Introduction
Cervical neck pain is a prevalent issue worldwide and constitutes a significant public health problem. According to a population-based study conducted in Canada, the lifetime prevalence of neck pain in adults is 66.7%, and 22.2% of Canadians reported neck pain on the day of the survey.
In Europe, annual neck pain prevalence ranges from 38% to 43% of the population. Neck pain is responsible for considerable medical and healthcare costs and is a leading cause of disability and dysfunction.
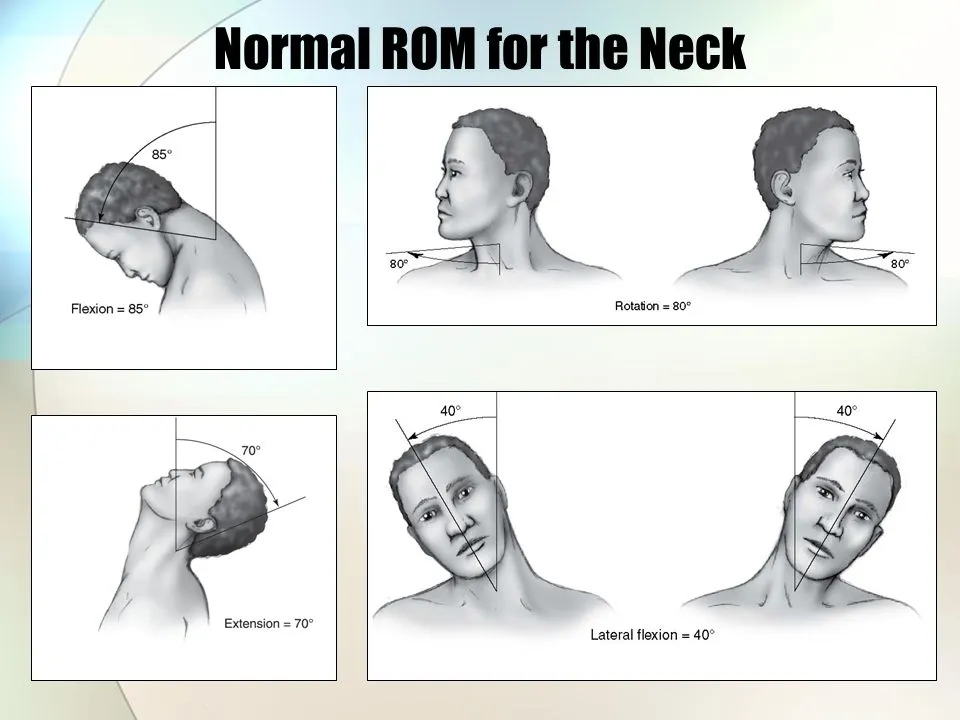
Individuals with neck pain typically exhibit weaker neck muscle strength and a smaller cervical range of motion (ROM) compared to those without neck pain. Neck muscle strengthening and ROM exercises are effective interventions for neck pain. Therefore, cervical muscle strength and ROM assessments are crucial clinical indicators of cervical function that can provide useful information for healthcare practitioners, including changes in status and treatment responsiveness.
Neck ROM refers to the degree of movement of all the joints within the cervical spine. Common clinical methods to assess cervical ROM include using a measuring tape, goniometers, inclinometers, and visual estimates. The digital inclinometer is reliable and valid compared to other methods such as measuring tape, goniometers, and visual estimates. While radiological images are considered the gold standard for cervical ROM measurement, they are not practical for monitoring recovery or setbacks in daily practice. Therefore, alternative methods such as cervical goniometers are preferred for establishing the validity of new ROM devices for clinical use.
Muscular strength has various operational definitions. According to Enoka’s definition, muscular strength is the magnitude of the torque exerted by a muscle or muscle group in a single maximal isometric contraction of unrestricted duration. Isokinetic and handheld isometric dynamometers are commonly used to measure cervical muscle strength.
