Hip Pain
What is a Hip Pain?
Hip pain refers to any pain or discomfort in the hip area, typically originating either from the hip joint itself or from surrounding muscles, connective tissues, or structures. It’s a common complaint that can interfere with daily activities like walking, standing up from a seated position, or climbing stairs.
The hip is a ball-and-socket joint made up of the femoral head at the top of the thigh bone (femur) that fits into the cup-shaped acetabulum of the pelvis. There is a great range of motion possible with this structure. However, it also means the joint is prone to wear and tear as well as injuries from repetitive movements or trauma.
There are several potential causes for hip pain including osteoarthritis, rheumatoid arthritis, injuries like strains/sprains or fractures, tendinitis, bursitis, labral tears, and avascular necrosis. In some cases, pain can be referred from issues in the lower back as well. In the elderly, even thinning of hip joint cartilage and bone mass can play a role.
Common symptoms include pain in the groin, outer hip, or thighs, stiffness, reduced mobility, limping, and problems moving from sitting to standing. There may also be grinding, clicking, or other audible joint sounds. Diagnosis often starts with a physical exam and then X-rays, MRI, or other imaging tests as needed.
Treatment focuses on relieving pain, recovering mobility, preventing future injuries, and improving related issues like misaligned posture or muscle weakness. Options range from rest, ice/heat, OTC pain medications, physical therapy, braces/supports, injections, and ultimately surgery if conservative treatments fail.
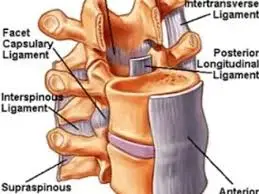
Clinically Relevant Anatomy
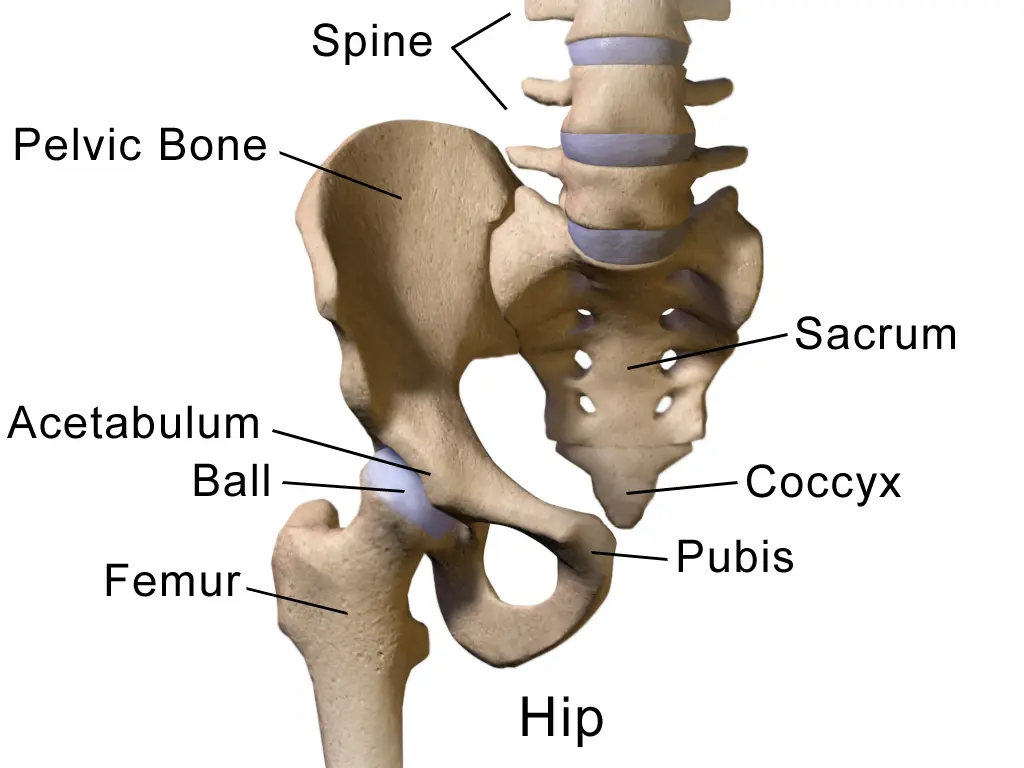
A. Acetabulum
- Part of the pelvis is formed by the ilium, pubis, and ischium bones
