What is a Semimembranosus Tendinopathy?
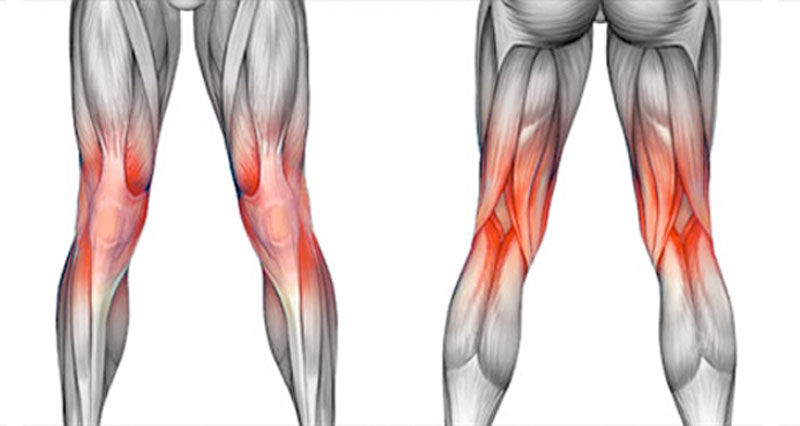
Semimembranosus tendinopathy is a condition characterized by pain, inflammation, and dysfunction of the semimembranosus tendon, which is one of the three hamstring muscles located in the posterior thigh.
Chronic knee pain is rarely caused by semimembranosus tendinopathy (SMT). Because the condition is not well understood, it could go undiagnosed or receive insufficient care. It is uncertain how often semimembranosus tendinopathy is in athletes, though it is most likely more prevalent in elderly patients.
The posteromedial side of the knee is typically painful when SMT presents. The distal semimembranosus tendon or its insertion on the medial proximal tibia are typically the sites of soreness that can be identified by physical examination.
The tendon of the three muscles (Semitendinosus, Sartorius, and Gracilis) that make up the pes anserinus runs on the medial side of the knee and inserts slightly below the tibia’s tuberosity on the medial side of the tibial plateau. To facilitate smooth tendon movement, there is a bursa beneath the tendon. When there is too much friction, the bursa is usually the one that ignites.
Related Anatomy
The lateral aspect of the ischial tuberosity is where the semimembranosus muscle originates. It descends along the thigh’s posteromedial aspect and inserts at the knee’s posteromedial aspect. The tendon that originates from the muscle belly ends just before the knee joint. It crosses medially to the gastrocnemius’s medial head and lateral to the smaller semitendinosus tendon. The tendon is thick and rounded.
Flexion and internal rotation of the knee joint are the semimembranosus muscle’s primary functions. In addition, it makes the hip joint extend and stabilizes the pelvis. The distal SM tendon is surrounded by a U-shaped bursa that divides it from the medial tibial plateau, MCL, and semitendinosus at its distal end. Degenerative alterations in the tendon and its insertions, as well as irritation of the bursa, can result from friction and recurrent eccentric tendon stress.
Pathophysiology (Mechanism of Injury)
The tendon that originates from the muscle belly ends just before the knee joint. It crosses medially to the gastrocnemius’s medial head and lateral to the smaller semitendinosus tendon. The tendon is thick and rounded. Semimembranosus tendinopathy usually appears at the main head, at reflected insertions, or in the distal tendon.
The medial femoral condyle, medial tibial plateau, semitendinosus tendon, and surrounding joint capsule all cause greater friction on the semimebranosus tendon during repeated knee flexion. Degenerative alterations in the tendon and its insertions, as well as irritation of the bursa, can result from friction and recurrent eccentric tendon stress.
Typical mechanisms of injury include the body attempting to make up for previous lower extremity injuries (meniscus tear) and stress imposed on the tendon as a result of an abrupt increase in training intensity, frequency, or duration. Activities that require the knee and hip to be used repeatedly and/or vigorously, such as distance running, triathlons, race walking, weightlifting, climbing, and running down slopes, increase risk. inadequate strength and flexibility, incorrect pre-activity warming up, flat feet, and misaligned knees (bowled over or knock knees).
