Tennis Elbow (Lateral Epicondylitis)
What is a Tennis Elbow?
Tennis elbow, clinically known as lateral epicondylitis, is a common condition characterized by pain and tenderness on the outer aspect of the elbow. Despite its name, tennis elbow can affect anyone, not just tennis players, and it typically occurs due to repetitive motion or overuse of the forearm muscles and tendons. Microtearing of the tendons can also result in Tennis elbow in certain situations.
The tennis elbow is known medically as lateral epicondylitis. Inflammation of the extensor muscle tendon is known as epicondylitis. Inflammation on the lateral side, or the outer edge when you hold your arms at your sides and face your palms forward in the same direction as your eyes, is referred to as lateral epicondylitis.
Tennis elbow can result from any motion that requires you to grasp, twist, or swing your forearm often. If you experience discomfort that doesn’t go away after a week or if you have an elbow injury, see a doctor. Your treatment choices (and their efficacy) may improve if you consult a professional as soon as the pain begins.
Lateral elbow discomfort or lateral epicondylitis are other names for tennis elbow. Tennis players are not the only people who can have the illness, despite its name. It is the most typical elbow overuse condition.
When you use a region of your body so frequently for the same sort of action that your tissue becomes damaged, you might have a repetitive strain injury.
The term “tennis elbow” refers to a frequent sports condition suffered by athletes who play racket sports, such as tennis. It occurs when you overuse the tendon (your extensor muscle tendon) that joins your elbow to your forearm muscles.
About 5% of persons who have to use their arms repeatedly or who use vibrating instruments are at a higher risk of developing tennis elbow, which affects 50% of tennis players. Plumbers, painters, carpenters, butchers, musicians, nail techs, and dentists are a few professions that could be included.
It often affects those in the age range of 30 to 50.
Tennis elbow discomfort mostly affects the area on the outside of your elbow where the tendons of your forearm muscles attach. It can also radiate to your wrist and forearm. Tennis elbow mostly affects the area where the forearm muscles’ hard, cord-like tissues join to an outward bony bump of the elbow. Tendons are the name for the tissues. Wrist and forearm pain is possible to spread.
Tennis elbow is frequently relieved by physical treatment, medication, and rest. Individuals who are unresponsive to these therapies or whose symptoms interfere with day-to-day functioning may need to have a procedure, such as surgery or an injection.
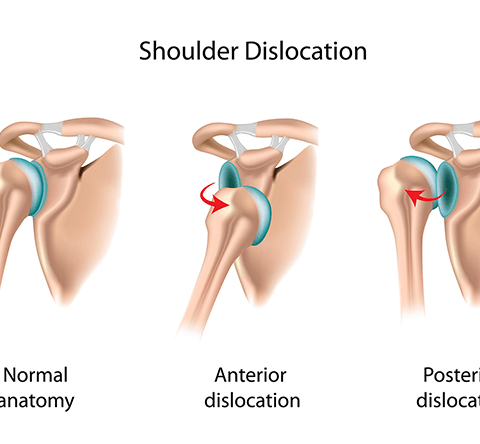
Anatomy
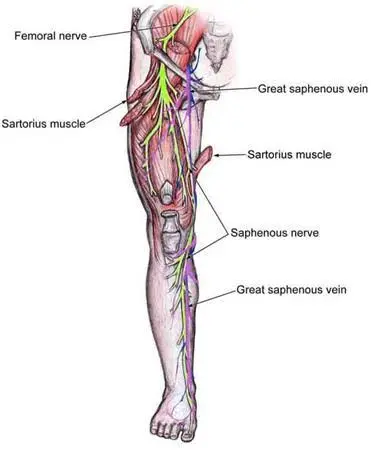
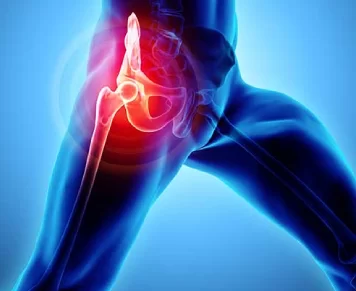
The humerus, the bone in your upper arm, and the radius and ulna, the two bones in your forearm, form your elbow joint. The epicondyles, which are bony protuberances at the base of the humerus, are the starting points of various forearm muscles. The lateral epicondyle is the bony protuberance located on the outside (lateral side) of the elbow.
The elbow joint is held together by ligaments, tendons, and interosseous muscles.
A condition known as lateral epicondylitis, or tennis elbow, affects the tendons and muscles in your forearm that allow your fingers and wrist to extend. Your fingers and wrists are extended by your forearm muscles. The tendons in your forearm, sometimes referred to as extensors, connect the muscles to the bone. The extensor carpi radialis brevis (ECRB) tendon is often implicated in tennis elbow.
Epidemiology
LET is categorized as an overuse injury that can lead to hyaline degeneration of the extensor tendon’s origin. The elbow tendons may be overworked due to overuse of the forearm and elbow muscles and tendons, as well as repeated motions or manual labor. These manual chores or contractions need hand manipulation, which results in tendon structural maladaptations and soreness over the lateral epicondyle. The lateral epicondyle is the primary source of anterior and distal discomfort.
Elbow tendinopathy affects the lateral rather than the medial portion of the joint in a 4:1 to 7:1 ratio, occurring at least five times more frequently. It affects 1-3% of people, most frequently those in their 35–50 year old age range. If the patient is younger than 35, it is critical to consider a differential diagnosis (growth plate problem, cervical spine referral). Consider osteoarthritis (OA), referred cervical spine discomfort, if the patient is older than fifty. Fifty percent of the 200 tennis players in Nirschl’s research who were older than thirty exhibited LET symptoms at some point.
Work-related activities that include wrist extension, pronation, or supination during manual labor, as well as household chores and hobbies, are thought to be significant contributing factors to this injury. Both sexes experience LET at the same rate. The illness strikes most often in people between the ages of 30 and 50. It is uncommon to have the disease at both lateral epicondyles; instead, the dominant arm is most likely to have LET. Of all cases, twenty percent last more than a year.