- Acts as a socket for the femoral head
B. Femoral Head
- Round bone at the proximal end of the femur
- Articulates with the acetabulum
- Covered in articular cartilage
C. Articular Cartilage
- Covers joint surfaces of femoral head and acetabulum
- Provides a smooth surface for movement and load distribution
- Damage to cartilage leads to osteoarthritis
Muscles and Supporting Structures
A. Gluteal Group Muscles
- Muscles that insert at the greater trochanter of the femur
- Includes gluteus maximus, gluteus medius, gluteus minimus
- Helps move and stabilize hip joint
B. Iliopsoas Muscles
- Includes iliacus and psoas major muscles
- Primary flexors of the hip joint
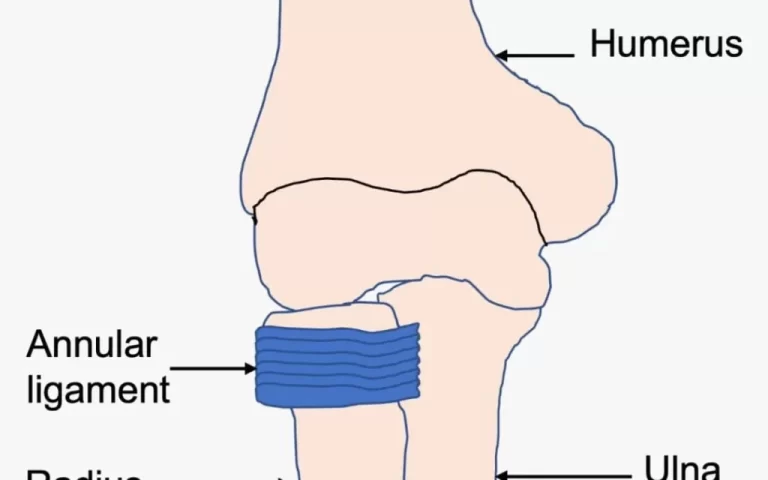
C. Bursae
- Fluid-filled sacs that decrease friction around the joint
- When inflamed, may cause troublesome bursitis
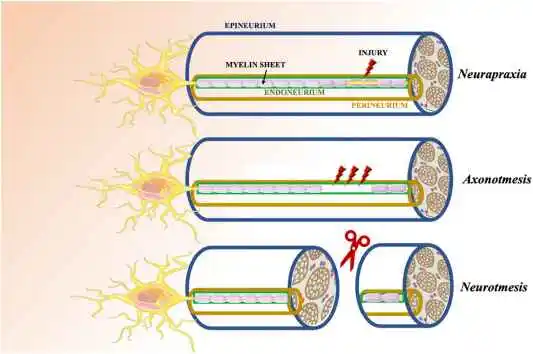
Nerves and Vascular Supply
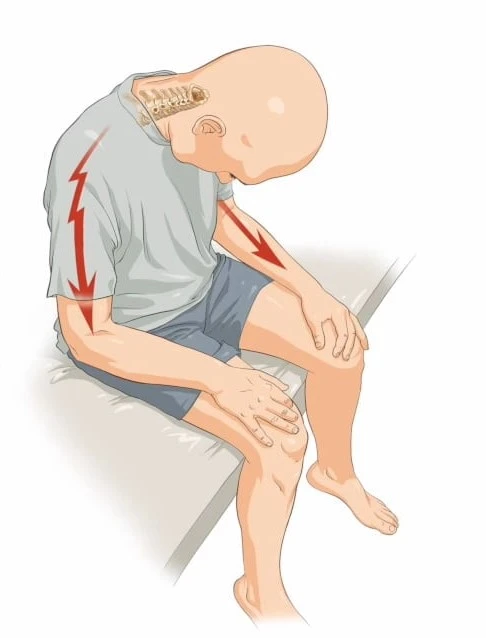
A. Sciatic Nerve
- Passes through the area can be impinged
- Compression causes radiating leg pain
B. Femoral Artery and Vein
- Pass behind the inguinal ligament near the joint
- Risk of vascular injury in hip fracture/dislocations
Causes of Hip Pain
Osteoarthritis
- Most common cause of chronic hip pain
- Wear-and-tear arthritis leads to the breakdown of protective cartilage
- Cartilage damage exposes bone, causes pain, stiffness, swelling
- Most often affects middle-aged and older adults
- Worsens over time without proper management
- Autoimmune disease causing chronic inflammation
- Can inflame the joint lining (synovial membrane)
- Leads to warmth, swelling, and tenderness in joints
- Systemic symptoms like fever and fatigue are common too
- Younger patients often affected
- Progressive destruction of bone and cartilage
Labral Tears
- The hip socket’s ring of cartilage is called the acetabular labrum.
