Knee Pain
What is Knee Pain?
Knee pain is a common ailment affecting people of all ages and backgrounds, often stemming from a variety of causes ranging from overuse injuries to degenerative conditions.
People of all ages frequently complain about knee pain. The knee joint is complex and vulnerable to various injuries and conditions that can lead to pain and impaired function. Knee pain can range from mild and temporary to severe and debilitating. Some common causes of knee pain include injuries to ligaments, tendons, or cartilage, arthritis, infections, and inflammatory conditions.
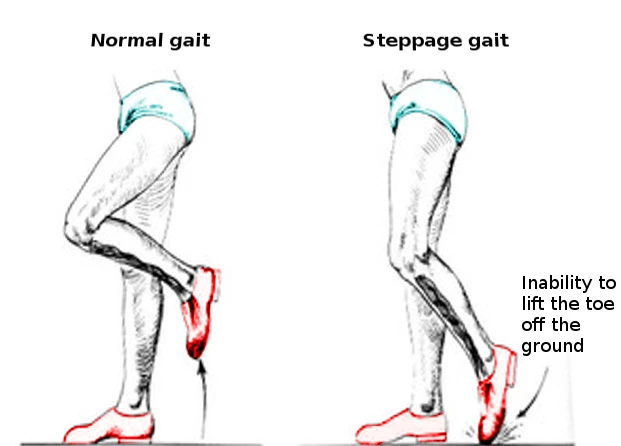
Symptoms of knee pain vary depending on the underlying condition but may include swelling, stiffness, difficulty bending the knee, limping, locking, or buckling of the knee joint. The location and type of pain also differ based on the structure that is damaged. Front knee pain is most common and often associated with overuse activities or patellofemoral pain syndrome. Inner or outer knee pain can signal injury to cartilage, ligaments, or bursae.
Getting an accurate diagnosis is important to determine the right treatment plan. A physical examination of the knee joint along with imaging tests like X-rays, MRI scans, or CT scans can help the doctor assess damage to bone, ligaments, tendons, and soft tissues. Other tests like joint aspiration or blood tests may also be done to aid diagnosis.
Treatment aims to reduce pain and inflammation while preserving movement and function. Options range from nonsurgical options like rest, physical therapy, braces, taping, and medications to surgery for repairing damaged structures. Maintaining appropriate strength, flexibility and biomechanics with physical therapy can also help prevent re-injury. While most cases of knee pain can be managed conservatively, severe injuries like ligament tears may require surgical reconstruction.
Clinically Relevant Anatomy
Bones
- Femur – The thigh bone which forms the proximal end of the knee joint. Femoral fractures or tumors can cause knee pain.
- Tibia – Forms the distal end of the knee joint. Tibial plateau fractures can occur and lead to knee pain.
- Fibula – Located on the lateral side of the tibia. Fractures of the proximal fibula can impact knee stability.
- Patella – The kneecap which articulates with the distal femur. Fractures, subluxation, or chondromalacia can cause anterior knee pain.
Joint Structures
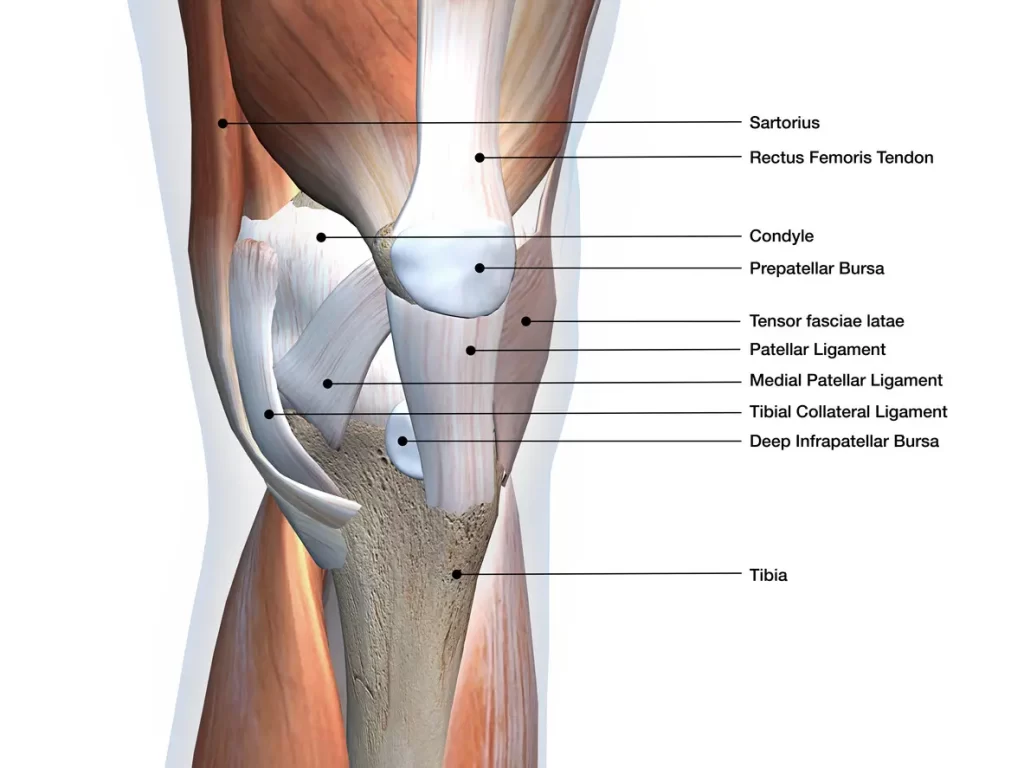
- Articular cartilage – Covers ends of femur, tibia, and patella. Injury and wear can cause pain and osteoarthritis.
