Popliteal Tendinitis
Popliteal tendinitis is an overuse injury that causes inflammation and pain in the popliteus tendon located at the back of the knee. It commonly occurs in runners or individuals with knee instability, leading to discomfort during downhill walking, running, or bending the knee.
Tendon. The popliteus tendon is the tendon that connects the popliteus muscle to the outside of the knee from the rear of the thigh bone. This structure is crucial for turning the leg bone and slowing the knee as it straightens. It is crucial for running or walking on banked terrain or downhill.
This is often a tendon strain of grade 1 or 2. A grade 1 strain is considered moderate. There is a small strain but no visible tears (it is tiny tendon tearing). The tendon is the proper length, and there is no loss of strength.
A moderate strain is classified as grade 2. Fibers within the tendon’s substance or at the tendon’s junction with a muscle or bone are damaged. Strength often decreases as the muscle-tendon-bone unit lengthens. A grade 3 strain, which is uncommon and typically associated with serious knee injuries, is a total rupture of the tendon.
Signs and Symptoms
- Pain and tenderness over the popliteus tendon at the outer knee joint or back of the knee on the outer side.
- pain that becomes worse when standing on the leg with the knee slightly bent or when walking or running, just as the foot of the affected leg lifts off the ground.
- pain that gets worse when rotating the leg; pain that begins or returns after running a specific distance.
- Crepitus, or a crackling sound, occurs when the tendon is moved or touched (rare, unless tested right after exercising).
Causes
- Overuse of the popliteus muscle-tendon unit is typically seen in athletes who train or run on banked or uneven surfaces.
- Acute trauma
- Poor physical activity
Anatomy
On the posterolateral corner of the knee, there is a little muscle called the popliteus.
Origin
The fibular head, the lateral meniscus, and the lateral femoral condyle are its three main sources. The popliteus muscle’s proximal insertion is located proximal to the linea muscli solei on the proximal side of the tibia.
Insertion
In 82.5% of cases, there is no implantation on the lateral meniscus. The tendon attaches itself to the lateral femoral condyle after passing through the popliteal gap in the coronary ligament and running deep into the collateral ligament. Although the tendon is extra-articular and extra-synovial, it is intracapsular.
Function
The internal rotation, or endo-rotation, of the lower leg, which occurs when walking, is the main function of the popliteus muscle. Its primary function is to stabilize the knee’s forward motion as well as the retraction of the knee joint‘s backside and the lateral meniscus during knee flexion. When the knee is fully extended, it allows flexion. The popliteus muscle is frequently thought of as the key to unlocking the knee because of its unlocking role.
Epidemiology
Overuse of the popliteus muscle-tendon unit may result in popliteus tendinopathy. Athletes who run or exercise on incline or banked surfaces are typically affected. Two common causes are sudden forced knee hyperextension with the tibia internally rotated, or a direct varus force with the tibia externally rotated. Because it results in an external rotation of the tibia, it could potentially be associated with hyperpronation of the foot.
Differential Diagnosis
After a thorough review of the case history and an extensive physical examination, the diagnosis should be made in large part. Patients typically experience pain with resisted outward rotation and pain along the proximal popliteus tendon.
An intra-articular pathology, such as a meniscus posterior horn rupture, should always be included in the differential diagnosis of reported posterior knee pain.
Other conditions that might have symptoms similar to those of popliteus tendinopathy include:
- Degeneration and re-calcification of articular cartilage and underlying bone are characteristic features of osteochondritis dissecans, an intra-articular osteochondrosis with an unclear origin.
- Iliotibial band syndrome is a disorder caused by overuse.
- The lateral side of the knee joint is palpably painful.
- Activity increases the pain that occurs.
Diagnostic procedures
- It’s critical to identify and accurately diagnose popliteus tendinopathy. Popliteus tendinopathy can restrict sports performance and cause severe pain. Unnecessary surgery may result from a misdiagnosis. Popliteus tendinopathy is a rare disease at the back of the knee that is frequently misdiagnosed.
- A physical examination and the case history should be the basis for a diagnosis of popliteus tendinopathy.
- Tendinopathy can be diagnosed by an MRI or other imaging. We detected an extraordinary amount of fluid associated with the popliteus sheath in a case study, although the tendon appeared to be healthy and free of soft tissue damage.
Medical Treatment
- It is often recommended to take non-steroidal anti-inflammatory drugs like aspirin and ibuprofen (avoid taking them within seven days before surgery) or other mild analgesics like acetaminophen. Take these as prescribed by your doctor. If you have any bleeding, upset stomach, or symptoms of an allergic reaction, get in touch with your doctor right away.
- Your doctor may prescribe painkillers if needed. Cortisone injections relieve inflammation; use only as prescribed. However, because cortisone damages muscle and tendon tissue, it can only be used in extreme circumstances. Pain is momentarily relieved by anesthetics.
Physiotherapy Treatment
Until you visit your doctor, physical therapist, or sports trainer again, you may begin your rehabilitation program with some of these activities. or until your symptoms go away.
- Rest: To reduce inflammation, stay away from physically demanding tasks and use ice.
Rest keeps the initial injury from getting worse. We may reduce the size of the connective tissue scar and stop further retraction of the ruptured muscle stump by allowing the injured extremity to rest for the first three to seven days following the traumatic injury.
A brief period of immobilization during the first few days following the injury speeds up the formation of granulation tissue at the site of injury. However, it should be noted that the duration of reduced activity mobilization could only be limited until the scar reaches sufficient strength to bear the pulling forces caused by muscle contraction without rupturing again. At this point, gradual mobilization should be started and followed by a progressively intensified exercise program to maximize healing by restoring the strength of the injured muscle and preventing muscle atrophy, loss of strength, and extensibility, all of which can follow prolonged immobilization.
