Introduction
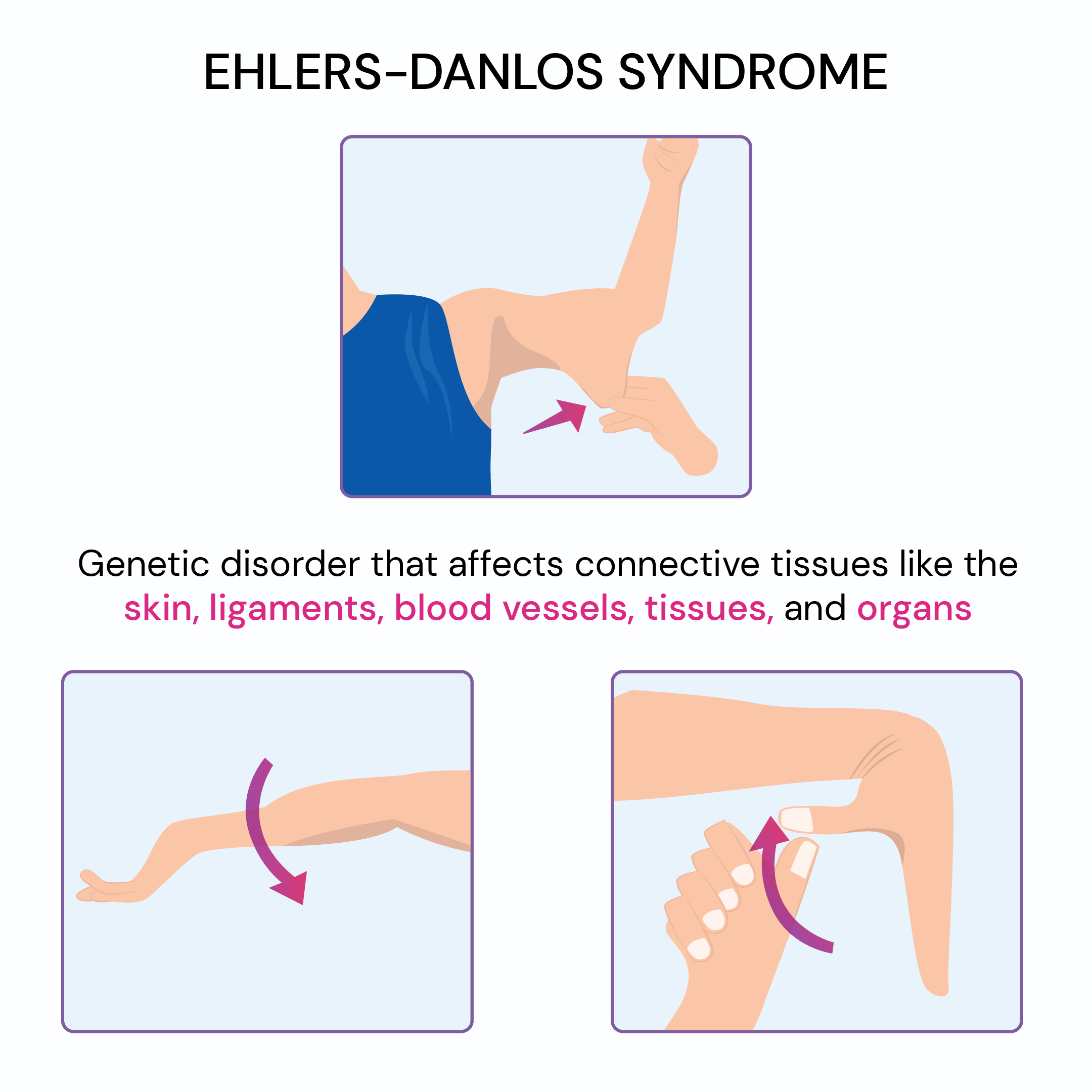
A genetic disorder called Ehlers-Danlos syndrome causes your body’s connective tissue to be weaker than it should be. It typically affects the joints and skin. Although there isn’t a cure, your doctor can help you find ways to manage your symptoms and avoid possible negative side effects.
An inherited group of diseases affects mainly the blood vessels, joints, and skin. The connective tissue of the skin, joints, and blood vessel walls is affected by Ehlers-Danlos syndrome. The skin is translucent, elastic, and prone to bruises. The joints are excessively flexible and can dislocate. In specific situations, the main blood vessels may dilate or even burst. Management of symptoms and observation for complications is assisted by treatment. Medicines, physical therapy, and sometimes surgery are options.