- Meniscus – Provides shock absorption and stability. Tears often cause pain, and locking of the knee.
- Synovial membrane – Lines joint cavity, produces fluid to lubricate the joint. Inflammation causes swelling and pain.
- Joint capsule – Surrounds the entire joint. Tears can cause instability and pain.
- Cruciate ligaments (ACL, PCL) – Provide front-to-back stability. Tears cause instability and can damage other structures.
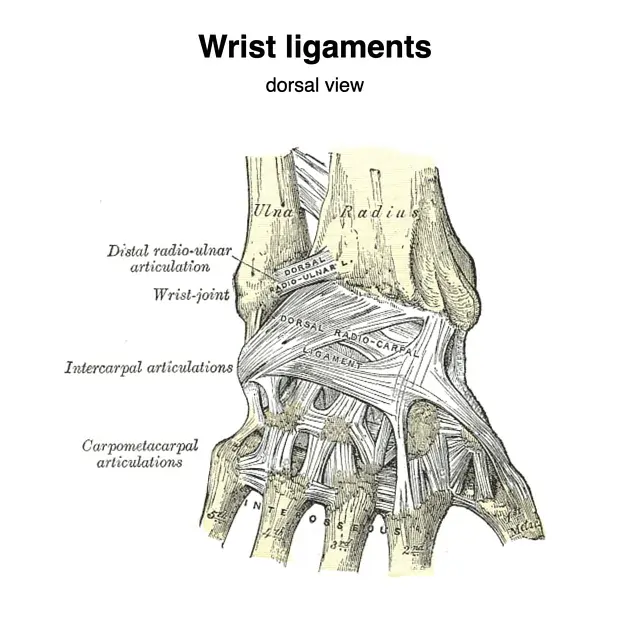
- Collateral ligaments (MCL, LCL) – Provide side-to-side stability. Sprains are common causes of acute knee pain.
Muscular Structures
- Quadriceps – Group of 4 muscles on the front of the thigh that extend the knee. Strains are common.
- Hamstrings – Posterior thigh muscles that flex the knee. Strains can cause posterior knee pain.
- Iliotibial band – Tendon that runs along the lateral knee. Friction syndrome causes lateral knee pain.
Bursae
- Prefemoral, suprapatellar, infrapatellar bursa – Provide cushion and reduce friction. Inflammation causes pain.
Nerve Supply
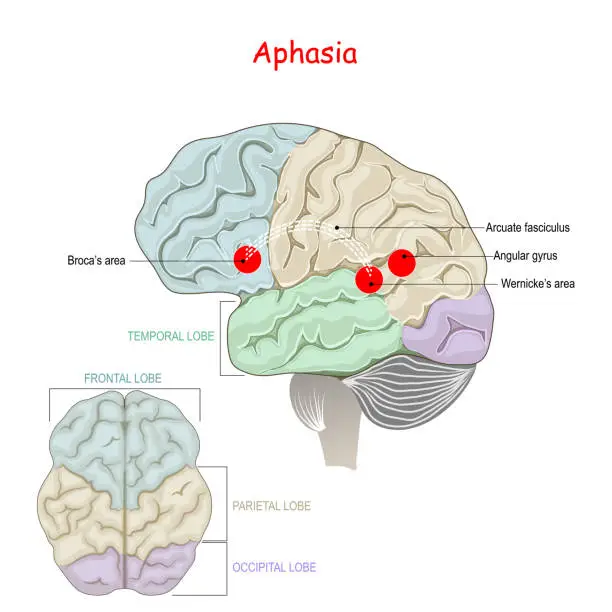
- The femoral nerve – supplies sensation to the anterior knee
- Sciatic nerve – supplies sensation to posterior knee
- Tibial nerve – supplies sensation to medial/posterior knee
- Common fibular nerve – supplies sensation to lateral knee
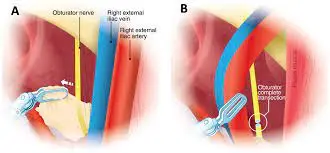
- Obturator nerve – less common, can contribute to inner knee pain
Blood Supply
- Femoral artery – major blood supply to the knee joint and muscles
- Popliteal artery – forms geniculate branches that supply distal femur and knee
- Anterior tibial recurrent artery – supplies anterior knee region
- Circumflex fibular artery – supplies lateral knee region
Causes of Knee Pain
Injuries
Sprains
- Injury to a ligament resulting from excessive or abnormal stretching
- Most commonly involves injury to the medial collateral (MCL), lateral collateral (LCL), or posterior cruciate ligaments (PCL) of the knee
- Caused by sudden twisting, turning, impact or over-stretching
- Symptoms: pain, swelling, instability, bruising
Strains
- Injury to a muscle or tendon by over-stretching, forceful contraction
- Common in the hamstrings or quadriceps muscles around the knee
- Caused by activities like running, jumping, acceleration/deceleration
- Symptoms: mild to severe pain, tenderness, muscle spasm and weakness
Tears
A. Meniscus tears
- Involve injury to the crescent-shaped fibrocartilage shock absorbers
- Medial meniscus tears most common
- Caused by sudden twisting, deep squatting, lifting
- Older people are vulnerable due to tissue degeneration
- Symptoms: pain, catching, locking, instability, swelling
B. ACL/PCL tears
- Injury to cruciate ligaments that cross inside the knee
- ACL tears are more common, especially in athletes
- Usually occur with sudden stops/changes in direction and landing from a jump
- This leads to instability and can increase the risk of other knee injuries
- Symptoms: pop sound, instability, swelling, loss of range of motion
C. Cartilage tears
- Involve injury to the articular cartilage covering knee bones
- Often related to trauma and high-impact activities
- Can progress to larger lesions, bone defects, loose bodies
- Increased risk for osteoarthritis
- Symptoms: localized pain, swelling, locking or catching
Fractures
- Break in continuity of a bone around the knee joint
- Common in patella (kneecap), distal femur, proximal tibia
- Caused by high-impact injuries, trauma from falls, motor collisions
- Pain depends on location, extent, displacement of fracture fragments
- Open fractures more severe with broken skin, higher infection risk
Dislocations
- Complete loss of contact between articulating bones in the knee joint
- Most often patellar dislocation (kneecap shifts out of the trochlear groove)
- Also, the risk of injury to ligaments, cartilage, nerves, and blood vessels
- Significant trauma and force required to cause dislocation
- Symptoms include severe pain, deformity, instability, limb shortening
Arthritis
- Degenerative joint disease involving wear-and-tear damage to cartilage
- The most common type affects the knees
- develops gradually over time, worse with age
- Loss of cartilage cushion causes bone-on-bone friction, bony spurs
- Pain, swelling, and stiffness that’s worse with activity, eased by rest
Rheumatoid arthritis
- Autoimmune inflammatory arthritis
- Synovial inflammation injures cartilage and bone over time
- Systemic symptoms like fever, fatigue in addition to joint pain
- Morning joint stiffness common
- Can cause gradual joint destruction, disabilities
- form of inflammatory arthritis caused by uric acid crystal deposits
- Often affects the joint at the base of the big toe, but can occur in the knees
- Intense flare-ups of joint pain, swelling, redness and tenderness
- Pain starts suddenly, often at night or after specific foods/alcohol
- Crystals stimulate the release of pro-inflammatory chemicals
Pseudogout
- Inflammatory arthritis caused by calcium pyrophosphate crystal deposits
- Affects the knees in about 15% of those with pseudogout
- Similar symptoms as gout – severe pain, swelling, tenderness
