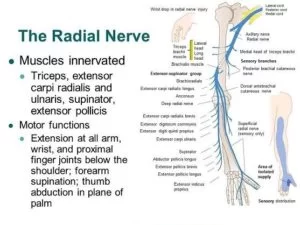
Radial Nerve
Radial Nerve Anatomy
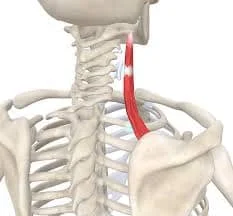
The radial nerve is a peripheral nerve that supplies specific regions of the arm, wrist, hand, and forearm (see Image). posterior nerves of the upper extremities. This nerve functions as a sensory and motor nerve. The extrinsic wrist and hand extensors, posterior forearm muscles, and posterior arm muscles are all triggered by the motor branches.
The sensory branches supply the skin on the anterolateral arm, posterior forearm, distal posterior arm, and posterolateral wrist and hand regions. The radial nerve’s distribution narrows laterally from the thumb to the ring finger. The digit pads of the medial 1-1/2 fingers are supplied by the ulnar nerve, while the digit pads of the lateral 3-1/2 fingers are supplied by the median nerve.
The radial nerve is a component of the posterior cord of the brachial plexus and arises from the ventral rami of the spinal nerves C5 to T1. Disruption of the radial nerve may result in neurologic deficits in its distribution area.
Root value:
It arises from the brachial plexus and is made up of fibers from the ventral roots of the C5, C6, C7, C8, and T1 spinal nerves.
Radial Nerve Structure
The C5 to T1 nerve fibers contribute to the radial nerve, which is the continuation of the posterior cord of the brachial plexus. After leaving the axilla, it passes through the anterior, posterior, and posterior forearm compartments in that order.
Course of the Radial Nerve
Radial nerve in the arm
The radial nerve passes through the triangular interval to enter the posterior arm compartment after leaving the axilla posterior to the brachial artery. The teres major superiorly, the humerus laterally, and the long head of the triceps brachii medially define the triangular interval.
This posterior cord derivative in the arm branches to the long and lateral heads of the triceps muscle after passing between its medial and long heads. Together with the profunda brachii, or deep brachial artery, it travels around the radial groove of the humerus further distally. The radial nerve branches at this level to the medial head of the triceps.
The nerve enters the lateral intermuscular septum at the lateral aspect of the humerus and passes between the brachialis and brachioradialis anteroinferiorly at the cubital fossa. The radial nerve splits into a deep motor-articular branch and a superficial cutaneous-articular branch anterior to the lateral humeral epicondyle.
Radial nerve in the forearm
The superficial branch of the radial nerve descends deeply to the brachioradialis in the forearm. After that, it passes distantly over the anatomic snuff box (see Image. Ulnar Styloid Process and Anatomical Snuff Box). The dorsal aspect of the hand and the lateral 3-1/2 digits are supplied by this nerve in terms of skin and joints.
Concurrently, the supinator is punctured by the deep branch of the radial nerve, which then passes around the lateral aspect of the radius’s neck and enters the posterior forearm compartment. This branch supplies the posterior forearm muscles and is the radial nerve’s distal continuation. The posterior interosseous nerve, which emerges from the deep branch of the radial nerve further distally and ends on the interosseous membrane, travels deep to the extensor pollicis longus.
The posterior cutaneous nerve of the forearm is the third branch that originates from the radial nerve in the forearm. The skin on the back of the forearm and wrist is supplied by this nerve.
Radial nerve in the hand
The cubital fossa is the origin of the radial nerve’s superficial sensory branch, which gives rise to the hand’s lone branches. Extrinsic muscles that originate in the forearm and are innervated by the deep branch of the radial nerve are called hand extensors.
Radial Nerve Functions
The radial nerve performs the following motor and cutaneous sensory functions.
Sensory Function:
Anterior lateral aspect of the mid-arm is the site to the arm’s inferior lateral cutaneous nerve.
Posterior aspect
- Posterior distal arm: posterior cutaneous nerve of the arm
- The forearm’s posterior cutaneous nerve is located as a strip on its back side.
