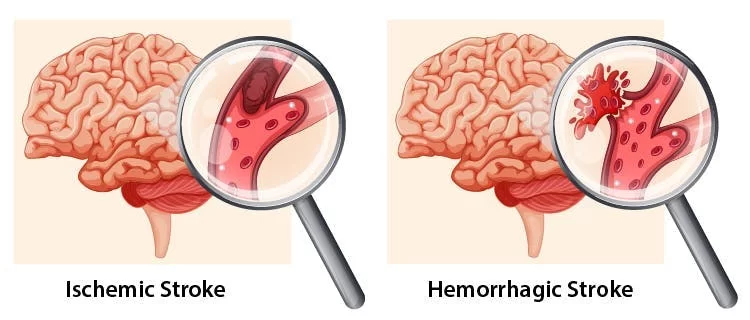
Hemorrhagic Stroke
- An uncontrollable bleeding hemorrhagic stroke occurs when there is bleeding within the brain or in the area between the brain and its outer layer. Since this type of stroke is particularly severe and may worsen, receiving medical attention is vital to preventing death or irreversible brain damage.
What is a Hemorrhagic Stroke?
- Hemorrhagic stroke, also pronounced “hem-or-aj-ick,” is a potentially fatal medical disorder caused by the burst and bleeding of a blood artery in the brain. This may interfere with blood flow in locations rich in oxygen. Additionally, the pressure of accumulated blood damages or destroys nearby brain regions.
- Because hemorrhagic strokes induce acute symptoms that worsen quickly, they are especially deadly. These strokes frequently result in death or irreversible brain damage if prompt medical assistance is not received.
- Important: Every second counts in the event of a stroke, which is a life-threatening emergency. You should call 911 (or your local emergency services number) as soon as possible if you or someone else you know is experiencing stroke symptoms. A stroke is more likely to result in death or irreversible brain damage the longer it is left untreated.
To identify the early indicators of a stroke, always remember to think quickly:
- The face is represented by F: Request a smile from the person. If you notice a droop on one or both sides of your face, it could indicate paralysis or weak muscles.
- The letter A stands for arm: One side of the body commonly experiences muscle weakness in stroke victims. Request that they lift their arms. Should they develop unilateral weakness (which they did not previously), one arm will remain up while the other would droop and descend.
- Speech is represented by the letter S: Speaking is frequently lost in victims of strokes. They could struggle to find the correct words to say or slur their sentences.
- The letter T stands for time: It’s urgent, so don’t put off getting assistance! Look at a clock or your watch, if you can, and try to recall when the symptoms first appeared. Providing your doctor with the exact date of onset of symptoms might help them determine the best course of treatment for you.
Types of Hemorrhagic Stroke
One of the following variables may lead to a hemorrhagic stroke:
- Internal bleeding (intracerebral): This results in internal bleeding within the brain, applying internal pressure to the surrounding brain tissue.
- Bleeding into the gap between your brain’s outer coating and subarachnoid membrane: The thin layer of tissue known as the arachnoid membrane surrounds your brain and gets its name from the pattern like a spiderweb on its surface. The subarachnoid space (the word “sub” means “under”) is the area that exists between that membrane and your brain. Bleeding from any blood vessels that break through the arachnoid membrane may cause the subarachnoid space to fill. This creates pressure from outside the brain itself inside your skull.
Symptoms of Hemorrhagic Stroke
How can you recognize the symptoms of a hemorrhagic stroke?
A hemorrhagic stroke may present with one or more of the following symptoms:
- Headaches (experts commonly refer to these as “thunderclap” headaches due to their sudden and powerful nature, akin to an unannounced thunderclap)
- Light sensitivity, or photophobia, in which bright lights produce excruciating pain akin to a headache
- Wooziness or dizziness
- Vomiting as well as nausea
- Seizures
- Fainting or passing out
- Coma
- Speaking slurred or garbled (dysarthria) or having difficulties speaking (aphasia)
- Weakness on one side, paralysis, or loss of tactile perception
- Loss of all two-sided senses (hearing, touch, and vision) on one side
- Stiffness in the neck
What are the causes of Hemorrhagic Stroke?