Causes of Semimembranosus Tendinopathy
Usually the result of a primary phenomenon in athletes who compete for endurance or a subsequent overuse compensatory condition resulting from a primary defect in the knee. Many times, degenerative medial meniscal tears and chondromalacia patallae combine with other knee pathologies, which might potentially contribute to the cause and complicate the clinical picture.
Due to nearby osteophytes on the joint line, elderly individuals with osteoarthritis may experience semimembranosus tendinopathy in the anterior reflected tendon insertion. Concomitant pes anserine tendinitis is another common condition among these patients.
Components of total knee replacements may also result in secondary semimembranosus tendinopathy. While some writers have seen a strong preference for women, others have not. One could speculate that this has something to do with women’s Q angles and higher valgus stress.
In the same way, excessive foot pronation can increase valgus stress. Although there may be more contact between the SM tendon and the medial femoral condyle in both situations, none of these characteristics has been assessed in research as a risk factor for semimembranosus tendinopathy.
Symptoms of Semimembranosus Tendinopathy
Semimembranosus tendinopathy can present in a variety of ways, but often it manifests as a subtle, gradually worsening pain in the posteromedial part of the knee. When acute pain occurs after a very abrupt increase in endurance activity, like cycling or running, it can be very severe.
Patients typically feel discomfort at the direct insertion of the posteromedial knee, although it can also spread distally to the medial calf or proximally up the posteromedial thigh. Activities that significantly activate the hamstrings, such as running, cycling, stair climbing, or abrupt deep knee flexion, exacerbate symptoms.
Differential Diagnosis
The popliteal muscle strain, baker’s cyst, pes anserine bursitis, tibial osteonecrosis, and chronic MCL sprain are among the disorders that can produce pain in the medial portion of the knee. Both anterior and distal knee pain can be used to distinguish between pes anserine bursitis.
Other disorders such as medial compartment OA, medial meniscal tears, semimembranosus bursitis, or “snapping knee” syndrome may also be associated with or predispose to semimembranosus tendinopathy. The subluxation of the gastrocnemius and semimembranosus tendons causes snapping knee syndrome, which usually affects sportsmen who play a lot of sports.
Diagnosis
The diagnosis of tendinopathy, a syndrome characterized by tendon pain and thickness, is mostly made on the basis of the physical examination and patient history.
Ultrasonography (US) and magnetic resonance imaging (MRI) are the preferred techniques for seeing the hamstring tendon complex. Better soft tissue contrast is one of MRI’s benefits.
When it comes to identifying tendinopathy and peritendinous edema of the proximal hamstring tendons, it is more sensitive than the US. Imaging is used to determine the degree of damage and to establish the existence of hamstring tendon pathology.
A diagnosis can also be verified by a bone scan. Increased tracer uptake is seen at the proximal tibia’s posteromedial side.
Upon physical examination, the semimembranosus tendon feels sensitive when palpated close to its tibial insertion point or a little closer. The semimembranosus tendon may become more noticeable while resisting flexion of the knee to a 90° angle, facilitating examination. The pain may be localized with a knee flexed to a 90° angle and passive internal tibial rotation.
When nearby structures impinge on the injured tendon and/or insertion, passive deep flexion of the knee may also make the discomfort worse. It is important to assess the morphology of the hip, ankle, and foot for biomechanical characteristics that may contribute to the overuse of the semimembranosus tendon.
Treatment of Semimembranosus Tendinopathy
Mild painkillers like acetaminophen or nonsteroidal anti-inflammatory drugs like aspirin and ibuprofen are frequently advised. Follow the directions and take these. In the event of bleeding, upset stomach, or indications of an allergic reaction, get in touch with your doctor right once.
For this condition, prescriptions for painkillers are typically not issued.