- Superficial branch: dorsal hand region and posterior aspect of the lateral 3-1/2 digits
Motor Function
Radial nerve
- Triceps brachii Muscle: Elbow extension
- Extensor carpi radialis longus Muscle: wrist extension
- Brachioradialis Muscle: elbow flexion and forearm pronation and supination, depending on the forearm’s position
- Anconeus Muscle: elbow extension
Deep branch of the radial nerve
- Extensor carpi radialis brevis: wrist extension, abduction
- Supinator: forearm supination
Posterior interosseous nerve
- Abductor pollicis longus: thumb abduction
- Extensor carpi ulnaris: wrist extension, adduction
- Extensor digiti minimi: 5th digit extension, Wrist Extension
- Extensor digitorum: extension of the medial four finger- digits
- Extensor indicis: index finger extension, wrist extension
- Extensor pollicis brevis: thumb extension, abduction at the carpometacarpal and metacarpophalangeal joints
- Extensor pollicis longus: extension of the thumb’s terminal (DIP Joints) phalanx
Embryology
The neural crest, or the strips of ectodermal cells at the edges of the neural tube in the developing embryo, is the origin of the radial nerve. It is bilaterally paired. Peripheral nerves, such as the radial nerve, are the result of neural crest cell migration to the upper limb area.
Blood Supply and Lymphatics Drainage
At the lower border of the teres major, the brachial artery—the continuation of the axillary artery—and the radial nerve leave the axilla together. The nerve and the deep brachial artery pass through the triangle to enter the posterior arm compartment further distally.
The radial nerve crosses the cubital fossa anteriorly after following the radial collateral artery. At the cubital fossa, the nerve branches superficially, running parallel to the posterior interosseous artery, deep branch of the radial artery, and radial artery.
Radial Nerve Branches
The biggest terminal branch of the brachial plexus and the direct continuation of the posterior cord is the radial nerve. The following branches make up this nerve, which originates from the C5 to T1 nerve roots:
Sensory Nerve
- Inferior lateral cutaneous nerve of the arm
- Posterior cutaneous nerve of the arm
- Posterior cutaneous nerve of the forearm
- Superficial branch of the radial nerve
Motor Nerve
- Deep branch of the radial nerve
- Posterior interosseous nerve
List of Muscles Supplied By Radial Nerve
The following muscles are innervated by the radial nerve and its branches:
- Abductor pollicis longus
- Anconeus
- Brachioradialis
- Extensor carpi radialis brevis
- Extensor carpi radialis longus
- Extensor carpi ulnaris
- Extensor digiti minimi
- Extensor digitorum
- Extensor pollicis brevis
- Extensor indicis
- Extensor pollicis longus
- Triceps brachii (long, medial and lateral heads)
- Supinator Muscle
Anatomical Variantions
The posterior interosseous nerve, which supplies innervation to the posterior forearm muscles, is normally formed by the deep branch of the radial nerve traveling between the heads of the supinators. The deep branch of the radial nerve passes through the Supinator Arch, also known as the arcade of Frohse, which may increase the risk of impingement in some people.
Surgical Importance
Neurologic deficits can arise distal to the site of injury from iatrogenic damage to the radial nerve. Sternal retraction, such as that which occurs during internal mammary artery dissection and cardiac surgery, can cause radial nerve tears at the brachial plexus level. This level of radial nerve damage is at risk due to elbow hyperextension, such as during upper extremity surgery or prolonged supine positions. Slight elbow flexion is necessary in anesthetized patients to prevent elbow-level radial injury. One possible side effect of surgically treating de Quervain tendinopathy is damage to the superficial radial nerve.
Clinical Importance
Neurologic deficits in the radial nerve’s distribution areas can result from a variety of conditions that impact the nerve. Both unusual and typical cases that arise in practice are covered in this section.
Radial Nerve Palsy
Radial nerve palsy/damage from compression, ischemia, arm fractures, penetrating wounds, and surgical complications is the most common cause of radial neuropathies. The degree of the injury determines how severe the symptoms are. Most often, there is a wrist drop, or the inability to extend the hand. “Crutch palsy,” “Saturday night palsy,” and “honeymooner’s palsy” are some additional names for radial nerve palsy, which all refer to protracted compression of the radial nerve close to or at the axillary level.
Radial Nerve Entrapment
Everywhere the radial nerve travels, it is susceptible to damage or compression. Consequently, in the regions that this nerve supplies, pain may appear first, followed by sensory and motor deficiencies. The radial nerve’s posterior interosseous branch passes between the supinator heads in the proximal forearm, which is frequently compressed.
