Ankle Pain
What is an Ankle Pain?
Ankle pain is an incredibly common issue that affects people of all ages and activity levels. It can range from a mild, nagging discomfort to severe, debilitating pain that makes it difficult to walk or bear weight on the affected ankle. Ankle pain can stem from a variety of causes, including injuries, arthritis, and other underlying conditions.
The ankle joint is a complex structure that connects the foot to the leg and bears the full weight of the body during activities like walking, running, and jumping. It is made up of several bones, including the tibia, fibula, and talus, as well as a network of ligaments, tendons, and muscles that work together to facilitate movement and stability. Due to its intricate nature and the high demands placed on it during daily activities and sports, the ankle is prone to various types of injuries and disorders.
Sprains, which occur when the ligaments that support the ankle are stretched or torn, are among the most common causes of ankle pain. Lateral ankle sprains, also known as inversion sprains, are particularly prevalent, accounting for approximately 85% of all ankle sprains. These injuries often occur when the foot rolls inward, causing excessive stretching or tearing of the ligaments on the outside of the ankle.
Fractures, which involve breaks in one or more bones that make up the ankle joint, are another frequent source of ankle pain. These fractures can range from hairline cracks to complete breaks and can be caused by a variety of factors, including falls, twists, or direct impacts.
While ankle pain can be a debilitating and frustrating condition, understanding the underlying causes and seeking proper treatment is crucial for managing the pain and preventing further complications. By addressing ankle pain promptly and effectively, individuals can improve their quality of life and maintain their ability to participate in daily activities and physical pursuits.
Clinically Relevant Anatomy
The ankle joint, also known as the talocrural joint, is a hinged synovial joint that connects the foot to the leg. It is responsible for facilitating dorsiflexion (upward movement) and plantarflexion (downward movement) of the foot.
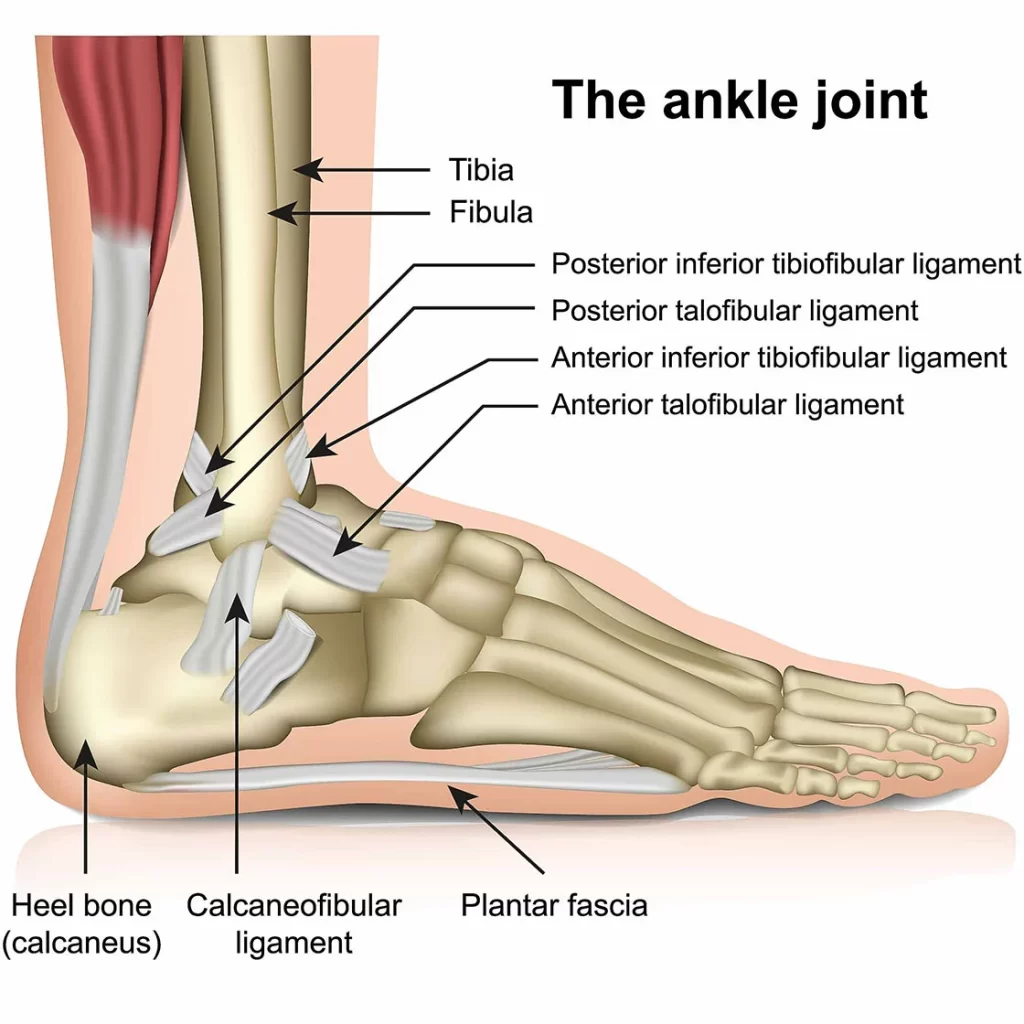
Bones:
- Tibia: The larger of the two leg bones, the tibia forms the medial (inside) portion of the ankle joint.
- Fibula: The smaller of the two leg bones, the fibula forms the lateral (outside) portion of the ankle joint.
- Talus: A small, irregularly shaped bone in the foot that articulates with the tibia and fibula to form the ankle joint.
The ankle joint is supported by a complex network of ligaments, tendons, and muscles, which are essential for maintaining stability and facilitating movement.
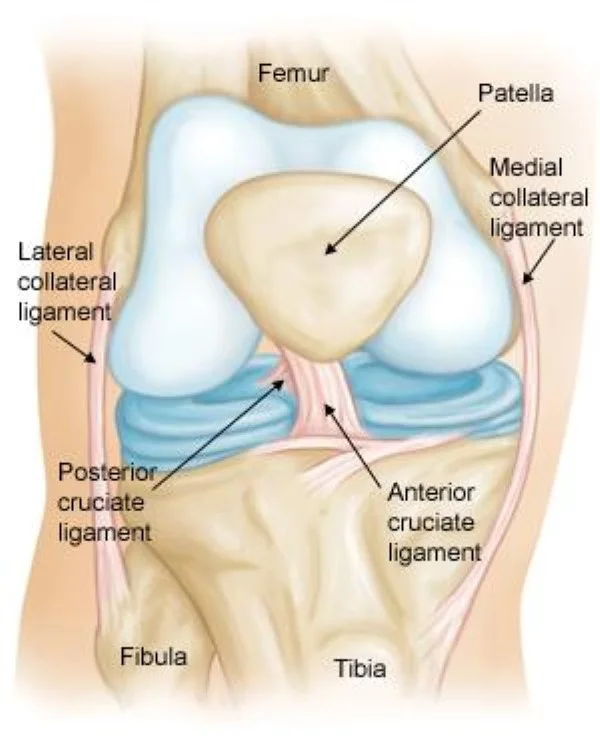
Ligaments:
- Lateral collateral ligaments: Consist of the anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), and calcaneofibular ligament (CFL). These ligaments provide lateral stability to the ankle joint and are often involved in lateral ankle sprains.