- Starts more gradually than gout but can last for weeks/months
- Risk increases with age, joint injuries, and other joint diseases
Tendonitis
Patellar tendonitis (jumper’s knee)
- Overuse injury to the patellar tendon connecting the kneecap to the shin bone
- Common in athletes and jumpers
- Caused by repetitive overloading or strain on the tendon
- Pain/tenderness just below the kneecap worse with activity
- Swelling may occur but often tendon simply degenerates
Iliotibial band syndrome
- Inflammation of IT band on lateral knee
- Caused by repetitive friction during activities
- Runners/cyclists often affected
- Lateral knee pain worse when walking/running downhill
- Tenderness at the lateral epicondyle of the femur bone
Bursitis
Pes anserine bursitis
- Involves pes anserine bursa near hamstring and MCL insertions
- Causes pain at the inner knee below the joint line
- Aggravated by medial knee strain, direct trauma, gout/RA
- Tenderness at the insertion of pes anserinus tendons
Infrapatellar bursitis
- Involves infrapatellar bursa under the patella
- This leads to pain below the kneecap
- Called clergyman’s knee or housemaid’s knee
- Aggravated by kneeling, squatting, stairs
- Noticeable swelling with fluid accumulation
Prepatellar bursitis
- Involves the prepatellar bursa anterior to the kneecap.
- Known as water on the knee
- Trauma, infection, and inflammatory arthritis can cause
- Fluid accumulation and swelling on the front knee
- Activities that stress the bursa will cause pain
Osgood-Schlatter Disease
- The condition causing pain below the knee joint in still-growing adolescents
- Related to inflammation and irritation of the patellar tendon
- Caused by overuse of running, and jumping in youth sports
- Swelling and pain get worse when you move and get better when you relax.
- Small bony ossicles may develop contributing to tendon injury
- Usually resolves on its own after skeletal maturity is reached
Fat Pad Impingement
- Also called Hoffa’s disease
- Involves irritation of the infrapatellar fat pad under the kneecap
- Can result from acute trauma or chronic overuse of the knee region
- Impingement from bone spurs or scar tissue also can cause pain
- Activities with kneeling, squatting, running, and jumping aggravate it
- Characteristic anterior knee pain not focal to a single structure
Infection
- Septic arthritis involves a joint space infection by bacteria or other microorganisms
- Can occur from the hematogenous spread of organisms or penetration injuries
- Sudden onset of severe knee pain along with fever and chills
- Significant joint inflammation leads to effusions and a limited range of motion
- Urgent treatment with joint drainage and antibiotic therapy needed
Bone Tumors
- Benign (giant cell tumor, osteoid osteoma, osteochondroma) or malignant
- Often present with progressive, worsening knee pain, sometimes at night
- Physical exam shows bony swelling, tenderness, limited motion
- Imaging like X-rays, MRI, and bone scans are required for diagnosis
- Treatment includes surgical resection, occasionally joint replacement
Symptoms of Knee Pain
Pain
Sharp Pain
- Sudden onset of intense or stabbing pain
- Results from acute injuries like ligament tears or fractures
- Subsidies quickly but may recur with re-injury
- Makes it difficult to bear weight or move the knee joint
Dull/Aching Pain
- Low-grade persistent pain more like soreness or discomfort
- Often associated with overuse injuries or arthritis
- Worsens slowly over time without acute event
- Aggravated by activities, may cause stiffness, especially with arthritis
Stiffness
- Difficulty fully straightening or bending the knee
- Taking initial steps after prolonged sitting is painful
- Gradually resolves with movement
- Common with osteoarthritis or inflammation after injury
Swelling
- Fluid accumulation in tissues surrounding the knee joint
- From inflammation, bleeding (hemarthrosis), or effusion
- Noticeable fullness, puffiness, or enlargement
- May cause a tight, stretched sensation around the knee
Locking/Catching
- Sudden loss of ability to fully extend the knee
- Painful episode resolves spontaneously
- Suggests mechanical causes like loose bodies, meniscal tear
- Catching is also described as popping, clipping, snapping
Instability/Giving out
- Feeling knee will buckle or fail to support body weight
- Results from ligament, cartilage, and tendon damage
- Requires immediate attention to prevent re-injury
Location of pain
Inner Knee Pain
- Medial joint line pain suggestive of medial meniscus or cartilage injury
- Pes anserine bursitis causes distinct tenderness below the medial joint line
- Medial collateral ligament sprains also cause inner knee discomfort
Outer Knee Pain
- Lateral joint line tenderness indicates lateral meniscus tear
- Iliotibial band friction syndrome causes lateral pain
- Injury to the lateral collateral ligament worsens on the outer aspect
Front of Knee Pain
- Patellofemoral syndrome behind the kneecap is common in young athletes
- Prepatellar bursitis causes swelling and inflammation over the kneecap
- Patellar tendonitis worsens just inferior to the patella
