Osteoarthritis
What is Osteoarthritis?
Osteoarthritis is the most common form of arthritis. Healthcare providers may refer to it as degenerative joint disease or OA. It occurs when the cartilage that lines your joints wears down over time, causing your bones to rub against each other as you use the affected joints.
Osteoarthritis is a relatively common condition that can affect any joint in the body. It is most likely to affect the joints that support the majority of our weight, such as the knees and feet. Commonly affected joints include the joints of the hand.
Typically, the ends of bones in your joints are covered in a layer of solid, smooth cartilage. Cartilage acts as both a shock absorber and a lubricant, allowing the bones in your joints to glide easily and safely past each other. If you have osteoarthritis, the cartilage in your affected joints decreases over time. Your bones will eventually scrub against one other as you move your joints.
Osteoarthritis can damage any of your joints, however, it typically develops in your:
- Hands.
- Knees.
- Hips.
- Neck (the cervical spine).
- Lumbar spine (lower back).
A healthy joint
In a healthy joint, a layer of tough yet smooth and slippery tissue known as cartilage covers the surface of the bones and allows them to move freely against one another. When a joint develops osteoarthritis, some of the cartilage thins, and the surface is affected. This indicates that the joint does not move as smoothly as it should.
When cartilage is worn or damaged, the tissues within the joint become more active than usual as the body tries to fix the damage. The repair processes may alter the structure of the joint, but they frequently allow it to function correctly and without pain or stiffness. Almost all of us will develop osteoarthritis in one or more of our joints as we age, even if we are unaware of it.
A joint affected by osteoarthritis
However, the repair processes do not always work well, and changes to the joint structure may result in or contribute to symptoms such as pain, swelling, or trouble moving the joint properly.
For example:
- The extra bone may build around the joint. These bone growths are known as osteophytes, and they can occasionally interfere with movement or rub against surrounding tissues. Some joints, particularly the finger joints, may show stiff, knobbly swellings.
- The lining of the joint capsule (known as the synovium) may thicken and create more fluid than usual, causing the joint to expand.
- Tissues that surround and support the joint may extend with time, making the joint less stable.
Types of Osteoarthritis
A healthcare physician may classify osteoarthritis into one of two types:
- Primary osteoarthritis: Primary osteoarthritis is the most prevalent form of osteoarthritis that develops in your joints over time. Experts believe it is mainly caused by the normal wear and tear of using your joints during your lifetime.
- Secondary osteoarthritis: Secondary osteoarthritis arises when something directly destroys one of your joints enough to produce osteoarthritis. Secondary osteoarthritis is most commonly caused by injuries and traumas. Other types of arthritis can also damage the cartilage in your joints, resulting in osteoarthritis.
Epidemiology
Osteoarthritis is common, affecting approximately 25% of individuals. The prevalence rises with age. Men are more likely to be afflicted under the age of 50, while women are more likely to be impacted by the elderly.
Radiographic evidence of OA is present in 80% of the population over the age of 65, with symptoms in 60% of this group.
People above the age of 45 suffer from osteoarthritis. It is most common in those aged 80 and up, with little over one-third (35%) reporting the condition.
Osteoarthritis has become very common. Experts estimate that osteoarthritis affects more than 80% of persons over the age of 55, even if some never feel symptoms. Around 60% of patients with osteoarthritis have symptoms that they can see or feel.
What causes Osteoarthritis?
Experts are unsure what causes osteoarthritis. Primary osteoarthritis normally develops gradually as people age. As you become older, the usual wear and tear on your joints may contribute to cartilage breakdown.
Anything that directly destroys your joints can induce osteoarthritis, such as:
- Sports injuries.
- Falls.
- Automobile accidents.
- Ehlers-Danlos syndrome and joint hypermobility syndrome are two examples of joint-related health problems.
Other types of arthritis, particularly inflammatory arthritis, can cause osteoarthritis, including:
- Rheumatoid arthritis.
- Gout.
- Ankylosing Spondylitis
It’s still unknown what causes osteoarthritis. We know it isn’t just ‘wear and tear’ and that your chance of developing osteoarthritis relies on some factors. some other cause:
- Age
This could be related to physiological changes associated with aging, such as weakened muscles, weight increase, and the body’s decreased ability to recover properly. - Gender
Women are more likely to develop and suffer from osteoarthritis in most joints. - Obesity
Being overweight is a risk factor for osteoarthritis, particularly in weight-bearing joints like the knee and hip. - Joint injury.
A serious injury or operation on a joint may result in osteoarthritis later in life. Normal activity and exercise do not cause osteoarthritis, however, extremely difficult, repeated activities or physically demanding work can raise your risk. - Joint abnormalities
If you were born with abnormalities or developed them as a kid, you may develop osteoarthritis earlier and more severely than others. - Genetic factors
The genes we inherit may affect our risk of developing osteoarthritis in the hand, knee, or hip. Some very uncommon forms of osteoarthritis have been linked to abnormalities in single genes that affect a protein known as collagen. This can cause osteoarthritis to develop in multiple joints at a younger age than usual.
What are osteoarthritis symptoms?
The primary symptoms of osteoarthritis are pain and stiffness in the affected joints. The discomfort gets worse when you move the joint or at the end of the day. Your joints may feel tight after rest, but this normally passes as soon as you resume moving. Symptoms may change for no obvious cause. Or you may notice that your symptoms change depending on what you’re doing.