- Medial collateral ligaments: Consists of the deltoid ligament, which provides medial stability to the ankle joint.
- Syndesmotic ligaments: Include the anterior inferior tibiofibular ligament, posterior inferior tibiofibular ligament, and interosseous membrane. These ligaments connect the tibia and fibula, providing stability and preventing excessive movement between the two bones.
Tendons and Muscles:
- Achilles tendon: Connects the gastrocnemius and soleus muscles (calf muscles) to the calcaneus (heel bone). It is the strongest tendon in the body and is responsible for plantarflexion of the foot.
- Posterior tibialis tendon: Attaches the posterior tibialis muscle to the navicular bone in the foot. It plays a crucial role in supporting the medial longitudinal arch of the foot.
- Peroneal tendons: Include the peroneus longus and peroneus brevis tendons, which run behind the lateral malleolus (fibula) and are responsible for the eversion (outward rotation) of the foot.
- Extensor tendons: Include the anterior tibialis tendon, extensor hallucis longus tendon, and extensor digitorum longus tendon. These tendons run over the anterior aspect of the ankle and are responsible for dorsiflexion of the foot and extension of the toes.
Other Structures:
- Subtalar joint: Located below the ankle joint, the subtalar joint connects the talus to the calcaneus and allows for inversion and eversion movements of the foot.
- Tarsal tunnel: A fibro-osseous tunnel located behind the medial malleolus, through which the posterior tibial tendon, flexor digitorum longus tendon, posterior tibial artery, and posterior tibial nerve pass.
Understanding the intricate anatomy of the ankle joint is crucial for healthcare professionals, as it aids in the accurate diagnosis and management of various ankle conditions, such as sprains, fractures, tendinitis, and nerve entrapment syndromes.
Causes of Ankle Pain
Sprains and strains
Inversion sprains (lateral ankle sprains)
Inversion sprains, also known as lateral ankle sprains, are the most common type of ankle sprain. They occur when the ankle rolls inward, causing excessive stretching or tearing of the lateral ligaments on the outside of the ankle. Sports like basketball, soccer, and jogging that require quick direction changes are common causes of this kind of injury.
The severity of an inversion sprain can range from mild (Grade I) to moderate (Grade II) or severe (Grade III), depending on the extent of ligament damage. Symptoms may include pain, swelling, bruising, and instability in the ankle joint.
Eversion sprains (medial ankle sprains)
Eversion sprains, or medial ankle sprains, are less common than inversion sprains. They occur when the ankle rolls outward, causing stretching or tearing of the deltoid ligament on the inside of the ankle. These types of sprains can happen during activities that involve sudden outward twisting of the foot, such as skiing or stepping on an uneven surface.
Medial ankle sprains can also range in severity from mild to severe, with symptoms including pain, swelling, and potential instability on the medial side of the ankle.
High ankle sprains
High ankle sprains, also known as syndesmotic sprains or high syndesmotic sprains, involve injury to the syndesmotic ligaments that connect the tibia and fibula bones above the ankle joint. These sprains can occur when the ankle is forcefully twisted or externally rotated, causing excessive stretching or tearing of the syndesmotic ligaments.
High ankle sprains are less common than lateral or medial sprains but can be more severe and take longer to heal. Symptoms may include pain, swelling, instability, and difficulty bearing weight on the affected ankle.
Achilles tendon strain
The large tendon that joins the gastrocnemius and soleus muscles of the calf to the calcaneus, the heel bone, is called the Achilles tendon. A strain or tear in this tendon can cause significant pain and impairment in the ankle and calf region.
Achilles tendon strains can occur due to sudden, forceful movements, such as during activities that involve jumping or sprinting, or as a result of overuse or repetitive stress on the tendon. Symptoms may include pain, swelling, stiffness, and difficulty walking or pushing off with the affected leg.
Fractures
Ankle fractures
Ankle fractures involve a break in one or more of the bones that make up the ankle joint, such as the tibia, fibula, or talus. These fractures can occur due to high-impact injuries, such as falls from a height, motor vehicle accidents, or severe twisting or rotational forces on the ankle.
Ankle fractures can range from simple (involving a single bone) to complex (involving multiple bones or displacement). Symptoms may include severe pain, swelling, bruising, deformity, and an inability to bear weight on the affected ankle.
Foot fractures (e.g., metatarsal, calcaneus)
Fractures can also occur in the bones of the foot, such as the metatarsals (bones in the forefoot) or the calcaneus (heel bone). These fractures are often caused by direct trauma, such as dropping a heavy object on the foot or sustaining a high-impact injury during sports or accidents.
Metatarsal fractures can cause pain, swelling, and difficulty walking or bearing weight on the affected foot. Calcaneus fractures, which are relatively uncommon but can be severe, can result in significant pain, swelling, bruising, and potential deformity in the heel area.
Arthritis
Osteoarthritis
The smooth, protective layer called cartilage that coats the ends of bones in joints gets broken down over time, leading to the degenerative joint disease known as osteoarthritis. In the ankle joint, osteoarthritis can lead to pain, stiffness, swelling, and decreased range of motion.
Risk factors for developing osteoarthritis in the ankle include age, previous injury (such as a severe ankle sprain or fracture), obesity, and genetic predisposition. As the cartilage wears away, the bones may rub against each other, causing inflammation, bone spurs, and further joint damage.
Rheumatoid arthritis
Rheumatoid arthritis is an autoimmune disorder in which the body’s immune system mistakenly attacks the lining of the joints (synovial membranes), causing inflammation, pain, and eventual joint damage. The ankle joint can be affected by rheumatoid arthritis, leading to swelling, stiffness, and deformity over time.
Rheumatoid arthritis is a chronic, systemic condition that can affect multiple joints throughout the body, including the ankles, wrists, hands, and knees. It is more common in women and often presents with morning stiffness, fatigue, and other systemic symptoms.
Gout
A kind of arthritis called gout is brought on by the accumulation of uric acid crystals in the joints. While gout most commonly affects the big toe joint, it can also sometimes involve the ankle joint.
When uric acid crystals accumulate in the ankle joint, they can cause sudden, severe pain, swelling, redness, and warmth in the affected area. Gout attacks can be triggered by certain foods high in purines, alcohol consumption, or medications that increase uric acid levels.
Tendinitis
Achilles tendonitis
Achilles tendonitis is an inflammation of the Achilles tendon, the large tendon that connects the calf muscles to the heel bone. This condition can be caused by overuse or repetitive stress on the tendon, such as from running, jumping, or sudden increases in activity levels.