Three risk variables were found by a systematic review: using tools weighing more than one kilogram, carrying weights weighing more than twenty kilograms at least ten times a day, and engaging in repetitive motions for longer than two hours a day. Additional risk factors include aging, poor circulation, problems, training mistakes, overuse, repetitive motions, imbalances in strength or flexibility, and psychological issues.
Regarding the development of LET, there are several points of view:
Inflammation
Even though the word “epicondylitis” suggests that an inflammatory state is present, inflammation is only evident in the early stages of the illness process.
Microscopic tearing
The extensor carpi radialis brevis (ECRB) muscle’s origin was found to have microscopic tearing with the production of reparative tissue (angiofibroblastic hyperplasia) by Nirschl and Pettrone. The ECRB muscle’s origin may experience macroscopic tearing and structural failure as a result of this micro-tearing and healing response.
Cyriax (1936) proposed the theory that the illness process involves microscopic or macroscopic rips of the same extensor origin.
Coonrad and Hooper were the first to report macroscopic tearing in relation to the histology results.
Tissue specimen histology shows that increased proteoglycan content, cellularity, neovascularization, and local necrosis cause collagen disorientation, disorganization, and fiber separation. Nirschl named this histological finding “bangiofibroblastic hyperplasia.”
Since then, the term bangiofibroblastic tendinosis has been used instead. He observed that the tissue had immature fibroblastic and vascular components along with disordered, immature collagen production. The extensor carpi radialis brevis is discovered to be torn in varied degrees in conjunction with this gray, friable tissue.
Degenerative Process
Regan et al. studied the histological characteristics of 11 individuals who had LET. They came to the conclusion that a degenerative process rather than an inflammatory one was more likely to be the cause of LET. Increased fibroblasts, vascular hyperplasia, proteoglycans, and glycosaminoglycans, as well as disordered and immature collagen, are indicative of a degenerative disease.
The underlying mechanism of this angiofibroplastic tendinosis of the ECRB is believed to be repetitive eccentric or concentric overloading of the extensor muscle mass. LET is a degenerative disorder characterized by elevated fibroblastic activity and the production of granulation tissue inside the tendon.
Hypovascularity
Functional tolerance declines as a result of the tendinous unit’s inability to appropriately respond to recurrent stresses sent by the muscle because this tendinous region comprises regions that are particularly hypovascular.
What are the Causes of Tennis Elbow?
Tennis elbow is the result of repeatedly using the arm incorrectly. Little rips in the tendon attachment at the elbow result from this. Tennis elbow may result from:
Tennis: Tennis elbow is a result of repeatedly striking a ball with a racket and exerting effort.
An improper technique might cause the racket to swing with enough power to twist through and around the wrist. Instead of creating a movement on the shoulder or elbow joint, it causes a movement on the wrist. This thus puts more strain on the tendon and causes inflammation and discomfort.
This tendon tear causes discomfort in the extensor muscles, which straighten the wrist.
Overuse: When the elbow is straight, the extensor carpi radialis brevis (ECRB) muscle helps keep the wrist in place. Overuse affects the ECRB, causing minute rips to occur in the tendon. Pain and inflammation follow from this.
The ECRB is highly vulnerable to damage because of its location. When the elbow bends and straightens, the ECRB muscles press on bony protuberances. It may cause the muscle to gradually deteriorate over time.
Other Causes
Overuse that results in tendon tears is the cause of tennis elbow. Tennis aside, it can also be brought on by regular activities that involve the forearm muscle being used repeatedly and vigorously or the wrist and hand being repeatedly extended, like:
- With scissors
- cutting difficult food
- Horticultural practices involving a lot of tossing Sports
- Swimming Hand movements that need repeatedly twisting or elevating the wrist.
- Painting,
- Plumbing,
- Woodworking
- Cooking with Butch
- Sometimes the specific etiology of tennis elbow is unknown.
Signs and Symptoms:
Tennis elbow signs appear gradually. Generally speaking, tennis elbow is not caused by a particular injury.
Pain is the most prevalent symptom. Over the course of the weeks and months, pain develops from a small, insignificant beginning.
The ache is located immediately below the elbow’s bend, outside the upper forearm. I sense the discomfort traveling down the arm and near the wrist.
Additionally, you get pain when bending or lifting your arm. It gets harder to write and hold tiny things when doing fundamental tasks.
Initially, if the pain is not otherwise evident, you can feel it when you try to completely extend your forearm, twist your forearm, or turn a door handle.
On the outside of your elbow, you could experience discomfort or burning. Even if you don’t have discomfort during the day, you could throughout the night. Tennis elbow causes the grip to weaken significantly.
- broad-based achiness.
- stiffness in the morning.
- Periodic ache in the night.
- dropping things or having a weak grasp.
- Palpable pain in the lateral epicondyle.
- discomfort while extending actively or resistively.
- Pain when using the affected hand to hold items.
- soreness or pain on the elbow’s outer side.
- ache when your wrists and hands are raised or straightened.
- Pain is exacerbated when moving a large, heavy object.
- Handshakes, turning door knobs, gripping objects, and fists all cause pain.
- ache that radiates up or down the forearm or upper arm from the elbow.
- Burning or soreness on the outside of your elbow that might radiate to your wrist (these feelings could get worse at night).
- discomfort or stiffness when your arm is extended.
- When holding little items, like pens, Use one’s forearm to twist anything, such as a doorknob or jar.
The majority of patients (90%) recover completely in a year, with tennis elbow typically lasting between six months and two years.
PAIN PHASES:
- Phase 0: No discomfort or pain.
- Phase 1: Post-activity soreness that goes away in most cases in 24 hours.
- Phase 2: Before an exercise, there is some mild stiffness and pain, but this goes away with a warm-up. No discomfort while exercising, but a little stiffness that goes away in a day or two thereafter.
- Phase 3: Moderate to mildly stiff and painful, along with slight discomfort that does not interfere with activities.
- Phase 4: Pain that arises from an activity that changes its course.