The damaged joint may occasionally be enlarged. The swelling can be:
Joints can be stiff and knobbly, particularly in the fingers, due to bone growth, or soft, due to joint lining thickening and fluid accumulation.
The most common symptoms of osteoarthritis are:
- Joint pain (particularly while moving it).
- Stiffness.
- Swelling near the joint.
- A decreased range of motion (the distance a joint can be moved).
- Feeling like a joint isn’t as strong or stable as it should be.
- A joint that looks noticeably different than it used to (joint deformity).
Clinical signs vary according to the affected joint, however, they typically share several characteristics. They’re mostly local. The symptoms are:
- Pain: This is a mechanical type of pain that occurs during mobilization, increases with fatigue, and reduces with rest. Pain develops in the morning or after a period of inactivity. Usually, there is no nighttime soreness. The intensity of discomfort varies. It can be bland and bearable at times, but it can also be extremely heavy with short peaks. It can be triggered by cold, trauma, or fatigue. This discomfort affects the subchondral bone as well as the capsuloligamentar and muscle systems.
- Movement limitation (loss of range of motion): Movement limitation is gradual and will become apparent after several years. This limitation is mostly due to the blockage of voluntary muscular function and reflex contracture. It is also the result of alterations in the articular spaces, resulting in incongruent joint surfaces. Some patients report morning stiffness that lasts longer but is less severe than that caused by rheumatoid arthritis or ankylosing spondylitis. The severity rises with time, as do joint abnormalities and cartilage wear.
- Sounds: You can hear cracking, scraping, and crepitation sounds. They are the result of joint mobilization. Irregularities in the articulating joint surfaces, as well as low-quality residual cartilage, are most likely to be the reason.
- Difficult and painful mobilization: It is important to know the difference between complete blockage and limited mobility. Total obstruction is caused by the existence of a meniscus, and uncommon structures, and will require additional examination.
Mild edema around the joint
How does osteoarthritis affect me?
Osteoarthritis affects individuals and joints differently. However, most people’s osteoarthritis does not become more severe over time.
For some people, the illness occurs a few years after symptoms appear and then remains stable or improves. Others may experience multiple stages of moderate joint discomfort, with improvements in between.
The degree of joint injury isn’t particularly useful in predicting how much pain you’ll have. Some persons experience severe pain and mobility issues as a result of minor joint damage, whilst others experience severe joint damage but few or no symptoms.
If you have severe osteoarthritis, being aware of your daily tasks may become more difficult depending on which joints are involved. Sleeping can be difficult for people with more severe osteoarthritis.
What joints are affected?
Osteoarthritis can affect every joint, however, the symptoms are most commonly associated with the knees, hips, wrists, spine, and big toes.
- The knee
Knee osteoarthritis is a common condition. This is most likely due to the enormous strains, twists, and bends that your knee must withstand while also holding your body weight. Osteoarthritis usually affects both knees. - The hip
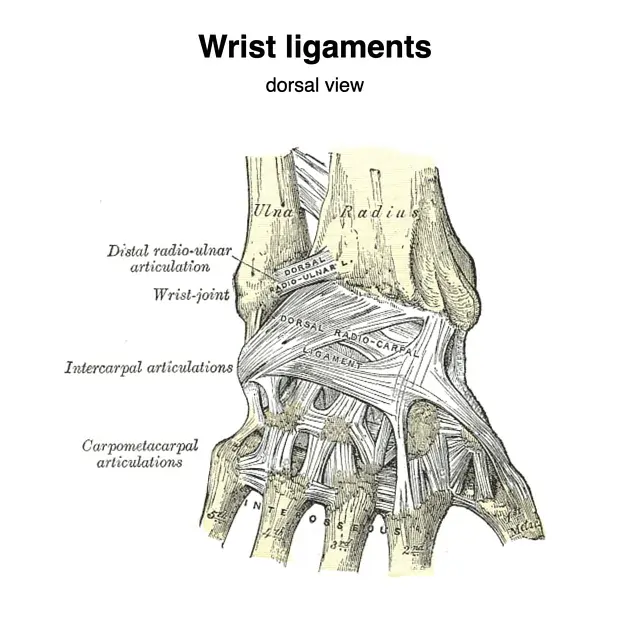
Hip osteoarthritis is also common, and it can affect one or both hips. The hip joint is a ball-and-socket joint that typically has a considerable range of motion. It also supports a lot of your weight. Hip osteoarthritis occurs equally in men and women. - The hands and wrists
Hand osteoarthritis is commonly associated with nodal osteoarthritis. This primarily affects women and typically begins around the time of menopause. It typically affects the base of your thumb and the joints at the ends of your fingers, although other finger joints may also be affected. - The back and neck
Changes in the bones of your spine and the discs in between can be followed by symptoms comparable to osteoarthritis. These abnormalities in the spine are commonly referred to as spondylosis. Although they are extremely frequent, they are not the leading cause of back or neck pain. - The feet and ankles
Osteoarthritis of the foot typically affects the joint near the base of the big toe. However, osteoarthritis in the midfoot is not common. The ankle is the least commonly affected area of the foot. - The shoulder
The shoulder is made up of two joints, both of which can be affected by osteoarthritis. - The glenohumeral joint is a ball-and-socket joint that connects the upper arm and shoulder blade.