Back of Knee Pain
- Popliteal cysts compress nerves causing posterior discomfort
- PCL, posterior horn meniscus tears manifest as back knee pain
- Certain muscular strains radiate pain to the posterior knee
Aggravating Factors
Weight-bearing Activity
- Pain worse with walking, running, jumping
- Suggests injury to load-bearing structures like cartilage, meniscus
- Standing from sitting is also provocative early in osteoarthritis
Kneeling
- Direct compression aggravates conditions like prepatellar bursitis
- The infrapatellar fat pad is compressed causing impingement pain
- Difficulty regaining extension suggests loose bodies or synovitis
Squatting
- Flexing the knee with added body weight strains damaged structures
- Meniscus tears worsen, collateral ligaments stressed
- Getting up from a squat is more painful than descending
Walking Up/Down Stairs
- Stair ascent requires repeated knee flexion under load
- Stair descent increases demands on the quadriceps
- Often difficult in both directions with arthritis, patellofemoral pain
- Typically worse descending for patellar tendinosis
Diagnosis of Knee Pain
Medical History
- Onset, location, severity, nature of pain
- Associated symptoms like swelling, instability
- Inciting events or injuries
- Factors that aggravate vs relieve pain
- Prior treatments were attempted and the response
- Relevant health history, medications, lifestyle factors
Physical Exam
Palpation
- Check for joint line tenderness, swelling, masses
- Assess for warmth, effusion suggesting infection/inflammation
- Reproduce pain through the patellar grinding test
- Tenderness over structures indicates a likely source
Range of Motion Assessment
- Active and passive ROM tested in flexion and extension
- Compared to unaffected knee
- The limited motion suggests a meniscus tear, loose bodies
- Measure flexion contracture in osteoarthritis
- Patellar mobility is also important in anterior knee pain
Stability Assessment
- Test the integrity of the knee joint’s ligamentous structures
- Varus and valgus stress tests check medial and lateral collateral ligaments
- Anterior and posterior drawer tests check the cruciate ligaments
- Increased laxity or pathologic motion indicates ligament tear
- Effusion, and pain with testing also suggestive findings
Special Tests
1. Anterior Drawer Test – tests the integrity of the anterior cruciate ligament
- The patient lies supine while the examiner bends the knee to 90 degrees
- The examiner applies anterior/forward pressure to the proximal tibia
- Abnormal increased anterior translation indicates ACL tear
2. Posterior Drawer Test – tests the integrity of the posterior cruciate ligament
- Similar to the anterior drawer test
- The examiner applies posterior force to the tibia
- Increased posterior tibial displacement signifies PCL injury
3. Valgus/Varus Stress Tests – assess medial and lateral collateral ligaments
- The patient lies supine while the examiner holds the knee in slight flexion
- Applies lateral pressure to the knee for valgus stress test
- Applies medial pressure for a varus stress test
- Pain, the opening of joint space indicates collateral ligament sprain
4. McMurray’s Test – evaluates meniscal pathology
- The patient lies supine, examiner fully flexes the hip while the knee bent to 90 degrees
- Extends knee while applying valgus stress and external rotation
- A painful “click” felt deep in the joint suggests a torn meniscus
5. Thessaly Test – assesses meniscus injuries
- The patient stands flat-footed and fully rotates the knee medially/laterally 5 times
- Positive test causes pain/discomfort with rotation
- More sensitive for detecting meniscal pathology than McMurray’s
Imaging
X-rays
- First-line imaging modality
- Useful for assessing bony anatomy for fractures, arthritis
- Can detect smaller bone tumors or loose bodies
- Limited utility for soft tissue pathology
- Weight-bearing films provide functional assessment
MRI
- Detailed evaluation of ligaments, menisci, cartilage, and other soft tissues
- Non-invasive with excellent resolution of knee anatomy
- Detects subtle bone marrow changes suggesting pathology
- Used to definitively diagnose injuries before arthroscopic surgery
CT Scan
- Better visualization of bone detail than plain films
- Useful for occult fractures or assessing bony anatomy
- Lower cost and often sufficient for assessing fractures
- MRI is preferred for soft tissue assessment unless contraindicated
Other Tests
Joint Fluid Analysis
- Aspiration of synovial fluid with laboratory tests
- Cell count, crystals, culture, viscosity
- Septic arthritis is a high WBC count with positive cultures
- Helps differentiate inflammatory from non-inflammatory causes
Blood Tests
- Complete blood count, ESR, and CRP to detect infection
- Rheumatologic workup for inflammatory arthritis
- Uric acid levels if suspecting gout
- Important for understanding systemic factors contributing to symptoms
Treatment of Knee Pain
Conservative Treatment
Rest/Immobilization
- Taking weight off injured knee encourages natural healing
- Crutches facilitate protected weight-bearing
- Braces provide external support, limit painful motion
