Midfoot Sprain
Introduction:
A midfoot sprain occurs when the ligaments that support the middle section of the foot, known as the midfoot, are overstretched or torn. This area plays a crucial role in stabilizing the arch of the foot and supporting proper movement during activities like walking, running, and jumping.
Midfoot sprains can range from mild to severe, often resulting from trauma, sudden twisting, or direct impact on the foot. Individuals with a midfoot sprain may experience pain, swelling, and difficulty bearing weight, requiring proper diagnosis and treatment to avoid long-term complications.
Sudden twists, falls, overuse, and high-impact activities can all cause this injury. While severe cases may necessitate surgery and prolonged rehabilitation, milder cases may only require rest and conservative care.
What is a Midfoot sprain?
Although a midfoot sprain may start out mildly, instability caused by damaged ligaments could make the injury worse.
It is a typical injury sustained while participating in sports, particularly those involving cutting and twisting. Watch live sports on the internet
These injuries are frequently misdiagnosed because they can be significantly more complex than straightforward sprains. It may require surgery if multiple bones and/or ligaments are affected, be quite serious, and take months to heal. This injury could be anything from a little strain on a ligament to a fractured bone or dislocation of a joint.
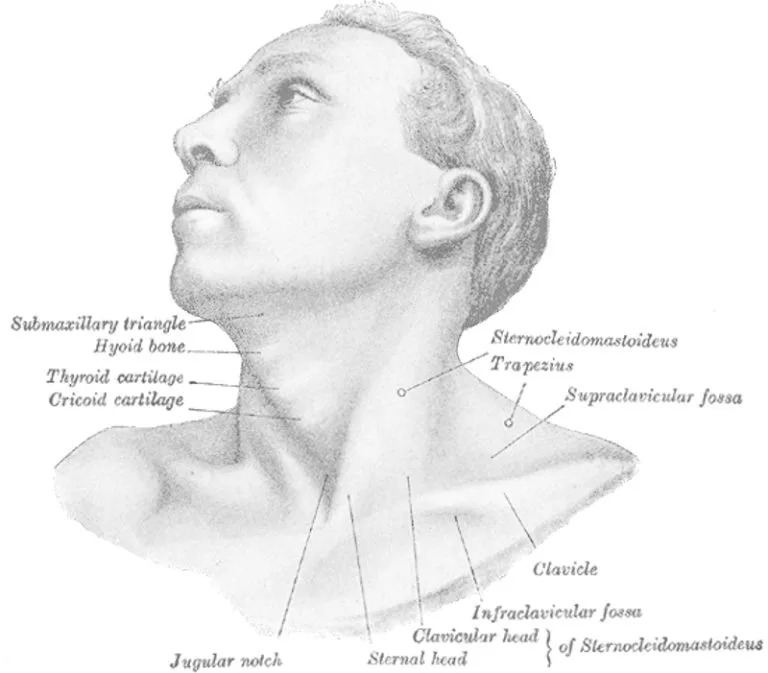
Relevant Anatomy of a Midfoot Sprain:
It is made up of a variety of bones, joints, ligaments, and muscles that cooperate to support different bodily processes.
Bones:
There are multiple bones that make up the midfoot, including:
- Cuboid Bone and Navicular Bone
- The medial, intermediate, and lateral cuneiform bones
- Talus Bone: a component of the midfoot joint although belonging to the hindfoot.
Joints:
- Chopart’s Joint (also known as the Calcaneocuboid and Talonavicular Joints): This joint allows for side-to-side movement and connects the hindfoot to the midfoot.
- Lisfranc’s Joint (Tarsometatarsal Joints): This joint, which joins the midfoot and forefoot, is important in maintaining the foot’s arch.
Mechanism of Injury:
This kind of injury usually happens as a result of an abrupt or powerful force that compromises the midfoot region’s stability. The following are some typical ways that midfoot sprains are caused:
- Twisting or Rotational Forces: This can happen when you rotate, make abrupt direction changes, or step on an uneven surface, for example.
- Direct Impact: Ligaments may be harmed as a result of the impact forcing the midfoot bones to shift in unnatural ways.