The acromioclavicular joint is a minor joint located between the collarbone and the top of the shoulder blade. - The elbow
Osteoarthritis rarely affects the elbow joint. When it is affected, it usually follows a single serious accident or a series of lesser ones. - The jaw
The jaw, or temporomandibular joint, is one of the most frequently used joints in the body, and its cartilage is especially prone to deterioration. Osteoarthritis in the jaw frequently develops at a younger age than in other joints.
Diagnoses
A physical exam and imaging tests are used by a healthcare provider to diagnose osteoarthritis. They will examine your joints and inquire when you first experienced any problems. Tell them if certain activities aggravate your symptoms, or if they come and go.
If you suspect you have arthritis, you ought to get a correct diagnosis because different types of arthritis typically require quite different therapies. Osteoarthritis is often diagnosed using:
your symptoms – how and when they started, how they’ve evolved, how they affect your life, and any situations that make them better or worse
During a physical examination, your doctor will check for Symptoms that may include joint discomfort,
- Crepitus,
- Edema,
- Fluid buildup,
- Restricted movement.
- Joint instability
- Weakness or weakening of the muscles supporting the joint
Tests For used to diagnose osteoarthritis:
Your healthcare professional may utilize X-rays to photograph your joints. They may also employ an MRI (magnetic resonance imaging) or CT scan.
You may require blood testing to rule out other illnesses or problems that cause similar symptoms.
Differential Diagnosis
Diagnosing OA is usually straightforward.
Periarticular structure derangement: Periarticular discomfort that does not respond to passive motion or joint probing should be referred to another cause, such as bursitis, tendinitis, or periostitis.
Inflammatory arthritis: If the painful joints include the MCP, wrist, elbow, ankle, or shoulder, OA is unlikely unless there are particular risk factors (occupational, sports-related, injury history). Prolonged stiffness (more than one hour) indicates inflammatory arthritis, such as rheumatoid arthritis. Warmth and erythema in the joint indicate a crystalline cause. If the diagnosis is not visible in history, physical exam, and radiographs, arthroscopy (joint aspiration) can assist in distinguishing between several kinds of arthritis. If an infected joint is detected, aspirate it and send the fluid for culture.
Other inflammatory/systemic conditions include weight loss, fatigue, fever, and loss of appetite, which may indicate a systemic illness such as polymyalgia rheumatic, rheumatoid arthritis, lupus, sepsis, or cancer.
Osteoarthritis can also be caused by damage from another type of joint disease, such as rheumatoid arthritis or gout.
The weather and food are two factors that can affect the symptoms of osteoarthritis but are not a direct cause of it.
- Weather
Many patients with osteoarthritis report that variations in the weather aggravate their pain, particularly when air pressure falls, such as shortly before it rains. The weather may affect your arthritis symptoms, but it does not cause them. - Diet
Some people discover that specific meals either exacerbate or relieve their pain and other symptoms. However, weight is more likely than any other dietary element to affect your chance of developing osteoarthritis.
Diagnostic Procedures
Osteoarthritis of the knee: Radiography can help determine the severity of osteoarthritis. In the following way, we can differentiate four levels of severity in osteoarthritis:
- Degree I: normal joint with minor osteophyte.
- Degree II: Osteophytosis on two points with minimal subchondral sclerosis, enough joint space, and no deformities.
- Degree III: Moderate osteophytosis, early distortion of the bone ends, and a narrowing joint space.
- Degree IV: Large osteophytes, bone-ending deformities, joint space constriction, sclerosis, and cysts.
Treatment of Osteoarthritis
The treatment aims for OA are to reduce pain and functional loss. The condition is managed using both non-pharmacological and pharmacologic therapy. Non-pharmacological treatment is tried first.
Non-pharmacologic therapy consists of avoiding activities that aggravate pain or overload the joint, exercising to build strength, losing weight as needed, and unloading joints with a brace, splint, cane, or crutch.
Formal physical therapy can greatly aid patients in using equipment (e.g., proper cane use) and training them on exercises. Exercise programs that include aerobic and resistance training have been shown in multiple investigations to reduce pain while improving physical function and should be promoted.
Malaligned joints can be repaired mechanically with realignment knee braces or orthotics.
Your doctor will assist you in finding treatments that reduce the symptoms of osteoarthritis. There is no cure for arthritis, and you can’t regenerate cartilage in affected joints. When you have symptoms, your physician will help you identify strategies to manage them.
Conservative Treatment
Managing symptoms.
Although there is no cure for osteoarthritis, there are therapies that help relieve symptoms and allow you to go about your daily life. This includes:
- Lifestyle changes
- Pain relief drugs
- Physical therapy
- Supplements and complementary treatments.
Warmth and Cold
Applying a hot water bottle covered in a towel to protect your skin, or a wheat bag heated in the microwave, can help relieve pain. An ice pack, wrapped in a towel to protect your skin, can help to minimize swelling and discomfort. Ice can be used for up to 20 minutes every couple of hours.
Pharmacological management
The most prevalent therapies for osteoarthritis are:
- Medication: OTC pain medications can help reduce discomfort and inflammation. You may require orally administered medication or topical pain medications (creams, ointments, or patches applied to your skin around the damaged joints). The medications commonly used to treat osteoarthritis have little effect on the condition itself, although they can assist in alleviating symptoms such as pain and stiffness.
- NSAID creams and gels.