- Casting is rarely needed except with fractures, severe instabilities
Ice/Heat
- Ice reduces swelling and, inflammation, especially after acute injuries
- Use ice packs, and immersion to maximize coverage
- Do not apply directly to skin
- Heat improves blood flow before activity, loosens stiffness
- Use heating pads, and warm packs taking care to avoid burns
Medications
1. NSAIDs
- Oral anti-inflammatories like ibuprofen, naproxen
- Reduce inflammatory chemicals causing pain, swelling
- Upset stomach and ulcers are potential side effects
- Use caution if you have a history of specific diseases
2. Corticosteroid Injections
- Directly inject steroid medication into the knee joint or bursa
- Potent anti-inflammatory effects
- Can provide symptomatic relief for months at a time
- Risk of depigmentation or atrophy with repeated injections
Surgical Treatment
Arthroscopic Surgery
- A minimally invasive procedure where the surgeon inserts a tiny camera and instruments through small incisions around the knee
- Most commonly performed for:
- Meniscus tears- Remove or repair damaged meniscus cartilage
- Loose bodies- Remove loose fragments of cartilage or bone
- Arthritis- Remove inflamed synovial tissue
- Often performed on an outpatient basis
- Recovery time is usually 4-6 weeks
Total Knee Replacement
- Orthopedic procedure to resurface damaged knee joint
- Appropriate for patients with severe arthritis pain unresponsive to other therapies
- Involves surgical exposure of the femur, tibia, and patella to implant prosthetic joint components
- Components are made of metal alloys, high-grade plastics, and polyethylene
- May be traditional or computer-assisted for precision
- Hospital stay is 1-3 days
- Recovery time is about 6 weeks with physical therapy
ACL Reconstruction
- Repairs torn anterior cruciate ligament
- Often utilizes an arthroscopic approach with camera assistance
- Graft tendon from patient or donor used to reconstruct ACL
- Common grafts are patellar tendon or hamstring tendon
- Fixation done with screws or hardware
- Approximately 6 months recovery time
- Return to sports requires clearance after functional rehabilitation
Cartilage Grafting/Transplantation
- Treats articular cartilage injury and defects
- Transplants healthy hyaline cartilage to the damaged area
- Autografts use the patient’s cartilage tissue
- Allografts use donated cartilage tissue
- Also scaffolds and cell-based regeneration techniques
- Integrates transplanted cartilage into bone
- Relieves pain and restores function
- Rehabilitation is prolonged, over 8+ weeks
Physical Therapy Treatment
Electrotherapy Modalities
Transcutaneous Electrical Nerve Stimulation (TENS)
- TENS delivers small electrical impulses through electrodes placed on the skin
- Helps decrease pain signals reaching the brain and activate pain-inhibiting pathways
- Electrodes placed around the knee or on acupressure points
- Provides short-term pain relief during and after treatment
Interferential Current Therapy (IFT)
- Delivers medicated ions through the skin using electrical stimulation
- Transports treatments like dexamethasone or non-steroidal anti-inflammatories
- Reduces inflammation associated with conditions like arthritis or tendonitis
Neuromuscular Electrical Stimulation (NMES)
- use electrical impulses to elicit muscle and nerve activity
Iontophoresis
- Delivers medicated ions through the skin using electrical stimulation
- Transports treatments like dexamethasone or non-steroidal anti-inflammatories
- Reduces inflammation associated with conditions like arthritis or tendonitis
Kinesiology Taping
- Involves strategically applying specialized stretchable tape over and around affected joints
- Can lift skin/tissue, improve circulation, reduce pain, and provide joint stability
- Different techniques utilized depending on the goal:
- Patellofemoral pain: Tape was applied in a circular pattern over and under the kneecap and helps track the patella properly in the groove during knee bending
- Strains/sprains: Tape along ligaments in the direction of pull provides support
- Swelling/inflammation: Taping from distal to proximal aids drainage
- The tape is worn for 3-5 days, then replaced
- Can be used alongside other modalities like ice, exercises, medications
Soft Tissue Mobilization
- Involves kneading, compressing, and stretching soft tissues around the knee
- Breaks up adhesions between superficial and deep fascia layers
- Relaxes muscles, releases trigger points, improves flexibility
- Techniques:
- Effleurage – Gliding strokes warm tissues and aid venous/lymph return
- Petrissage – Kneading motions along muscle bellies
- Friction massage – Small cross-fiber movements ease chronic thickened tissue
- Trigger point release – Ischemic pressure applied to hyperirritable knots
- Allows better tissue mobility so the knee can move through a full pain-free range
- Decreases swelling and muscle tension contributing to knee pain
The combination of kinesiology taping for joint stabilization with soft tissue mobilization to relax muscles can significantly relieve multiple sources of knee discomfort.