Handheld dynamometers are preferred for clinical use due to their convenience and lower cost. In the absence of an isokinetic dynamometer, isometric handheld dynamometry has greater sensitivity than manual muscle testing, allowing clinicians to detect small to moderate changes in muscular strength.
The spinal vertebrae play a crucial role in anchoring limbs and the head, protecting the spinal cord, and serving as a significant attachment to the rib cage and torso muscles. Consequently, it is commonly referred to as the backbone. The different structural anatomy of the vertebrae gives rise to various functional anatomy and mobility properties, resulting in its vast functions. Therefore, examining different parts along the vertebrae may provide varying measurements and ranges of movement during clinical examination.
This article aims to provide a brief overview of available bedside instruments for examining cervical range of motion, including the goniometer, inclinometer, and cervical range of motion (CROM) instrument. However, this paper will not discuss additional signs that may be elicited from the cervical spine examination or associated neurological examinations of cervical spine nerve roots or extremities. Therefore, maneuvers such as Bakody’s sign and Jackson’s compression test will not be mentioned.
A complete examination of the vertebrae should always begin with a general inspection, followed by palpation, range of motion, and special maneuvers. However, this paper will focus primarily on assessing the range of motion of the cervical spine. It is important to remember that a thorough examination of the vertebrae should only take place if there is no sign of acute fractures or persistent spinal instability. In such instances, utmost caution should be exercised during spinal examination and movement, adhering to appropriate protocols relevant to such cases.
Posture
Observe the patient’s standing and sitting position. Postural deviations can be corrected as part of the study to determine the effect on the patient’s symptoms. Common postural abnormalities:
- Protracted cervical spine or forward head posture
- Protracted shoulder girdle and rounded shoulders
- Upper Thoracic Spine
- Kyphotic or Flexed
- Lordotic or Extended
- Normal
- Middle Thoracic Spine
- Kyphotic or Flexed
- Lordotic or Extended
- Normal
- Movement Tests
Functional Movement
Above all else, ask the patient to demonstrate the functional movement that most easily mimics their symptoms. The movement shown by the patient can provide many clues about the root cause of the problem as well as a good result based on performance.
Cervical AROM, PROM, and excessive pressure
Before the motion test, the examiner asks the patient about the location and intensity of the main symptoms. The examiner notes any changes in position or intensity during the test and where the movement occurs.
The examiner must assess the concentration of symptoms and the presence of the periphery during testing. Repetitive moves can be used as part of this assessment.
The patient underwent all cervical AROM tests (neck flexion, extension, rotation, and lateral flexion) while seated upright.
An inclinometer can be used to assess cervical range of motion testing. Reliability coefficients for cervical ROM measured with an inclinometer ranged from 0.66 to 0.84 (ICC). A universal goniometer is used to measure cervical rotation while sitting. Passive overpressure can be used at the end of the active movement to assess pain response and final sensation.
Combination movements: Cervical retraction is used to measure both lower cervical extension along upper cervical flexion. Upper and lower cervical extension is assessed by cervical elongation.
In the cervical quadrant, cervical extension is combined with ipsilateral rotation and lateral flexion.
Methods for cervical range of motion examination
No special equipment is needed for the general examination and physical examination of the cervix. However, the use of certain tools in the evaluation of the commercial area allows an objective and standardized evaluation during monitoring. Literary instruments used may include a tape measure, a tape measure, a flexible draftsman’s ruler, a fingertip method, a goniometer, an inclinometer, and a CROM device.
Since this document is specifically designed for bedside instruments, ancillary equipment such as x-rays, imaging, and motorized or electronic equipment such as digital goniometers and inclinometers, it should not be mentioned further. A link demonstrating the examination technique with bedside instruments can be seen at the following link:
Cervical flexion and extension
Ask the patient to sit upright in a chair with the thoracic spine against the back of the chair, and arms hanging from the chair. sides, and feet on the floor. Then observe the patient from the side. This position can be considered as 0°. To assess cervical flexion, ask the patient to lean forward and bring the chin to the chest. Normal cervical flexion is usually around 80º.