- Phase 5: Constant discomfort, even when at rest.
CONTRIBUTING FACTORS:
- weak muscles.
- Overuse: Using excessively strong grips repeatedly while working or playing.
- keeping a grip while bending or rotating the wrist.
- Tools or racquets that are imbalanced or overly heavy.
- Inappropriate tools: grip size is wrong, and strings are too tight.
- Inadequate playing technique: excessive wrist movement, jerky blows, and inadequate ball contact.
Differential diagnosis
- Radial Tunnel Syndrome
Pain in the forearm’s posterolateral region
Occasionally, the dorsal side of the wrist becomes inflamed.
- Paraesthesia Weakness (musculoskeletal system overuse injuries)
syndrome of the posterior interosseous nerve.
- Osteoarthritis in the elbow pain
Inadequacy concerning the extension of the wrist and fingers
deficiencies in motor skills
pain
reduction in range of motion
- Fractures
Distal Radial Bone Breaking
Fractures of the Radial Head, Fracture of the Olecranon
Radiculopathy of the Cervical Region
discomfort radiating from the arm that matches the dermatomes
ache in the neck
Paraesthesia
Myotome muscle weakening
Impairment or lack of reflex
Headache
Pain in the scapula
impairment of the senses and motor function in the neck and upper limbs
- Cervical Disc Disease
- Cervical Myofascial Pain
- Cervical Spondylosis
- Fibromyalgia
- Medial Epicondylitis
Diagnosis
Tennis elbow can be diagnosed with a simple test that you can do at home.
Take a position behind a chair. Place your palms face down on the back of the chair, keeping your elbows straight. Try to lift the chair while holding it.
Tennis elbow may be indicated by pain on the outside of the elbow. Get in touch with your doctor if you have any pain.
When diagnosing you, your doctor will take a number of things into account. These include the course of your symptoms, any risk factors related to your job, and your involvement in leisure activities.
Your physician will discuss with you the activities that trigger your symptoms as well as the location of your arm’s problems. If you have ever had an elbow injury, make sure your doctor knows about it. Inform your physician if you have ever experienced nerve damage or rheumatoid arthritis.
Your doctor will employ a range of tests throughout the examination to determine the exact diagnosis. To check if this produces discomfort, your doctor could, for instance, ask you to try straightening your wrist and fingers against resistance while keeping your arm completely extended. Your doctor will be informed that certain muscles might not be in good health if the tests are positive.
Physical Exam:
The physical examination involves the therapist touching and visually examining the patient’s elbow, arm, and maybe other body joints. When the lateral epicondyle, or the outside surface of the elbow, is pushed upon by the therapist and the pain is replicated, it is generally thought that lateral epicondylitis has occurred.
The therapist will examine bone and joint alignment in addition to using a hammer to measure nerve responses. The patient’s skin may be inspected for signs of autoimmune diseases, such as rheumatoid arthritis, and blood may be collected to check for these signs. In order to determine whether or not this produces discomfort, the therapist may also ask patients to extend their affected arms straight and then press their hands and fingers back.
When the extensor muscles’ origin in the lateral epicondyle is palpated, pain is the most common sign of LET. In rare instances, the pain may even spread to the third and fourth fingers. It may also radiate upward along the upper arm and downward down the outside of the forearm. In addition, it is frequently seen that the posterior shoulder muscles and wrist extensors are weak and flexible.
Regarding the severity of the symptoms, Warren states that there are four phases in the development of this damage.
- Faint discomfort a few hours following the action that caused it.
- Pain that occurs during or right after the activity that provoked it.
- Pain that starts during the provocative action and is worse after it stops.
- Constant discomfort that makes it impossible to do anything.
In addition, it is frequently seen that the posterior shoulder muscles and wrist extensors are weak and flexible. Patients at least describe grip weakness or trouble holding things in their hands, particularly when their elbows are extended. Finger extensor and supinator weakness is the cause of this weakness. Though rare, some people experience paralysis.
The usual duration of symptoms is two weeks to two years. With the possible exception of avoiding uncomfortable activities, 89% of patients recover in a year without any therapy (sports injuries).
Assessment Findings
To ensure that the right treatment plan is followed and that the healing process is accelerated, a comprehensive evaluation and examination are essential components. A differential diagnosis should not be excluded from the evaluation.
Potential results of a subjective evaluation may be:
beginning of the pain 24-72 hours following an inciting incident involving the extension of the wrist
Pain might be felt all the way down the forearm to the wrist and hand.
Lifting and gripping difficulties (pain+/- weakness)
biomechanical variables changing, such as a new tennis racquet, a damp ball, excessive training, bad technique, or a shoulder injury
Within the impartial evaluation, one might discover:
Over the lateral epicondyle and/or 1-2 cm distal to the epicondyle, there is pain and point tenderness.
Weakness and discomfort when resisting wrist extension
Weakness on the Dynamo-meter test of grip strength
Pain and/or reduced range of motion when passively extending the elbow, flexing the wrist, and pronating the ulna
weak flexors and extensors of the elbow
Special Test:
The diagnosing process begins with obtaining a patient’s medical history and asking about their activity level, occupational risk factors, participation in recreational sports, medication, and other health issues. It’s critical to understand the activities that trigger your arm’s symptoms as well as their location.
The structure of the elbow and other joints is evaluated during the physical examination. Examined include the muscles, bones, nerves, and skin as well. Tenderness over the ECRB or common extensor origin supports the LET diagnosis. The physical therapist or therapist should be able to replicate the usual discomfort using the following techniques.
A dynamometer and the Patient-rated Tennis Elbow Evaluation Questionnaire (PrTEEQ) can be used to assess the severity of tennis elbow. Grip strength is measured with a dynamometer. A 15-item survey called the PrTEEQ is used to measure forearm pain and impairment in lateral epicondylitis patients. There are two subscales on which the patients must score their degrees of tennis elbow discomfort and impairment on a scale from 0 to 10. There are two subscales: function (0 = no problem, 10 = impossible to accomplish) and pain (0 = no discomfort, 10 = worst imagined).