Application of Heat or Ice
- Heat helps relax muscles, increase blood flow, and reduce stiffness/spasm
- Modalities like hot packs, paraffin wax, or moist heat pads
- Ice helps decrease inflammation and edema. Used for acute injuries
- Cryotherapy like ice packs, ice massage, or cold-water immersion
- Contrast therapy alternating heat and cold is also used
Assistive Devices
Crutches
- Help offload painful knee by bypassing lower extremity
- Axillary (underarm) or forearm types available
- Ensure proper sizing, fitting, and use of crutches
- Can protect postoperatively or with certain acute injuries
Knee Braces
- Custom or off-the-shelf varieties for stability/support
- Some feature hinges to guide motion in addition to support
- Help prevent excessive medial/lateral or anterior translation
- Useful postoperatively or with ligamentous knee injuries
Taping
- Specialized athletic tapes to provide external joint support
- Can help lift kneecap alignment in patellofemoral disorders
- McConnell taping most commonly used technique
- Must be applied properly ensuring no constriction
- Provides proprioceptive feedback during activity
Exercises for Knee Pain
Straight Leg Raises

- With your legs outstretched and your arms at your sides with your palms facing down, take a flat, flat lay position on your back.
- Plant that foot firmly on the floor while bending one knee. The other leg will remain straight. This is your stable leg.
- Tighten the thigh muscles of your straight working leg to lock the knee. Contract your quadriceps to keep the knee straight.
- Keeping the knee straight and quadriceps contracted, slowly raise your straight leg off the floor about 6-12 inches. Do not bend the knee.
- Hold the straight leg in the raised position for 2-5 seconds, feeling the quadriceps engage to keep the knee locked.
- Slowly lower the straight leg back down to the starting position in a controlled manner, but do not allow the back to arch off the floor.
- Repeat 10 times on that side, then switch legs and raise the opposite leg for 10 controlled repetitions.
- Rest 30-60 seconds between sets if needed. Complete 2-3 sets per side, progressing the number of reps or resistance tubing as muscle strength increases.
Proper form is very important with this exercise – keep abdominal muscles pulled in and the spine neutral against the floor at all times. Concentrate on slowly engaging the quadriceps in both directions.
Calf Stretch

- Stand facing a wall with your arms extended, palms on the wall at about eye level. Place one leg back with the foot flat on the floor. The other leg is bent at the knee with the foot positioned toward the wall.
- Keeping the back leg straight and heel planted, slowly bend the front knee until you feel a comfortable stretch in the back calf muscle. Make sure the back knee stays straight.
- Hold this mild stretch for 30 seconds while breathing slowly. Concentrate on relaxing the calf muscle.
- Release the stretch and repeat 2-3 times on that side. Then switch leg positions, placing the other foot back with the knee straight to stretch the opposite calf.
- To increase the intensity of the stretch, move the front foot slightly closer to the wall. Do not bounce or overstretch the calf.
- When the stretch feels less intense, bend the front knee more until you feel slight tension again in the calf. Hold each side for thirty seconds.
- Repeat the calf stretch 2-3 times per day, especially after exercise or periods of inactivity. Stretching both sides promotes flexibility.
Proper form is very important, so keep the back knee straight and heel grounded throughout the entire stretch. Modifications can be made using a step or wedge to achieve more range of motion as flexibility improves over time.
Hamstring Stretch

- Lean back and stretch both legs out. Bend one knee and draw that foot toward your buttocks. Grasp the thigh just below the knee with both hands.
- Straighten the knee of that leg toward the ceiling as far as is comfortable. Do not force the stretch. Stop short of pain while feeling tension in the back of the thigh.
- Hold the stretch for 30 seconds, breathing slowly and relaxing the muscles around the knee. Avoid bending the knee or lifting your hips off the floor.
- Release the stretch and repeat 2-3 more times on the same side, progressing the stretch slightly further each time while keeping the lower back pressed to the floor.
- Switch legs, repeating the hamstring stretch with the opposite leg. Gently extend knee until stretch is felt in hamstring, then hold 30 seconds. Complete 2-3 reps.
- Use a strap, rope, towel, or partner to help extend the leg further if needed, while keeping shoulders, and buttocks grounded.
Over time, flexibility will improve to stretch the knee to complete extension. Never force, bounce, or strain the lower back during this stretch. Go slowly to avoid injury. A mild-moderate tension stretch will produce optimal gains in flexibility.
Leg Extensions (quadriceps strengthening)

- Adjust the leg extension machine’s seat height so your knees are lined up with the machine’s pivot point.
- Sit up tall with full back support. Place feet under the padded lever, lining knee joints with the lever rotation axis.
- Keep the chest lifted, engage the core, and grip handles for stability. Ankles and knees ought to be 90 degrees apart.
- Extend one knee in a slow, controlled motion, fully straightening the leg against the resistance pad. Avoid locking knee hyperextension.
- Hold extended position 1 count. Squeeze quadriceps.
- Slowly bend the knee back to start position with control. Keep the weight stack from falling.
- Repeat for 10-15 reps. Complete 2-4 sets per leg with 30-60 sec rest between sets.
Proper form prevents injury: Avoid lifting buttocks from the seat during motion. Adjust resistance as strength increases over time.
Hamstring Curls
- Lie face down with a pad behind your ankles.
- Keep the torso, and pelvis flat on the bench. Stabilize upper body by holding handles or front of seat.
- Start with knees fully extended, and feet dorsiflexed. This is the muscle-lengthening position.
- Slowly bend knees up towards buttocks, pulling feet along pad’s arc toward the back of thighs.
- Squeeze hamstrings to achieve full knee flexion ROM. Hamstrings will be in the fully contracted position.
- Slowly reverse motion under control, straightening knees back to the open position without dropping the weight stack.
- Repeat 10-15 reps. Perform 2-4 sets with 30-60 sec rest between sets.
Proper form prevents injury: Avoid arching low back during motion. Adjust resistance level appropriately as strength improves over time.
Quadriceps Stretch
- Stand upright near a wall for balance. Bend one leg up and grasp the ankle with the same-side hand.
- Gently pull the heel toward your buttocks until you feel a mild stretch in the front of the thigh. Avoid over-arching low back.