- Tears often caused by acute trauma/twisting
- Can also result from FAI (femoroacetabular impingement)
- Often affects young, active individuals
- Causes sharp groin pain, catching sensation
- Limits mobility, and affects the quality of life if not treated
Tendinitis
- Inflammation of hip flexor tendons or gluteal tendons
- Often caused by overuse with running, climbing stairs
- Associated with other hip problems like impingement
- Leads to pain with straightening leg or weight-bearing
Iliotibial Band Syndrome
- IT band rubs against the bony area on the lateral hip
- Caused by overuse, tight IT band putting pressure
- Runners/cyclists often affected
- Causes sharp, stabbing pain on the outer hip/thigh
- Often relieved by rest and flexibility training
Bursitis
- Inflammation of small fluid-filled bursal sacs around the hip joint
- Usually caused by repetitive hip movements or prolonged pressure
- E.g. trochanteric, iliopsoas, or ischial bursitis
- Leads to severe, achy pain around hip/thigh depending on site
- Pain usually worse at night or with activity like walking, lying on the side
Snapping Hip Syndrome
- Audible, painful snapping of an irritated tendon
- Usually iliopsoas tendon slides over the hip (or vice versa)
- Sounds and feels like a ‘popping hip joint’
- Often caused by muscle imbalances/overuse in active persons
- Can lead to bursitis or tendinitis if not managed
Hamstring/Glute Strains
- Acute muscle tears or chronic tendon issues
- Can involve hamstrings attaching around the hip joint
- Also gluteal muscles like gluteus medius
- Happens with explosive movements like sprinting
- Causes pain with muscle contraction or stretch
Pelvic Stress Fractures
- Stress injuries of the sacrum, pubis, and ilium from overuse
- Common in runners or athletes with a sudden increase in training
- Cause aching, diffuse pain over sacrum/pelvic area
- Rest, and activity modification essential for healing
Avascular Necrosis
- Interrupted blood supply causes the death of bone tissue
- Mostly affects the femoral head leading to hip joint collapse
- Can be caused by trauma or medication side effects
- Leads to sudden, progressive hip pain
- Requires early surgery to preserve joint
Hernias
- Weakness in the muscle wall allows tissue bulging
- Can occur in the lower abdomen near the groin region
- Causes muscle pain that worsens with straining/heavy lifting
- Risk of incarceration if untreated
Other causes
Sciatica:
- Compression or irritation of the sciatic nerve or its roots in lower back and hips
- Causes sharp, radiating pain from lower back/buttocks into legs
- Can result from lumbar disc herniations or spinal stenosis
- Aggravated by sitting, bending, coughing
Piriformis Syndrome:
- Irritation/compression of the sciatic nerve by the tight piriformis muscle
- Muscle spasms cause compression of the nerve
- Sciatic pain, tingling down legs
- Often triggered by exercise, prolonged sitting
Hip Flexor Strains:
- Strains or tears of iliopsoas/rectus femoris muscles
- Pain in the front of the hip that may radiate down the thigh
- Caused by explosive motions like kicking/sprinting
- Associated swelling, stiffness, bruising
Trochanteric Bursitis:
- Bursa inflammation close to the greater trochanter
- Characteristic lateral hip pain, aggravated at night
- Caused by sports overuse, trauma, arthritis, tendinitis
Bone Tumors:
- Benign or cancerous tumors arising from hip bone
- Cause persistent, progressive hip pain, worse at night
- Require imaging tests for diagnosis
Legg-Calve-Perthes Disease:
- Children’s avascular necrosis of the femoral head
- Caused by disruption of femoral head blood supply
- Leads to limping, hip/groin pain
- Requires support therapy until remolding occurs
Symptoms of Hip Pain
Location of Pain:
- Hip pain can present as pain in the groin, thigh, or outer buttock region depending on the underlying cause
- Pain from the hip joint itself is typically felt in the inner thigh and groin
- Can radiate down front or back of thigh depending on irritated innervation
The character of Hip Pain:
- Often described as an ache or deep pain within the hip
- Can also feel stabbing, sharp pains, indicating irritated nerve roots/sciatica
- Stiffness and reduced mobility are common complaints
Referred Pain Patterns:
- Hip disorders can cause pain felt in the knee or lower back region
- Likewise diseases of the lumbar spine can be felt as hip pain
Impact on Daily Function:
- Difficulty walking, climbing stairs, or transitioning positions
- Pain while straightening hip or bringing knee toward chest
- Limping, altered gait or balance disturbances
- Difficulty standing or sitting for prolonged periods
- Night pain disrupting sleep
Associated Manifestations:
- Joint stiffness, reduced range of motion
- Catching, locking sensation
- Clicking, crunching, grinding hip joint noises
- Joint instability, the feeling of giving way
- Joint line tenderness, swelling, and warmth in some forms of arthritis
- Muscle spasms or atrophy depending on chronicity
- Sites of swelling or masses around joint concerning tumors
Diagnosis
History and Physical Exam
- Thorough health history looking at onset, location, nature of pain
- Identify aggravating and relieving factors
- Changes to gait or activity levels
- Medical history and prior injuries
- Physical exam assessing range of motion, strength, gait
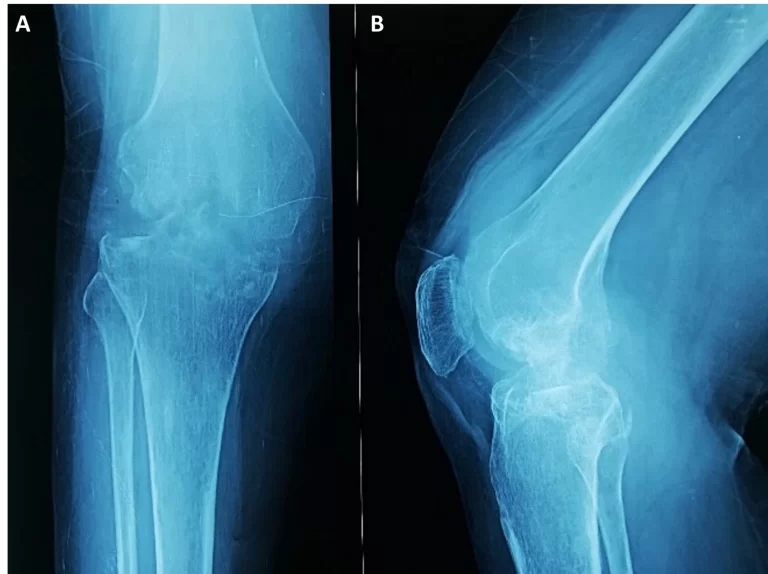
Imaging Studies
X-rays:
- First-line modality, great for visualizing bony structures
- Anteroposterior view visualizes joint spaces and detects narrowing suggesting arthritis
- Lateral view provides additional visualization for subtle fractures
- Frog-leg lateral useful for round femoral head morphology
MRI:
- Provides detailed visualization of soft tissues including cartilage, labrum, ligaments
- Helps identify early arthritis and injuries not seen on x-ray
- Allows assessment of avascular necrosis before bony changes
- Evaluate extra-articular causes like muscle tears, tendinopathy
CT Scans:
- Better detail of subtle bone fractures compared to X-rays
- Useful for trauma, stress injuries
- Assesses femoral/acetabular anatomy in complex cases of impingement
- Associated radiation exposure makes MRI preferred for soft tissue
Bone Scan:
- Nuclear imaging identifying areas of increased bone turnover
- Helps detect stress fractures, infections, and bone tumors early
- Follow-up scans assess treatment response
Ultrasound:
- Inexpensive way to assess extra-articular issues
- Can guide therapeutic injections and aspirations
- Limited utility for intra-articular joint assessment
- User-dependent results
Arthrogram:
- Involves injection of contrast dye before taking advanced images
- Outlines labral tears, and cartilage defects not seen on MRI
- Not commonly used now with advanced MRI protocols
Physical Therapy Special Tests
FABER (Patrick’s) test:
- Tests hip abduction and internal rotation.
