travel through pores in the bone.
Muscles and soft tissues in the neck:
The following are other structures that surround or are related to your cervical spine:
Muscles in your neck that support your spine
The following are the main muscles that attach to your cervical spine:
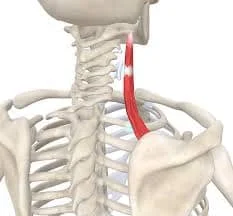
The sternocleidomastoid.
This muscle, one on each side, runs from behind your ear to the front of your neck. It is attached to the collarbone and sternum, the breast bone. You can tilt your chin forward and rotate your head from side to side thanks to this muscle.
Trapezius.
From the base of your brain, through your cervical and thoracic spine, and out to your shoulder blade, lie these two triangle muscles. They assist in raising your shoulder blade, rotating your head to the left or right, and tilting your head forward or backward.
Levator scapulae.
This muscle is attached to the top of your shoulder blade (scapula) and your first four cervical vertebrae. It facilitates rotating your head, bending your head to the side, and raising your shoulder blade.
Erector spinae.
This muscle group is composed of several muscles. These muscles aid in posture, neck rotation, and backward neck extension in the cervical spine.
Deep cervical flexors.
Along the front of your cervical spine are these muscles. They support the stability of your cervical spine and let you flex your neck forward.
Suboccipital muscles.
The base of your head and the top of your cervical spine are joined by these four muscle pairs. You may turn and extend your head using them.
Ligaments of your cervical spine
Your cervical spine’s ligaments, which join bone to bone, aid in maintaining the stability of your neck. There are three main cervical spine ligaments:
Anterior longitudinal ligament.
This ligament runs down the front of the cervical vertebra from the base of your skull. It stretches to prevent the neck from moving backward.
Posterior longitudinal ligament.
This ligament runs the length of your cervical vertebrae, beginning at C2. It stretches to prevent the neck from moving forward.
Ligamentum flava.
The back side of each vertebra’s internal opening, through which your spinal cord runs, is lined with these ligaments. Your spinal cord is covered and protected from behind by these ligaments.
Disks in the cervical spine
The “shock absorber cushions” in between each vertebra are called cervical disks. There are seven cervical vertebrae, with six disks altogether (one between two vertebrae). The disks not only protect your neck from strains but also make it easier for you to flex and rotate your head when exercising.
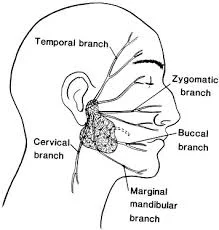
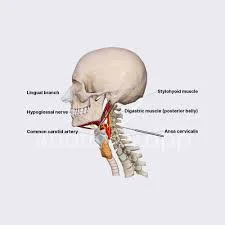
Nerves in the cervical spine
In your cervical spine, eight pairs of spinal nerves leave through tiny holes called foramen between each pair of vertebrae. They carry the codes C1 through C8. They provide you with feeling and activate the muscles in your hand, arm, shoulder, and neck.
Your head and neck movements can move forward, backward, or sideways thanks to the C1, C2, and C3 cervical nerves. Your head’s upper region is sensed by the C2 nerve, whereas the sides and back of your head are sensed by the C3 nerve.
One of the nerves that regulates your diaphragm, or the breathing muscle at the base of your rib cage, is the cervical nerve 4. It also governs your upward shoulder motion. Certain areas of your neck, shoulders, and upper arms are sensed by C4.
Your biceps and shoulders’ deltoid muscles are under the control of the cervical nerve 5. Sensation is supplied to the upper arm down to the elbow by C5.
Your wrist extensor muscles and your biceps are both under the control of the cervical nerve 6. Your forearm, hand, and thumb side are all sensed by C6.
Your wrist extensor muscles and triceps are under the control of the cervical nerve 7. C7 gives your middle finger and the back of your arm a feeling.
The pinky side of your hand and forearm are sensed by cervical nerve 8, which also controls your hands.
spinal column
A bundle of nerve tissue called the spinal cord connects the base of your brain to the rest of your body. It transmits signals from your brain to the aforementioned muscles.