Symptoms of Achilles tendinitis may include pain, stiffness, and swelling in the back of the heel or along the Achilles tendon. In severe cases, the tendon can partially tear or rupture, causing significant pain and impaired function.
Posterior tibial tendonitis
The posterior tibial tendon runs along the inside of the ankle and helps support the arch of the foot. Posterior tibial tendonitis is an inflammation or degeneration of this tendon, often caused by overuse or excessive strain.
Symptoms of posterior tibial tendinitis may include pain along the inner ankle, swelling, and difficulty walking or bearing weight on the affected foot. In severe cases, the tendon can become dysfunctional, leading to a flatfoot deformity or adult-acquired flatfoot.
Nerve-related issues
The posterior tibial nerve is compressed or trapped as it travels through the tarsal tunnel, a small opening on the inside of the ankle, leading to tarsal tunnel syndrome. This nerve compression can result from injury, arthritis, cysts, or other factors that cause swelling or narrowing of the tarsal tunnel.
Symptoms of tarsal tunnel syndrome may include burning pain, numbness, tingling, or weakness in the foot or along the course of the posterior tibial nerve. These symptoms can radiate into the heel, arch, or toes.
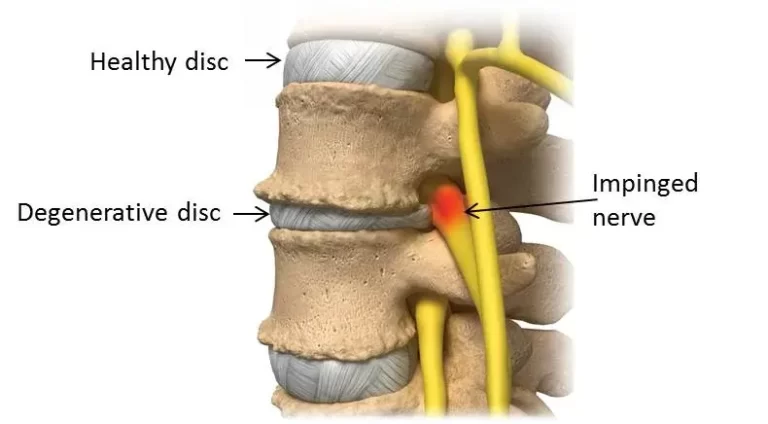
Peripheral neuropathy
Peripheral neuropathy is a condition that results from damage to the peripheral nerves, which carry information to and from the brain and spinal cord to the rest of the body. Diabetes is a common cause of peripheral neuropathy, but it can also be caused by other conditions, injuries, or exposure to certain toxins.
In the ankle and foot region, peripheral neuropathy can cause numbness, tingling, burning sensations, or loss of sensation. This can increase the risk of unnoticed injuries or ulcers, as well as balance and gait problems due to impaired sensation and muscle weakness.
Symptoms
Swelling
One of the most common symptoms of ankle pain is swelling or edema around the ankle joint. This can occur due to inflammation, fluid accumulation, or soft tissue damage. Swelling may be localized to a specific area or generalized around the entire ankle region. It can range from mild puffiness to significant swelling that distorts the normal contours of the ankle.
Bruising
Bruising or discoloration around the ankle is often a sign of an injury involving trauma or tearing of the blood vessels. Immediately after an injury, the area may appear reddened, but as time passes, the bruising may turn purple, blue, or even greenish-yellow as the blood breaks down and is reabsorbed by the body. The extent and pattern of bruising can sometimes indicate the type and severity of the injury.
Stiffness
Ankle stiffness or a limited range of motion is a common symptom associated with various ankle conditions. It can be caused by swelling, inflammation, or mechanical restrictions within the joint. Stiffness may be present during certain movements, such as dorsiflexion (pointing the toes upward) or plantarflexion (pointing the toes downward), or it may be a constant limitation in the joint’s mobility.
Tenderness
Tenderness or localized pain upon palpation (pressing) around the ankle joint is often indicative of an underlying injury or condition affecting that specific area. Tenderness may be felt over the bony prominences, such as the malleoli (ankle bones), or in the soft tissues surrounding the joint, such as the ligaments, tendons, or muscles.
Difficulty bearing weight
In cases of severe ankle pain or instability, individuals may experience difficulty bearing weight on the affected ankle or foot. This can significantly impact mobility and make it challenging to perform daily activities that involve standing, walking, or climbing stairs. Difficulty bearing weight may be accompanied by limping or the need for assistive devices, such as crutches or a cane.
Instability or giving way
Some ankle conditions, particularly those involving ligament injuries or nerve damage, can lead to a feeling of instability or a sensation that the ankle is “giving way” during weight-bearing or movement. This instability may be due to weakened or torn ligaments, muscle imbalances, or proprioceptive deficits (impaired awareness of joint position and movement).
Crepitus
Crepitus refers to the grinding, cracking, or popping sensations that may be felt or heard when moving the ankle joint. This symptom is often associated with arthritis or other degenerative conditions affecting the joint surfaces or the presence of loose bodies or bony fragments within the joint.
Muscle weakness or atrophy
In some cases, ankle pain may be accompanied by muscle weakness or atrophy (wasting) in the muscles surrounding the ankle joint. This can occur due to nerve damage, prolonged immobilization, or compensatory changes in muscle activation patterns resulting from the pain or instability.
Numbness or tingling
Numbness, tingling, or a “pins and needles” sensation in the foot or ankle area may indicate nerve compression or damage, such as in cases of tarsal tunnel syndrome, peripheral neuropathy, or nerve entrapment syndromes.
Diagnosis
Physical Examination
Visual Inspection:
- Observe the patient’s gait and weight-bearing pattern.
- Look for swelling, bruising, deformities, or muscle wasting around the ankle joint.
- Inspect for any external wounds or skin changes.
Palpation:
- Palpate (feel with the hands) the bony landmarks around the ankle, including the medial and lateral malleoli, the Achilles tendon, and the anterior joint line.
- Assess for tenderness, warmth, or crepitus (grating or crackling sensation) over specific areas.
- Palpate the posterior tibial and dorsalis pedis pulses to assess vascular supply.
Range of Motion (ROM) Assessment:
- Evaluate the active and passive range of motion in the ankle joint, including dorsiflexion (pulling the foot towards the shin), plantarflexion (pointing the toes down), inversion (turning the sole inward), and eversion (turning the sole outward).
- Compare the ROM to the unaffected side and note any limitations or pain during specific movements.
Special Tests
1. Thompson Test (Calf Squeeze Test):
This test assesses for an Achilles tendon rupture. It is performed by squeezing the calf muscle while observing the foot. In an intact Achilles tendon, squeezing the calf should cause plantarflexion (downward movement) of the foot. If there is no movement, it may indicate an Achilles tendon rupture.
2. Single-Leg Heel Raise Test:
This test evaluates the strength and function of the Achilles tendon and calf muscles. The patient is asked to raise the toes on one leg repeatedly. The inability to perform this test or significant weakness may indicate Achilles tendinopathy or a tear.