- Patient lies supine, flexes, and rotates the hip in the figure 4 position.
- Pain on the same side suggests sacroiliac dysfunction or hip joint/capsule pathology.
Log Roll Test:
- Tests hip joint capsule and extracapsular structures.
- Examiner passively rotates flexed hip in and out while stabilizing pelvis.
- Pain indicates pathology like synovitis, fracture, and snapping tendons.
Trendelenburg Sign:
- Tests function of gluteus medius muscle.
- Patient stands on one leg – hip drop on opposite side is positive.
- Indicates possible muscle tears, nerve issues, and arthritis problems.
Flexion, Abduction, and External Rotation (FADER) Test:
- Detects intra-articular hip problems.
- In supine, the hip passively flexed to 90 degrees and rotated.
- Pain suggests anterior hip impingement and labral tears.
Ober Test:
- Assess tightness of the iliotibial band contributing to greater trochanteric pain syndrome.
- Patient lies on the unaffected side as the affected leg is passively abducted, extended, and released.
- Decreased adduction indicates a tight band.
Thomas Test:
- Assesses hip flexor tightness
- Patient lies supine, one leg flexed to chest, other leg lowered to the table
- If the thigh rises off the table, indicates tight rectus femoris/iliopsoas
Ely’s Test:
- Tests for rectus femoris or iliopsoas tendonitis
- Patient lies prone, examiner passively extends knee and flexes hip
- Pain suggests tendinopathy
Scour Test:
- Evaluate iliopsoas tendon disorders
- Resisted hip flexion in supine with the knee extended elicits pain
Hip Scour Test:
- Detection of labral tear
- Patient extends and adducts hip while supine
- Pain indicative of acetabular labral pathology
Dial Test:
- Assesses hip capsule laxity about lumbar spine/SI dysfunction
- Prone lying with hips alternately extended and externally rotated
- Asymmetry indicates hypomobility
Straight Leg Raise Test:
- Detects lumbar spine involvement
- Positive if back/extremity symptoms reproduced on passive SLR
Medical Treatment
Analgesics:
- Acetaminophen, NSAIDs (ibuprofen, naproxen)
- Reduce inflammation and provide pain relief
- Topical NSAID creams/gels can directly target hip joint
Corticosteroid Injections:
- Potent anti-inflammatories directly injected into a hip joint or bursa
- Offer symptomatic relief in osteoarthritis, bursitis, tendinitis
- Can provide pain relief for months allowing a return to activity
Visco-supplementation:
- Injections to restore viscosity and cushioning effect of synovial fluid
- Used in early knee osteoarthritis to potentially delay joint replacement
Nerve pain modulation:
- Local anesthetic/steroid epidural injections for referred spinal pain
- Gabapentin/pregabalin for chronic neuropathic symptoms
Disease-modifying agents:
- Medications that slow the progression of autoimmune arthritis
- E.g. Methotrexate, biologics (TNF inhibitors)
- Goal is inducing disease remission to prevent joint damage
Nutraceuticals:
- Supplements like glucosamine, chondroitin, turmeric
- Anti-inflammatory effects, chondroprotection debatable
- Often used by patients alongside conventional treatment
Surgical Treatment
Hip Arthroscopy
- Minimally invasive surgery performed through very small incisions
- Involves inserting a camera into the hip joint to visualize tissues
- Common indications:
- Repair torn labrum
- Remove loose bodies
- Treat femoroacetabular impingement
- Advantages:
- Shorter recovery time
- Less pain
- Lower infection risk
- Disadvantages
- Technically difficult procedure requiring expertise
- Risks include nerve damage, bleeding, stiffness
Open/Arthroscopic FAI Surgery
- Reshapes abnormal bone growths and bumps in the hip joint
- Fixes impingement between the femoral neck and acetabular rim
- Two approaches:
- Open dislocation of joint for full access
- Arthroscopic through small incisions
- Improves hip mobility and delays arthritis
- Allow return to normal activity levels after surgery/rehab
Total Hip Replacement
- Most reliable surgery for end-stage hip arthritis
- Diseased femoral head and acetabulum replaced with prosthetics
- Dramatically improves function by relieving pain
- About 95% success rate at 10-15 years
- Significant risks include infection, dislocation, blood clots
- Crucial procedure for restoring quality of life in eligible patients
Partial Hip Replacement
- Only one side of the hip joint is replaced
- Two types:
- Hemiarthroplasty – Just replacing the femoral head
- Unipolar arthroplasty – Acetabulum resurfaced with a metal component
- Indications:
- Younger patients not eligible for total hip replacement
- Isolated damage to the femoral head or acetabulum
- Advantages:
- Bone preserving surgery
- Easier revisions later if required
- Shorter recovery period
- Disadvantages:
- Durability less than total hip replacement
- Still significant procedure with risks
Hip Osteotomy
- Surgically repositioning and reorienting hip bone
- The goal is to redistribute weight and load forces better
- Delay the need for total hip replacement
- Two main approaches:
- Periacetabular (around socket)
- Intertrochanteric (femoral shaft)
- Indications:
- Hip dysplasia, impingement syndromes
- Early hip arthritis in active young adults
Core Decompression
- Removes necrotic bone and tissue in the femoral head
- Reduces intraosseous pressure to improve blood flow
- Encourages new bone regeneration
- Preserves femoral head and delays hip replacement
- Indications:
- Early-stage avascular necrosis
- Before the collapse of the femoral surface
Physical Therapy for Hip Pain
Modalities
Heat Modalities
- Heating pads – Use an electric heating pad for 15-20 minutes to relax tight hip muscles and increase blood flow. Helps loosen stiffness before activity.
- Hot packs – Heat packs and moist hot towels applied for 10-15 minutes can reduce pain signals and soothe irritated hip tissue if used before exercise.
- Hydrotherapy pools – Walking or exercising in warm water takes pressure off the hips allowing for gentle movement. Can boost circulation and relax muscles.
- Warm paraffin wax – A brief immersion of the hip area in warm paraffin wax and then wrapped in plastic can provide moist heat benefits for up to 30 minutes at a time before reapplication.
Apply heat modalities for 15-30 minutes before exercise or activity for best effects. Use caution to prevent burns and avoid direct application over sites of inflammation.
Cold Modalities
- Ice packs – Applying ice packs wrapped in a thin towel for 10-15 minutes decreases swelling/inflammation in overworked hip joints or soft tissues.
- Cold gel packs – Specialized cold packs worn around the hip provide sustained cooling benefits to manage pain and swelling after activity or later in arthritis flare-ups. Keep tissue protected underneath the pack strap.
- Cryotherapy chambers – Brief 2-3 minute exposures of hips to intense cold in specialized chambers accelerate recovery by temporarily numbing tissues and constricting blood vessels.
Use ice-based modalities for 10-15 minutes following activity or injury for ideal effectiveness and always insulate cold packs to prevent frost nip on exposed skin. Can repeat every few hours as needed.
Electrical Stimulation
Electrical stimulation introduces electrical impulses to stimulate peripheral nerves innervating the hip and leg. This serves several purposes for hip pain management:
- Pain Reduction – TENS units transmit low-voltage electrical currents which block the transmission of pain signals through the nervous system. Electrodes can target hip muscles and related dermatomes.
- Muscle Strengthening – Neuromuscular Electrical Stimulation (NMES) can activate muscle contractions. This is used to either spasm tight musculature or strengthen weak/atrophied musculature as part of rehabilitation.
- Swelling/Edema Reduction – Electrical stimulation causes muscle pumps to contract and promote circulation and lymphatic drainage, removing inflammatory waste products, hence reducing swelling around the hip joint.
The parameters of electrical stimulation units are adjusted based on the treatment goals, including adjusting the intensity, duration, frequency, and type of contraction.
Traction
Traction applies a longitudinal or perpendicular pull force to the hip joint to help separate the joint surfaces and relieve compression. This helps to:
Decrease pain and muscle spasms
- Increase space within the joint to improve circulation of synovial fluid for nutrition
- Stretch stiff soft tissue structures like the joint capsule
- Relax muscles surrounding the hip
There are a few different types of traction that can be utilized:
- Manual Traction – The physical therapist applies a mobilization/traction force by holding the patient’s leg and moving the hip joint within its available range. This allows the therapist to control and modify the traction force as needed.
- Mechanical Traction – A special traction machine is used where the amount of traction force can be standardized, ranging from 10-20% of the patient’s total body weight. The duration and frequency are progressed as tolerated.
- Pelvic Traction – A belt is placed around the ASIS of the pelvis which delivers a perpendicular distraction force, providing decompression to the hip joint. This technique avoids placing direct traction on the leg.