- Hyperflexion or Hyperextension: In addition to overreach, overbending, or forcefully extending the midfoot, these actions can also result in ligament damage.
- Falls: Excessive force can cause sprains to the midfoot if you fall from a height or land awkwardly on your foot. This is especially true if the foot hits with its toes pointed down, or plantarflexed, with force.
- Sports and Physical Activities: Playing high-impact sports like basketball, football, or soccer increases the risk of spraining the midfoot because of the combination of changing directions, cutting actions, and possible player collisions.
- Missteps or Tripping: The integrity of the ligaments may be compromised by the abrupt force exerted on the midfoot.
- Repetitive Stress: While less frequent, long-term overuse or repetitive stress on the midfoot such as from repetitive impact activities can weaken the ligaments and increase their vulnerability to injury.
They can be difficult to diagnose, and in order to determine the precise degree of the damage, imaging tests like CT or X-rays may be necessary.
What are the Causes of Midfoot Sprain?
Although they are not common, midfoot sprains can be severe and need to be treated right away.
- Trauma or direct impact: A midfoot sprain can result from a sudden, strong blow to the midfoot, such as that sustained in a sports collision, automobile accident, or fall. This is a frequent reason why sportsmen from contact sports, such as rugby or football, have Lisfranc injuries.
- Twisting or pivoting: Injured ligaments in the midfoot can be severely strained by quickly twisting or rotating the foot while it is firmly planted on the ground. Sports like basketball and soccer that need rapid direction changes are prone to this kind of injury.
- Falls from height: When a person falls from a considerable height and lands on their feet, the midfoot may be compressed and twisted, which can cause a sprain.
- Mistakes or tripping: If you trip over something or take a bad step, your foot may be forced into an abnormal position, which could harm your midfoot ligaments.
- Accidents during high-impact sports: If there is a fall or collision while participating in sports like skiing, snowboarding, or skating, it can occasionally result in midfoot sprains.
- Overuse or repetitive stress: This is especially true when engaging in activities like sprinting or jumping that require repeated pressure on the midfoot.
- Weak foot arches and ligaments: Due to decreased stability in the midfoot area, those with weak foot arches or lax ligaments may be more susceptible to midfoot sprains.
- Improper footwear: When engaging in vigorous activities, wearing shoes that don’t offer enough protection or support for the midfoot can raise the risk of injury.
- Sports: Generally, cutting and twisting foot motions like planting the foot during a rotation and push-off lead to injury.
Symptoms of Midfoot Sprain:
- Pain: In the center of the foot, moderate to severe pain frequently gets worse with pressure or movement. pain that worsens with movement and standing. If you push off with the injured foot, it can get worse, therefore you might require crutches.
- Swelling: It’s possible for the affected area to swell and appear bigger than the other foot.
- Bruising: Damage to the blood vessels in the midfoot may result in bruises or discolorations.
- Tenderness: There may be some tenderness in the midfoot region.
- Difficulty bearing weight.
- Reduced range of motion.
- Instability: It could be challenging to walk or stand on the midfoot because it feels weak or unsteady.
Risk Factors:
A number of variables can raise the risk of midfoot sprains, often known as Lisfranc injuries. Those who are aware of these risk factors may be able to lower their chance of suffering from injuries by taking preventative action.
- Sports and Physical Activities: Playing high-impact sports or engaging in physical activities that require sudden turns, leaping, or possible collisions raises the risk.
- Inappropriate Footwear: Midfoot injuries can result from wearing shoes that are too small or ill-fitting while engaging in physical activity. Shoes lacking adequate stability, cushioning, or arch support may not be able to shield the midfoot from abrupt blows or motions.
- Training Intensity and Technique: Inadequate warm-ups, abrupt increases in training volume or intensity, and poor training practices can all lead to midfoot problems. The risk of sprains rises when the foot is not appropriately prepared for the demands of an activity.
- Foot Alignment and Structure: People who have alignment problems or specific foot structures may be more vulnerable to midfoot injuries. For example, people with flat feet or high arches may have changed biomechanics that put more strain on the midfoot ligaments.
- Previous Injuries: Past foot injuries, particularly those that were not sufficiently healed, might weaken the midfoot’s ligaments and structures, increasing their vulnerability to sprains.