If your doctor does recommend painkillers, be sure you take them exactly as prescribed.
Due to a lack of scientific data about the efficacy of currently used therapies, there is still no widespread agreement on the optimal conservative care of semimembranosus tendinopathy.
When it comes to conservative treatment, the methods used for semimembranosus tendinopathy are largely similar to those used for other tendinopathies. These methods include soft tissue mobilization, physiotherapy, reduction or pause of sports activity, nonsteroidal anti-inflammatory drugs (NSAIDs), relative rest and ice for the first phase of symptoms, and a continuous home exercise program with a focus on progressive hamstring strengthening.
Typically, a full recovery takes one to three months. Patients with chronic tendinopathy can benefit from the safe and efficient treatment of shockwave therapy.
Cold Pack: Cold therapy is used to lower inflammation and ease pain. For pain and inflammation, apply cold for ten to fifteen minutes every two to three hours. You should also apply cold right after engaging in any activity that exacerbates your symptoms. Apply ice packs or get a cooling massage.
Hot Pack: Before engaging in the recommended stretching and strengthening exercises, apply heat. Take a warm bath or apply a heat pad.
Corticosteroid Injections:
A corticosteroid injection may be taken into consideration as a temporary relief option in cases of extreme pain and inflammation that do not respond to conservative therapy. However, because of the possible adverse effects and risk of weakening the tendon, corticosteroid injections should be administered rarely and carefully.
Exercises for Semimembranosus Tendinopathy
These are a few of the basic exercises you can perform as part of your rehabilitation program until your symptoms go away or you schedule another appointment with your doctor, physical therapist, or sports trainer.
Please keep in mind:
Tissue that is flexible may withstand additional forces during activities.
A mild stretching feeling should be experienced during each stretch, which should be held for 20 to 30 seconds.
Stretching Exercises
Hamstrings Stretching:

- As demonstrated, lie on your back with your leg bent and both hands resting on it behind your thigh.
- With your thigh pointed directly up at the ceiling, your hip should be bent to a 90-degree angle.
- Extend your knee as far as possible. Maintain a straight leg pointed up at the ceiling.
- Maintain a flat surface with the opposite leg.
- Hold for 10 to 15 seconds.
- Perform exercise 2 times a day, or 8 to 10 times.
Doorway Hamstrings Stretch
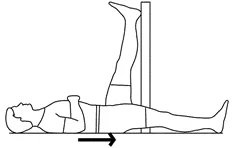
- As indicated, lie on your back close to a doorway’s edge.
- While maintaining your knee straight, place the leg you are stretching up the wall.
- Keep your other leg level on the ground and your buttock as close to the wall as you can.
- The back of your thigh ought to feel stretched.
- Hold for 10 to 15 seconds.
- Perform exercise 2 times a day, or 8 to 10 times.
Hamstrings, Ballet
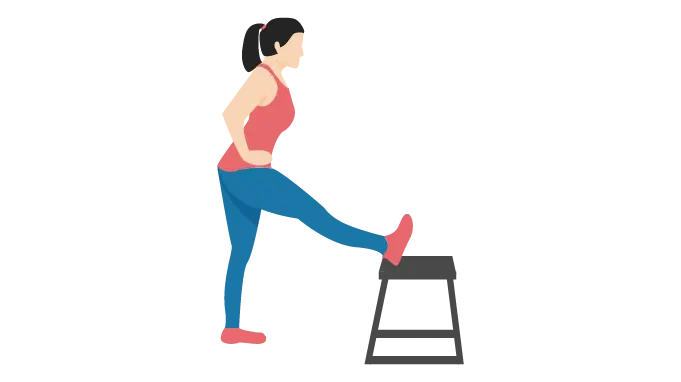
- Stretch your leg while standing, supporting it with a chair, table, or other sturdy object.
- Put both of your hands on the outside of the leg that has to be stretched.
- Verify that the leg you are stretching is facing your hips and pelvis as well.
- Gently run your hands along your leg’s exterior.