Cozen’s test: The resisted wrist extension test is another name for Cozen’s test. Ninety-degree flexion stabilizes the elbow. The patient’s hand is placed in radial deviation and forearm pronation by the therapist as they palpate the lateral epicondyle. Next, it is requested that the patient resist wrist extension. If the patient feels a sudden, intense pain above the lateral epicondyle, the test is positive. increased sensitivity Positive results have been observed, indicating the presence of LET, although the specificity to exclude other differential diagnoses is low.
Chair test: The patient stands behind the chair, grasps its back, and tries to raise it with a three-finger squeeze (thumb, index, and long fingers) and a fully extended elbow. When pain is felt at the lateral epicondyle, the test is considered positive.
Mill’s Test: The patient sits with their elbow extended and their upper extremities relaxed at the side. The examiner extends the wrist in pronation and flexion passively. A good indicator for LET is pain at the proximal musculotendinous junction of the wrist extensors or at the lateral epicondyle.
Maudsley’s test: The examiner palpates the lateral epicondyle while resisting the urge to extend the hand’s third digit. Pain above the lateral epicondyle indicates a positive test result. It has been discovered that there is an 88% sensitivity when the LET diagnosis is included but not confidently excluded.
The coffee cup test involves doing a specific task, like picking up a milk bottle or a full cup of coffee. On a scale of zero to 10, the patient is asked to rate their level of pain.
Diagnostic Imaging:
Diagnostic imaging is often not necessary for tennis elbow; nevertheless, in order to rule out other potential explanations of the patient’s symptoms, scan tests may be requested. As an illustration:
X-rays:
While tennis elbow is not visible in these images, they can be utilized to identify other diseases such as bone fractures and misaligned joints.
Plain elbow X-rays (AP and lateral views) may be obtained in chronic instances to rule out elbow arthritis. Common findings include osteochondritis dissecans, degenerative joint changes, calcification along the lateral epicondyle, and heterotopic calcification.
Magnetic resonance imaging (MRI):
MRI can assist in ruling out further elbow issues, such as ligament tears or cartilage damage.
A Magnetic Resonance Imaging (MRI) scan may be requested if there is a suspicion that the symptoms are connected to the neck.
This might indicate the presence of arthritis or a potential herniated disk in the neck region. Arm discomfort is a common symptom of both of these disorders.
In the event of LET, an MRI may also reveal thickness, hypoechogenicity, or abnormalities in the tendo-osseous enthesis nonetheless, the existence of these findings should be carefully considered when making treatment choices.
Electromyography (EMG):
This test may be requested to assess nerve conduction if the physician believes that the patient’s elbow symptoms are due to nerve compression or entrapments in the elbow.
By using electromyography (EMG), nerve compression can be ruled out. Numerous nerves around the elbow, therefore tennis elbow and nerve compression sensations are comparable.
Power Doppler ultrasound:
This kind of ultrasound may be used to rule out tennis elbow as well as other tendon issues in addition to diagnosing tennis elbow.
When investigating individuals with lateral elbow discomfort, ultrasound testing can be performed to show the extent of tendon injury and whether or not a bursa is present.
A Magnetic Resonance Imaging (MRI) scan may be requested if there is a suspicion that the symptoms are connected to the neck.
This might indicate the presence of arthritis or a potential herniated disk in the neck region. Arm discomfort is a common symptom of both of these disorders.
In the event of LET, an MRI may also reveal thickness, hypoechogenicity, or abnormalities in the tendo-osseous enthesis nonetheless, the existence of these findings should be carefully considered when making treatment choices.
A Magnetic Resonance Imaging (MRI) scan may be requested if there is a suspicion that the symptoms are connected to the neck.
This might indicate the presence of arthritis or a potential herniated disk in the neck region. Arm discomfort is a common symptom of both of these disorders.
In the event of LET, an MRI may also reveal thickness, hypoechogenicity, or abnormalities in the tendo-osseous enthesis nonetheless, the existence of these findings should be carefully considered when making treatment choices.
Treatment of Tennis Elbow
Medical Management
Non-Operative Medical Treatment
The initial line of treatment for LET is non-operative medical care. Initially, it is predicated on two ideas: reducing inflammation and easing pain. This might consist of:
- Rest and activity moderation are standard recommendations for pain relief.
- In acute situations, NSAIDs may be used to reduce inflammation and provide temporary pain relief. It’s also advised to apply ice three times a day for fifteen minutes each time to reduce edema and the inflammatory response via vasoconstriction and lower the degree of chemical activity. If there is edema in the fingers or wrist, elevation of the extremities is also advised.
- One such useful tool for lessening the pain associated with LET contractions may be an elbow counterforce brace. In the context of a forearm orthosis, it can serve as a supplementary point of muscle attachment and ease strain at the lateral epicondyle insertion. Applying the brace around the forearm (behind the head of the radius) and tightening it just enough prevents the patient from fully contracting the wrist extensors.
- Subperiosteally, injections can be administered to the extensor brevis origin. There are reports of an early and positive reaction from these injections. On the other hand, more discomfort might be felt in the first 24 to 28 hours. A steroid injection should not be given more than twice and is often followed by a rest period of one to two weeks. According to reports, hyaluronic acid and steroid injections work for around three months, therefore the patient has to stick to their workout regimen. The preparation and effectiveness of autologous blood and platelet-rich plasma injections differ. In the intermediate or long term, no definite advantage of injections over placebo has been demonstrated, and it is important to take potential recurrence into mind.
- Brace: Applying a brace across the rear of your forearm may also assist in reducing tennis elbow discomfort and symptoms.
Brace with counterforce. - Rest: It’s crucial to give the injured arm some time to heal. Give the tears in the tendon attachment time to heal by taking a vacation from the activities that are causing the issue. For more severe cases of tennis elbow, tennis players use ultrasound therapy, soft tissue massages, cold packs, and anti-inflammatory drugs.