The most frequent cause of a hemorrhagic stroke is hypertension or elevated blood pressure. This is particularly true if a person has extremely high blood pressure, high blood pressure that doesn’t go down, or both. Additional ailments or reasons behind hemorrhagic strokes consist of:
- Brain aneurysms are aberrant blood artery wall bulges in areas where the wall is weaker than usual
- Brain tumors encompass both primary brain tumors and malignancy with metastases
- Additional disorders such as cerebral amyloid angiopathy and moyamoya disease cause the blood arteries in your brain to deteriorate
- Blood-thinning drugs (which may exacerbate or cause brain hemorrhage)
- Head wounds
- Hemorrhagic stroke with subsequent bleeding
Associated conditions
Your overall risk of having a stroke or high blood pressure might also be influenced by the following circumstances and conditions:
- Alcohol use disorder
- High blood pressure (which increases the risk of an ischemic stroke by damaging blood vessels)
- Hyperlipidemia, or high cholesterol
- Headaches caused by migraines (which can resemble stroke symptoms, and migraineurs, particularly those with auras, are more likely to experience a hemorrhagic stroke)
- Substances used recreationally or prescribed medications misused
- Smoking as well as using alternative tobacco products (such as vaping and smokeless tobacco)
- Diabetes type 2
Diagnosis and Tests
How are strokes caused by hemorrhage diagnosed?
- A medical professional will perform diagnostic imaging, a neurological examination, and other procedures to identify a hemorrhagic stroke. During a neurological evaluation, a patient may not be able to respond to questions or follow instructions from a clinician because many patients who suffer from a hemorrhagic stroke are unconscious.
- Because of this, healthcare professionals frequently check for changes in processes that are beyond your conscious control, such as how your pupils react to light, and test-specific reflexes. Even when you’re unconscious, these can provide vital hints for medical professionals to diagnose a hemorrhagic stroke.
What examinations are planned to identify a hemorrhagic stroke?
The following are the most often performed tests when a medical professional detects a hemorrhagic stroke:
- CT scan (computerized tomography)
- Laboratory blood testing (to check liver and kidney function, blood sugar levels, clotting ability, and other signs of infection or heart damage)
- An electrocardiogram, often known as an ECG or EKG, to rule out a cardiac condition as the cause of the issue
- Scans using magnetic resonance imaging (MRI)
Adverse Effects and Complications
The reasons behind a stroke, where it occurs in the brain, the treatments administered, your medical history, and other factors can all affect the side effects of stroke treatments. More information about potential side effects and how to manage or even avoid them can be obtained from your healthcare professional.
Treatment of Hemorrhagic Stroke
Because hemorrhagic strokes are hard to treat immediately, they are frequently challenging to access. This implies that stopping bleeding directly is frequently not possible. Instead, by strengthening your body’s clotting mechanisms and lowering blood pressure, the main goal is usually to lessen the bleeding or stop it completely.
In certain instances, surgery might also be required. Medication may be required to lessen edema that occasionally occurs around bleeding or in other parts of the brain, which increases intracranial pressure. The location and severity of the stroke, among many other variables, determine the course of treatment.
With this condition, is there anything I shouldn’t eat or drink?
Your healthcare professional can advise modifying your diet to lower your blood pressure if you suffer a hemorrhagic stroke (or any kind of stroke, for that matter). As instances of this, consider:
- Caffeine-containing beverages: tea, coffee, soft drinks, etc
- Foods high in sodium or salt, which can raise blood pressure
- Foods heavy in saturated fats, like fried dishes, etc
- Recreational usage of alcohol or stimulants (cocaine, methamphetamine, amphetamines, etc.)
Which drugs or therapies are applied?
Hemorrhagic strokes can be treated with a variety of drugs and therapies. These medications and therapies frequently work in one of two ways: controlling your blood pressure or promoting better blood clotting. Sometimes, significant bleeding or specific side effects necessitate surgery for the patient.
Blood pressure management
Lowering and maintaining a safe blood pressure level is crucial for the treatment of hemorrhagic strokes, as elevated blood pressure is the primary cause of these strokes. You can lessen the amount of bleeding in your brain by doing this. Additionally, it facilitates the clotting of blood to seal the injured blood artery.
Clotting support
Normally, hemostasis—which is defined as “standing still” and “hemo” as “blood”—is triggered by any location of bleeding in the body. Your body uses this process to create a clot that seals wounds and fixes damage.