The radial aspect of the wrist and the middle and proximal thirds of the humeral shaft—where humeral fractures occur—are less frequently affected sites. The pathology determines the treatment. For minor injuries, conservative treatment is used; surgery is saved for more serious or unresponsive cases.
Cheiralgia Paresthetica (Wartenberg Syndrome)
A common cause of cheiralgia paresthetica, a hand neuropathy, is trauma or compression of the radial nerve’s superficial branch. Usually, it affects the dorsum of the hand close to the anatomical snuffbox, but it can also affect the dorsal aspect of the hand. Pain, numbness, tingling, or a burning feeling are some of the symptoms. Being purely sensory, there is no motor involvement in the superficial branch. It is believed that wrist compression, from wearing a bracelet or watch band, is the cause. The term “handcuff neuropathy” refers to the condition’s association with the use of handcuffs.
Radial Tunnel Syndrome
The radial tunnel begins at the radiocapitellar joint, also called the lateral elbow, and ends at the proximal border of the supinator. It is 5 centimeters long. The origin of the radial nerve’s forearm branches is not far from this area.
This level of the radial nerve is affected by a rare compression neuropathy called radial tunnel syndrome. The disorder is linked to specific jobs or sports activities and is usually caused by repetitive forearm movements, especially supination and pronation.
Among the symptoms are fatigue and a dull, aching pain at the proximal part of the forearm during use. Less frequently, pain occurs at the dorsal aspect of the wrist or hand. Due to the cutaneous branches of the radial nerve being most frequently affected, extensor and supinator weakness is typically not observed.
There is a connection between posterior interosseus nerve compression syndrome and radial tunnel syndrome. This neuropathy affects the posterior interosseus nerve, which innervates the supinator and the extensors of the wrist and hand. Consequently, the most typical presentation is one of motor deficits.
Radial tunnel syndrome can be treated with both medication and surgery. The main surgical landmark for treating radial tunnel syndrome is the palpable proximal aspect of the radial head. The posterior interosseus nerve leaves the body at the superficial head of the supinator muscle, 7.4 cm distal to this landmark.
Posterior Interosseus Nerve Compression Syndrome
The difference between posterior interosseus nerve compression syndrome and radial tunnel syndrome is the motor deficits to the muscles innervated by the posterior interosseus nerve. The nerve at the Frohse arcade is compressed. Most often, trauma, tumors, and inflammation are the cause of this neuropathy.
Radial Nerve Injury at Radial groove
The radial nerve is vulnerable to injury after a humeral shaft fracture because it is situated in the radial groove of the humerus. This level of damage to the radial nerve can cause wrist drop, a condition where the wrist cannot be extended. A lateral supracondylar fracture can also cause damage to the radial nerve, though it manifests differently from a midhumeral injury.
Nerve branches that innervate the brachioradialis and extensor carpi radialis longus muscles originates just above this fracture, largely sparing these muscles. The patient’s wrist does not exhibit a wrist drop when asked to extend their hand; instead, it extends radially but weakly.
FAQ
Which muscles does radial nerve innervate?
The triceps brachii, which acts to extend the arm at the elbow, is innervated by it in the arm. The brachioradialis and extensor carpi radialis longus (the posterior forearm muscles) are supplied by branches of the radial nerve.
What are the landmarks of the radial nerve?
The radial nerve can be found using two anatomic landmarks: the point of confluence and the triceps aponeurosis.
Which areas of the radial nerve are frequently injured?
Anywhere along the nerve’s distribution can experience compression or entrapment, but the proximal forearm is where it happens most frequently. An uncommon diagnosis that is often underdiagnosed is radial nerve entrapment.
What is the function of the radial nerve?
A peripheral nerve that supplies particular areas of the arm, wrist, hand, and forearm is the radial nerve. Upper Extremity Posterior Nerves). This nerve serves as a motor and sensory nerve. The motor branches innervate the extrinsic wrist and hand extensors, posterior forearm muscles, and posterior arm muscles.
What does the radial nerve control?
It facilitates hand, wrist, and arm movement. The radial nerve supplies movement to the triceps muscle located at the back of the upper arm as it travels down the arm. Additionally, it extends the wrist and facilitates hand and wrist movement and sensation.

3 Comments