What is a Ehlers-Danlos Syndrome?
A set of hereditary conditions known as Ehlers-Danlos syndrome mainly affects the connective tissues in your body, such as the skin, joints, and blood vessel walls. The complicated mixture of proteins and other materials that make up connective tissue gives the underlying structures in your body their strength and flexibility.
People with stretchy, fragile skin and excessively flexible joints are common characteristics of Ehlers-Danlos syndrome. Having a wound that needs stitches may be a challenge as the skin is frequently not strong enough to support the stitches.
Vascular Ehlers-Danlos syndrome is a more severe form of the disorder that can result in ruptures of the uterine, intestinal, or blood vessel walls. Before starting a family, you might want to speak with a genetic counselor about vascular Ehlers-Danlos syndrome because it can cause major potential complications during pregnancy.
You may have Ehlers-Danlos syndrome in any connective tissue in your body, such as your:
- Cartilage.
- Bones.
- Blood.
- Fat.
Your symptoms from EDS may be felt in the following areas of your connective tissue:
- Skin.
- Joints.
- Muscles.
- Blood vessels.
A hereditary condition is Ehlers-Danlos syndrome. If you believe someone in your biological family has EDS, speak with a healthcare professional about getting tested (an immediate relative like a biological parent, grandparent, or sibling).
Symptoms of Ehlers-Danlos Syndrome
Ehlers-Danlos syndrome comes in a variety of forms, but the following are the most typical indications and symptoms:
- Bruising easily or more often than usual.
- Abnormal scarring or an unusually prolonged healing period following a cut or minor wound.
- Joint and muscle pain.
- Fatigue (feeling tired all the time).
- Difficulty concentrating.
- Overly flexible joints. Your joints have a wider range of motion (ROM) because the connective tissue that maintains them together is looser. Joint pain and dislocations are common.
- Stretchy skin. Skin that has weaker connective tissue can stretch much beyond its normal limits. If you manage to pull a small portion of skin away from your body, it will immediately return to its original position when you release it. Your skin might also feel exceptionally soft and velvety.
- Fragile skin. Damaged skin often doesn’t heal well. For example, it is common for the stitches used to close a wound to come out, leaving a gaping scar. These scars may look thin and crinkly.
Depending on the particular form of Ehlers-Danlos syndrome you have, the severity of your symptoms may differ from person to person. The hypermobile Ehlers-Danlos syndrome is the most common form.
Main types of Ehlers-Danlos syndromes (EDS)
- There are thirteen types of EDS, most of which are rare.
- Hypermobile EDS (hEDS) is the most typical type.
- Classical EDS, vascular EDS, and kyphoscoliotic EDS are other forms of EDS.
Hypermobile EDS
People with hEDS may have:
- joint hypermobility
- flexible, unstable joints that dislocate easily
- joint pain and clicking joints
- excessive tiredness (fatigue)
- skin that contusions easily
- digestive issues, such as heartburn and constipation
- dizziness and a raised heart rate after standing up
- issues with internal organs, such as mitral valve issues or organ prolapse
- difficulties with bladder control (urinary incontinence)
Currently, there are no examinations to confirm whether someone has hEDS. A physical examination and the patient’s medical history are used to make the diagnosis.
Classical EDS
Classical EDS (cEDS) is less typical than hypermobile EDS and tends to affect the skin more. People with SIDS may have:
- joint hypermobility
- loose, unstable joints that dislocate easily
- stretchy skin
- Especially over the forehead, knees, shins, and elbows, delicate skin that splits readily
- smooth, velvety skin that bruises easily
- wounds with broad scars and a slow healing rate
- hernias and organ prolapse
Vascular EDS
Vascular EDS (vEDS) is a rare type of EDS and is mostly considered to be the most serious. It involves the blood vessels and internal organs, which can cause them to break open and lead to life-threatening bleeding.