Clinical Importance
Issues with the cervical spine and the surrounding soft tissues and nerves lead to a number of diseases and disorders. Among them are:
Cervical radiculopathy
When a cervical nerve is compressed by the cervical vertebrae, this disease develops. You might feel pain, tingling, numbness, and weakness. You may have localized symptoms or ones that affect your entire arm, hand, and fingers. Another name for cervical radiculopathy is pinched nerve or cervical nerve compression.
Neck pain
One of the most prevalent signs of a wide range of illnesses and injuries is neck pain. Meningitis, rheumatoid arthritis, cancer, growths (tumors, cysts, bone spurs), whiplash, emotional stress, physical strain, bad posture, and degenerative disorders (osteoarthritis, spinal stenosis, herniated disk, pinched nerve) are among the common causes.
Cervical degenerative disk disease.
When the disks in your cervical spine deteriorate, you can develop cervical degenerative disk disease.
Herniated disk.
This disorder is caused by a rupture or leak in the disks that act as a cushion between the vertebrae. Intervertebral disks make it easy for you to move and bend.
Cervical osteophytes (bone spurs in the cervical spine)
Growths called bone spurs can develop on any one of the cervical spine’s seven vertebrae.
Cervical spondylosis.
Your cervical spine’s disks and joints slowly deteriorate with age, a condition known as cervical spondylosis or arthritis of the neck.
Cervical spinal cord injury.
An injury to your cervical vertebrae is known as a cervical spinal cord injury. The majority of spinal cord injuries are caused by a violent, unexpected blow to the vertebrae.
Cervical spinal fracture.
A vertebral fracture can occur from a burst fracture (a vertebra crushed in all directions), a compression fracture (usually from mild trauma in an osteoporosis patient), or a fracture-dislocation (mainly from car accidents or falls from heights).
Cervical spinal cord compression (cervical spondylotic myelopathy).
This is a condition where the cervical region of your spine is compressing your spinal cord. Osteoarthritis, a disorder caused by wear and tear on the spine’s bones, is one of the most frequent reasons.
Cervical spinal tumor and cancer.
Unusual tissue growths inside your spinal column are called tumors. They could be malignant, or cancerous, or benign, or neither.
Meningitis.
An infection of the meninges is called meningitis. The lining that surrounds your brain and spinal cord is called the meninges.
Osteomyelitis.
A bacterial or fungal infection of the bone, in this case the vertebrae in your spine, is called osteomyelitis. Vertebrae may die if treatment is not received.
How are cervical spine disorders and diseases diagnosed?
Prior to beginning any treatment, your doctor will review your medical history, ask you about your medications, conduct a physical examination, order tests, and do imaging investigations.
Imaging and tests could involve:
CT scan, or computed tomography. This scan creates extremely tiny “slices” of the area being examined using X-rays and computers. Your spinal canal’s size, shape, contents, and surrounding bone can all be seen on a CT scan. It aids in the diagnosis of osteophytes, bone spurs, bone fusion, and tumor- or infection-induced bone deterioration.
Magnetic resonance imaging (MRI).
This test creates detailed images using radio waves, a computer, and a big magnet. This scan can identify malignancies, spinal degeneration, disk herniation, infections, and issues with your spinal cord and nerves leaving the spinal column.
X-rays.
X-rays use a tiny quantity of radiation to produce images of your soft tissues and bones. X-rays can reveal arthritis, disk issues, fractures, and issues with spinal alignment.
Electromyogram (EMG) and nerve conduction studies.
An EMG aids in assessing the condition and functionality of muscles and nerves. The speed at which an electrical impulse passes through your nerve is measured during a nerve conduction investigation. These examinations aid in identifying the location of nerve compression and any ongoing nerve damage.
Myelogram.
This imaging examination delineates the spinal cord and the nerves that leave your spinal column, as well as the interaction between your vertebrae and disks. It indicates whether anything that could be causing pain, numbness, or weakness is your spinal cord, nerves, or nerve roots—such as a tumor, bone spurs, or herniated disk.
How are conditions involving the cervical spine treated?
Many of the diseases affecting the cervical spine can be treated with both nonsurgical and surgical methods. The decision is based on the severity and underlying cause of the cervical spine problem.
What nonsurgical methods are available for treating disorders of the cervical spine?
If you have neck pain that isn’t related to a tumor or trauma, your doctor might first suggest less invasive methods. Typical nonsurgical treatment choices include the following:
- Rest.