- Cold: It is believed to reduce blood flow to the injured region and lower intramuscular temperature. It has been demonstrated that applying cold to damaged skeletal muscle early on results in a much smaller hematoma between the ruptured myofiber stumps, less tissue necrosis and inflammation, and faster early regeneration. However, the most current research on the subject indicates that chilling the damaged skeletal muscle should be done for a long duration (6 hours) with the goal of significantly reducing bleeding and tissue necrosis at the site of the injury.
- Compression:When combined with elevation, this may assist in reducing blood flow at the site of injury and reducing the buildup of extra interstitial fluid. The objective is to reduce tissue ischemia by preventing hematomas and interstitial edema. On the other hand, prolonged immobilization will have a negative impact on muscle regeneration. Compression and cryotherapy should be administered for 15 to 20 minutes at a time, separated by 20 to 50 minutes. The quadriceps should be maintained largely still during this time to promote proper healing and stop further damage to the area.
- Elevation: When an injured extremity is raised above the level of the heart, hydrostatic pressure decreases, which in turn reduces the buildup of interstitial fluid and minimizes swelling at the site of injury.
Ultrasound is a therapeutic technique that produces deep heat, micro-massages soft tissue, increases localized blood flow to the region, improves flexibility, and encourages tissue recovery. and eventually easing suffering.
Short wave diathermy (SWD)
Short-wave diathermy is a deep heating technique that uses heat to relieve pain, improve blood flow to the affected area, and remove waste.
TENS (transcutaneous electrical nerve stimulation)
An electrical technique called trans cutaneous electrical nerve stimulation reduces pain by modulating it. Additionally activates the body’s own opioid system, which stops the anterior grey horn from releasing chemicals.
Stretching
Hamstring stretching
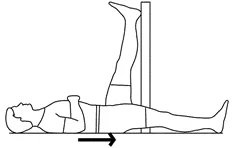
- With one leg straight, lie on your back.
- Lift the opposing leg, keeping it slightly straight, and press it up against the wall.
- Hold for thirty seconds.
- Repeat after switching legs.
- Perform this exercise on each leg three times.
Wall-Calf Popliteus Stretch
- Positioning: Use your hands for balance as you face a wall.
- Step Back and Stretch: return one foot while maintaining a straight back leg and a downward heel.
- Hold and Release: For thirty seconds, slightly bend your front knee.
- This popliteus stretch helps in knee joint lengthening and tension release.
Floor Seated Stretch
- Starting Position: Extend both legs in front of you while sitting on the floor.
- Press by crossing one ankle over the knee on the other side. Apply little pressure on the crossed knee.
- Hold and Repeat: After 20 seconds of holding, alternate legs.
- By focusing on the popliteus muscle, this stretch helps release tension while improving knee stability.
Exercise
Wall squat

- Place your feet a few steps away from a wall while keeping your shoulders and back against it.
- To squat, bend your knees so that your back slides down the wall. Your knees should be positioned over your ankles and bent at a 90-degree angle. Keep applying pressure to the wall, your shoulders, and your back.
- As you maintain this position, concentrate on tightening your thigh muscles.
- Next, slide back up the wall to your starting position by pushing through your feet.
- You may feel your hip and thigh muscles working as you complete each repetition.
Hamstring isometric exercises
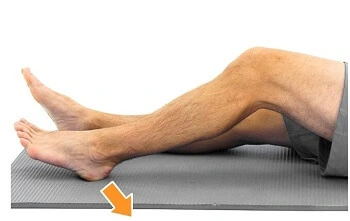
- On a level surface, lie on your back.
- Bend both your left and right knees by around 40 to 50 degrees.
- Pull your heel toward your buttocks by pressing it into the surface.
- To “dig” as hard as you can without causing further pain, tighten the muscles at the back of your thighs.
- Maintain this posture for ten seconds.
- Between each exercise, release the tension gently and let your muscles five to eight seconds to totally relax.
Hamstring Curls
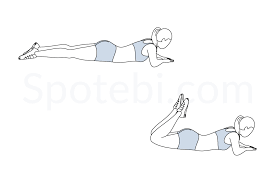
- Spread your legs wide while lying on your stomach.
- Make a 90-degree bend in your knee. For ten seconds, maintain this posture.
- Return your leg to the beginning position slowly.
- Perform the workout 15 times, twice a day.
FAQs
Can you walk with popliteus tendinitis?
The patient’s symptoms may worsen, and scar tissue may develop if he keeps loading his knee, which might make physical activity even more painful. Walking, running, and climbing stairs are examples of physical activity that may be difficult, particularly soon after an injury.
What does popliteal tendonitis feel like?
Typical signs and symptoms include: Back of the Knee Pain: Usually felt on the outside of the knee, this pain can get greater with activity, especially while descending stairs or walking downhill.
How do you test for popliteal tendonitis?
The patient is seated with their knee and hip flexed at a 90-degree angle. The examiner opposes the patient’s aggressive outward rotation of the lower leg. If the popliteus muscle or tendon hurts during the motion, the test is considered positive.
How long does popliteus tendinitis take to heal?
Although many cases improve in 10 to 14 days, it is often curable within 6 weeks if conservative therapy is used and the affected region is rested.
References
- Nicholas JA & Hershman EB. (1995). Popliteus tendinitis. https://brattonmd.com/wp-content/uploads/POPLITEUS-TENDINTIS.pdf
- Popliteus_Tendinopathy, https://www.physio-pedia.com/Popliteus_Tendinopathy