Nonsteroidal anti-inflammatory medicines (NSAIDs) are lotions, gels, or patches that can be applied directly to the skin. Ibuprofen and diclofenac gels are sold over the counter in pharmacies and supermarkets. Others, such as ketoprofen, are only available by prescription. Creams, gels, or patches function well for some joints, like the knees and hands, but may not work as well for joints like the hips that are deeper under the skin. - Paracetamol
Paracetamol is normally advised as the safest sort of pain reliever to start with. It’s preferable to take them before the pain gets too acute. Paracetamol is readily accessible over the counter at pharmacies and supermarkets, and there is no benefit to purchasing from more expensive brands. - Nonsteroidal anti-inflammatory medications (NSAIDs)
NSAID medications are often more potent painkillers than paracetamol. The most popular is ibuprofen, which is easily accessible over the counter at grocery and pharmacy shops. You can try these for 5-10 days; if they don’t work after that, they’re unlikely to. - If you require them, your doctor might prescribe: To lessen the risk of ulcers and bleeding in the gut, consider using higher dosages of ibuprofen, stronger NSAIDs like naproxen or diclofenac, or newer NSAIDs like celecoxib or etoricoxib.
If your doctor recommends an NSAID, he or she will most likely also prescribe a proton pump inhibitor (PPI) to protect the gut. PPIs include omeprazole and lansoprazole. - Hyaluronic acid injections
Hyaluronic acid, also known as hyaluronan, is a naturally occurring lubricant and shock absorber in joint fluid. Hyaluronic acid injections have been used to treat osteoarthritis of the knee. The treatment is now unavailable on the NHS due to contradicting research results on its long-term effectiveness. However, the treatment is only provided privately.
Assistive devices can improve function and mobility.
Physiotherapists are in a perfect position to recommend, fit, and teach the usage of these devices. These include devices like scooters, canes, walkers, splints, shoe orthotics, and useful devices like jar openers, long-handled shoe horns, and steering wheel grips. Some braces and foot orthotics must be fitted by a therapist.
- Supportive devices Supportive devices: Wearing shoe inserts or a brace might help support and stabilize your joints. Using a cane or walker can relieve strain on your damaged joints and allow you to move comfortably.
- Heat and Cold Therapies: Applying heat or ice to the afflicted joints may alleviate pain and stiffness. Your physician will advise you on how frequently (and for how long) you should use a heating pad, ice packs, or cool compress.
- Complementary therapies: Complementary therapies may be used with other treatment approaches. Acupuncture, massage, meditation, Tai Chi, and dietary supplements are all forms of supplementary medicine. Consult your doctor before beginning to take any herbal or dietary supplements.
Physiotherapy Treatment of Osteoarthritis
Exercise: Moving your joints helps reduce stiffness and strengthen the muscles that surround them. Low-impact activities such as swimming, water aerobics, and weight training can all be effective. Your clinician may recommend that you consult with a physical therapist.
OA involves decreased muscular strength (especially in the muscles surrounding the affected joint), decreased flexibility, weight gain, limitations in the ability to perform ADL activities, and frequently restricted mobility. An integrated exercise program’s major goals are to improve physical and psychological function, as well as to boost feelings of well-being. Immediate goals include increasing joint motion, improving muscle strength, increasing aerobic capacity, and maintaining an ideal body weight.
OA patients are more likely to fall because of decreased function, muscle weakness, and impaired balance. Side effects from pain relievers can also contribute to falls. Narcotic pain medicines can make you feel dizzy and unstable.
Physiotherapy is an important part of OA management because it teaches people how to use their joints properly, exercise correctly in both motion and flexibility exercises, as well as cardiovascular exercises (e.g., hydrotherapy, swimming), recommend assistive devices, and use modalities.
Physical activity: Many patients have issues that would exacerbate their discomfort and create additional joint injury. While resting injured joints may make them feel more comfortable first, excessive rest might cause stiffness.
Do not be frightened to use your joints. If pain makes it difficult to begin exercising, consider taking a pain reliever such as paracetamol beforehand. And if you think you’ve overdone it, try applying warmth to the hurting joint; if it’s swollen, an ice pack may assist.
If you haven’t exercised much in a while, consult a physiotherapist. They will be able to assist you in developing a program that is appropriate for you. The most important thing is to begin slowly and progress steadily.
You might wish to try our workouts for healthy joints.
The goal of Physical Therapy:
- Reduce pain and inflammation: Pain and inflammation can be reduced using a range of procedures used by physiotherapists, including manual therapy, exercise, and modalities such as heat, cold, and electrical stimulation.
- Improve joint mobility and function: Osteoarthritis can induce stiffness and loss of motion in joints. Physiotherapy can enhance joint range of motion and flexibility, making moving around and doing daily tasks simpler.
- Strengthen your muscles: Weak muscles can cause joint pain and instability. Physiotherapy can assist in strengthening the muscles around the joints, reducing pain, and improving function and balance.
- Maintain or improve physical fitness: Regular exercise is useful for overall health and well-being, as well as managing OA. Physiotherapists can assist you in developing a safe and effective fitness plan that is suited to your specific requirements.
- Physiotherapists may teach patients about osteoarthritis, how to manage their symptoms, and how to avoid future difficulties. This education may enable patients to take an active role in their own care, thereby improving their quality of life.
- Balance issues: Osteoarthritis might increase the chance of falling. Physiotherapy can improve your balance and lower your chance of falling.