Sometimes, after a hemorrhagic stroke, the body’s natural ability to create a clot is compromised in many cases. In certain cases, bolstering and improving the body’s hemostasis mechanisms should come first. To do that, blood components or drugs that facilitate clotting are typically infused. Examples of treatments include vitamin K therapy, prothrombin or clotting factor infusions, and other therapies.
Surgery
When accumulated blood puts too much pressure on the brain tissue surrounding the leaking blood artery, it might result in a hemorrhagic stroke, which is one of the most deadly complications. In cases such as these, emergent surgery may be required to drain the collected blood and release pressure on the brain.
Physical Therapy Treatment for Post-Stroke Rehabilitation:
Early Mobilisation:
Many post-stroke problems, including deep vein thrombosis, are linked to immobility. Early mobilization attempts to increase the patient’s amount of physical activity outside of bed by shortening the time that passes after a stroke and the first time the patient exits the bed. The goal of early mobilization is to reduce the risk of problems from immobility and enhance functional recovery. Examples of these activities include sitting up in bed, transferring, standing, and walking.
Strategies to Improve Sensory Function:
Tactile, mechano, and muscular receptors are stimulated when repetitive sensory stimuli are presented. One may use techniques like stroking, stretching, applying both deep and superficial pressure, and approximation. Direct selection of the senses should be made.
Rubbing variously textured textiles against the hand, pressing coins, buttons, or keys into the hand, or creating designs, letters, or numbers on the skin. Approximation to extended UE during weight-bearing exercises (e.g., in sitting or standing/modified plantigrade position) might be given during functional training.
Stepping and standing are examples of LE tasks that can incorporate approximation. The right amount of stimulation is needed to activate the system, but not too much to cause negative side effects like withdrawal. The patient’s concentration must be fully on the task and stimulation during stimulation.
Initially, the eyes are closed (EC). The patient may be permitted to look with their eyes open if they are unable to identify the stimuli (EO).
Initially, the eyes are closed (EC). The patient may be permitted to look with their eyes open if they are unable to identify the stimuli (EO).
Techniques for Improving Motor Function
Exercises for range of motion and soft tissue/joint mobilization are started early to preserve joint integrity and mobility and avoid contractures. Every day, in all motions, AROM and passive ROM (PROM) with terminal stretch should be performed.
Stretching at a low load for an extended period of time and a more frequent range of motion (at least twice a day) is recommended if a contracture is forming.
Maintaining soft tissue length also requires careful consideration of positioning techniques.
Stroke Rehabilitation
- People frequently experience some residual effects in the days and months following a stroke. Many people experience a modest worsening of their stroke symptoms in the initial days following their stroke, followed by an improvement.
- Different forms of treatment and rehabilitation are especially beneficial for persons recovering from a stroke because it is normal for people to have persistent issues following a stroke. Sometimes, rehabilitation only consists of getting you back to your pre-stroke state. In other situations, this type of treatment can assist you in relearning specific skills.
- Pronounced “new-row-plass-tiss-it-ee,” neuroplasticity is a wonderful ability in your brain. This implies that when necessary, your brain can adjust and transform. Your brain may occasionally “re-map” a skill, giving control of that function to a healthy area of your brain. Numerous stroke rehabilitation techniques capitalize on this capacity to expedite the process.
There are various approaches to stroke rehabilitation, such as:
- Speech therapy: The areas of your brain that control your capacity to communicate and comprehend others when they speak are the main focus of this kind of therapy. Additionally, it can be beneficial if you experience any form of weakness or loss of control over the muscles in your neck and tongue. In addition to helping with speech, speech therapy can also aid with breathing, swallowing, eating, and drinking.
- Physical therapy: The goal of this therapy method is to increase muscle control and strength, particularly in the arms, hands, legs, and feet. With this kind of therapy, you can restore your ability to eat, dress, and walk. If you lose a skill permanently or over time, it can also help you adjust.
- Cognitive rehabilitation: This type of therapy supports the development of your mental skills. This type of therapy primarily focuses on enhancing your capacity for thought, focus, and memory.
- Various treatments might be appropriate for you, based on your situation. The ideal person to advise you on what kinds of therapies will be beneficial for you is your healthcare professional.