To assess cervical dilatation, ask the patient to look as far as possible until the neck is fully extended. The normal cervical extension is usually 50°. The cervical range of motion from full flexion to full extension should be 130°. However, it is possible to measure whether the patient has normal cervical flexion and whether the patient can touch the chest with the chin.
Tape Measure
The lower end of the sternal notch should be marked as a fixed point or reference point. Next, request that the patient extend and flex their neck. During maximum flexion and extension, measure the distance between the reference point and the jaw.
Inclinometer
Ascertain that the inclinometer reading is 0° by placing it atop the patient’s head in the sagittal plane. Next, request that the patient extend and flex their neck. Note the inclinometers at each end of the motion.
Goniometer
First, place the axis of the goniometer over the external ear canal. Place the fixed arm horizontally to the floor alternatively vertically. Direct the moving hand to the root of the nose. Mark it as 0°. Next, have the patient flex and extend their neck while you take readings with the goniometer at each extreme of the range of motion. The axle should remain in the external ear canal and the stationary hand should be vertical to the floor, but the moving hand should be redirected to the base of the nose.
CROM Instrument II
Place the CROM II on the patient’s head and make sure it fits by adjusting the strap. Take note of the goniometer’s measurement on the side of the head; with it in the neutral position, it should read 0°. Then ask the patient to flex and extend their neck, recording readings at each end of the range of motion.
Lateral cervical flexion
Ask the patient to sit upright in a chair with the thoracic spine against the back of the chair, arms hanging at the sides, and feet on the floor. Instruct the patient to look straight ahead, preferably at a specific point at eye level. Guard the patient. Take this as the starting point (ie 0°). Ask the patient to tilt the head laterally to the left without turning the head while keeping the shoulders still (ie, bring the ear as close to the shoulders as possible without raising the shoulders).
Investigators can help stabilize the shoulder position by gently placing their hands on the patient’s shoulders. Repeat the procedure on the opposite side and note the bending angle of the head. The normal bending of the starting point on each side is 45°, and the total angle of maximum lateral bending of the head should be 90°. The eye is difficult to look at, so using a goniometer or CROM device will help you accurately measure head tilt.
Tape Measure
The acromion process on each side must be fixed as a point or reference point. Then ask the patient to bend the neck to the side. During maximum side bending, measure the distance between the fixed point and the lowest point of the earlobe.
Repeat on the opposite side.InclinometerPlace the inclinometer on the patient’s head along the coronal plane and make sure the inclinometer reading is 0°. Then ask the patient to flex their neck laterally and record the inclinometers at each end of the range of motion.
Goniometer
First place the axis of the goniometer; Above the C7 vertebra when viewed posteriorly or the sternal notch when viewed anteriorly. Align the patient’s immobile arm along an imaginary line between the two acromion processes, either vertically or perpendicular to the floor or horizontally and parallel to the floor. Guide the patient’s moving arm; above the external occipital protuberance when examining the nose of the patient from behind, or in the middle when examining from the front.
Keep this position at 0°. Then instruct the patient to flex their neck laterally and record the goniometer readings at each end of the range of motion. Make sure the shaft and stationary arm stay in place during the movement and adjust the moving arm accordingly.
CROM Instrument II
Place the CROM Instrument II on the patient’s head and adjust the strap to ensure a secure fit. Take note of the goniometer’s reading on the forward side of the head, which in the neutral position ought to read 0°. Then instruct the patient to flex the neck laterally and record readings at each end of the range of motion.
Cervical Rotation
Place the CROM II on the patient’s head and make sure it fits by adjusting the strap. Take note of the goniometer’s reading on the other side of the head; with the head in the neutral position, it ought to indicate 0°. Then ask the patient to flex and extend their neck, recording readings at each end of the range of motion.