3. Too-Many-Toes Sign:
This test is used to assess for posterior tibial tendon dysfunction. The patient is asked to stand on their toes while the examiner observes the foot from behind. If the posterior tibial tendon is dysfunctional, the patient may not be able to maintain the arch, causing the forefoot to appear flat or abducted (turned outward), resembling the appearance of “too many toes.”
4. First Metatarsophalangeal (MTP) Squeeze Test:
Similar to the too-many-toes sign, this test involves squeezing the first MTP joint (base of the big toe) while observing the foot from behind. If the posterior tibial tendon is dysfunctional, the foot may collapse or appear flat, indicating an inability to support the arch.
5. Anterior Drawer Test:
This examination evaluates the anterior talofibular ligament’s (ATFL) integrity.The examiner stabilizes the leg and pulls the foot forward while holding the ankle in a slightly plantarflexed position. Excessive forward translation of the talus relative to the tibia may indicate an ATFL tear or laxity.
6. Talar Tilt Test:
This test evaluates the integrity of the calcaneofibular ligament (CFL). The examiner stabilizes the leg and attempts to invert (tilt inward) the calcaneus relative to the talus. Excessive tilt or opening of the lateral ankle joint may indicate a CFL injury.
Imaging Studies
1. X-rays:
X-rays are often the initial imaging study ordered for ankle pain. They can detect fractures, dislocations, and bony abnormalities. Weight-bearing and stress views may be obtained to assess for instability or subtle fractures.
2. Magnetic Resonance Imaging (MRI):
MRI is the preferred imaging modality for evaluating soft tissue structures, such as ligaments, tendons, and cartilage. Sprains, tendon rips, and other soft tissue injuries that might not show up on X-rays can be found using it.
3. Computed Tomography (CT) Scan:
CT scans provide detailed images of bony structures and can be useful in evaluating complex fractures or assessing for subtle bony abnormalities. They may also be used to guide injections or surgical procedures.
4. Ultrasound:
Ultrasound can be used to evaluate tendons, ligaments, and other soft tissues around the ankle. It can detect tendon tears, tendinitis, and fluid collections. Ultrasound is also useful for guiding injections or aspirations.
5. Bone Scan:
A bone scan is a nuclear medicine test that can detect areas of increased bone metabolism, which may indicate fractures, infections, or other bony abnormalities. It can be helpful in cases where the cause of ankle pain is unclear.
The choice of imaging study depends on the suspected underlying condition, the patient’s history, and the findings from the physical examination. In some cases, multiple imaging modalities may be required to arrive at an accurate diagnosis and guide appropriate treatment.
Differential Diagnosis
Ankle Sprains:
- Lateral ankle sprain (inversion injury)
- Medial ankle sprain (eversion injury)
- High ankle sprain (syndesmotic injury)
Fractures:
- Lateral malleolus fracture
- Medial malleolus fracture
- Posterior malleolus fracture
- Bimalleolar fracture (involving both malleoli)
- Trimalleolar fracture (involving all three malleoli)
- Calcaneus (heel bone) fracture
- Talus fracture
- Metatarsal fractures
- Lisfranc injury (midfoot fracture-dislocation)
Tendon Injuries:
- Achilles tendinitis or rupture
- Posterior tibialis tendinitis or rupture
- Peroneal tendinitis or tear
Arthritis:
- Osteoarthritis
- Rheumatoid arthritis
- Gout
- Post-traumatic arthritis
Nerve Entrapment Syndromes:
- Tarsal tunnel syndrome
- Anterior tarsal tunnel syndrome
- Superficial peroneal nerve entrapment
- Sural nerve entrapment
Vascular Conditions:
- Deep vein thrombosis (DVT)
- Peripheral artery disease
Bursitis:
- Retrocalcaneal bursitis
- Anterior ankle impingement syndrome
Osteochondral Lesions:
- Osteochondritis dissecans (OCD)
- Osteochondral fractures
Infections:
- Septic arthritis
- Osteomyelitis
Neoplastic Conditions:
- Bone tumors
- Soft tissue tumors
Referred Pain:
- Lumbar radiculopathy
- Calf muscle strains or tears
The differential diagnosis for ankle pain can be extensive, and a thorough history, physical examination, and appropriate imaging studies are essential to accurately identify the underlying cause. Age, mechanism of injury, associated symptoms, and risk factors can help guide the diagnostic process and narrow down the potential diagnoses.
Treatment for Ankle Pain
Rest, Ice, Compression, and Elevation (RICE)
RICE method is a widely recommended initial treatment approach for many acute ankle injuries, such as sprains or strains. It aims to reduce inflammation, manage pain, and promote healing.
Rest:
Resting the injured ankle is crucial in the early stages of recovery. This may involve using crutches or a walking boot to avoid putting weight on the affected ankle and allow the injured tissues to heal without further strain or stress.
Ice:
Applying ice or cold therapy to the injured area can help reduce swelling, inflammation, and pain. It is typically recommended to apply ice for 15-20 minutes several times a day, especially in the first 48-72 hours after the injury.
Compression:
Applying compression bandages or elastic ankle supports can help minimize swelling and gently support the injured area. It is important not to wrap too tightly, as this can impair circulation.
Elevation:
Keeping the injured ankle elevated above the level of the heart can help reduce swelling and inflammation by promoting the drainage of excess fluid from the injury site.
Medications
Non-steroidal Anti-inflammatory Drugs (NSAIDs):
NSAIDs, such as ibuprofen, naproxen, or aspirin, can be effective in reducing inflammation, pain, and swelling associated with ankle injuries or conditions like arthritis. They work by inhibiting the production of prostaglandins, which are involved in the inflammatory process.
Corticosteroid Injections:
In some cases, corticosteroid injections may be administered directly into the affected area to help reduce inflammation and pain. These injections are typically reserved for more severe or chronic conditions, such as persistent tendinitis or arthritis when other conservative treatments have been ineffective.
Corticosteroid injections can provide temporary relief from symptoms, but they do not address the underlying cause of the condition. They are often used in conjunction with other treatments, such as physical therapy or orthotics, to manage the condition more effectively.
It’s important to note that while corticosteroid injections can be beneficial, they should be used judiciously and under the guidance of a healthcare professional, as they can have potential side effects, including the risk of joint damage or infection if used excessively or improperly.
For both NSAIDs and corticosteroid injections, it is essential to follow the prescribed dosage and instructions carefully, as well as discuss potential risks and side effects with a healthcare provider, especially for individuals with certain medical conditions or getting other medications.
Braces and Supports
Braces and supports are commonly used to provide stabilization, protection, and support to the injured or weakened ankle joint. They can be beneficial in various stages of recovery or for long-term management of certain conditions.
Ankle Braces:
- Lace-up ankle braces: These braces provide compression and support to the ankle joint, helping to prevent excessive inversion (rolling inward) or eversion (rolling outward) movements.