- Overuse and Fatigue: Excessive or repetitive activity that puts the foot under stress without adequate rest and recuperation can weaken the ligaments and raise the risk of injury. The ability of worn-out muscles and ligaments to support the foot properly is reduced.
- Factors related to the place of work: Prolonged standing, heavy lifting, and exposure to uneven surfaces are some jobs that can raise your risk of midfoot injuries. Those who spend a lot of time on their feet, such as construction workers and healthcare workers, are more susceptible.
- Age and Gender: Due to their participation in sports and other physical activities, younger, active people are more likely to sustain Lisfranc injuries. However, conditions like diminished flexibility and bone density may also put older people in danger.
- Accidents and Trauma: Traumatic events, including car crashes or falls from great heights, can apply abrupt, powerful stresses to the midfoot, increasing the chance of sprains.
- Insufficient Warm-Up: Inadequate warming up before physical activity can cause ligaments to become less flexible and stiff, which increases the risk of injury.
- Biomechanical Factors.
- Genetic Predisposition: Although the exact role that heredity plays in ligament laxity and overall foot anatomy is unknown, it may contribute to an increased risk of midfoot injuries.
Midfoot sprains can be prevented by addressing these risk factors, which include wearing the right shoes, escalating activity levels gradually, using the right training methods, and making sure to warm up properly. If you participate in activities that increase your chance of suffering a midfoot injury, you should think about getting advice from a physician regarding injury prevention techniques.
Classification of Midfoot sprain:
Numerous grading schemes, each with advantages and disadvantages of its own, can be used to grade ankle sprains.
The midfoot region, which is made up of a complicated combination of bones and joints, is where midfoot sprains occur when ligaments and tissues are injured. Medical practitioners may use several classification schemes, however the following is a broad overview:
Mild Grade 1 Midfoot Sprain:
- Tenderness and mild swelling are typical.
- little loss of stability or functionality.
Moderate Grade 2 Midfoot Sprain:
- partial tear in the ligamentous tissues.
- increased intensity of pain, bruising, and swelling.
- Moderate instability and function loss.
- can require physical therapy and a period of immobilization (such as wearing a brace or cast).
Severe Grade 3 Midfoot Sprain:
- Total rip or rupturing of the ligament(s).
- severe pain, bruises, and swelling.
- considerable loss of stability and functionality.
- frequently necessitates more intensive care, such as casting, potential surgery, and a lengthier recovery time.
Additionally, the location and type of midfoot sprain are described using particular terminology in certain classification systems:
- Lisfranc Injury: The fact that several joints and bones may be involved makes this injury potentially more complicated. It frequently calls for more meticulous diagnosis and management.
- Dorsal Midfoot Sprain: Usually caused by an abrupt hyperextension of the midfoot, this injury affects the ligaments on the top (dorsal) portion of the foot.
- Plantar Midfoot Sprain.
Differential Diagnosis:
Similar symptoms to those of a midfoot sprain (Lisfranc injury) can be caused by a number of disorders. To guarantee an accurate diagnosis and suitable treatment, it is crucial to take into account these possible differential diagnoses. To distinguish between these disorders, a medical practitioner will review your medical history, perform a physical examination, and order imaging tests. The following are some typical differential diagnosis for sprains of the midfoot:
- Midfoot Fractures: Midfoot sprains can be comparable in symptoms to fractures of the metatarsals, cuneiforms, or other midfoot bones. Differentiating between ligament injuries and fractures can be aided by X-rays and other imaging procedures.
- Midfoot Dislocations: Pain and instability may result from a whole or partial dislocation of the midfoot bones. It is possible that a dislocated bone has moved from its natural position, producing symptoms akin to a sprain.
- Stress Fractures: They could be misdiagnosed as sprain and produce localized pain.
- Tendon Injuries: Pain and swelling may result from injuries to the tendons in the midfoot, such as the peroneal tendons.
- Plantar Fasciitis: It may result in arch and heel pain that spreads to the midfoot.
- Tarsal Tunnel Syndrome: The midfoot area may experience tingling and soreness as a result of it.
- Morton’s Neuroma.
- Rheumatoid Arthritis.