- Gait abnormalities: OA may affect the way you walk. Physiotherapy can help you improve and make your gait more efficient.
- Painful activities: OA might make it difficult to perform some tasks. Physiotherapy can help you alter your activities so that you can keep doing what you enjoy.
Basic physiotherapy
Not recommended for those with acute severe joint swelling or cardiovascular problems.
- Warm-up and Range of Motion
- Strengthening exercises: quad sets, supine straight leg raises, prone hip extensions, seated isometric knee extensions, single-leg leg presses, standing hamstring curls, and standing heel raises.
- Aerobic program.
- Cool down with muscular stretching (quadriceps femoris, hamstring, and calf muscle stretching)
- Long-sitting knee flexion and extension range of motion, treadmill walking
- All lower-extremity exercises should be done bilaterally.
- Manual therapy can help treat osteoarthritis. A systematic evaluation found that manual therapy (mobilization with movement, passive joint mobilization, patellar mobilization therapy) and exercises effectively reduce knee discomfort and improve function. However, more research is required to assess the long-term effects of manual treatment on knee osteoarthritis.
There are three kinds of exercises you should aim to include the following:
- Range of motion exercises
These exercises involve moving joints through a comfortable range of motion before smoothly and gently easing them just a little bit further. - Strengthening workouts.
These are resistance-based exercises that strengthen the muscles that move and support your joints. You may use light weights, a resistance band, or work out in the water. - Aerobic workout.
This refers to any physical exercise that increases your heart rate and causes you to breathe more heavily. This form of activity burns calories, which can help you lose weight. It can also help you sleep better and feel less pain. - Walking, cycling, and swimming are all great kinds of exercise for those with arthritis. Alternatively, you may try an exercise bike or a cross trainer. Walking laps at the shallow end of a swimming pool is also an excellent way to improve leg muscles.
- Hydrotherapy or aquatic therapy pools are warmer than traditional swimming pools. The warmth soothes and reduces pain and stiffness, whereas the water supports your weight while also providing resistance for muscle-strengthening workouts.
Mobility and the Alteration Training Techniques
Agility Techniques:
- Sidestepping
- Braiding (lateral stepping, forward and backward crossover steps)
- Front crossover steps during forward ambulation.
- Back crossover steps during backward ambulation.
- Shuttle walking (forward and backward walking to and from specific markers)
- A drill that requires many changes in direction.
- Perturbation methods and balance training
Weight Loss and Diet
If you are overweight, decreasing even a small amount of weight can significantly improve your symptoms, particularly in weight-bearing joints (the hips, knees, back, and feet).
The most effective approach to losing weight is to eat a healthy, balanced diet. Reduce the number of calories you consume from high-fat and sugary foods, but ensure that you include all of the important food groups in your diet to avoid missing out on essential nutrients. Gradually increasing your physical activity will also help you lose weight.
There is no single diet that has been shown to help with osteoarthritis. If you suspect that a particular meal aggravates your symptoms, you should try eliminating it for a few weeks before reintroducing it. Be wary of any diet that claims to treat arthritis or recommends eliminating a specific food group.
Some suggest consuming fatty fish or fish oils may help with the symptoms of certain types of arthritis, particularly rheumatoid arthritis. However, increasing your intake of fatty fish or taking a supplement may be worthwhile if you want to use nutrition to control osteoarthritis.
Complementary medicine for osteoarthritis.
Taking supplements
In many circumstances, there is limited evidence that vitamins and herbal therapies can alleviate arthritis or its symptoms, although many people believe they help.
The following are some of the supplements commonly taken by people with osteoarthritis.
- Glucosamine: Glucosamine occurs naturally in the body in structures such as ligaments, tendons, and cartilage. Supplements are often made from crab, lobster, or prawn shells, however, shellfish-free options are available. Some research suggests that it may help with painful osteoarthritis, particularly in the knee. Most trials employed a dose of 500 mg thrice daily, and the evidence suggests that glucosamine sulfate may be more beneficial than glucosamine hydrochloride. It does not relieve pain immediately, therefore you will need to take it for a few months. If it hasn’t helped after two months, it’s unlikely to.
- Chondroitin: Chondroitin is found naturally in our bodies and is known to help cartilage maintain its suppleness. The study evidence is restricted to animal studies, which indicates that it may aid in halting cartilage breakdown. Don’t expect any progress for at least two months. And if your cartilage is severely injured, you are unlikely to profit from chondroitin.
- Fish Oils: Fish oils and fish liver oils are widely regarded to be helpful to the joints. In truth, there is little research to determine if they are useful for osteoarthritis, although there is strong evidence that fish oils can help with rheumatoid arthritis symptoms. Supplements derived from fish livers frequently contain high levels of vitamin A, which can be dangerous in excess. Supplements made from whole fish typically include less vitamin A, making them safer if you find that you require a large dose of fish oils to reap any additional advantages.
- Complementary treatments: There are several various therapies available, and they can usually be combined with prescribed or over-the-counter medications.
Some of the most popular therapies are listed below:
- Acupuncture claims to restore the natural balance of health by putting small needles into precise places on the body to rectify abnormalities in the flow of energy. Acupuncture has been shown to help reduce some osteoarthritis symptoms.
- The Alexander technique teaches you how to be more aware of your posture and move with less physical effort. There is evidence that it can help with low back pain, but not specifically osteoarthritis.