- Physical Therapy: Physical therapy is an option for you. Your therapist will provide you with workout recommendations to help strengthen your abdomen, upper arm, and shoulder muscles. When moving the arms and shoulders, wrist extensors can be weakened with strengthening workouts.
- Muscle-stimulating methods and ice massages can aid in the healing of the muscles.
- Strap or tape the forearm: A splint can be used to support the injured region. By doing so, pressure on the affected location can be released and the muscle fibers realigned. Your physician could advise wearing a splint to immobilize your elbow for two to three weeks.
Surgical treatment
Surgical intervention may be necessary if non-operative care is unsuccessful for more than six months. The majority of surgical treatments for this illness entail cutting off sick muscle and reattaching good muscle to the bone. Many different considerations will determine the best surgical strategy. These consist of the extent of the damage, overall health, and individual requirements.
a surgical incision. The most popular method for LET repair is this one. An incision across the elbow must be made. Typically, open surgery is carried out as an outpatient procedure. Rarely does it need for an overnight hospital stay.
arthroscopy for Small incisions and tiny equipment can also be used to repair LET. This is an outpatient, same-day operation, much like open surgery.
Surgical risks: There are several risk considerations for each procedure. Typically, surgical risks include:
- Damage to blood vessels and nerves
- Decrease strength
- Reduced flexibility
- Infection
Rehabilitation:
Your arm can be temporarily immobilized following surgery. Your doctor may use a splint to support the injured region. After a week, the splint is taken off.
Stretching exercises are then initiated to regain the flexibility. However, the strengthening workouts begin two months following the operation.
Your doctor will let you know when you may resume your sports activities if you are an athlete, whether it be tennis or another sport. After surgery, this typically takes four to six months. Eighty to ninety percent of individuals had satisfactory outcomes after tennis elbow surgery. Rarely, nevertheless, patients experience strength loss.
Because your job requires you to use your arms often, tennis elbow may be quite damaging in terms of both money and physical health. It may even cause an athlete to give up on their sport.
Thus, pay attention to the symptoms. Testing is usually advised, even if you are only unsure.
Physiotherapy Management
Among the general physical therapy treatment techniques for LET are:
Information and guidance about managing pain and/or altering one’s activities
Shockwave therapy, laser, massage, ice, ultrasound, and transcutaneous electrical nerve stimulation (TENS) are some of the modalities used.
Exercises Under SupervisionMulligan – Manual therapy – Strengthening and stretching – Mobilization via movement
Rehabilitation is specific to a sport or occupation.
Evidence for Physical Therapy
There is currently little data to determine how best to employ physical therapy techniques in the treatment of LET. As a result, different physicians and patients may choose different appropriate approaches or combine different ones.
You may read more about a few of the physical therapy techniques described above down below.
Extracorporeal Shockwave therapy (ESWT)
Treatment for several tendonopathies, including LET, involves ESWT. Strong mechanical wave impulses that may be applied in a reasonably exact position are exposed to the patients. Numerous research looks at how ESTW affects LET. Even though the process is usually thought to be safe, there is a possibility of bleeding and localized soft tissue damage because of cavitation; it appears that these side effects are more frequent with greater doses.
Cyriax Physical therapy
Deep transverse friction (DTF) is used in Cyriax physical therapy in conjunction with Mill’s LET manipulations. The prescribed order must be followed when using both therapy components together. For four weeks, the patient has to adhere to the treatment three times a week. Regarding this therapy, there are a number of contraindications, including active rheumatoid arthritis, bursitis, abnormalities of the nerve structures, ossification and calcification of the soft tissues, and anticoagulants. Cyriax physical therapy shows considerably improved scores on all follow-up assessments (p<0.05), suggesting that it is a superior treatment for LET when compared to phonophoresis and exercise.
Deep Transverse Frictions
A particular kind of connective tissue massage called deep transverse friction is given carefully to the soft tissue structures. To prime the tendon for Mill’s manipulations, the therapist must attempt to produce an analgesic effect by applying the DTF at the lesion site for ten minutes, or until a numbing effect is achieved. Pain experienced during a friction massage is seen as an incorrect indicator. There must be a 48-hour gap between the two sessions. Preserving the soft tissue structures’ mobility is the aim of deep friction massage.
More research is required, but it appears to have a pain-relieving effect because it softens scar tissue, improves connective tissue fibril alignment, modulates nociceptive impulses (gate control hypothesis), and enhances blood flow.
After positioning the patient with their arm fully supinated in a 90° elbow flexion, locate the sensitive spot on the lateral epicondyle and apply pressure (DTF) in a posterior direction on the teno-osseous junction using the tip of their thumb on the lateral epicondyle. The patient’s wrist is stabilized by the opposite hand.
Mills Radial Head Manipulation
Physical therapists most frequently employ Mill’s manipulation, which involves a small-amplitude, high-velocity push near the end of elbow extension with the wrist and hand held flexed. By breaking up adhesions at the teno-osseous junction, this procedure aims to lengthen the scar tissue and restore mobility and painlessness to the affected region. It is employed in imitation of the spontaneous recovery mechanism. Mill intended to replace and move the annular ligament. According to Cyriax, the annular ligament gives the extensor carpi radialis muscles the most stretching stress; thus, the manipulative operation should be performed with a strong jerk to open the tendon rip and release strain on the tendon scar by converting.
This treatment needs to be done only when an elbow extension can be made completely pain-free and with the right form. During the process, complete wrist flexion must be attained to stop the symptoms from getting worse. The patient is sitting with internal rotation and 90° abduction of the affected extremity (olecranon facing up). With one hand on the olecranon and the other supporting the patient’s wrist in full pronation and flexion, the therapist stands behind the patient. It is crucial to maintain complete wrist flexion since failing to do so may cause the humeroulnar joint to absorb most of the thrusting effort.
At the end range of elbow extension, the high-velocity low amplitude (HVLA) thrust is a rapid movement in the direction shown.
When this maneuver is performed, there may be some little pain. This approach can be used by the physician two to three times per week for a total of four to twelve sessions.