- Gout: It may result in abrupt, severe pain that usually affects the big toe joint but may also affect the midfoot.
- Other Ligament Injuries: Similar symptoms can also be caused by injuries to ligaments located in locations other than the midfoot, such as the ankle ligaments.
- Nerve Compression.
- Bone Spurs: In the midfoot area, bone spurs or other bony growths can form and can be painful.
- Other Foot and Ankle Injuries: Ankle sprains and Achilles tendon injuries are examples of other foot and ankle ailments that can occasionally cause pain in the midfoot.
Diagnosis:
A midfoot sprain, sometimes referred to as a Lisfranc injury, can be diagnosed using a variety of methods, including imaging tests, clinical assessment, and even specialist consultation. A common diagnostic process for sprains of the midfoot looks like this:
Clinical Evaluation:
- Medical History: The physician will begin by discussing your symptoms, the way the injury occurred, and any relevant medical history.
- Physical Examination: The doctor will examine your foot carefully to search for any unusualities, pain, swelling, or bruises. We’ll also evaluate your range of motion and midfoot stability.
Imaging Studies:
- X-rays.
- CT Scan: The finely detailed cross-sectional pictures provided by CT scans can help make the bones and joints of the midfoot easier to see.
- Magnetic resonance imaging, or MRI.
Specialist Consultation:
- Orthopedic specialist: Depending on the severity of the injury and the intricacy of the case, you can be sent to an orthopedic or podiatric expert. Based on their experience, these professionals can propose courses of treatment and conduct additional assessments.
Diagnostic Considerations:
- Differential Diagnosis: It’s important to distinguish a midfoot sprain from conditions that may present with similar symptoms, such as fractures, dislocations, or other ligament injuries.
Special Tests:
Physical therapists commonly utilize a number of specialized tests to diagnose midfoot sprains and assess the extent of the injury. These tests are designed to elicit certain movements and sensations that can provide insight into the sort of damage. Keep in mind that the best individuals to do these tests are licensed healthcare professionals. A few common specific tests used by physical therapists to diagnose midfoot sprains are as follows:
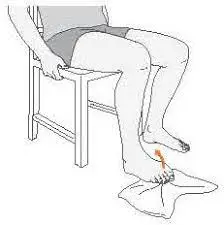
Midfoot Compression Test (Squeeze Test):
The midfoot area on both sides of the foot is compressed by the physical therapist. Pain or discomfort during this compression may be an indication of inflammation of the ligaments or joint capsule.
Midfoot Dorsiflexion Test:
The physical therapist elevates the forefoot gradually into dorsiflexion while holding the heel in place and directing the toes upward. Midfoot soreness or stiffness during this activity may be an indication of ligamentous or joint involvement.
Talar Tilt Test:
The physical therapist tests the heel for pain and excessive movement by placing the foot in a neutral posture and applying inversion and eversion forces.
Anterior Drawer Test:
This pushes the foot forward, requiring an examination of any unusual movement in the midfoot.
Plantarflexion and Dorsiflexion Range of Motion:
The midfoot ligament may be involved and have limitations when the range of motion for dorsiflexion raising the toes upward and plantarflexion pointing the foot downward is assessed.
Single Leg Balance Test:
This test measures the patient’s stability and strength in the midfoot area by having them balance on the foot that is affected.
Treatment
Medical Treatment:
Rest: To spare the damaged foot’s ligaments and tissues from more strain, avoid bearing weight on it.
Immobilization Devices: Immobilisation aids in healing, safeguards the wounded area, and stops more harm. For the right immobilization procedures and times, it’s crucial to adhere to the doctor’s instructions.
- Walking Boot: Walking boots are commonly used in the treatment of midfoot sprains. It offers greater support than a brace and allows for a gradual return to bearing weight as the healing process progresses.
Casting: To totally immobilize the foot and midfoot, a cast may be applied in certain situations.
Pain Management: Over-the-counter analgesics like acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) or naproxen (Aleve) can help with pain management and reduce inflammation.
Elevation: To help minimize swelling, raise the affected foot above the level of your heart when you are not moving. This may work especially well in the initial days following an accident.