Lateral cervical flexion
Ask the patient to sit upright in a chair with the thoracic spine against the back of the chair, arms hanging at the sides, and feet on the floor. Instruct the patient to look straight ahead, preferably at a specific point at eye level. Guard the patient. Take this as the starting point (ie 0°). Ask the patient to tilt the head sideways to the left without turning the head while keeping the shoulders still (ie bring the ear as close to the shoulders as possible without raising the shoulders).
Investigators can help stabilize the shoulder position by gently placing their hands on the patient’s shoulders. Repeat the procedure on the opposite side and note the bending angle of the head. The normal bending of the starting point on each side is 45°, and the total angle of maximum lateral bending of the head should be 90°. The eye is difficult to look at, so using a goniometer or CROM device will help you accurately measure head tilt.
Tape measurement
The acromion process on each side must be fixed as a point or reference point. Then ask the patient to bend the neck to the side. During maximum lateral bending, measure the distance from the fixed point to the lowest point of the earlobe. Repeat on the opposite side.
Inclinometer
As you position the inclinometer along the coronal plane on the patient’s head, ensure sure the reading is 0°. Then ask the patient to flex their neck laterally and record the inclinometers at each end of the range of motion.
Goniometer
First place the axis of the goniometer; Above the C7 vertebra when examining posteriorly, or the sternal notch when examining anteriorly. Align the patient’s immobile arm along an imaginary line between the two acromion processes, either vertically or perpendicular to the floor or horizontally and parallel to the floor.
Guide the patient’s moving arm; above the external occipital protuberance when examining the nose of the patient from behind, or in the middle when examining from the front. Keep this position at 0°. Then instruct the patient to flex their neck laterally and record the goniometer readings at each end of the range of motion. Make sure the shaft and stationary arm stay in place during the movement and adjust the moving arm accordingly.
CROM Instrument II
Place the CROM Instrument II on the patient’s head and adjust the strap to ensure a secure fit.
Take note of the goniometer’s reading above the front of the head, indicating that the neutral position should be 0°.
Then instruct the patient to flex the neck laterally and record readings at each end of the range of motion..
Discussion for measurement of cervical ROM through goniometer
The range of motion can be assessed with the eyelid. However, this is a rough method of measurement and is prone to observer bias. Furthermore, it is not an objective, accurate, and reproducible measure of vertebral motion.
A meter is often readily available in clinics; it works by measuring changes in the distance the cervix moves from a specific part of the body. However, it is not suitable for measuring neck range of motion.
However, it is a reliable method for clinical assessment of cervical motion, excluding cervical dilatation. However, Koning et al. still question the reliability and validity of meter use because some studies are not blinded.
The inclinometer allows you to estimate the range of motion by measuring the difference in different angles of the head during movement. This is a simple method that only requires the use of one hand. It also shows good reliability and intraobserver agreement for cervical evaluation, but its validity remains questionable.
The goniometer is used to measure the angles of change associated with movements of the head, neck, and back. It is often used to measure joint angles in limbs.
Using a goniometer makes it possible to accurately measure the degree of movement of body joints. However, the examiner must use both hands to adjust the goniometer arms during the examination, so he cannot stabilize the patient’s neck during movement. However, there is a critical need to standardize the central axis of the joint for each movement, because changing the axis by different researchers leads to different results. A systematic review perpetuates fears about its reliability and validity. The CROM instrument consists mainly of goniometers and a compass attached to a rigid headband. As such, its position remains consistent and allows accurate measurement of head and neck range of motion.
The CROM instrument can be attached directly to the patient’s head and body, which eliminates the distraction of the examiner in addition to the need to determine a fixed point on the body. It is also easy to do during installation and does not require hands. It takes time to assemble and adjust to the size of the patient’s head. It is also more expensive than all the previously mentioned instruments, and its practicality for clinical use has been questioned.