People with vEDS may have:
- skin that bruises very easily
- thin skin, especially on the legs and upper chest, with tiny blood vessels visible
- Delicate blood vessels that have the potential to rupture or bulge, causing severe internal bleeding
- a risk of organ problems, such as bowel tearing, womb tearing (in late pregnancy), and partial collapse of the lung
- hypermobile fingers and toes, impressive facial features (such as a thin nose and lips, large eyes, and small earlobes), varicose veins, and slowed wound healing
Kyphoscoliotic EDS
Kyphoscoliotic EDS (kEDS) is rare. People with kEDS may have:
- curvature of the spine – this begins in early childhood and usually gets more harmful in the teenage years
- joint hypermobility
- loose, unstable joints that dislocate easily
- weak muscle tone from childhood (hypotonia) – this may induce a hold in sitting and walking, or problem walking if symptoms get worse
- fragile eyes that can easily be damaged
- Skin that is soft, velvety, prone to bruises, and leaves scars
Hypermobility spectrum disorder (HSD)
Some people have problems generated by hypermobility but do not have any of the specific EDS conditions. They could be examined as a hypermobility spectrum disorder (HSD), which is managed similarly to hEDS.
Vascular Ehlers-Danlos syndrome
Individuals who have vascular Ehlers-Danlos syndrome usually share unusual facial features of a thin nose, thin upper lip, small earlobes, and prominent eyes. They also have very easily bruised thin, translucent skin. Fair-skinned individuals have highly visible blood vessels beneath their skin. For those with vascular Ehlers-Danlos syndrome, the aorta—the main artery in your heart—as well as the arteries that supply blood to other areas of your body may weaken. Any of these larger blood arteries has the potential to rupture and cause death. The risk of rupture may also increase if the vascular type weakens the walls of the uterus or large intestine.
Causes of Ehlers-Danlos syndrome
Many genetic factors, some of which are inherited and passed down from parent to child, are linked to different forms of Ehlers-Danlos syndrome. You have a 50% chance of passing on the gene to each of your children if you have the hypermobile form of Ehlers-Danlos syndrome, which is the most common form.
Complications
The types of symptoms and indicators you experience determine the complications. Joint dislocations and early-onset arthritis, for example, can be caused by excessively flexible joints. Prominent damage may occur on fragile skin. Individuals with vascular Ehlers-Danlos syndrome are prone to major blood vessel ruptures, which can be fatal. The intestines and the uterus are two examples of organs that can rupture. Uterine rupture is one of the risks associated with pregnancy. The most frequent complication of Ehlers-Danlos syndrome is dislocations.
The medical word for bones being forced out of their normal position in one of your joints is a dislocation. If you believe you may have a dislocation, never attempt to realign a joint by yourself. Visit the hospital’s emergency department as soon as possible. Surgery might be required to realign a dislocation. Blood vessel rupture (tear) can be a complication of vascular Ehlers-Danlos syndrome. Stroke and hazardous internal hemorrhage may result from this.
Additionally, organ rupture is more common in people with these forms of Ehlers-Danlos syndrome.
- Problems with the valves that push blood through your heart.
- Severe spine curvature (scoliosis).
- Thin corneas in your eyes.
- Bowed (curved) limbs.
- Teeth and gum problems.
Diagnosis
A family history of Ehlers-Danlos syndrome, extremely loose joints, and fragile or stretchy skin are frequently sufficient for a diagnosis. In rarer cases of Ehlers-Danlos syndrome, genetic testing on a blood sample can confirm the diagnosis and help rule out other conditions. There is no genetic testing available for the most common form of Ehlers-Danlos syndrome, hypermobile syndrome.
Your physician will likely start with a physical exam:
- Your ability to bend your fingers, knees, elbows, and waist will all be tested. Does your forearm meet your thumb? Does your pinkie have a maximum bend of 90 degrees?
- In addition to evaluating the entirety of your skin, they will pull to check for any scars left behind by the sickness.
- They’ll inquire about your medical background and whether you or any family members have ever experienced similar symptoms.
- An echocardiogram, which creates an image of your heart using sound waves, may be part of your examination if your doctor suspects you may have issues with your heart or blood vessels.
- Other imaging tests may also be given to you. To create a more comprehensive image, the physician may request a computerized tomography (CT) scan, which combines X-rays taken from various angles. As an alternative, they could request an MRI scan. Strong magnets and radio waves are used in this to create a detailed image.
- Your physician may also perform a biopsy. To do that, they will take a tiny sample of skin and examine it under a microscope for indications of abnormal collagen. Additionally, they might try to identify the type of EDS you might have by doing chemical tests on the sample. Certain genes that may be the source of the issue can be identified by other tests.
Treatment of Ehlers-Danlos syndrome
Ehlers-Danlos syndrome has no known cure, although medication can help you control your symptoms and prevent more problems. You can discuss how to manage your symptoms with your doctor once they have determined which form of EDS you have. You might need the help of a variety of doctors, such as:
- Orthopedics, a specialist in skeletal and joint issues
- A dermatologist, who treats skin conditions
- A rheumatologist, an expert in illnesses of the connective tissues
Some treatment options include:
- Exercise and physical therapy can improve coordination and muscle tone. You may be less likely to dislocate a joint if your muscles are stronger. Walking, low-impact aerobics, swimming, or cycling are a few beneficial workouts. In particular, physical therapy is crucial for kids with EDS.