Aromatherapy employs plant oils that can be vaporized, breathed, used in baths or burners, or included in an aromatherapy massage. There is no proof that aromatherapy is good for osteoarthritis symptoms, however, it can help patients relax. - Massage can relax stiff muscles, relieve tension, improve muscular tone, and promote blood flow. A good massage might make you feel calm and cared for, but there’s little evidence that it helps treat osteoarthritis.
- Osteopaths and chiropractors manually modify the body’s posture and apply pressure on its soft tissues. The goal is to address weaknesses in structure, increase mobility, alleviate discomfort, and allow the body to heal naturally. There is limited research evidence that chiropractic is useful for spinal osteoarthritis. However, there is no particular research proof on whether osteopathy is useful in treating osteoarthritis.
- T’ai chi is a mind-body exercise that uses slow, smooth movements to relax the mind and promote self-healing. There is good evidence that t’ai chi can help with osteoarthritis symptoms, particularly in the knee.
Surgical treatment
Surgery: Most people do not require surgery to treat osteoarthritis. If you have significant symptoms and alternative therapies have not been effective, your provider may propose surgery. You may need a joint replacement (arthroplasty). Your provider or surgeon will explain what to expect.
Joint surgery can repair or replace severely injured joints, particularly the hips and knees. A doctor is going to refer an eligible patient to an orthopedic surgeon for surgery
Surgery is typically considered a last resort for osteoarthritis patients who have exhausted other therapy options.
Options include:
- Joint Replacement Surgery: Arthroscopy lavage is a type of keyhole surgery that removes loose bone fragments and tissue from the knee. Joint fusion is a surgical procedure that fixes the bones of a joint, preventing movement and pain.
If you’re considering having surgery, take some time to learn what to expect, what the risks are, and how you can best prepare for your procedure and plan for your recovery. - Splints and Other Supports: There are a variety of splints, braces, and supports available for joint pain. These can be especially useful if osteoarthritis is affecting a joint’s alignment. Before deciding on one, you should seek expert counsel from an occupational therapist or physiotherapist to make sure that it is suitable for your needs.
- Footwear: Choosing comfortable, supportive shoes will be helpful to not only your feet but also to other weight-bearing joints such as the knees, hips, and spinal joints. In general, the perfect shoe would have a thick but soft sole, soft uppers, and sufficient space for the toes and ball of the foot. If you have specific foot concerns, you should consult a podiatrist for more information.
- Walking Aids: If your leg occasionally ‘gives way’, a stick can help you feel less fearful of falling. When held in the opposite hand, it might assist relieve pressure on a sore knee or hip. It is important to get assistance from a healthcare practitioner, as the reason for utilizing a stick will determine which side to use it on.
- Posture: If you have arthritis, good posture might assist in reducing strain on your joints. When you have good posture, your body feels more relaxed. Think about your posture all day. Check yourself when walking, working, driving, or watching television.
- Pacing yourself: If your pain changes from day to day, it’s tempting to take on too much on good days, which might lead to additional pain later. Learn how to pace yourself. If there are jobs that frequently cause you discomfort, try breaking them down, scheduling rest periods, and alternating with easy jobs. Consider different ways of carrying out work that would be less painful.
Osteoarthritis can have many different effects on your life, but there are steps you can take to alleviate the symptoms.
Diet for osteoarthritis
Foods to focus on:
- Fruit and vegetables: These are high in antioxidants and anti-inflammatory chemicals, providing a wide range of health advantages. Aim for a wide range of colors, including berries, citrus fruits, leafy greens, bell peppers, and tomatoes.
- Omega-3 fatty acids are found in fatty fish such as salmon, mackerel, and sardines and have been shown to have anti-inflammatory qualities. Aim for two servings each week.
- Whole grains are higher in fiber, important nutrients, and sustained energy than refined grains. Choose brown rice, quinoa, oats, and whole wheat bread.
- Healthy fats: Olive oil, almonds, and seeds are good sources of vital fats and have anti-inflammatory properties. Include them in moderation as part of a healthy diet.
- Legumes: Beans, lentils, and chickpeas are high in plant-based protein, fiber, as well as important minerals such as magnesium and folate. Add them to soups, stews, and salads.
Foods to Limit:
- Red meat and processed meats can cause inflammation and aggravate osteoarthritis symptoms. Limit your intake and choose thinner cuts while consuming.
- Added sugar and processed carbohydrates: Sugary drinks, pastries, and white bread can cause inflammation and weight gain, increasing joint stress. Choose naturally sweet fruits and complex carbohydrates instead.
- Unhealthy fats: Saturated and trans fats found in fried foods, fatty meats, and processed snacks can exacerbate inflammation. Minimize your options.
- Excessive alcohol consumption can cause inflammation and interfere with nutritional absorption.
Living With
What can I do to make life with osteoarthritis easier?
You may need to adjust your routine to make life with osteoarthritis easier. Depending on when you get symptoms (and how severe they are), you may need to avoid or modify your activities while you manage them. If you require assistance with your daily duties, you may consider working with an occupational therapist. Occupational therapists are healthcare professionals who can assist you with physical issues such as arthritis. They may recommend:
- Adaptive equipment, such as grips to open jars.
- Techniques for conducting hobbies, sports, and other activities safely.
- Tips for relieving joint discomfort during arthritis flare-ups
When should I see my healthcare provider?
If you observe any symptoms of osteoarthritis, see a doctor right once. Even minor joint pain can indicate the need for treatment, especially if it persists for more than a few days.