Surgical Treatment:
For more serious midfoot sprains that involve fractures, substantial ligament injury, or joint instability, this intervention might be advised. Its choices could consist of:
- Ligament Repair or Reconstruction: To give the midfoot stability again, injured ligaments can be surgically repaired or rebuilt.
- Fracture fixation: The surgical implantation of screws, pins, or plates to stabilize damaged bones is known as fracture fixation.
- Joint Fusion: To stabilize the joint and lessen pain in cases of severe joint instability, fuse adjacent bones together.
- Tendon repair
Physical Therapy Treatment:
The following is the precise way that physical therapy can be used to treat a midfoot sprain:
Pain Management:
- Manual Therapy: To release muscular tension, mobilize joints, and relieve pain, the therapist may apply hands-on techniques.
- Modalities: To control pain and inflammation, modalities including ultrasound, electrical stimulation, or cold therapy may be employed.
Range of Motion Exercises:
After a sprain, range-of-motion (ROM) exercises are essential for maintaining flexibility and preventing midfoot stiffness.
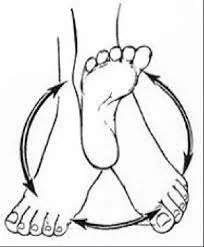
Ankle Circles:
Toe Flexion:
- Curl your toes slightly downward, like you’re trying to make a fist.
- Let go and unwind your toes.
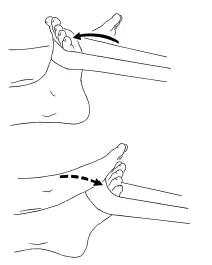
Plantar Flexion and Dorsiflexion:
- Plantar Flexion:
- Your toes will move apart from your body when you perform plantar flexion. Try standing on your toes.
Alphabet Writing:
“Alphabet toes,” also known as “toe writing” or “the alphabet,” are a simple and enjoyable foot exercise that improves the flexibility and dexterity of the toes. It’s a great method to strengthen your toe muscles, which will increase your feet’s functionality and range of motion. This exercise program encourages various stretches and actions of the midfoot.
- Try to complete the exercise slowly and thoughtfully to ensure that the toe muscles are fully engaged.
Calf Stretch:
- Stretch your leg muscles against the wall while facing it with your hands flat at shoulder height.
- Repeat the stretch with the other leg.
Strengthening exercises are essential to the healing process after a midfoot sprain since they help to stabilize the injured area, prevent more injuries, and preserve general foot health. Licensed physical therapists or medical professionals can oversee the incorporation of the subsequent strengthening exercises into your rehabilitation program:
Toe Raises:
- After a few seconds of holding the position, let go of your toes.
- After a number of repetitions, repeat.
Marble Pick-Up:
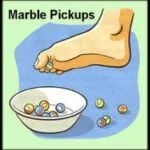
- You can perform the marble pick-up exercise in the following ways:
- While sitting in a chair, place a small dish or container on the ground in front of you that is filled with marbles or other little balls.
- Take off your shoes and socks so you can use your bare feet to grab the marbles securely.
- For five to ten minutes, or for whatever long it takes you to feel comfortable, keep picking up and moving the marbles.
Calf Raises:
- Calf lifts should be done as follows:
- Return your heels to the ground slowly. Execute a series of reps.
Ankle Band Resistance Exercises:
- Incorporate actions such as rolling the sole inward and outward, dorsiflexion (drawing toes towards you), and plantar flexion (pointing the toes down).
Short Foot Exercise:
- Pay attention to your right foot.
- Your foot should develop a slight arch as a result of this action because the muscles on the underside contract.
Towel Curl Exercise:
- Think about using your toes to try to curl the towel.
- Try to curl for at least ten to fifteen reps each time you perform this exercise.
Heel Walking:
- Heel walking is the practice of walking on your heels rather than your toes. Lift your toes off the ground. By concentrating on your calves, this exercise can help strengthen your feet.
Single-Leg Balance Exercises:
- Standing on one foot, maintain your balance. You can progress this exercise by closing your eyes or by making small movements, like raising your arms.
- Stand on one leg, keeping the other leg raised off the floor.
- After switching, repeat with the other leg.