- Ice or heat.
- A soft cervical collar: Your neck is supported and immobilized by a collar.
- Stay away from physically demanding or uncomfortable activities.
- Regular Physical therapy.
medication, such as analgesics (acetaminophen), muscle relaxants, and anti-inflammatory drugs (ibuprofen and naproxen).
Steroid injections.
For arm and/or neck pain, two particular kinds of steroid injections may be taken into consideration. The process of injecting a steroid into the epidural space—the area close to your spinal cord’s covering—is known as a cervical epidural block. A cervical facet joint block involves injecting a steroid into the facet joint’s capsule, which is the connective tissue covering that covers the tiny joint that joins the top and bottom of each vertebra to allow for motion.
Radiofrequency therapy and medical branch block.
Some people with persistent neck pain may be candidates for this surgery. Initially, a local anesthetic is administered into the nerve supplying the vertebral facet joint. Making pain relief permanent is the next step if it has been alleviated. This is accomplished by using a procedure known as radiofrequency ablation to injure your nerve. Months pass as the pain is relieved. Your nerve may grow back and cause discomfort again.
How can I find out if I qualify for surgery on my cervical spine?
A cervical spine surgery may be appropriate for you if:
- Other therapies don’t work.
- Your arms, legs, and/or spine-related symptoms are getting worse.
- It’s safe for you to get surgery.
What surgical treatments are available to treat problems of the cervical spine?
Typical surgical methods include:
surgery for cervical spinal decompression
The term “cervical spinal decompression surgery” refers to a broad range of operations intended to ease symptoms resulting from compression or pressure on your spinal cord or nerve roots. The initial portion of a nerve that emerges from your spinal cord via the tiny spaces between your vertebrae is called a nerve root.
Typical surgical methods for decompression consist of:
Cervical diskectomy
In order to relieve pressure on the adjacent nerve roots, your surgeon will remove a part of a disk during this treatment.
Cervical laminotomy or laminectomy.
During these operations, the lamina, a tiny portion of the spinal canal’s bony arches, is removed by your surgeon. A laminotomy removes only a little portion of the lamina. During a laminectomy, the entire lamina is removed, along with any disk material, bone spurs, and thickened ligament that may be necessary. Pressure is released by enlarging the spinal canal after the lamina is removed.
Cervical foraminotomy or foraminectomy.
By extracting some bone in that location, both of these treatments enlarge the apertures through which your spinal cord’s nerve roots can exit. A foraminectomy removes a significant amount of bone.
Cervical corpectomy.
To relieve pressure on the spinal cord, your surgeon will remove the disk and the body of the vertebra, which is the massive front section of the vertebra. To maintain the stability of your cervical spine, fusion of the vertebrae—a permanent joining of two or more vertebrae—may occur in certain situations after this.
Cervical disk replacement surgery
During a cervical disk replacement procedure, a diseased cervical disk is removed and replaced with an artificial disk. Cervical disk deterioration is the procedure’s most frequent cause.
Cervical spinal fusion
A surgical procedure known as cervical spinal fusion involves permanently joining one or more cervical vertebrae. The mobility between the vertebrae is eliminated after surgery.
Functional electrical stimulation for spinal cord injury
Your upper body muscles that are controlled by your cervical nerves will once again work thanks to this therapy, which employs tiny electrical impulses to activate particular muscles and nerves.
Is it possible to undergo minimally invasive cervical spine surgery?
Consult your surgeon. Minimally invasive spine surgery is an option in many circumstances. Minimally invasive surgery is carried out through one or more minor incisions as opposed to the single major incision made through your skin during traditional open surgery. Compared to a single lengthy incision, working through tiny incisions significantly lessens injury to soft tissues and muscles.
Conclusion
The neck portion of your spinal column, or backbone, is called the cervical spine. Your first seven bones (C1–C7) make up this structure. The muscles, tendons, ligaments, spinal cord, intervertebral disks, and nerves are additional components in or surrounding your cervical spine. Your cervical spine facilitates a broad range of head movement and carries the weight of your head.
Additionally safeguarding your spinal cord is its circular bone surround. Cervical spine illnesses and diseases can affect you in many ways. Thankfully, these problems can be treated with a variety of surgical and nonsurgical treatments.





29 Comments