You can’t restore existing cartilage degeneration (breakdown), but commencing osteoarthritis treatment will help slow down additional damage inside your joints.
Consult your doctor if you notice that your symptoms are recurring or becoming more severe than before. Ask your provider about additional treatment options or changes you can make to your current treatments if you believe they aren’t functioning as well as they should.
Osteoarthritis Risk Factors
Anyone can get osteoarthritis. Adults over the age of 55, as well as those in menopause, are more likely to get osteoarthritis.
People with specific health issues are more likely to have osteoarthritis.
- Obesity (BMI greater than 30) or overweight (BMI over 25).
- Diabetes.
- Hyperlipidemia (high cholesterol).
- Some autoimmune disorders damage the joints.
- Age. The most important risk factor is age. Cartilage gradually breaks down with age, leaving older people more susceptible to osteoarthritis.
- Genetics: A family history of OA considerably raises your risk, indicating a genetic susceptibility.
- Joint injury: Fractures, rips, or ligament damage can all degrade cartilage and raise the risk of OA in that particular joint.
- Repetitive stress: Jobs or activities that require repetitive movements or improper load on certain joints might lead to OA over time.
- Obesity. Obesity increases stress on weight-bearing joints such as the knees and hips, speeding up cartilage degradation and the development of osteoarthritis.
- Muscle weakness: Weak muscles around joints make them less stable and more prone to injury and arthritis.
- Bone deformities: Abnormalities in bone alignment or structure can cause uneven strain on joints, resulting in OA.
- Certain medical diseases, such as rheumatoid arthritis and gout, can cause joint damage and raise the risk of osteoarthritis.
- Sex: Women are statistically more prone than males to develop osteoarthritis, especially after menopause.
- Occupation: People who work in jobs that require heavy lifting, kneeling, or kneeling for long periods are more likely to develop OA in certain joints.
- Nutritional deficiencies: Low vitamin D and calcium levels may contribute to bone weakening and, indirectly, the development of osteoarthritis.
Prevention
The greatest strategy to avoid osteoarthritis is to maintain good general health, including:
- Avoiding tobacco products.
- Performing in low-impact exercise.
- Following a good food plan.
- Always wear your seatbelt.
- Wear suitable protection equipment for any activity, sport, or job you are undertaking.
- Visit a healthcare provider frequently and as soon as you notice any changes in your joints.
- Maintain a healthy body weight. Excess weight puts more strain on your joints, raising your risk of osteoarthritis.
- Stay active. Regular exercise strengthens the muscles surrounding your joints, helping to protect them from harm.
- Select low-impact activities. Swimming, walking, and biking are all lower-impact exercises compared to running and jumping. warm-up before exercise.
- After you’ve finished exercising, cool down. Cooling down helps to avoid muscle discomfort and stiffness.
- Exercise using the correct form. Using appropriate forms helps to prevent undue stress on your joints.
- Wear supportive shoes. Supportive shoes can reduce shock and protect your joints.
- Eat a nutritious diet. Eating a nutritious diet can assist in preventing inflammation and maintaining joint health.
- Avoid smoking. Smoking can raise your risk of developing osteoarthritis.
- Schedule regular appointments with your doctor. Regular examinations can assist you detect any early signs of osteoarthritis, allowing you to begin treatment earlier.
Complications
The changes in cartilage that occur with osteoarthritis can cause crystals to develop within the joints. These might be:
- Sodium urate crystals can trigger gout attacks. The big toe is the most often affected joint.
Calcium pyrophosphate (CPP) crystals may result in acute discomfort and edema. CPP crystals can affect any joint, although they are more common in those already affected by osteoarthritis. - Pain and stiffness are the most common complications of osteoarthritis, and they can range from minor to severe. The discomfort may be constant or irregular, making it difficult to move your joints.
- Reduced mobility: OA can make it difficult to move, climb stairs, or get out of bed. This can lead to a dependence on others for assistance with everyday activities and raise your risk of falling.
- Joint damage: Over time, OA can harm the cartilage and bone in your joints. This might cause abnormalities, such as bone spurs, which may aggravate the pain.
- Other health issues: Obesity, heart disease, and depression are also possible complications of OA.
- Osteonecrosis: A condition in which bone tissue dies. It can be caused by osteoarthritis or by taking certain medications, such as corticosteroids.
- Baker’s cyst: A fluid-filled sac that develops under the kneecap. It may be caused by OA or other disorders.
Conclusion
Most osteoarthritis patients must manage their symptoms for the remainder of their lives. Your doctor will assist you in determining the best treatment regimen for managing your symptoms.
If you have osteoarthritis, you should stay as active as possible. If joint pain and other symptoms make it difficult for you to move, you may be at a higher risk of developing major health disorders such as heart disease, diabetes, and some types of cancer.
Consult your doctor if osteoarthritis makes it difficult (or impossible) to stay active. They’ll assist you in discovering new ways to control your problems.
- Stable symptoms: Some persons suffer limited progression, allowing them to manage pain and continue with their normal activities.
- Functional limits may arise as the disease develops, making movement and daily tasks more difficult and requiring the use of assistive devices or support.
- Joint replacement surgery: In cases of severe arthritis, surgery may greatly improve function and quality of life.
General Outlook:
- No Cure: Osteoarthritis is a progressive disease that cannot be cured. However, there are numerous ways to treat symptoms and slow their progression.