Ankle Plantarflexion and Dorsiflexion Resistance Exercise:
- Theraband: Toes should first be pulled towards you (dorsiflexion) against the band’s resistance, and then progressively pointed away from the body (plantar flexion). This can support the midfoot indirectly by strengthening the muscles that govern ankle mobility.
Ankle Inversion and Eversion Resistance Exercise:
Ankle Eversion:
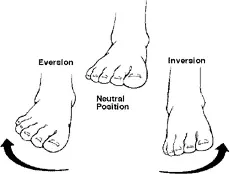
- Slowly evert your foot (move it outward) against the resistance of the band, keeping your heel on the ground.
Ankle Inversion:
- Seated on a chair or flat surface, spread your legs wide in front of you.
- While pointing your toes straight ahead, keep your gait composed.
- Feel the muscles surrounding your ankles contract as you maintain an inward stance.
Toe Spreading:
- Spread your toes apart consciously, as though you were trying to make as much space as possible between them, to begin expanding them.
- The toe-spreading motion must be done again.
Proprioception and Balance Training:
Because proprioception and balance training improve the general function, stability, and coordination of the injured foot, they are crucial components of the rehabilitation process for a midfoot injury. Proprioception is the capacity of your body to sense its position in space and the relative positions of its parts, even in the absence of visual cues. After a midfoot sprain, the proprioception and balance exercises listed below can aid in the healing process:
Single Leg Stance:
- Here’s how to strike the one-leg pose:
- Select One Leg: First, select one leg.
- Keep your balance on the supporting leg.
- hold onto the pose: For as long as you can stand on one leg comfortably, try to maintain this position for 20 to 30 seconds.
- Change Legs: Before tackling the other leg, return the lifted leg to its original position.
Balance Board or Wobble Board Exercises:
First, stand on the board using both feet. Strength and stability can be enhanced by using the muscles surrounding the midfoot, which are activated by the board’s instability.
- Basic Balance:
- Rocking side to side:
- Front-Back Rocking:
Slightly lean forward to make the board tilt forward, then straighten back up.
The board will tilt back when you lean back, but it will then straighten again.
Maintaining balance, repeat the front-back rocking action. - Rotational Movements:
Heel-to-Toe Walk:
- Take 20 to 30 steps ahead, paying attention to your posture and balance, and then turn around to go back to where you started. This exercise tests your ability to walk with a limited base of support and enhances balance and coordination. Your proprioception and balance are tested by this.
Calf Raises on an Unstable Surface:
- This improves your balance and uses your stabilizing muscles, making the workout harder.
- Using your calf muscles, raise your heels for a brief while before lowering them again.
- Because the uneven surface makes it harder for your muscles to keep their balance during the exercise, calf raises are superior for building muscle and improving balance.
- Start with a hard surface if you’re new to calf raises, and then gradually increase the height.
Squatting on an Unstable Surface:
- This variation on the squat workout works your core muscles and requires more balance and coordination by adding an element of instability.
- In order to perform a squat on uneven ground, bend your knees and lower your hips while keeping your balance.
- Press your heels on the ground in order to stand again.
- If you’re not familiar with squats or unstable surfaces, start with a solid surface and work your way up to the unstable surface as you become more comfortable and confident.
Toe Tapping:
- This exercise tests your proprioceptive awareness and foot control.
- After a little break, tap your toes once more.
Lateral Hops:
- If necessary, use a resistance band for support. With your damaged foot, hop laterally (side to side) while keeping your balance and control. Lateral hops are quick side-to-side leaps with smooth landings on both feet. Step laterally, starting with your feet hip-width apart, and repeat for a couple of sets, 10 to 15 repetitions per side. Maintain your core active and concentrate on deliberate motions.
Single-Leg eyes Closed Balance:
- Your body is forced to rely only on proprioception and muscle control as a result of the removal of visual cues.
- Maintaining your focus on the focal point, carefully raise your selected foot off the ground.
- To further assess your balance, if you feel comfortable doing so, consider raising your arms above your head or extending them to the sides.