Ultrasound
- Uses high-frequency soundwaves to generate deep heat within hip joint tissues and musculature up to 5cm deep
- Often applied to areas of tendinopathy or muscle tightness around the hip joint for 5-10 minutes
- Increases blood flow, reduces stiffness/spasm, speeds up healing of strained tissues
- Transducer glides smoothly over ultrasound gel across the affected area with light circular motions
- Can be used before activity to relax muscles or after to facilitate healing
- Should not be used over areas of active inflammation or infection
Iontophoresis
- Uses electrical current to transdermally deliver anti-inflammatory corticosteroid medications into hip tissues
- Patient holds soaked pads over the greater trochanter bursa or another area of irritation
- Low voltage current drives negatively charged dexamethasone ions into the skin over 20 min
- Reduces inflammation associated with common hip issues like bursitis
- Can be repeated up to 3 times per week as needed to reduce localized swelling and discomfort
Stretching Exercises
Hip Flexor Stretch

- Stand upright next to a table or chair for support. Use the hand on the same side as the leg you’re stretching for balance.
- Place the foot of the leg you’re stretching out in front on the floor. Your knee and hip should be bent at a 90-degree angle.
- While maintaining a straight back, gradually push your hips forward until the side of your leg that is forward causing your front hip and thigh to expand. Do not arch your lower back.
- Hold this stretch position for 30 seconds. Breathe slowly and deeply. You should feel the stretch in the front of your upper thigh and the hip crease area of the back leg.
- Repeat this hip flexor stretch 2-3 times on both legs. Feel free to pause and rest between each hold for 30 seconds.
- To increase the stretch intensity, carefully lunge the hips forward more until a deeper, but still pain-free, stretch is felt on your extended thigh and hip. Do not overstretch the muscle.
Proper form is important on this stretch. Avoid excessive arching of your lower back and make sure your hip and knee are at 90-degree angles to isolate the hip flexors without placing strain elsewhere. Holding for 30 seconds maximizes the lengthening benefits before repeating.
Butterfly Stretch

- Sit upright on the floor with your legs bent out to the sides and the soles of your feet touching each other.
- Grasp on both feet together with your hands, keeping your back straight.
- Slowly lower your upper body, while keeping the back straight as much as possible. Feel the inner thighs and hips getting stretched.
- Hold for 30 seconds then use the elbows to press the thighs down towards the floor to intensify the stretch if possible.
- Slowly return to the starting position. Repeat 2-3 times.
Pigeon Pose Yoga Stretch
- Start on all fours. Bring your right knee forward towards your right wrist while sliding your right ankle towards the left wrist.
- Carefully lower both hips towards the floor as you slide the right foot away from your chest. Focus on sinking evenly on both hips.
- Hold for 30 seconds then lower your upper body closer to your bent right leg, keeping the hips squared open. Hold for another 30 seconds.
- Push back to all fours and repeat on the other leg, bringing the left knee forward and left ankle back.
- Perform 2-3 repetitions holding for 30 seconds on each side. Breathe deeply throughout the pose.
Figure Four Stretch
- Lie on your back with both legs extended. Bend your right knee and cross your right ankle over your left thigh into a “4” shape.
- Reach both arms around your left thigh and slowly pull it towards your chest until you feel a comfortable stretch in your right hip and glute.
- Hold this position for 30 seconds, keeping your back pressed to the floor. Breathe deeply.
- Release and repeat the stretch on the opposite side, crossing your left ankle over your right thigh.
- Perform 2-3 repetitions on each side. Pull the thigh closer to increase stretch intensity.
Yoga Squat

- Place your feet somewhat wider than the width of your hips apart.
- Turn your toes and knees outward at 45-degree angles.
- Bend your knees deeply as if sitting back in a chair. Try to get your both thighs parallel to the ground.
- In a pose of prayer, bring your palms together at your chest.
- Lean slightly forward at the hip while keeping your back straight.
- Hold this low squat for 30-60 seconds, feeling a deep stretch in your inner thighs and hip crease. Breathe slowly.
- Carefully return to standing by pushing through your heels. Repeat 2-3 times.
Strengthening Exercises
Lateral Squats
- Stand with your feet shoulder-width apart and your toes facing forward, hands on your hips. Keep good posture.
- Take a big step sideways with your right leg, bending your right knee and hip while keeping your left leg straight.
- Push your hips back as if sitting in a chair, while leaning your upper body slightly over the bent right leg.
- Feel a stretch down the outside of the left hip, thigh, and inner calf. Keep the right knee behind the toes.
- Hold the stretch for 20-30 seconds, then slowly return to standing. Keep the hips and shoulders facing forward the entire time.
- Repeat the stretch with the left leg stepping sideways and bending while stretching the right hip and thigh.
- Perform 2-3 repetitions per side, holding for 20-30 seconds in the stretched position.
- For a deeper stretch, lower the hips closer to the ground. To decrease, don’t sit back as far while in the lateral squat position.
Side-lying leg raise
- Assume a side-laying position and place one leg on top of the other.
- Support your head with your bottom arm.
- Keeping the top leg straight, slowly raise it upwards leading with your heel. Go only as high as you can while keeping the leg straight.
- Raise the top leg as high as comfortably possible without bending your knee or rotating your hips.
- Hold this end position for 20-30 seconds, feeling a stretch down the outer thigh and outer hip area of the top leg.
- Keep your hips stacked and steady. To increase the stretch, carefully raise the top leg higher. But do not strain.
- Slowly lower the top leg back to the starting position, keeping control. Repeat 2-3 times per side.