- Semi-rigid ankle braces: Made of lightweight, semi-rigid materials, these braces offer more substantial support and protection for the ankle joint while still allowing some range of motion.
Ankle Supports:
- Elastic ankle supports: These supportive wraps or sleeves provide compression and mild support to the ankle joint, helping to reduce swelling and provide stability during activities.
- Ankle stirrups: These devices consist of a foot plate connected to a calf cuff by adjustable straps, providing support and limiting excessive plantar flexion or dorsiflexion movements.
Braces and supports are often used in the rehabilitation phase after an ankle injury to protect the joint and allow for a gradual return to activity. They can also be beneficial for individuals with chronic ankle instability or conditions like ankle arthritis, providing additional support and stability during daily activities or exercise.
Physical Therapy Management for Ankle Pain
Goals
Pain Relief:
Physical therapy aims to reduce pain and discomfort associated with ankle injuries or conditions. Through various techniques such as manual therapy, stretching, and modalities like ultrasound or electrical stimulation, physical therapists can help alleviate pain and promote healing.
Improved Range of Motion:
Ankle pain and stiffness can significantly limit the range of motion, affecting daily activities and mobility. Physical therapists utilize stretching exercises and joint mobilization techniques to improve flexibility and restore the full range of motion in the ankle joint, allowing for better movement and function.
Strengthening of Supporting Muscles:
The ankle is supported by various muscles in the leg, including the calf muscles, shin muscles, and intrinsic foot muscles. Physical therapy exercises focus on strengthening these supporting muscles, which can help stabilize the ankle joint, improve balance, and reduce the risk of future injuries.
Prevention of Further Injury:
By addressing the underlying causes of ankle pain and improving strength, flexibility, and proprioception (the ability to sense the position of your body in space), physical therapy can help prevent further injury or re-injury to the ankle. Therapists also provide education on proper body mechanics, footwear, and activity modifications to reduce strain on the ankle.
Improved Balance and Stability:
Ankle injuries can often lead to balance and stability issues, increasing the risk of falls or further injuries. Physical therapists incorporate balance and proprioceptive exercises into their treatment plans, such as standing on one leg, using balance boards, or performing agility drills. These exercises help improve overall stability, coordination, and confidence in weight-bearing activities.
Initial Assessment and Evaluation
Before beginning treatment, a physical therapist will conduct a comprehensive evaluation to assess the nature and severity of the ankle pain. This typically involves:
- Taking a detailed medical history
- Performing physical tests to assess range of motion, strength, and stability
- Observing gait and movement patterns
- Identifying any contributing factors or underlying conditions
Pain Management Strategies
Physical therapists employ various techniques to help manage and reduce ankle pain, including:
Ice/Heat Therapy:
- Ice therapy can help reduce inflammation, swelling, and pain in the acute stages of an injury.
- Heat therapy may be used in chronic conditions or before exercise to increase blood flow and promote muscle relaxation.
Electrical Stimulation:
- Transcutaneous electrical nerve stimulation (TENS) can help block pain signals by delivering low-voltage electrical currents through electrodes placed on the skin.
- Electrical muscle stimulation can also be used to facilitate muscle contraction and promote healing.
Ultrasound:
- Ultrasound therapy uses high-frequency sound waves to generate deep heat within the tissues, promoting increased blood flow and healing.
- It can be effective in reducing pain, muscle spasms, and joint stiffness.
Massage:
- Therapeutic massage can help relax tight muscles, improve circulation, and reduce muscle tension and spasms around the ankle joint.
- Techniques may include Swedish massage, deep tissue massage, or myofascial release.
Stretching Exercises for Ankle Pain
Achilles Tendon & Plantar Fascia Stretch:
This stretching exercise targets both the Achilles tendon and the plantar fascia, which are common areas of tightness and pain in the ankle and foot region.
Instructions:

- Sit on the floor with your legs extended in front of you.
- Loop a towel, resistance band, or stretching strap around the ball of your foot.
- Keeping your knee straight, gently pull the towel or band towards you, bringing your toes towards your shin.
- You should feel a stretch along the back of your calf and Achilles tendon.
- Hold the stretch for 30 seconds.
- To target the plantar fascia, flex your toes upwards, feeling the stretch along the bottom of your foot.
- For thirty seconds, hold the plantar fascia stretch.
- Stretch each foot two to three times.
Sitting Plantar Fascia Stretch:

- Sit upright on a chair or the edge of a bench, keeping your back straight.
- Extend one leg in front of you, with the knee straight and the heel resting on the floor.
- Lean forward from your hips, keeping your back straight, and grab the toes of your extended leg with both hands.
- Gently pull the toes towards your body, feeling a stretch along the bottom of your foot (the plantar fascia area).
- Hold the stretch for 30 seconds, breathing normally.
- To increase the intensity of the stretch, you can use a towel or resistance band looped around the ball of your foot and pull it towards you.
- After holding the stretch for 30 seconds, release and repeat on the other foot.
- Stretch each foot two to three times.
Plantar Fascia Stretch:
- Sit on the floor or a firm surface with your legs extended in front of you.
- Loop a towel, resistance band, or stretching strap around the ball of one foot.
- Keeping your knee straight, gently pull the towel or band towards you, bringing your toes towards your shin.
- Hold the stretch for 30 seconds.
- To target the plantar fascia, flex your toes upwards, feeling the stretch along the bottom of your foot.
- For thirty seconds, hold the plantar fascia stretch.
- Release and repeat on the other foot.
- Perform 2-3 repetitions on each foot.
Standing Calf Stretch:

- With your hands at shoulder height on the wall, face the wall.
- Step back with one leg, keeping the knee straight and the heel on the ground.
- Lean into the wall, feeling the stretch in your calf muscle of the back leg.
- Hold the stretch for 30 seconds.
- Bend the same knee slightly to stretch the soleus muscle (lower calf).
- Hold the soleus stretch for 30 seconds.
- Repeat the stretch on the other side after switching the legs.
- Perform 2-3 repetitions on each leg.
Deep Calf Stretch:

- Start in a half-kneeling position, with one knee on the ground and the other leg extended behind you.
- Place a folded towel or pad under your knee for comfort.
- Maintain a straight back while using your core muscles.
- Lean back slightly, transferring your weight onto your back leg.
- Your back leg’s calf muscles should be deeply stretched.
- To increase the intensity of the stretch, lean back further or slide your back foot away from your body.
- Hold the stretch for 30 seconds.
- Repeat the stretch on the other side after switching the legs.
- Perform 2-3 repetitions on each leg.
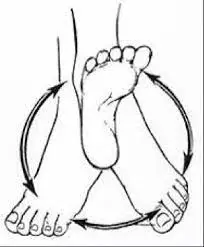
Range of motion exercises for the ankle:
Ankle Circles:
- Sit or stand with your legs extended in front of you.
- Slowly move your foot in a circular motion, rotating your ankle clockwise.