- Moving around is made easier with the use of braces or other assistive devices, such as a wheelchair or scooter.
- You can strengthen your bones by taking calcium and vitamin D supplements.
- drugs available over the counter to relieve joint pain. You might require a prescription medication if those don’t work.
- Pregnant women with EDS may require special attention due to potential pain concerns.
Medications
Your physician may recommend medication to assist you in managing symptoms:
- Pain. Acetaminophen (Tylenol), ibuprofen (Advil, Motrin IB, etc.), and naproxen sodium (Aleve) are examples of over-the-counter pain relievers that are the basis of treatment. Only severe injuries should be treated with more powerful drugs.
- Blood pressure. Your doctor might want to keep your blood pressure normal and maintain the strain on your blood vessels because certain types of Ehlers-Danlos syndrome cause the blood vessels to be more delicate.
Physical therapy for Ehlers-Danlos Syndrome
Weak connective tissue increases the risk of dislocation in joints. The main course of treatment for Ehlers-Danlos syndrome involves strengthening muscles and stabilizing joints through exercise. Your physical therapist may suggest a particular brace to help avoid joint dislocations.
A splint is a device or support used to limit the range of motion in a particular body part. Ring splints aid in restricting movement in the finger joints, which are frequently excessively mobile in individuals suffering from hypermobility spectrum disorder (HSD) or a form of Ehlers-Danlos syndrome (EDS).
Ring splints can help with joint control, alignment correction, and finger and thumb stability. To lower the risk of injury and hand pain, ring splints can be helpful if you have unstable joint hyperextension, lateral (side to side) joint instability, dislocations, or subluxations.
Surgical and other procedures
Surgery might be suggested to fix joints that have been repeatedly dislocated or to patch up organ and blood vessel ruptures. However, because the stitches could tear through the fragile tissue, the surgical wounds might not heal correctly.
Lifestyle and home remedies
It’s critical to avoid injuries if you have Ehlers-Danlos syndrome. These are some precautions you can take for your safety.
- Choose sports wisely. Exercises like swimming, tai chi, recreational biking, walking, or using an elliptical or stationary bike are all beneficial options. Steer clear of contact sports, weightlifting, and other activities that put you at risk for harm. Reduce the amount of strain on your ankles, knees, and hips.
- Rest your jaw. To prevent your jaw joint, avoid chewing gum, hard rolls, and ice. Take recesses during dental work to close your mouth.
- Wear supportive shoes. To help control ankle sprains, wear laced boots with good arch help.
- Improve sleep. For sore joints, body pillows, and extremely deep foam mattresses can offer support and cushioning. Resting on your side may also help.
Coping and support
It’s difficult to deal with a chronic illness. Your ability to function at work, at home, and in interpersonal relationships may be affected by the severity of your symptoms. The following advice could assist you in adjusting:
- Increase your knowledge. Gaining more knowledge about Ehlers-Danlos syndrome will enable you to manage your condition. Search for a physician with expertise in treating this kind of illness.
- Tell others. Tell your boss, your friends, and family about your condition. If you believe any accommodations will help you be a more productive worker ask your employer about them.
- Build a support system. Establish a positive and compassionate relationship with your family and friends. Speak with a counselor or a member of the religious leaders may also be helpful. People can share common experiences and possible solutions to problems by participating in in-person or virtual support groups.
Helping your child cope
If your child has Ehlers-Danlos syndrome, you may want to try the following tips to support them:
- Maintain normalcy. Your child should be treated similarly to other kids. Request that your other grandparents, aunts, uncles, and teachers follow similarly.
- Be open. Even if your child expresses anger sometimes let them express how they feel about having Ehlers-Danlos syndrome. Make sure the carers, including your child’s teachers, are informed about your child’s condition. Examine with them as necessary
Promote safe activity. Encourage your kids to engage in physical activities within reasonable bounds. Encourage activities that don’t require lifting weights, like swimming, and prevent contact sports. Recommendations can be obtained from your child’s physician or physical therapist.