Prevention
How can I lower or perhaps completely avoid the chance of suffering a hemorrhagic stroke?
The most crucial thing you can do to stop a hemorrhagic stroke is to keep your blood pressure at a healthy range. It’s critical to control high blood pressure if you have it. Your medical professional can assist you with this by making suggestions about lifestyle modifications and available treatments.
Additional actions you can take to lower your chance of suffering a hemorrhagic stroke include:
- Take control of your medical circumstances. Hemorrhagic stroke is mostly caused by high blood pressure, while other factors such as Type 2 diabetes and high cholesterol may also play a role.
- Have an appropriate diet and stay within a healthy weight range. Stroke can result from several heart and circulation health issues. Managing your weight and food can help prevent or postpone a stroke because they have a significant impact on heart and vascular health.
- Every year, schedule a wellness appointment or check-up with your primary care physician. Many times, stroke-causing factors can be identified long before any physical symptoms appear. The first step in identifying those issues early on is a yearly examination with your healthcare physician.
- Make safer lifestyle decisions or alter your habits. Your chance of having a hemorrhagic stroke might be raised by a variety of lifestyle decisions or actions. Examples include abusing prescription medications or using drugs recreationally, smoking and using tobacco products (including vaping), misusing alcohol, and more. You can lessen the severity of a stroke you already have or prevent one entirely by stopping these.
Prognosis
In the event of a hemorrhagic stroke, what can I expect?
Hemorrhagic strokes typically occur quite quickly and present with severe symptoms. Since these symptoms typically worsen quickly, seeking medical attention right once is essential. A person’s chances of life and recovery might vary greatly depending on the site of the stroke, the amount of blood, and how quickly they receive care.
Although there are certain similarities among strokes, every individual will experience a stroke differently. As a result, you should discuss what to anticipate in your particular situation with your healthcare provider. Your provider can provide you with information and advice based on the particulars of your situation.
When can I go back to work, school, or my regular schedule after a hemorrhagic stroke?
The duration of hemorrhagic strokes is determined by the amount of blood or the pressure the hemorrhage puts on the brain. In other words, the stroke will persist until you get medical attention. Hemorrhagic strokes are almost invariably fatal if left untreated.
The consequences of a hemorrhagic stroke may not go away even after treatment. A few days or weeks may be all that certain effects last. Others might endure for several months or perhaps a lifetime. In your circumstance, the best person to advise you on what to expect is your healthcare professional.
What is the prognosis for this medical condition?
Compared to other types of stroke, the prognosis for hemorrhagic stroke is less good. This is because these strokes are hard to halt bleeding from. Additionally, only a small amount of blood is needed to produce severe effects. One important element that reduces the likelihood of a positive outcome is the accumulation of more blood than one fluid ounce (30 mL). In the worst circumstances, hemorrhagic stroke victims may experience significant brain damage that results in locked-in syndrome, a lifelong vegetative state, or even a coma.
Some people can recover from a hemorrhagic stroke and have a positive prognosis if they receive medical attention quickly. But each situation is different in this regard. The greatest person to advise you on what to anticipate and the most likely course of action in your instance (or the case of a loved one) is your healthcare professional.
Living With
How should I look after myself following a hemorrhagic stroke?
- Your healthcare professional will discuss treatment options, recovery timeframes, self-care, and other matters with you if you have a hemorrhagic stroke. Among the most crucial things you may do to aid in your recovery are:
- As directed by your doctor, take your prescriptions. It is imperative to manage long-term medical issues, particularly high blood pressure, following a hemorrhagic stroke.
Attend your appointments and see your provider. Therapy, rehabilitation, follow-up treatment, and other types of appointments can all aid in your fastest and fullest recovery. - Remember to take care of your mental wellness. Following a stroke, despair, and anxiety are frequent among stroke survivors, which can complicate their rehabilitation. One way you can support yourself as you heal is by talking to a mental health professional about these concerns.
- If you can, change your lifestyle in the suggested ways. Your doctor might advise you to make changes to your lifestyle, such as eating a different diet, exercising more, giving up smoking, etc. You can speed up your recovery and prevent further issues down the road according to their advice.
When should I visit my medical professional?