- Perform 10-15 repetitions in the clockwise direction.
- Reverse the direction and perform 10-15 repetitions counterclockwise.
- Repeat with the other ankle.
Alphabet Tracing:
- Sit or stand with your legs extended in front of you.
- Use your big toe to trace the letters of the alphabet in the air.
- Trace each letter as clearly as possible, moving your ankle through its full range of motion.
- Repeat with the other ankle.

Ankle Pumps:
- Lie on your back with your legs extended.
- Keeping your heels on the ground, point your toes away from you as far as possible.
- Then, flex your ankles by pulling your toes towards you.
- Perform 10-15 repetitions, moving through the full range of motion.
- Repeat with the other ankle.
Calf Raises:

- Stand with your feet shoulder-width apart, holding onto a wall or chair for balance if needed.
- Take off your heels and balance on your toes.
- Hold for a little moment at the top of the movement.
- Slowly lower back down with control.
- Perform 10-15 repetitions.
These range of motion exercises help improve flexibility, mobility, and overall function of the ankle joint. They can be incorporated into a physical therapy program to enhance recovery and prevent further injury.
Strengthening Exercises for Ankle Pain
Seated Foot & Heel Raise:
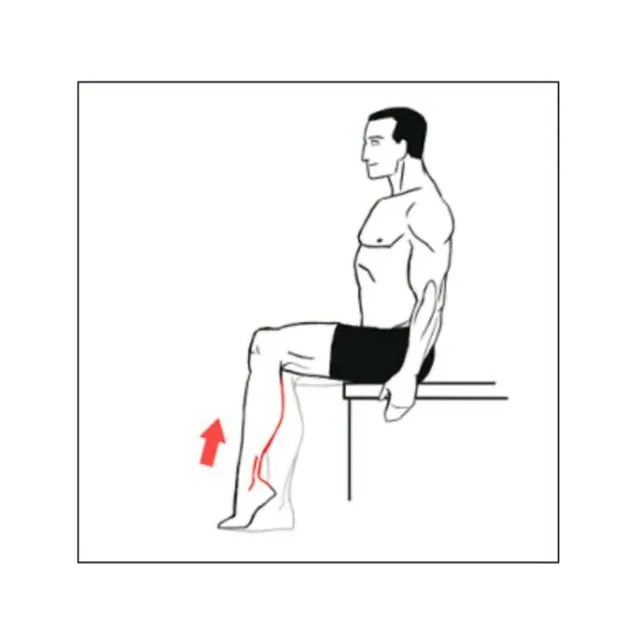
- With your feet flat on the ground, take an erect seat in a chair.
- Keeping your toes on the ground, raise your heels off the floor, lifting your feet and ankles upwards as high as possible.
- Hold the raised position for 2-3 seconds.
- Slowly bring your heels back to the beginning position.
- Repeat for 10-15 repetitions.
- Next, raise your toes off the floor, keeping your heels on the ground.
- Hold the raised toe position for 2-3 seconds.
- Slowly lower your toes back to the starting position.
- Repeat for 10-15 repetitions.
Toe Bend:
- With your feet flat on the ground, take an erect seat in a chair.
- Keep your heels on the ground and bend your toes downwards, pressing the balls of your feet into the floor.
- Hold the bent toe position for 2-3 seconds.
- Slowly release and straighten your toes.
- Repeat for 10-15 repetitions.
- Next, keep your toes on the floor and raise your heels, bending your ankles upwards.
- Hold the raised heel position for 2-3 seconds.
- Slowly bring your heels back to the beginning position.
- Repeat for 10-15 repetitions.
Big Toe Lift and Hold:

- Sit upright on a chair or the edge of a bench.
- Place a small weight or resistance band around the big toe of one foot.
- Keeping your heel on the floor, raise your big toe upwards, lifting the weight or resisting against the band.
- Hold the raised position for 5-10 seconds.
- Slowly lower your big toe back to the starting position.
- Repeat for 10-15 repetitions.
- Repeat the exercise with the other foot.
Towel Pickup:
- Sit upright on a chair or the edge of a bench.
- A tiny cloth or towel should be placed on the ground in front of you.
- Keeping your heel on the floor, use your toes to grab and crunch the towel towards you.
- Release the towel and straighten your toes.
- Repeat for 10-15 repetitions.
- For added resistance, you can place a small weight on the end of the towel.
Step-ups:

- Stand facing a step or raised platform (around 6-8 inches high).
- Step up with your right foot, pressing through your heel to bring your left foot up to meet the right.
- Step back down with your right foot, followed by your left foot, returning to the starting position.
- Repeat the step-up motion, leading with your left foot this time.
- Perform 10-15 repetitions, alternating the lead leg with each step.
- You can hold onto a wall or railing for balance if needed.
Heel Raises:
- Stand with your feet shoulder-width apart, holding onto a wall or chair for balance if needed.
- Raise your toes, lifting your heels off the ground as high as possible.
- Hold the raised position for 2-3 seconds, keeping your knees straight.
- Return to the starting position gradually and deliberately.
- Repeat for 10-15 repetitions.
- For added difficulty, you can perform the heel raises on one leg at a time.
Balance and Coordination Exercises for Ankle Rehabilitation
Single-Leg Stance

- Stand next to a wall, chair, or sturdy surface for support if needed.
- Shift your weight onto one leg, keeping that knee slightly bent and your core engaged.
- Lift your other foot off the ground, keeping the knee bent at 90 degrees.
- Focus on maintaining your balance by keeping your weight evenly distributed on the standing foot.
- For thirty seconds, maintain this posture while breathing normally.
- If you need to use the wall or chair for support, try to use it as little as possible.
- Repeat on the other side after switching your legs.
- As you improve, try closing your eyes or standing on a cushion or foam pad to increase the challenge.
Heel-to-Toe Walking

- Place your feet together and tense your core as you stand.
- Take a step forward, placing the heel of your front foot directly in front of the toes of your back foot.
- Maintain proper posture, keeping your head up and your eyes focused straight ahead.
- Take another step, placing the heel of your back foot directly in front of the toes of your front foot.
- Continue walking in this heel-to-toe pattern for 10-15 steps, focusing on your balance and stability.
- Turn around and walk back to your starting position, using the same heel-to-toe pattern.
- You can use a wall or sturdy surface for support if needed.
Tandem Stance
- Stand with your feet together, one foot directly in front of the other.
- Distribute your weight evenly between both feet.
- To keep your balance and posture in check, contract your core muscles.
- Hold this position for 30 seconds, focusing on your stability.
- If you need to use a wall or sturdy surface for support, try to minimize the amount of support you use.
- Switch the position of your feet, placing the other foot in front, and repeat the exercise.
Bosu Ball Squats

- Start by standing on a Bosu ball with the dome side facing down.
- Place your feet shoulder-width apart, with your weight distributed evenly on the ball.
- Maintain a straight back and contract your core muscles.