- Turn over and perform the same side lying leg raises with the opposite leg, stretching the other side.
Fire hydrant
- Assume a tabletop position on the floor, hands and knees. Maintain a straight back and a contracted core.
- Keeping the thigh perpendicular to the body, slowly raise one leg straight out to the side just like a fire hydrant until parallel to the ground.
- Raise the leg only as high as you can maintain good form. Do not let the hips rotate.
- Slowly lower back down to the start position with control. Repeat 10 times.
- Switch to the other leg, raising it out to the side in the same controlled manner keeping hips and leg parallel to the floor.
- Complete 10 controlled reps on each side, keeping abs braced.
- To increase difficulty, attach a resistance band above the knees or ankle weights on the moving leg.
- To decrease difficulty, do not raise your leg as high off the floor. Go only to your point of control.
Single-leg glute bridge exercise
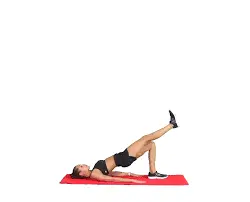
- Lie face up on the floor with arms to your sides, palms down, and knees bent with feet flat on the floor.
- Extend the knee by raising one leg off the floor. Maintain foot dorsiflexion.
- Push down firmly through your planted heel, engage your glutes, and drive hips up towards the ceiling until the body forms a straight line from shoulders to elevated knee.
- Pause briefly at the top position when hips are fully lifted off the floor. Squeeze glutes.
- Slowly lower hips back down to the floor with control while keeping abdominals braced.
- Repeat 10-15 reps keeping tension on the glutes throughout movement. Keep hips square.
- Switch sides and perform single-leg glute bridges with the opposite leg lifted to complete the full set on each side.
- To increase difficulty, place an exercise band around the thighs or straight leg. To decrease difficulty, perform double-leg glute bridges instead.
Donkey kick exercise
- Get on all fours with palms flat under your shoulders and knees directly below your hips in a tabletop position.
- Keep your back in a neutral, straight line and engage your core muscles.
- Keeping the knee bent at 90 degrees, slowly kick one leg up and back towards the ceiling without arching your back. Aim your heels towards the ceiling.
- Raise your leg only as high as you can control while keeping your pelvis and hips stable and centered. Avoid twisting your body.
- Pause briefly as you reach the top contracted position, squeezing your glutes.
- With control, slowly lower the raised leg back to the starting position just off the floor.
- Before moving on to the second leg, repeat for ten to fifteen controlled repetitions.
- Complete the desired number of reps for each leg, maintaining stability throughout.
Rehabilitation phases after hip surgery for hip pain
Phase 1 (0-6 weeks):
Goals: Protect repair, decrease pain and inflammation, prevent muscle atrophy
Interventions:
- Use crutches/walker for protected weight-bearing
- Passive range of motion exercises
- Isometric strengthening
- Modalities – ice, compression, e-stim
- Progress weight bearing and gait as tolerated
Phase 2 (6-12 weeks):
Goals: Restore full range of motion, improve strength and flexibility, normalize gait
Interventions:
- Advanced weight-bearing status
- Active range of motion and stretching exercises
- Progress core and hip strengthening
- Begin proprioception and balance activities
- Start functional mobility retraining
Phase 3 (3-6 months):
Goals: Build strength and endurance, continue mobility gains, prepare to return to activities
Interventions:
- Advanced flexibility and strengthening program
- Dynamic weight-bearing exercises – squats, lunges
- Balance challenges – single-leg standing
- Impact control exercises – step downs
- Sport/job-specific training
Phase 4 (6+ months):
Goals: Maximize function, progress muscle power for activities, gradual return to full duties
Interventions:
- Sport/job-specific agility drills
- High-level balance challenges
- Monitor hip joint mechanics with activity
- Maintenance fitness program
Prevention strategies for hip pain
- Strengthen hip and core muscles: Weak gluteal, hip abductor, quadriceps, and core muscles can contribute to poor alignment, instability, and overuse injuries. Perform targeted strengthening exercises 2-3 times per week.
- Stretch tight muscles: Tight hip flexors, IT bands, hamstrings, and piriformis can pull on the hip joint and limit mobility. Perform consistent stretching daily targeting these muscle groups.
- Use proper exercise form: Whether weight lifting, running, or playing sports, always use proper biomechanics and engage your core to help prevent compensation injuries. Consider seeing a PT if unsure.
- Wear appropriate footwear: Shoes with adequate cushion and arch support can better absorb impacts to the hips and spine. Replace running shoes every 300-500 miles.
- Lose excess weight: Carrying extra weight, especially around the abdomen and hips, increases stress and loading on the hip joints which can accelerate wear and tear.
- Use anti-inflammatory foods: Foods containing healthy fats like avocados, fatty fish, nuts and seeds can help reduce inflammation related to arthritis.
- Rest and recovery: Listen to pain signals and avoid overtraining or overusing the hip joint. Take regular rest days for any high-impact activities.
- Posture awareness: Sitting or standing with poor posture for prolonged periods can contribute to hip discomfort. Maintain a neutral spine.