- Take the lead by using your breastbone. Maintain a straight back. Avoid stooped postures at the shoulders.
- Do not let your toes drop.
- The back of your thigh should feel stretched.
Hamstrings/Adductors, V-Sit
- With your legs as wide apart in front of you as possible, take a seat on the floor. Straightening your knees is necessary.
- Use both hands to lean over one leg.
- Reach for your toes while maintaining an erect chest.
- Hold for 10 to 20 seconds.
- Remain calm and take a step back to where you were.
- Now extend your arm through your legs.
- Carry out Step again.
Strengthening Exercises
These are a few of the basic exercises you can perform as part of your rehabilitation regimen until your symptoms go away or you schedule another appointment with your doctor, physical therapist, or sports trainer.
Please keep in mind:
Strong muscles and high endurance are better able to handle stress.
Follow your doctor’s, physical therapist’s, or sports trainer’s initial workout instructions. With each exercise, increase the weight and number of repetitions progressively while following their instructions.
Hamstring Curls
- Lie on your back (Prone Position) and extend your legs straight out.
- Bend your knee 90 degrees. Continue in this posture for 5 to 10 seconds.
- Gradually bring your leg back to its starting position.
- Perform exercise 2 times a day, or 8 to 10 times.
Isometrics Hamstring Exercises
- On the ground or a bed, lie on your back.
- Raise your knee to about 70 degrees.
- As much as you can, press your heel into the ground or the bed.
- Hold for 10 to 15 seconds.
- Perform exercise 2 times a day, or 8 to 10 times.
Eccentric Strengthening Exercises:
It has been shown that eccentric exercises, in which the muscle is lengthened during contraction, are advantageous for tendon rehabilitation. For those with semimembranosus tendinopathy, eccentric strengthening exercises that focus on the hamstring muscles can assist enhance tendon strength, resilience, and function.
Biomechanical Assessment and Correction:
By treating underlying biomechanical problems like muscular imbalances, anomalies in gait, or inappropriate footwear, tendinopathy can be prevented from recurring and the tension on the semimembranosus tendon can be lessened. For the purpose of maximizing foot and ankle alignment during physical activity, orthotics or shoe adjustments may be advised.
Surgical Treatment
If conservative measures fail to alleviate severe or refractory semimembranosus tendinopathy, surgery may be the next step to take. Depending on the degree of tendon injury and functional impairment, surgical procedures for tendon debridement, repair, or reconstruction may be available.
Treatment regimens should be customized for each patient based on their unique needs and objectives, taking into consideration elements including activity level, underlying medical disorders, degree of symptom intensity, and responsiveness to conservative therapy.
Conclusion
Semimembranosus tendinopathy presents challenges to mobility and performance, particularly in active individuals. It is essential to understand its causes and symptoms in order to manage it effectively. Treatment involves a multifaceted approach, including rest, therapy, and possibly interventions like injections or surgery. Further research is needed for improved care and outcomes.
FAQ
How do you treat semimembranosus tendinopathy?
A brief course of nonsteroidal anti-inflammatory medicine, ice, pain-relieving modalities, relative relaxation from uncomfortable activities, and physical therapy exercises, such as hamstring strengthening and stretching, are all part of the first conservative treatment for SMT.
How do you strengthen the semimembranosus tendon?
Place one leg flat along the floor and through the doorway while you lie on the floor with your back to the wall. To feel the stretch, pull as near to the wall as you can. These stretches for your hamstrings are just as beneficial as standing ones. Complete ten repetitions of the exercise on each leg.
What is Tenosynovitis of the semimembranosus?
In those over 50, semimembranosus tenosynovitis is a prevalent knee condition that primarily affects women. Both the bursa beneath the tendon and the reflected section of the semimembranosus muscle are affected.
How do you fix semimembranosus pain?
Nonoperative therapy involves rest, stretching, and physical therapy with an emphasis on strengthening the quadriceps and hamstrings.