- Individual Variability: The prognosis for each person differs depending on individual characteristics such as:
- Affected joints: Weight-bearing joints (knees, hips) frequently see rapid development.
- Severity: Early diagnosis and management result in better outcomes.
- Overall health: Underlying conditions and lifestyle choices affect progress.
- Symptom Management: Most people manage their symptoms for the rest of their lives, with a focus on pain reduction, mobility, and quality of life.
Prognosis
The prognosis for patients with OA differs based on the affected joint. Patients with bilateral knee OA experience faster deterioration than those with fewer joints afflicted. Patients with several medical diseases (heart and lung) are more likely to suffer from lower extremity disability than those with only knee arthritis. Medication does not stop the progression of OA, but it can improve the patient’s quality of life by reducing discomfort. Physiotherapy can assist in identifying and adjusting joint-stressing activities, as well as reduce osteoarthritis symptoms.
FAQs
At what age does osteoarthritis usually begin?
Osteoarthritis mainly affects persons over the age of 55. However, there is no specified schedule or age limit for when you may experience it. It also doesn’t start the way some health disorders do — there’s not always a clear starting point your healthcare professional can properly identify.
It can take a long time for the cartilage in your affected joints to wear down to the point where pain and stiffness develop. So, even if you discover symptoms around the age of 55, it may not indicate that osteoarthritis started at that time.
What should you not do if you have osteoarthritis?
Repetitive motions. Repetitive actions could speed up the damage to joints already caused by osteoarthritis. These motions can result from work or leisure activities. It is important to take frequent rests and use the proper form if some actions are unavoidable.
What are the ten foods you should avoid if you have osteoarthritis?
Foods to Avoid with Arthritis
Added sugars. Everyone can benefit from lowering their sugar intake, especially those with arthritis. …
Processed and red meat.
Foods that contain gluten.
Examples of highly processed foods include certain vegetable oils.
Salty foods.
Foods with high AGE levels
What are the top five vegetables to avoid for arthritis?
Some people with arthritis argue that nightshade vegetables such as tomatoes, potatoes, eggplants, and peppers cause their condition to aggravate. While there is little evidence to establish a link between arthritis discomfort and most nightshades, tomatoes could be an exception. This is because they increase levels of uric acid.
Is egg helpful for osteoarthritis?
On the contrary, eggs have been confirmed to contain chemicals with potential anti-inflammatory activity. Most adults, including those suffering from arthritis, are advised to consume two eggs per week as part of a well-balanced diet.
Is rice unhealthy for arthritis?
5 Foods to Avoid with Arthritis. Aim to avoid refined carbs. White bread, white rice, grocery store cereals, and other refined carbohydrates fall within this broad category. Digesting refined carbs may cause or aggravate the release of cytokines, often known as inflammatory messengers in the body.
What drinks are beneficial for arthritis?
7 Beverages to Reduce Arthritis Pain
Tea. Tea is one of the greatest beverages for arthritis patients because it has numerous health advantages. … Milk. Contrary to popular opinion, if you have arthritis, you do not need to avoid dairy products. Drink options include coffee, fresh juices, smoothies, red wine, and water.
When to seek medical advice
Can I drink milk with arthritis?
For the most part, the benefits of reducing dairy are extremely individual, and there is insufficient evidence to recommend that persons with arthritis avoid milk. Tips: Drinking milk, which is high in calcium, vitamin D, and protein, may help avoid gout and slow the course of osteoarthritis (OA).
How do I lubricate my joints naturally?
8 Simple Ways to Improve Joint Lubrication and Health
Warm up and drink up! To get those juices flowing, begin your workout with a mild 5-10-minute warm-up and progressively raise the duration of your workout.
Stretch regularly.
Work on your strength.
Give some TLC…
Exercise in different ways.
Lose some weight.
Take a warm bath or shower.
Get some ZZZs.
What’s the finest oil for joints?
Dr. recommends applying 15 drops of essential oil, such as lavender, chamomile, or eucalyptus, directly on the skin. Dilute the oil with 1 oz. (2 Tbsp.) of a “carrier” or neutral oil, such as almond, avocado, or jojoba.
Which oil supplement is best for the joints?
three Best Fish Oils…
Nature’s Branch Triple Strength Omega 3 Fish Oil Supplements.
VitaMedica Super EPA and DHA Fish Oil.
OceanBlue Professional Omega-3 2100
What are the two best spices for arthritis?
Best Spices for Arthritis. General Tips for Using Spices.
Anti-inflammatory Spice Basics. When you have arthritis, your joints and other parts of your body become inflamed, and several species block particular inflammatory pathways in the body. Ingredients include garlic, turmeric, ginger, cinnamon, and cayenne.
Reference
- Professional, C. C. M. (n.d.). Osteoarthritis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
- Osteoarthritis (OA). (n.d.). Versus Arthritis. https://versusarthritis.org/about-arthritis/conditions/osteoarthritis/
- Osteoarthritis. (n.d.). Physiopedia. https://www.physio-pedia.com/Osteoarthritis
- Knee Osteoarthritis. (n.d.). Physiopedia. https://www.physio-pedia.com/Knee_Osteoarthritis
- Therapia – Physiotherapy for Osteoarthritis. (2020, November 10). Therapia. https://therapia.com/conditions/physiotherapy-for-osteoarthritis/







66 Comments