Home remedies that can help treat hip pain
- Ice Packs Wrapping ice packs around the hip area for 15-20 minutes several times per day can reduce inflammation and pain. Make sure to wrap ice packs in a towel before applying to prevent cold burning of the skin.
- Heat Packs Applying a heat pack, heating pad, or warm compress to the hip for 15-20 minutes 2-3 times per day helps relax the muscles, increase blood flow, and reduce stiffness in the hip joint.
- Epsom Salt Baths Taking a warm bath with Epsom salts a few times per week can help ease muscle soreness and relax the body. The magnesium in the Epsom salt has anti-inflammatory benefits.
- Ginger Consuming ginger daily in food, tea, or supplements can help reduce inflammation related to arthritis or bursitis that causes hip discomfort.
- Turmeric Similar to ginger, taking turmeric containing curcumin daily has natural pain relieving abilities due to its anti-inflammatory effects.
- Stretching Performing simple hip, thigh, and gluteal stretches at home daily keeps muscles flexible and prevents stiffness. Hold stretches for 30 seconds, repeating 2-3 times each.
- Massage Using a tennis ball or foam roller to self-massage the hip muscles increases blood flow and relaxes tight tissues. Can be done daily.
Summary
Hip pain is an increasingly common complaint, especially among active adults and older populations. This uncomfortable and often debilitating pain can stem from a variety of hip joint, muscular, and nerve-related issues.
In this blog post, we dive into the complex anatomy of the hip area along with common causes of hip pain like osteoarthritis, bursitis, strains, and femoro-acetabular impingement syndrome. Illustrations and MRI images help provide visual examples of what’s occurring inside the hip joints during these painful conditions.
Comprehensive prevention strategies are provided, highlighting ways to promote hip health through targeted stretching and strengthening regimens. The importance of core stability, anti-inflammatory lifestyle habits, proper biomechanics with exercise, and responsible progressions in activity levels is discussed.
Conservative treatment options are covered, including various medications, injections, physical therapy, and bracing alternatives to help manage irritated hip issues at home. Surgical options like hip arthroscopy and replacement are explored as last resort when conservative methods fail to provide lasting relief after an adequate trial period.
FAQs
What are the most common causes of hip pain?
Some of the most common causes include osteoarthritis, strains, bursitis, tendinitis, fractures, and femoroacetabular impingement syndrome (FAIS). Hip pain can also arise from referred pain from the lower back.
What are some symptoms that may accompany hip pain?
Symptoms that often accompany hip pain include stiffness, limping, difficulty bearing weight on the affected leg, popping sounds, reduced range of motion, and inflammation/swelling around the hip joint.
What home remedies help relieve hip pain?
Applying ice packs, using heating pads, performing gentle stretches, taking anti-inflammatory medication, and resting the hip can help temporarily relieve discomfort from strained muscles or arthritis flare-ups.
When should you visit a doctor if you have hip pain?
See your doctor if pain persists longer than 1-2 weeks, causes severe disability, results from injury, or is accompanied by symptoms like sudden swelling, numbness, fever, abdominal pain, or inability to bear weight following a fall.
How is hip pain typically diagnosed?
Doctors use medical history, physical examination, palpation, range of motion tests, manual muscle tests, neurological tests, and imaging like X-ray, CT scan, or MRI to diagnose the underlying cause of hip pain.
What treatment options are available for chronic hip pain?
Conservative options involve medication, injections, physical therapy, orthotics, bracing, and lifestyle changes. Surgery like osteotomy, debridement, arthroscopy, or total hip replacement may be considered if conservative treatment fails.
What exercises help strengthen hips and reduce pain?
Stretching tight muscles and strengthening weakened gluteal and core muscles through bridges, monster walks, clamshells, and resisted band exercises help provide stability and support for the hip joint.
How can I prevent future hip pain?
Prevention strategies involve maintaining a healthy body weight, proper strength & flexibility, using good exercise form, wearing supportive shoes, stopping activity if severe hip pain occurs, and addressing underlying issues early.
References
- Blake, K. (2023, March 14). Everything You Need to Know About Hip Pain. Healthline. https://www.healthline.com/health/hip-pain
- Watson, S. (2010, June 8). Hip Pain: Causes and Treatment. WebMD. https://www.webmd.com/pain-management/hip-pain-causes-and-treatment
- Hip pain. (2023, September 1). Mayo Clinic. https://www.mayoclinic.org/symptoms/hip-pain/basics/definition/sym-20050684
- Professional, C. C. M. (n.d.). Hip Pain. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/21118-hip-pain
- Hip Pain and Mobility Deficits. (n.d.). Physiopedia. https://www.physio-pedia.com/Hip_Pain_and_Mobility_Deficits
- Dpt, K. G. P. (2023, October 7). How To Relieve Hip Pain. Verywell Health. https://www.verywellhealth.com/hip-pain-relief-5093637#toc-surgery
- Davis, N. (2023, March 15). Try This: 12 Exercises to Relieve Hip and Lower Back Pain. Healthline. https://www.healthline.com/health/pain-relief/exercises-for-hip-pain
- Dpt, K. G. P. (2024, February 2). What to Expect From Trochanteric Bursitis Physical Therapy. Verywell Health. https://www.verywellhealth.com/trochanteric-bursitis-physical-therapy-5189471#toc-prevention



14 Comments