Risk factors
There are genetic forms of Ehlers-Danlos syndrome. It also means that the mutations can be inherited by offspring of biological parents. Other kinds are somatic; they occur at random and are not inherited by family members. If one or both of your parents have EDS, your chances of getting the condition may be higher. In a similar vein, if you have EDS, there’s a chance that your biological kids will inherit the mutation that caused it.
Consult a medical professional about the possibility that someone in your biological family will inherit or pass on Ehlers-Danlos syndrome to you. Your physician may recommend genetic counseling. Genetic counselors can assist you in assessing your likelihood of inheriting or developing specific conditions.
Prevention
It is not possible to avoid Ehlers-Danlos syndrome. There is no way to stop EDS because you cannot stop the genetic mutations that cause it. If you are concerned about passing on EDS (or any other genetic condition) to your biological children, speak with your healthcare provider about genetic counseling.
Prognosis
You will likely need to live with the symptoms of Ehlers-Danlos syndrome for the rest of your life. EDS has no known treatment. But once you learn how to manage your symptoms, you should be able to resume all of your regular activities. Certain types of intense physical activity (such as contact sports) may need to be avoided.
Each person with Ehlers-Danlos syndrome is affected differently. The type of EDS you have and the intensity of your symptoms will determine what you go through. Inquire with your provider about expectations specific to your circumstances.
What is the life expectancy of someone with Ehlers-Danlos syndrome?
The majority of Ehlers-Danlos syndrome types do not affect life expectancy and don’t reduce it. You may be more susceptible to a stroke or other serious vascular problems if you have vascular Ehlers-Danlos syndrome, a form of EDS that affects your blood vessels.
Your healthcare provider will work with you to find a course of treatment and lifestyle modifications that will help you live a safe, healthy life, even if you have vascular Ehlers-Danlos syndrome. See your doctor about what to anticipate and the warning signs and symptoms of potentially harmful complications.
FAQ
Which four symptoms indicate Ehlers-Danlos syndrome?
People with hEDS may have:
hypermobility of the joints.
joints that are unstable and prone to dislocation.
pressing and aching joints.
feeling extremely fatigued
skin that is prone to bruises.
Problems with digestion like constipation and heartburn.
feeling lightheaded and having a faster heartbeat after getting up.
What is Ehlers-Danlos syndrome life expectancy?
For those with vascular EDS, the median life expectancy is approximately 48 years. Individuals with kyphoscoliotic EDS, which is characterized by a hunched back and sideways curvature of the spine, may also have a shorter life expectancy.
How you can describe Ehlers-Danlos syndrome?
A group of inherited connective tissue disorders known as Ehlers-Danlos syndrome (EDS) is characterized by clinically atrophic scarring, fragility of blood vessels, hypermobility of joints, and hyperelasticity of the skin.
Can someone with EDS live a normal life?
Affected individuals with EDS can lead normal lives, though their mobility may be limited. A person suffering from vascular EDS is at risk for potentially fatal complications, such as rupturing an important blood vessel or organ.
What age is the typical diagnosis for Ehlers-Danlos?
It is not unusual for Ehlers-Danlos Syndrome to be diagnosed in a toddler because it can manifest itself at birth or very soon after. Examining their symptoms, family history, urine tests, and skin biopsies can all help achieve this. A cardiac ultrasound may be useful in certain situations.
Do the EDS people sleep more?
Studies have shown that patients with hypermobile EDS may have abnormal autonomic nervous system function. In addition, a lot of patients deal with exhaustion and chronic pain, which can interfere with sleep or make it harder to get enough good sleep.
References
- Ehlers-Danlos syndrome – Diagnosis and treatment – Mayo Clinic. (2022, August 25). https://www.mayoclinic.org/diseases-conditions/ehlers-danlos-syndrome/diagnosis-treatment/drc-20362149
- Professional, C. C. M. (n.d.-f). Ehlers-Danlos Syndrome. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17813-ehlers-danlos-syndrome
- Website, N. (2023, November 24). Ehlers-Danlos syndromes. nhs. uk. https://www.nhs.uk/conditions/ehlers-danlos-syndromes/
- Smith, M. (2017, March 5). What is Ehlers-Danlos Syndrome? WebMD. https://www.webmd.com/a-to-z-guides/ehlers-danlos-syndrome-facts
- National Organization for Rare Disorders. (2023, November 20). Ehlers Danlos Syndrome – Symptoms, causes, treatment | NORD. https://rarediseases.org/rare-diseases/ehlers-danlos-syndrome/

[…] Ehlers-Danlos syndrome and joint hypermobility syndrome are two examples of joint-related health problems. […]