You must follow up with your healthcare professional as prescribed. Your healthcare practitioner will arrange for checkups, but you should also give them a call or make an appointment if you experience any new symptoms or problems that seem related to your stroke. Even if the problems and changes don’t seem to be related to your stroke, you should still speak with them if you observe any changes that impact your daily activities or way of living.
Additionally, if you encounter any of the risky post-stroke consequences that are common, you should visit the hospital. The following are the most typical complicating conditions:
- DVT, or Deep vein thrombosis
- Embolism in the lung
- Heart attack
Conclusion
A hemorrhagic stroke is a serious, perhaps fatal medical condition that frequently occurs suddenly and with little to no warning. Every minute matters if you are experiencing the signs of a hemorrhagic stroke, therefore you must seek medical attention right once.
Even though this kind of stroke frequently has more severe symptoms and is more challenging to cure, receiving medical attention quickly increases your chances of surviving and recovering.
FAQs
What differentiates a brain bleed from a hemorrhagic stroke?
One kind of brain hemorrhage that results from bleeding from a major brain blood artery is called a hemorrhagic stroke. Despite having many characteristics in common, these illnesses are not the same. An intraventricular bleed is an illustration of a different kind of brain bleed that isn’t a hemorrhagic stroke. These occur when bleeding occurs within the ventricles of your brain (intraventricular refers to “inside the ventricles,” which are tiny, naturally occurring openings between distinct brain regions).
What differentiates a hemorrhagic stroke from an aneurysm?
When a blood vessel in your brain bursts or breaks, it can cause serious bleeding, which is known as a hemorrhagic stroke. When a blood vessel in your brain expands or bulges abnormally, it is called an aneurysm. Although they are not the same, brain aneurysms that leak or burst can cause hemorrhagic strokes.
How long does someone usually live after a hemorrhagic stroke?
After a hemorrhagic stroke, a person’s life expectancy varies greatly depending on a multitude of conditions. The ideal person to advise you about the life expectancy for yourself or a loved one is your healthcare physician.
Is it possible to heal and live through a hemorrhagic stroke?
It is possible to survive and recover from a hemorrhagic stroke. Surviving and healing, however, are dependent on numerous things. The best course of action to improve your chances of survival and recovery is to seek medical attention as soon as you suspect a hemorrhagic stroke.
Who is impacted by Hemorrhagic Stroke?
People who suffer from illnesses that impact their circulatory system—which includes their heart and blood vessels—are more likely to get hemorrhagic strokes. various kinds of issues are more prevalent in older adults, which means that various stroke types are more common in later life.
Approximately two-thirds of stroke victims are older than 65. Those who have more serious health problems at a younger age may also experience them.
How often do hemorrhagic strokes occur?
Strokes occur frequently. Worldwide, strokes rank as the second most common cause of mortality. They are ranked fifth in the US. About 10% to 15% of all strokes are hemorrhagic strokes.
What effects does this illness have on my body?
There is significant bleeding in or around the brain during a hemorrhagic stroke. There is a limited amount of room for the bleeding to spread because this is occurring inside your skull. That damages the surrounding brain tissue by applying excessive pressure to it. The brain cells are permanently damaged if the pressure is too high or remains high for an extended period.
Additionally, hemorrhagic strokes impair blood flow to the brain. It has the same effect as piercing a hole midway through a plastic straw. Although liquid can still escape through the hole, the straw is still functional but more difficult to use. When that occurs in a blood vessel in your brain, the amount of blood that may reach neighboring brain locations is decreased because blood cannot pass through the injured vessel as quickly.
Do hemorrhagic strokes spread easily?
It is not possible to transmit hemorrhagic strokes from one person to another.
How can I treat the symptoms or look after myself?
Stroke is a medical emergency that requires immediate medical attention; do not attempt to self-diagnose. You should dial 911 or your local emergency services number as soon as possible if you or someone you know is experiencing stroke-like symptoms. The risk of dying or suffering irreversible brain damage rises when stroke diagnosis and treatment are postponed.
When will I feel better following treatment?
The amount of time it takes to recover from a stroke and start feeling better after treatment depends on several factors. The greatest person to advise you on what to anticipate and how to aid in your recuperation is your healthcare practitioner.



One Comment