- Examining Your Gait:
Exercises for improving gait that you might include in your recovery regimen for a sprained middle foot. The goals of these exercises are to restore normal biomechanics and enhance your gait. Before beginning any new workouts, as always, speak with your doctor or physical therapist, particularly if you have an ailment like a midfoot sprain. - Heel-to-Toe Rocker:
People who have midfoot sprains or injuries such as metatarsal fractures are frequently advised to wear a heel-to-toe rocker sole. This kind of shoe design can facilitate healing by lessening the strain and motion on the midfoot region, resulting in a more pleasant and seamless gait.
Place your feet hip-width apart and stand erect. Start with a little swaying motion from your heels to your toes. - Step-Ups:
Look for a platform or low step. Step back down using the foot that is hurt first, then the foot that is not affected. This workout enhances strength and coordination for climbing and descending curbs or steps. - Mini Lunges:
Lower your body by bending both knees. Maintain the front knee above the ankle. Repeat on the other side. Start off by performing a few reps on each leg. - Slow-Motion Walking:
- Marching in Place:
While standing still, raise your knees to a high position like you’re marching. Instead of dragging your feet on the ground, concentrate on raising them from the midfoot area. - Balance on One Leg:
Raise your damaged foot just a little bit off the ground while standing on your uninjured foot. Proprioception and stability are enhanced by this workout. - Tandem Walking:
Your coordination and balance will be challenged during this workout. - Backward Walking:
This exercise can support the maintenance of good foot mechanics and placement. - To get the most outcomes from your physical therapy program, you must be committed and consistent. Maintaining contact with your physical therapist, following their instructions, and sharing any updates or worries can help guarantee a full recovery from your midfoot sprain.
FAQs
How can I lessen my chance of being hurt again when my midfoot sprain heals completely?
Reducing the risk of re-injury can be achieved by wearing appropriate footwear, warming up before physical activity, maintaining strong foot and ankle strength, and using proper form throughout exercises.
When may I resume my usual exercises and sports following a midfoot sprain?
Timing for returning to activities varies according to the extent of the injury and your personal development. When it’s safe to continue particular activities, your physical therapist or healthcare practitioner will offer advice.
Is it possible to recover from a midfoot sprain by self-myofascial release or massage?
Myofascial release methods combined with a light massage can help reduce muscle tension and increase blood flow. Before beginning any self-treatment, though, speak with your physical therapist and refrain from applying direct pressure to the damaged area.
What signals of recovery are present when recovering from a midfoot sprain?
Reduced pain, better range of motion, decreased edema, and enhanced strength and stability in the damaged foot are all possible indicators of improvement.
Can someone who has a midfoot sprain still exercise or participate in sports?
Generally speaking, it’s advised to stay away from sports and high-impact activities that place undue strain on an injured foot while it heals.
When should I get help if I think I may have a sprain of the midfoot?
It’s vital to get medical help as soon as possible if you have severe pain, swelling, bruising, or trouble walking following a midfoot injury to guarantee a proper diagnosis and course of treatment.
Can I avoid getting midfoot injuries again?
Even while mishaps still happen, you may lessen your chance of getting a midfoot injury in the future by wearing appropriate shoes, warming up before exercise, strengthening your ankle and foot muscles, and using the correct form when performing exercises and other physical activities.
Even with a midfoot sprain, can I walk?
When you can resume regular walking how much weight you can put on the damaged foot will be determined by your healthcare professional.
After suffering a midfoot sprain, when can I begin exercising?
Early in the rehabilitation phase, you may start non-weight-bearing workouts and mild range-of-motion exercises after you are cleared.
What kind of care is usually given for a sprain of the midfoot?
RICE (rest, ice, compression, and elevation) is a common treatment strategy that includes immobilization using a brace or cast. Other common elements of treatment include pain management, physical therapy, and a gradual return to weight-bearing activities.
How do you identify a midfoot sprain?
A medical practitioner, who specializes in sports medicine or orthopedics, can identify a midfoot sprain by performing imaging tests such as MRIs or X-rays, reviewing your medical history, and performing a physical examination.
References
- Patel, D. (2023b, August 13). Midfoot Sprain – Cause, Symptoms, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/midfoot-sprain/
- SportsMD. (2024, August 12). Midfoot Sprain | Diagnose, treatment, and surgery options | SportsMD. https://www.sportsmd.com/sports-injuries/foot-ankle-injuries/midfoot-sprain/