- Keep knees together pointing straight down. Maintain an upright posture. Hold the stretch for 30 seconds.
- Release the stretch leg to the floor and repeat 2-4 times on each leg. Move the heel closer to the buttocks to gently increase the stretch as flexibility allows.
VMO Exercises
- Lie on the floor with knees bent at 90-degree angles. Place a small ball/pillow directly under one knee.
- Tighten quadriceps with knee pushed into a ball to activate VMO. Hold 5 seconds.
- Slowly straighten the knee until the leg is completely extended, keeping thigh tension.
- Slowly return to the starting position with knee bent at 90 degrees, foot on the floor.
- Repeat movement 10-15 times. Complete 2-3 sets per leg
- Progress by adding a resistance band above the ankles to provide light resistance against knee extension.
Remember to keep abdominal muscles tight throughout the motion to protect the lower back by stabilizing the pelvis.
Active Heel Slides

- Lie on the back with legs straight out on a smooth surface. Place a towel roll under the knee if needed.
- Place one foot flat on the floor. Slowly bend the opposite knee by sliding the heel toward the buttocks, maintaining foot contact with the floor.
- Use thigh muscles to actively pull the heel up the shin until a mild stretch is felt in the hamstrings or a pain-free range of motion is achieved. Do not force a stretch.
- Hold the bent knee position for 5 seconds while tightening the quadriceps.
- Slowly return to the starting position allowing the knee to slide back down, controlling descent with muscles.
- Repeat 10 times then switch legs. Build to 3 sets per side. Add towel roll thickness to progress the depth of slide motion.
Wall Squats

- Lean back into the wall with feet shoulder-width apart and placed 2 feet from the wall.
- Keep your lower back touching the wall. Bend your knees and slide slowly down the wall until your thighs are parallel to the floor. Do not go lower than 90-degree knee flexion.
- Hold a squatted position for 10 seconds while contracting quadriceps muscles. Stand tall, do not collapse your knees inward.
- Press into heels and slowly slide back up the wall return to upright standing knee extension. Keep abdominal muscles engaged for support.
- Repeat 8-10 times. Complete 2-3 sets. Can progress by holding dumbbells for added resistance or resting free hands behind the head with elbows out to the side.
Always follow the pain-free range of motion appropriate for current recovery status. Progress exercises slowly under guidance. Stop if swelling or discomfort persists. Consult a physical therapist or physician for modifications if needed.
Side Leg Raises

- Lie on one side with legs straight, resting head on lower arm. Place your top hand on the floor in front at shoulder level for support.
- Keeping both legs straight, the top leg in line with the lower leg, and slowly raising the top leg upwards as high as comfortably possible without twisting.
- Raise the leg to about 45 degrees. Pause 1 second. Feel engagement of hip and outer thigh muscles.
- Maintain a straight line from the shoulder joint through the hip and legs. Do not bend the knee or hip joint. Keep pelvis still.
- Slowly lower the top leg back to the starting position in a smooth, controlled motion. The leg should nearly graze the floor before repeating the raise.
- Complete 10-15 controlled reps before switching sides. Work to 2-3 sets per side.
Proper form prevents low back strain. Adjust height based on flexibility. Can use ankle weights to add resistance as able.
Prone Leg Raises

- Lie face down with legs straight out behind. Rest forehead on folded arms with a neutral spine.
- Keep legs straight with knees extended, and toes pointed. Contract glutes and lift one leg off the floor about 6 inches.
- Hold the raised leg position for 1-2 seconds before slowly lowering back to start with control.
- Repeat for 10-12 reps before switching legs. Complete 2-3 sets per side.
- For progression, add ankle weights for resistance. Or combine with alternating arm raises.
Always maintain stabilized spine alignment. Avoid overarching low back during lifts. Increase the number of repetitions gradually at first.
Home Care to Manage Knee Pain
Apply Ice Packs
- Use cold packs or ice for 15-20 mins several times per day, especially after activity
- Can help relieve acute pain or swelling from injuries
- Wrap an ice pack in a thin towel to protect the skin
Use Compression Bandage
- Compression wraps, sleeves, or braces can help stabilize the knee
- Useful for supporting weakened joints or reducing swelling
- Ensure proper sizing and do not wear overnight
Elevate Leg
- Prop legs up above the level of the heart while lying down
- Use pillows under the ankle/calf to elevate
- Helps decrease fluid buildup and knee swelling
Over-the-Counter Medications
- Acetaminophen or anti-inflammatories like Advil can relieve pain
- Topical menthol gels can ease arthritis achiness
Apply Heat Packs
- Heating pads, warm towels, hot water bottles can relax muscles
- Improves circulation and relieves stiffness before exercise
- Do not use heat for acute swelling or inflammatory conditions
Supportive Devices
- Canes, walkers, and knee braces take stress off injured knees
- Consult a medical supply store or physical therapist
Tips to Prevent Knee Pain
Maintain a Healthy Weight
- Carrying excess weight puts more stress on the knee joints during daily activities
- Losing weight takes the pressure off the knees and reduces the risk of osteoarthritis over time
Improve Muscle Strength in Legs
- Weak quadriceps and hamstrings can lead to poor stability and more injuries
- Do exercises to strengthen thigh and hip muscles 2-3 days per week
- This provides better joint support and shock absorption
Use Proper Form with Activities
- Incorrect form and alignment with exercise, sports increase injury risk
- Always warm up muscles before activity and use appropriate technique
- Wear supportive footwear designed for your sport or activity
Stretch and Roll Out Leg Muscles
- Flexibility in quads, hip flexors, and calves helps muscles function better
- Gentle stretching while warmed up can maintain a good range of motion
- Use a foam roller before and after workouts on thigh and calf tissues
Brace Unstable Knees as Needed
- Knee braces with hinges or sleeve supports can protect unstable joints
- Helps prevent awkward twisting or hyper-extensions
- Consult a doctor or athletic trainer to determine the best brace
Rest and Recovery After Injuries
- Give injured knees proper rest to promote healing
- Employ the rest, ice, compression, and elevation (RICE) regimen.