Heat Therapy:
One of the best and most dependable treatments for tennis elbow is heat therapy. Use heat treatment to encourage blood flow if you’ve had tennis elbow for a time and your muscles are tight. It promotes healing and helps the muscles relax.
Platelet-rich plasma: PRP, or platelet-rich plasma, is a biological therapy intended to enhance the tissue’s biological environment. Your physician will draw a tiny amount of blood from your arm for PRP and separate the platelets from the mixture.
The injured region will receive an injection of platelets, which are renowned for having a high concentration of growth factors in them.
Numerous studies are being conducted to determine the usefulness of PRP; some have yielded conflicting results, while others have shown encouraging outcomes.
Massage: Therapeutic massage can assist to release tense muscles and restore healthy blood flow.
Taping
Rigid tape used in the diamond taping technique may help with pain management, grip strength, and functional performance.
Electrotherapy modalities:
Numerous forms of physical therapy seek to enhance function and lessen discomfort by stimulating the body’s electrical, magnetic, light, sound, or thermal energy.
- Ultrasound: Using ultrasonic waves, therapeutic ultrasound delivers energy to deep tissue areas. In order to improve bodily tissue repair and muscle relaxation, the goal of therapy is to raise tissue temperature and cause non-thermal physiological changes.
- Transcutaneous electrical nerve stimulation (TENS): This technique stimulates underlying nerves by applying electrodes to the whole skin surface in the area of discomfort.
- LASER: The light beam produced by low-level laser treatment has the ability to reach tissue depths under the skin.
Exercises for tennis elbow:
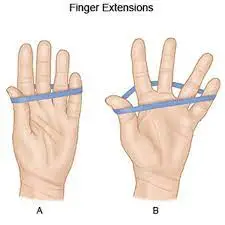
- Finger stretch with rubber band:
Wrap the patient’s thumb and fingers in a rubber band and gently cup their hand. and instructed them to gently stretch their fingers and thumbs apart before putting them back together. Repeat three sets of ten times.
- Grip:
This workout involves holding an object in your hand and squeezing it constantly for 10 to 15 minutes, twice or three times a day, using any soft object, such as a smiling ball or a little rubber ball.
- Downward wrist stretch:
With one arm extended straight, grip the hand with the other. Till you feel a stretch, slowly bend your wrist down and slightly out. Tension should be released after 15 to 30 seconds of holding. Do this twice or three times.
- Wrist curl (Palm up, Palm down):

Position the forearm flat over a table so that the palm faces up. For resistance, lay a weight or fitness band over your palm. Pull the wrist back toward the body with a different hand. Reposition the wrist back to the starting position slowly (about five seconds). Holding the exercise band or dangling weight, repeat this exercise with your hand facing down. For three sets, repeat each exercise ten times.
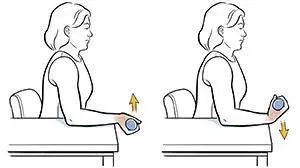
- Elbow curls (Palm up, palm down):
Step one ahead of the other. Place one end of an exercise band beneath the hinged foot and use one of two grips to grasp the other end with your hand. With your hand, pull up the band, then bend your arm in the direction of your shoulder. Instead of using an exercise band, you may use a dumbbell.
- Forearm pull (optional):
Stand with your legs slightly bent. With your hands down and your upper arms close to your sides, hold the weight bar at shoulder height. Lower the weight and then raise it again. Repeat three sets of ten times.
- Forearm Twist (optional)
Sit with your forearm propped up. Place your palm down on a hammer. Turn your forearm as far up and down as you can without hurting it.
- Resisted wrist extension.
- Resisted wrist flexion.
- Resisted forearm supination and pronation.
- Wrist flexor stretch.
- Wrist extensor stretch.
- Finger extension.
- Hand squeeze.
- Wrist range of motion:
As much as possible, bend your wrist forward and backward. Ten times over, repeat. Perform three sets.
- Range of motion for the forearm:
Bending your elbow to a 90-degree angle, raise your palm and hold it there for five seconds. Then, slowly lower it down and keep it there for another five seconds. Ten times over, repeat. Perform three sets. For the whole exercise, make sure your elbow is bent at a 90-degree angle.
- Range of motion of the elbow:
Bend your elbow as far as possible and gently raise your palm up toward your shoulder. Next, extend your elbow as far as possible. Ten times over, repeat. Perform three sets.
- Forearm pronation and supination:
Bend your elbow to a 90-degree angle while holding a soup can or hammer handle in your hand. Turn your hand slowly, first palm up, then palm down. Ten times over, repeat. Perform three sets.
- Extension of the wrist:
Take a stand and grasp a broom handle with both hands. Roll the broom handle backward in your hand as if you were reeling something in while keeping your elbows straight and your arms at shoulder height. After a minute of repetition, rest. Perform three sets.
Wrist strengthening:
- Wrist flexion:
Bend your wrist slowly upward while holding a soup can or hammer handle with your palm facing up. Lower the weight gradually and return to the starting position. Ten times over, repeat. Perform three sets. Increase the weight of the can you are holding gradually.
- Wrist extension:
Bend your wrist slightly upward while holding a soup can or hammer handle with your palm down. Once you’ve lowered, go back to the starting position.
the weight gradually. Ten times over, repeat. Perform three sets. Increase the weight of the can you are holding gradually.
Gradually raise the can’s weight that you are holding.
- Wrist radial deviation:
Raise your thumb and hold your wrist sideways. With your thumb pointing toward the ceiling, slowly bend your wrist up while holding a soup can or hammer handle. Reduce to the beginning point gradually. This exercise should be performed without moving your forearm. Ten times over, repeat. Perform three sets.
Stretching
One of the most crucial elements of fitness regimens is stretching and strengthening workouts. The basic idea behind stretching is that we may lessen the tendon’s stretching during offensive motions by extending it during rest.
The best position to stretch the Extensor Carpi Radialis Brevis tendon is with the elbow extended, forearm pronated, wrist flexed, and wrist ulnarly displaced, depending on the patient’s tolerance. During each therapy session, this stretching should be held for 30 to 45 seconds, three times before and after the eccentric movements, with a 30-second break in between.