Comparing the CROM instrument to other research methodologies, it has demonstrated strong validity and reliability based on considerable study.
Systematic reviews by Koning et al. and Yee Won et al. Due to its clinometric properties and practicality, we recommend using an inclinometer, goniometer, and CROM instrument. It is a reliable measuring method, much more than a simple visual assessment.
Discussion for measurement of cervical ROM through other devices
The CROM device measurements in this investigation for every cervical movement were quite close to the normative values for adults in the same age range (20–69 years) published by Youdas et al. 27.
The mean active cervical range of motion in this earlier investigation was, in fact, 67.1° in extension, 46.1° in flexion, 63.5° in right rotation, 61.3° in left rotation, 37.5° in right lateral flexion, and 36.0° in left lateral flexion. The results of our study show good concurrent validity of the CROM device compared to Fastrak.
The results showed that the correlation coefficients were 0.93 for flexion, 0.96 to 0.97 for bilateral flexion, and 0.98 for extension and bilateral rotation. These were higher than the correlation values reported in the only other study24 evaluating the validity of the CROM. We obtained somewhat higher correlation values, especially in the lateral directions of flexion and right rotation, which is probably due to methodological limitations about movement in these directions, as suggested by the study by Tousignant et al.
However, both studies confirm the validity of the CROM. dimensions. Good agreement between the 2 measurement units in all directions was also found by the calculated mean differences and limits of agreement. The distribution of points around the zero point within 95% agreement indicates that the CROM device can be used appropriately to replace a more expensive measuring device such as Fastrak.
It also shows that the test-retest reliability of CROM measurements is excellent according to Portney and Watkins criteria20, with ICC values ranging from 0.89 to 0.98 for all cervical measurements. Although we are the first to disclose different experiments, Hole et al.14 (0.86–0.96), Youdas et al.27 (0.73–0.95), and Fletcher and Bandy10 (0.87–0.94) have previously presented similar results. -retest reliability measures. days Comparing the reliability of measurements made with the CROM device to more sophisticated tools used in research, such as the OSI Spine Motion Analyzer (intratester ICCs, 0.78–0.94),19 the Zebris CMS system (intratester ICCs, 0.78–0, 93 ). ). either the CA6000 Spine Motion Analyzer (intratester ICCs, 0.75–0.92),17, or both, it may be said that the ICCs displayed by the CROM device are adequate. In addition, the CROM device has the advantage of ease of use in a clinical setting and portability, which enables rapid measurements both in the field and at home.
Compared to other personalized, rapid cervical ROM measurement techniques, the CROM device stands out as a very good tool that can be used in clinical settings to obtain more objective measurements than other currently used tools, such as visual assessment (intertester ICC, 0.42–0.82). , error estimated between 5° – 45°)3 and a universal goniometer (intertester ICC, 0.54-0.79; intratester ICC, 0.78-0.90),28 with lower reliability characteristics. Finally, the dependability of the data produced by the CROM is greater than that of the ordinary bubble inclinometer14,25, most likely as a result of the more standardized location on the head. CROM is more expensive, but both are very easy to use in a clinical context.
The use of standardized test methods was very important to ensure good reliability throughout the study. The sitting position of the subjects was kept unchanged from the beginning of the recording. In addition, 1 training trial per direction was performed before ROM measurement.
It was considered important to emphasize the instructions given to the subjects by reminding them subjects to isolate the head movements without moving the shoulders and body. Straps were very important in the Fastrak procedures to prevent movement of the chest and shoulders. Finally, on days 1 and 2, CROM measurements were taken every 48 hours, always at the same time of day, to eliminate effects due to variations in ROM at different times of the day.9 These precautions must be taken into account. when the CROM device is used in a clinical setting to ensure good reliability and validity of the procedures.