- Bend your knees and lower into a squat position, keeping your heels on the ball and your knees behind your toes.
- Go down as far as you comfortably can, while maintaining your balance.
- Put pressure on your heels to get back to the beginning position.
- Repeat for 10-15 repetitions, focusing on proper form and balance.
Surgery (for severe cases)
In some cases, surgical intervention may be necessary to address severe or persistent ankle conditions that do not respond to conservative treatments. Surgery is typically considered when non-operative treatments have failed to provide adequate relief or when the condition is severe enough to warrant immediate surgical intervention.
Ankle Fracture Repair:
- Open reduction and internal fixation (ORIF): This procedure involves realigning the fractured bones and stabilizing them with plates, screws, or other hardware to allow for proper healing.
Ligament or Tendon Repair/Reconstruction:
- Ankle ligament reconstruction: For severe ankle sprains or chronic ankle instability, ligament reconstruction may be performed to restore stability and prevent future sprains.
- Achilles tendon repair: Surgical repair or reconstruction may be necessary for complete or partial Achilles tendon ruptures or chronic tendinitis that does not improve with conservative treatment.
- Posterior tibialis tendon reconstruction: This surgery is performed to restore the function of the posterior tibialis tendon, which is essential for supporting the arch of the foot.
Arthroscopic Procedures:
- Ankle arthroscopy: This minimally invasive technique uses small incisions and a camera (arthroscope) to diagnose and treat various ankle conditions, such as removing loose bodies, repairing cartilage lesions, or addressing impingement syndromes.
Joint Fusion or Replacement:
- Ankle arthrodesis (fusion): In cases of severe ankle arthritis or deformity, fusion of the ankle joint may be performed to eliminate pain and restore stability by permanently joining the bones together.
- Ankle arthroplasty (replacement): For advanced ankle arthritis, total ankle replacement may be an option, where the damaged joint surfaces are replaced with artificial components.
The decision to pursue surgical treatment depends on various factors, including the severity of the condition, the patient’s age, activity level, and overall health. A thorough evaluation by an orthopedic surgeon is necessary to determine the most appropriate surgical approach and to weigh the potential risks and benefits.
Prevention Strategies for Ankle Pain
Proper Warm-up and Cool-down:
Before engaging in any physical activity or exercise, it’s crucial to warm up properly. This helps increase blood flow, loosen up the muscles and joints, and prepare the body for the upcoming physical demands. Dynamic stretches, light cardio, and sport-specific movements can be incorporated into a warm-up routine.
After exercise or physical activity, performing a cool-down routine is equally important. This involves gentle stretching and low-intensity exercises that gradually bring the body back to its resting state. Cooling down helps remove lactic acid buildup, reduces muscle soreness, and prevents injury.
Wearing Appropriate Footwear:
Choosing the right footwear for your specific activity can significantly reduce the risk of ankle injuries. Shoes with proper cushioning, arch support, and stability features can help protect the ankles from excessive stress and strain. Replace worn-out shoes regularly, as they can compromise support and increase the risk of injury.
Strengthening Exercises:
Incorporating exercises that target the muscles and tendons around the ankle joint can improve stability, balance, and overall joint health. Resistance exercises like calf raises, ankle circles, and resistance band exercises can strengthen the muscles that support the ankle.
Maintaining Flexibility:
Tight muscles and limited range of motion in the ankle joint can increase the risk of strains and sprains. Regular stretching exercises targeting the calves, Achilles tendon, and other muscles around the ankle can help maintain flexibility and prevent injuries.
Proprioception and Balance Training:
The body’s capacity to perceive its location and motion in space is known as proprioception. Exercises that improve proprioception and balance, such as standing on one leg, using balance boards, or performing agility drills, can help enhance ankle stability and reduce the risk of sprains and instability.
Gradual Progression:
When increasing the intensity or duration of physical activity, it’s important to do so gradually. Sudden increases in training load or rapid changes in exercise routines can overload the ankles and increase the risk of injuries. Allowing the body to adapt to new demands is crucial for injury prevention.
Proper Technique:
Practicing proper form and technique in sports and exercises is essential for preventing ankle injuries. Poor mechanics can place excessive stress on the ankle joint and surrounding structures, increasing the risk of sprains, strains, or other injuries.
Cross-Training:
Engaging in a variety of physical activities or cross-training can help reduce the repetitive stress on the ankle joint and allow for recovery and strengthening of different muscle groups. This can enhance general fitness and lessen the risk of overuse problems.
Adequate Rest and Recovery:
Allowing adequate rest and recovery time between intense physical activities is crucial for preventing overuse injuries and avoiding excessive strain on the ankle joint. Listen to your body and take breaks when necessary to allow for proper recovery.
Seeking Professional Guidance:
If you have a history of ankle injuries or are experiencing persistent ankle pain, it’s advisable to consult with a healthcare professional, such as a physical therapist or orthopedic specialist. They can assess your condition, provide personalized recommendations, and develop a tailored prevention and rehabilitation program.
When to Seek Medical Attention for Ankle Pain:
Severe Pain
If you experience severe, debilitating pain in your ankle that does not improve with rest, ice, compression, and elevation (RICE), it is crucial to seek medical attention. Severe pain can be a sign of a serious injury, such as a fracture, tendon rupture, or joint dislocation. Ignoring severe pain can lead to further damage and delayed healing.
Inability to Bear Weight
If you are unable to bear weight on the affected ankle or experience significant difficulty walking, it is important to seek medical evaluation. The inability to bear weight may indicate a fracture, severe sprain, or other serious injury that requires prompt treatment and immobilization.
Significant Swelling or Bruising
While some swelling and bruising are common after an ankle injury, significant or rapidly progressing swelling and bruising can be a sign of a more serious underlying condition. Severe swelling can indicate a fracture, tendon rupture, or bleeding within the joint or surrounding tissues. Seek medical attention if the swelling or bruising is severe, does not improve within a few days, or is accompanied by other concerning symptoms.
Additional symptoms and indicators that call for medical intervention include:
- Deformity or abnormal positioning of the ankle joint
- Numbness, tingling, or loss of sensation in the foot or ankle area
- Inability to move the ankle or foot
- Fever, chills, or signs of infection (redness, warmth, or pus)
- Persistent pain or swelling that does not improve after a few days of RICE treatment
- Recurrent ankle instability or frequent sprains
It is important to seek prompt medical attention if you experience any of these symptoms, as they may indicate a more serious condition that requires prompt diagnosis and treatment. Delaying medical attention can lead to further injury, chronic pain, or long-term complications.
When seeking medical attention, a healthcare professional, such as a primary care physician, orthopedist, or sports medicine specialist, can perform a thorough evaluation, order appropriate imaging tests (if necessary), and provide proper treatment, which may include immobilization, medications, physical therapy, or, in severe cases, surgical intervention.
Early and accurate diagnosis is crucial for proper management and optimal recovery from ankle injuries or conditions.