According to some regimens, the extensor muscles of the fingers and wrists should be stretched in the following ways: Elbow completely extended, wrist primarily flexed. Hold the maximal, painless extension position for a duration of fifteen to twenty-five seconds. With two sets of ten exercises every session, this exercise is performed four to five times a day. The patient should always cease at the first symptom of pain. The patient should additionally engage in isotonic exercises during this phase of therapy, one a day, in accordance with the following schedule:
- Ten repetitions of stretching exercises (15–25 seconds)
- Isotonic workouts: repeat three series 15 times.
- Perform ten repetitions of the stretching exercises (15–25 seconds)
- Icing: Apply ice or crushed ice to the sore spot and massage it for ten to fifteen minutes.
Theraband Exercise:
Every day, three sets of ten theraband exercises—or exercises with a modest weight—are performed. One side of the theraband is fixed beneath your feet or in another location, while the other side is held in your hand or is supported by a little weight.
The patient begins the exercise by flexing his or her wrists, extending them, and then gently returning to the starting position. This wrist extensor workout alternates between concentric and eccentric movements. Compared to the Cyriax physical therapy strategy, supervised exercise consisting of static stretching and eccentric strengthening for four weeks may have a greater impact on pain, strength, and function. Patients can advance to a different color of theraband or you can raise the weight once they can accomplish this.
Flexbar Exercises

At home, one can utilize a resistance tool called the Flexbar.
Three sets of fifteen reps of the FlexBar workout are done every day. Every repeat takes 4 seconds, with a 30-second break in between each set of 15 repetitions. Patients advance to a different color FlexBar with a higher strength of eccentric resistance after they can complete three sets of 15. The patient’s symptoms won’t go away till the therapy is finished.
Elbow rehabilitation program:
It is crucial that the workouts be progressed gradually. The enclosed instructions may appear simple at first, but you must attentively follow them to avoid aggravating or worsening your symptoms.
Warm up your body to a mild sweat before starting the strengthening exercises. Try brisk walking, cycling, running, etc. for three to five minutes.
Exercise just once a day; doing so will not improve your condition and may make it worse. If your therapist recommends it or if you feel discomfort when doing the exercises, use the Counter-Force brace. Perform every workout at your own pace. Certain workouts will allow you to reach heavier weights more quickly than others. Take your time and carefully complete each exercise; don’t rush through them.
Stage 1 exercises:
- Keep your elbow at a ninety-degree angle. Lean forward and bend your elbow farther if this is painful. Make sure your forearm is securely resting on your thigh or a table.
- Perform 10 to 15 repetitions of each exercise at first without any weight.
- As your elbow allows, gradually increase the repetitions in sets of ten every few days until you can perform three sets of ten comfortably for two days in a row without experiencing a worsening of your symptoms.
- Raise the weight to one pound (a little soup can work great for this). Return to doing each exercise for 10 to 15 repetitions.
- Return to 3 sets of 10 repetitions slowly.
- Once more, reduce to 10 to 15 repetitions after increasing to a two-pound weight.
- Increase to three sets of ten repetitions gradually.
- Maintain this slow increase until you can perform three sets of ten repetitions with a three-pound weight without experiencing worsening discomfort.
- As you are able, move on to the next phase.
Stage 2 exercises:
- Exercises with rubber bands and squeezes:
- Start with your elbow bent at your side and work your way up to stretch your arm as far in front of you as you can. These two exercises should be performed many times a day, every day. Maintaining a ball and rubber band in handy locations, such as your workplace, car, or TV, is a smart idea. Exercises like this should not be overdone since this might make your discomfort worse.
- Ice following physical activity.
Self-care advises:
There are a few steps you may take to prevent tennis elbow from arising or reoccurring, such as avoiding painful tasks and finding an alternative way to perform them, as well as focusing less on utilizing your elbow and wrist than the rest of your arm.
Boost the strength of your forearm muscles.
When working or engaging in activities, use a splint.
Outcome Measures
It is not well documented that outcome metrics are used in LET elbow clinical practice and research. Nonetheless, the following are a few often utilized scales:
measure of pain-reported outcome
The Numerical Pain Rating Scale (NPRS).
Visual analog scale (VAS)
Self-reporting Questionnaires
The Patient Rated Tennis Elbow Evaluation (PRTEE):
Upper Limb Functional Index (ULFI):
Disability of the Arm, Shoulder, and Hand (QuickDASH):
Patient-Specific Functional Scale (PSFS): Shown to be valid, reliable, and responsive to change in other conditions like knee dysfunction, cervical radiculopathy, acute low back pain, mechanical low back pain, and neck dysfunction.
In a consensus report that was recently published, a global panel of tendinopathy specialists proposed nine basic categories linked to health that researchers and doctors may use to gauge patient outcomes:
Patient evaluation of their state
Engaging in daily activities
discomfort with exercise or loading
Operation
Psychological factors
Capacity for physical function Disability
Pain in terms of living quality over a given period of time
There are efforts underway to create a core set of outcomes for LET (COS-LET).
Prevention
- Avoiding overusing your arm and elbow is the best defense against tennis elbow.
- When engaging in physical activities, such as sports:
- Use the appropriate safety gear for all jobs, sports, and hobbies.
- Avoid “playing through pain” either prior to or following a workout.
- After a strenuous workout, give your body time to rest and recuperate.
- Warm up and stretch before participating in sports or physical exercise.
- After a workout, stretch and cool down.
- Exercise for your sport or to maintain your physical fitness for your career, hobbies, or sports.
Prognosis
If I have tennis elbow, what can I expect?
Anticipate taking a hiatus from the strenuous activities that resulted in tennis elbow. Certain tasks may need to be fully discontinued or modified (e.g., by wearing a brace while working or taking more frequent breaks).
Tennis elbow nearly often results in a full recovery. Even if you require surgery, you should be able to return to all of your regular activities when your tendon recovers.
How much time does a tennis elbow last?