The computed SEM and MDC in this investigation ranged from 1.6° to 2.8° for SEM and 3.6° to 6.5° for MDC, which were reasonably low for all movements. These values are slightly lower than the 4,444 in the 4,444 Fletcher and Bandy study10 (SEM, 2.3°–4.0° MDC, 5.4°–9.3°), which again represented only measurements taken during the same session.
Some of the potential sources of error in our study may be because the CROM devices have display quadrants spaced at 2° intervals, which may have resulted in limited accuracy of reading ROM values. Other variations in the rotational movements measured with the CROM device may have been due to the repositioning of the quadrant when it was reset to the 0° position before each movement.
However, we can interpret our results as showing satisfactory agreement and responsiveness, which are important ingredients for the proper interpretability of measurements in a clinical setting. Based on this information about the minimum difference required for a true change in change, we can be confident that a change in cervical ROM greater than 6.5° in any direction is a true change.
Actual change must be distinguished from minimally significant change, which is associated with minimal improvement or worsening of the patient and condition obtained by comparing the change in postprocedural ROM with the patient’s self-report of overall observed change or disease. 7 Therefore, in clinical settings, it is recommended to use the CROM device together with other subjective and objective assessments of the patient and general condition to evaluate the outcome of the procedure.
Conclusion
The study’s findings support the validity of measurements taken on different days using the CROM equipment in other investigations. These results also showed relatively low SEM and MDC values with the CROM device in all six directions of motion at the cervical level. Knowing that the use of objective instruments is increasingly emphasized in clinical practice, this device can be recommended to measure cervical ROM both for research purposes and in rehabilitation. However, future studies involving patient groups should be conducted to confirm the present results.
A uniform and standardized method should be used to assess the motion of the cervical spine. In this way, interobserver variability can be reduced and reliable monitoring of cervical range of motion progression or impairment can be ensured. Finally, it is very important to perform a complete neurological evaluation of the upper extremities, especially brachial plexus testing to complement the cervical spine. Limb testing can help elicit signs of spinal cord injury (eg, Kernig’s and Brudzinski’s sign in meningitis).
The examination techniques must also be changed according to the patient, and it must always be ensured that the patient does not experience unnecessary pain or pressure during the examination of the vertebrae.
FAQs
How do you test for cervical range of motion?
An inclinometer can be used to assess cervical range of motion testing. Reliability coefficients for cervical ROM measured with an inclinometer ranged from 0.66 to 0.84 (ICC). A universal goniometer is used to measure cervical rotation while sitting.
What is the range of motion for the neck exam?
Range of motion refers to the ability of a joint to go through its full range of motion. It can be passive or active. Passive range of motion can be defined as that achieved when an external force, such as a therapist, causes the joint to move.
What are the cervical ranges of motion?
The range of motion of the cervical spine is approximately 80° to 90° flexion, 70° extension, 20° to 45° lateral flexion, and up to 90° rotation on both sides.
What is abnormal neck motion?
The painful disease known as cervical dystonia, often referred to as spastic torticollis, causes your head to twist or turn to the side due to an involuntary contraction of your neck muscles. Additionally, uncontrollably tilting the head forward or backward might be a symptom of cervical dystonia.
Why is a cervical range of motion important?
In particular, the vertebrae in the cervical spine are most closely connected to your spinal cord. By moving the muscles around your neck, you can encourage blood flow to the spinal cord and brain – the central parts of the nervous system. Increased circulation promotes the nervous system and healthy functioning.
References
- Tests for muscle strength as well as cervical range of motion are valid and reliable. The Journal of Strength and Conditioning Research. https://doi.org/
- An observational study found that the upper cervical range of rotation during the flexion-rotation test depends on age. Therapeutic Advances in Musculoskeletal Disease. https://doi.org/
- Assessing the Range of Motion within the Cervical Spine: Employing Different Bedside Instruments. The Medical Science Journal from Malaysia. https://doi.org/10.21315/mjms
- Cervical Examination. Physiopedia. https://www.physio-pedia.com/Cervical_Examination

[…] Decreased cervical range of motion […]