Home Remedies to Help You Provide Relief from Ankle Pain
Rest, Ice, Compression, and Elevation (RICE):
- Rest: Avoid activities that aggravate the pain and give your ankle time to heal.
- Ice: Apply an ice pack or a bag of frozen peas wrapped in a thin towel to the affected area for 15-20 minutes, several times a day. Ice helps reduce swelling and pain.
- Compression: Use an elastic bandage or ankle brace to compress the area and limit swelling.
- Elevation: Elevate your ankle above the level of your heart to help reduce swelling.
Over-the-counter Medications:
- Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help alleviate pain, swelling, and inflammation.
- Acetaminophen can also be used for pain relief if you cannot take NSAIDs.
Epsom Salt Soaks:
- Add 1-2 cups of Epsom salt to a warm water footbath.
- Soak your ankle for 15-20 minutes to help reduce inflammation and promote healing.
Essential Oil Massage:
- Massage the affected area with a few drops of essential oils like peppermint, eucalyptus, or lavender mixed with a carrier oil (e.g., coconut or olive oil).
- These oils have anti-inflammatory and analgesic properties that can help reduce pain and swelling.
Turmeric:
- Turmeric is a natural anti-inflammatory spice that can be consumed in your diet or taken as a supplement.
- You can also create a paste by mixing turmeric with warm water and applying it directly to the affected area.
Ginger:
- Ginger has anti-inflammatory properties and can be consumed as a tea or added to your meals.
- You can also make a ginger compress by soaking a towel in warm ginger tea and applying it to your ankle.
Contrast Baths:
- Fill two tubs or buckets with warm and cold water.
- Soak your ankle in the warm water for 3-4 minutes, then transfer to the cold water for 1 minute.
- Repeat this process 3-4 times, ending with the cold water.
- Contrast baths can help reduce inflammation and promote blood flow.
Stretching and Light Exercise:
- Gentle stretching and low-impact exercises, as recommended by your physical therapist or healthcare provider, can help improve your range of motion and promote healing.
Summary
Ankle pain is a widespread issue that can arise from various causes, ranging from acute injuries like sprains and fractures to chronic conditions such as arthritis and tendinitis.
Common causes include lateral ankle sprains, fractures of the ankle or foot bones, osteoarthritis, rheumatoid arthritis, gout, Achilles tendinitis, posterior tibial tendinitis, and nerve entrapment syndromes. Symptoms may involve swelling, bruising, stiffness, tenderness, difficulty bearing weight, instability, and numbness or tingling.
Diagnosis often involves a physical examination, imaging studies like X-rays or MRI, and special tests to assess ligament integrity, muscle strength, and nerve function. Treatment options include the RICE (Rest, Ice, Compression, Elevation) method, medications like NSAIDs or corticosteroid injections, braces or supports, physical therapy, and in severe cases, surgical interventions.
Preventive measures are essential to reduce the risk of ankle injuries and chronic pain. These include proper warm-up and cool-down routines, wearing appropriate footwear, strengthening exercises, maintaining flexibility, proprioception and balance training, gradual progression of activity, practicing proper technique, cross-training, allowing adequate rest, and seeking professional guidance when needed.
Seeking prompt medical attention is crucial when experiencing severe pain, inability to bear weight, significant swelling or bruising, or other concerning symptoms. Early diagnosis and treatment can prevent further complications and promote optimal recovery. By understanding ankle pain, its causes, and available treatment options, individuals can take proactive steps to manage their condition effectively and promote long-term joint health and mobility.
FAQs
What causes ankle pain the most often?
The most common cause of ankle pain is an ankle sprain, particularly a lateral ankle sprain (inversion injury) involving the lateral ligaments on the outside of the ankle joint.
How do I know if my ankle is sprained or broken?
While both sprains and fractures can cause swelling, pain, and difficulty bearing weight, a fracture typically results in more severe pain, deformity, and an inability to bear weight on the affected ankle. Imaging tests, such as X-rays, may be necessary to confirm a fracture.
Can ankle pain be a sign of arthritis?
Yes, ankle pain can be a symptom of various forms of arthritis, including osteoarthritis, rheumatoid arthritis, and gout. These conditions can cause inflammation, joint damage, and pain in the ankle joint.
What is the RICE method for treating ankle injuries?
RICE stands for Rest, Ice, Compression, and Elevation. It is a widely recommended initial treatment approach for acute ankle injuries, such as sprains or strains, to reduce inflammation, manage pain, and promote healing.
When should I seek medical attention for ankle pain?
Seek medical attention if you experience severe pain, an inability to bear weight, significant swelling or bruising, deformity, numbness, or tingling, or if the pain persists for more than a few days despite RICE treatment.
Can ankle braces or supports help with ankle pain?
Yes, ankle braces and supports can provide stabilization, compression, and support to the injured or weakened ankle joint. They can be beneficial during the recovery process or for long-term management of chronic conditions like ankle instability or arthritis.
What is the recovery time for a severe ankle sprain?
The recovery time for a severe ankle sprain (Grade 3) can range from several weeks to several months, depending on the extent of the injury and the individual’s healing process. Proper treatment, immobilization, and rehabilitation are crucial for a full recovery.
Can ankle pain be prevented?
Yes, several preventive measures can help reduce the risk of ankle injuries and chronic ankle pain, such as proper warm-up and cool-down routines, wearing appropriate footwear, strengthening exercises, maintaining flexibility, proprioception, and balance training, gradual progression of physical activity, practicing proper technique, cross-training, allowing adequate rest and recovery, and seeking professional guidance when needed.
References
- Ankle Sprain. (n.d.). Physiopedia. https://www.physio-pedia.com/Ankle_Sprain
- Cluett, J. (2023, December 29). Causes and Treatment of Ankle Pain. Verywell Health. https://www.verywellhealth.com/ankle-pain-causes-2549409#toc-when-to-see-a-healthcare-provider
- Professional, C. C. M. (n.d.). Ankle Pain. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/15295-ankle-pain
- Preventing Ankle Sprains. (n.d.). Student Health and Wellness Services. https://health.williams.edu/medical-diagnoses/general-health-concerns/preventing-ankle-sprains/
- Guide | Physical Therapy Guide to Ankle Sprain. (2023, February 14). Choose PT. https://www.choosept.com/guide/physical-therapy-guide-ankle-sprain
- Prajapati, N. (2022, March 18). Ankle Pain: Cause, Symptoms, Physiotherapy Treatment, Exercise | Mobile. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/ankle-pain-physiotherapy-treatment/#Electrotherapy_treatment
- Iavarone, K. (2023, January 18). What to know about ankle pain treatments. https://www.medicalnewstoday.com/articles/ankle-pain-treatments#home-treatment-and-self-care\
- Common Ankle Tests in Orthopedic Examination – Physical Therapy Web. (2023, November 11). Physical Therapy Web. https://physicaltherapyweb.com/common-ankle-tests-orthopedic-examination/






6 Comments