- Returning too quickly leads to re-injury or worsening damage
Ergonomic Tips to Prevent Knee Injuries for Occupations
Kneeling
- Use knee pads – Well-padded knee pads reduce pressure and distribute weight. Look for thick gel padding and non-slip backing.
- Take breaks – Frequently alternate tasks or straighten legs to avoid sustained kneeling which compresses the patella.
- Proper flooring – Low pile carpet or rubber workout flooring offers some cushion under the knees, unlike hard surfaces.
Squatting
- Use lower heights – Squat to lower surface levels or erect platforms to get closer rather than deeply squatting.
- Widen stance – Turning feet and knees outward reduces muscle strain required to balance in a deep squat.
- Step stools – Carry a small step stool for working at lower levels rather than holding a sustained squat.
Climbing Ladders/Steps
- Limit carrying weight – Heavier loads during climbing shifts balance and strain landing legs after descent.
- Ensure railings – Having bilateral rails aids stability when ascending/descending steep structures.
- Non-skid shoes – Wear footwear with textured soles for grip rather than smooth slip-on.
- Take fewer trips – Consolidate tasks requiring ladder ascents rather than repeated climbs.
Summary
Knee pain is a very common complaint with a wide variety of potential causes including injuries affecting ligaments, tendons, cartilage, or bones, different types of arthritis, overuse conditions, and occasional infections or tumors. Typical symptoms can be described as sharp or dull pain, swelling, stiffness, and instability and may be provoked by activities that load the joint. An accurate diagnosis is made based on medical history, physical examination assessing stability and structures involved, and appropriate imaging like x-rays or MRI and sometimes joint fluid analysis or blood work.
Initial treatment focuses on rest, ice, heat, medications like NSAIDs for pain relief and inflammation, braces, taping, or ambulatory aids to remove stress from the injury. Other options include injections, physical therapy to regain motion and strength, and surgery for damaged structures not amenable to conservative treatment.
Common surgical options include arthroscopy for meniscal repair or cartilage procedures, ACL reconstruction, fracture fixation, arthroplasty for arthritis, and biopsies or resections for tumors based on the underlying pathology. Identifying the origin of knee pain symptoms guides the appropriate management to reduce pain, preserve function, and prevent long-term impacts like osteoarthritis.
FAQs
What are the causes of knee pain?
The most common causes are osteoarthritis, injuries such as ligament tears or meniscus tears, tendonitis, bursitis, strains, dislocation, and overuse injuries.
When should I see a doctor for knee pain?
See a doctor if the pain comes on suddenly, doesn’t improve with rest over a few days, causes swelling/instability, prevents you from full weight-bearing, or interferes with sleep. Seek emergency care for injuries causing deformity.
How is knee pain diagnosed?
Diagnosis involves assessing pain location, onset, and severity along with a physical exam checking range of motion, swelling, tenderness, and ligament stability. Imaging tests like X-rays, and MRIs may visualize soft tissue damage or arthritis.
What home remedies help relieve knee pain?
Applying ice packs for 15 minutes several times a day, elevating the legs, OTC NSAID medications, and knee braces, and doing easy stretches and low-impact exercises can help manage knee pain at home.
When is surgery necessary for the knee?
If conservative measures fail for severe arthritis or complete ACL/meniscus tears, if fractures cause deformity, or if there is a progressive loss of function, surgical options range from arthroscopy to partial/total knee replacement.
What exercises are best for sore knees?
Low-impact cardio like swimming, cycling, or elliptical protects knees. Strengthening quads, and hamstrings maintains support around the joint. Stretching promotes flexibility of the calf, thigh, and hip muscles.
What lifestyle changes help knee pain?
Losing excess weight minimizes knee strain with movement. Shock-absorbing shoes cushion impact. Avoiding high-intensity pivoting sports prevents recurrent injury. Assistive devices ease mobility.
How to prevent future knee pain?
Build leg muscle strength, control weight, use proper form and technique with activity, rest/ice right after injuries, wear knee braces if prescribed, and balance leg flexibility with regular stretching.
References
Pt, B. S. (2023, March 20). Physical Therapy for Knee Pain. Verywell Health. https://www.verywellhealth.com/physical-therapy-for-knee-pain-2696411
Knee pain – Symptoms and causes – Mayo Clinic. (2023, January 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/knee-pain/symptoms-causes/syc-20350849
Cluett, J. (2023, May 9). Causes of Knee Pain and Treatment Options. Verywell Health. https://www.verywellhealth.com/knee-pain-symptoms-2549628
Dhameliya, N. (2023, November 1). Knee Pain: Cause, Symptom, Diagnosis, Treatment, Exercise. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/knee-pain-physiotherapy-exercise/
Lindberg, S. (2024, January 31). 10 Exercises to Help Relieve Knee Pain. Healthline. https://www.healthline.com/health/exercises-for-knee-pain
Knee Pain Overview. (2006, November 30). WebMD. https://www.webmd.com/pain-management/knee-pain/knee-pain-overview
A. (2021, July 19). Office Ergonomics and Knee Pain. SimpleTherapy. https://www.simpletherapy.com/blog/office-ergonomics-and-knee-pain/




42 Comments