The duration of tennis elbow might range from several months to over a year. The average recovery time is six months, however, some people require up to eighteen months.
Your recuperation period will change based on multiple variables:
- the reason behind the tennis elbow.
- The extent of the tendon injury.
- which medical interventions you require.
Conclusion
If you have never hit a tennis racquet before, it might be perplexing to hear that you have tennis elbow. However, the word “tennis elbow” (lateral epicondylitis) refers to the specific arm motions that have the potential to aggravate and harm an elbow tendon. To have tennis elbow, you don’t have to be a serious contender at Wimbledon. Actually, the majority of those who have it never even play tennis.
To allow their torn tendon to recover, most patients require many months of rest and nonsurgical therapy. Your healthcare physician will advise you on the best course of action for you as well as the duration of any motion or activity avoidance required.
FAQs
How can elbow discomfort be prevented?
One possible treatment for elbow discomfort is to perform the exercises that your physical therapist has recommended to progressively strengthen
the tendons.
massage with softer tissues.
massage with cold. acupuncture.
elbow bracing or taping.
While they can help you manage the discomfort, anti-inflammatories and painkillers don’t boost long-term results.
Does doing pushups help with tennis elbow?
If you have tennis elbow, though, you should absolutely stay away from this activity. Although pushups are meant to strengthen your shoulders, pectorals, and triceps, performing them will require you to often bend your elbows. This implies that the already damaged elbow tendons will be subjected to further stress.
How could tennis elbow be avoided?
Tennis Elbow Exercises You Should Avoid: Chin-ups, push-ups, and bench presses These workouts may put undue strain on your flexors, aggravating your tennis elbow and making it worse.
workouts for the wrist: A lot of wrist workouts might put additional strain on your elbow and forearm, aggravating your injury and prolonging the discomfort.
Is tennis elbow an appropriate use for Tiger Balm?
Which is better for treating tennis elbow discomfort at night: topical creams or pills? Applying a lotion, cream, or liniment on your elbows and forearms just before bed may also be beneficial. In particular, Tiger Balm, “IcyHot,” and other liniment-type products that “warm” the region by boosting circulation.
If you have tennis elbow, how do you sleep?
Have a restful night on your back.
Many people spend entire nights resting on their sides. Because this posture restricts blood supply to the damaged tendons, it can exacerbate the tennis elbow. Lying on your back reduces strain on your arm and facilitates faster healing as you sleep.
What is the quickest at-home treatment for tennis elbow?
Tennis elbow may be relieved by the self-care techniques listed below:
Relax. Avoid doing anything that makes your elbow ache worse.
painkillers. Try over-the-counter pain medicines such as naproxen sodium (Aleve) or ibuprofen (Advil, Motrin IB, etc.).
Ice. Three to four times a day, use ice or a cold pack for fifteen minutes.
What can I apply to rub on my elbows?
Creams for Topical Use. It has been demonstrated that prescription-based anti-inflammatory lotions are useful in treating tennis elbow. For nerve pain, your pharmacist could even make a special combination that includes gabapentin and lidocaine. One effective method of avoiding the adverse effects commonly associated with oral drugs is to use a topical lotion.
Is a hot compress beneficial for elbow tennis?
Tennis elbow may also benefit from heat. Applying heat dilates blood vessels, which improves circulation. Providing the wounded region with new oxygen and nutrients can speed up the healing process. Several times a day, spend 15 to 20 minutes at a time using a heating pad or taking a warm bath.
What is the duration of tennis elbow?
The duration of tennis elbow might range from several months to over a year. The average recovery time is six months, however, some people require up to eighteen months.
Is it possible to relieve the tennis elbow?
Compresses that are heated or cooled, non-steroidal anti-inflammatory medicines (like Ibuprofen), and paracetamol can all help reduce inflammation and discomfort. Forearm deep tissue massage is a highly useful way to relieve tennis elbow and speed up the healing process compared to rest alone.
Is it possible to treat tennis elbow with exercise?
“The best way to heal tennis or golfer’s elbow is to exercise; once that’s done, you just need to relax and give it some rest,” said Chris Zarski, a clinical assistant professor at the Augustana Campus Faculty of Rehabilitation Medicine.
Is there a natural way to treat tennis elbow?
Eight tennis elbow exercises and preventative advice
The most common home remedies for tennis elbow are rest and over-the-counter (OTC) medications. Certain movements, such as towel twists, and wrist rotations, can also help reduce discomfort and stop it from coming back. It happens when someone strains their forearm tendons.
What causes tennis elbow?
The main cause of tennis elbow is overusing your forearm as a result of hard or repeated activities. It can also occasionally happen if your elbow is knocked or banged. Tiny rips and inflammation may appear in the vicinity of the bony bump (lateral epicondyle) on the outside of your elbow if the muscles in your forearm are stretched.
Which medication works the best for tennis elbow?
medications that reduce inflammation, including naproxen or ibuprofen. applying a compression bandage on your elbow.
What is the most effective tennis elbow treatment?
Tennis elbow non-surgical treatment: modifying activities.
injections of corticosteroids into the elbow joint.
Extracorporeal shock wave treatment delivers energy waves to injured elbow tissues under the guidance of ultrasonography.
Ice.
painkillers or anti-inflammatory drugs.
physical therapy and range-of-motion exercises.
References
- Rupapara, D. (2023, June 16). Tennis Elbow (Lateral epicondylitis) Cause, Symptoms, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/tennis-elbow-treatment-exercise/
- Dhameliya, N. (2023, July 24). Tennis Elbow. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/tennis-elbow/
- Physiotherapist, N. P. (2023, June 10). Lateral Epicondylitis : Cause, Symptoms, Diagnosis, Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/lateral-epicondylitis-tennis-elbow-physiotherapy-management/
- Lateral Epicondylitis. (n.d.). Physiopedia. https://www.physio-pedia.com/Lateral_Epicondylitis
- Professional, C. C. M. (n.d.). Tennis Elbow (Lateral Epicondylitis). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/7049-tennis-elbow-lateral-epicondylitis




7 Comments