Dyspnea (Shortness of Breath)
Dyspnea (Shortness of Breath) refers to a sensation of difficulty or discomfort in breathing. It can be caused by various conditions, including lung diseases (like asthma or COPD), heart problems, anxiety, or high-altitude exposure.
The severity ranges from mild to severe and may be acute or chronic. Proper diagnosis and management depend on identifying the underlying cause.
Dyspnea: What is it?
Healthcare professionals use the term dyspnea, which is pronounced DISP-nee-uh, to refer to feeling out of breath. You could characterize it as chest tightness, difficulty in breathing, or an inability to acquire enough air (air hunger).
Breathlessness is often an indication of heart and lung problems. But it could also be a sign of other conditions including asthma, allergies, or nervousness. Breathlessness can also be caused by a cold or vigorous exercise.
Dyspnea on exertion:
The feeling of running out of air and not being able to breathe quickly or deeply enough while exercising is known as dyspnea on exertion.
What distinguishes shortness of breath from dyspnea?
Shortness of breath and dyspnea are interchangeable. Dyspnea is the medical name for the sense of not being able to receive enough air.
Mechanism
The respiratory system‘s inappropriate reaction to unrestricted motor control is the first cause of dyspnea.
Dyspnea appears to be caused by the activation of sensory systems related to breathing. The final appearance of the evoked sensation is shaped by environmental, cognitive, and behavioral factors as well as central processing of respiratory-related signals after sensory information has been transmitted to higher brain centers.
A framework for understanding the mechanisms of dyspnea is provided by the homeostatic systems involved in the regulation of respiration.
Both the limbic system and the brain are probably involved in the neural basis of dyspnea.
Dyspnea has a significant emotional component and is characterized by an elevated awareness of respiratory feeling.
Dyspnea can occur in healthy persons in a variety of circumstances, such as high altitudes, after holding their breath, in stressful situations that create anxiety or panic, and most frequently during intense activity.
The mechanisms of dyspnea are influenced by a number of elements, including central motor output, mechanical and chemical afferents, and the functional state of the breathing muscles.
Types of Dyspnea:
It can be Acute or Chronic.
The duration and onset phases of acute and chronic dyspnea are different. Their causes are distinct.
Acute dyspnea
Acute dyspnea can happen unexpectedly and lasts for a short time (hours to days). Acute dyspnea can be caused by allergies, worry, physical activity, and illnesses like the flu or the common cold.
Acute dyspnea can also be caused by serious illnesses including a heart attack, a blood clot (pulmonary embolism), or acute airway restriction (anaphylaxis).
Chronic dyspnea
Breathlessness that persists for a long period of time (weeks or more) or occurs frequently is known as chronic dyspnea. Chronic dyspnea can be caused by long-term medical disorders such COPD, heart failure, and asthma.
Because your muscles are attempting to obtain more oxygen, not getting enough exercise might also lead you to feel out of breath all the time.
Dyspnea occur in various positions:
Orthopnea
It is the feeling of dyspnea while lying down, which is relieved by standing or sitting.
Paroxysmal Nocturnal Dyspnea (PND)
It is a dyspnea sensation that usually occurs after one or two hours of sleep and disappears when the patient is upright.
Trepopnea
It is a sensation of dyspnea that occurs more commonly in one lateral decubitus position than the other.
Platypnea
It is a type of dyspnea that is relieved by lying down immediately after standing.
Symptoms
Shortness of breath, or dyspnea, can be caused by exerting oneself excessively, spending time at high elevations, or being a sign of a number of illnesses.
A person may exhibit the following symptoms of dyspnea:
- Breathlessness following work or strained breathing
- Chest tightness and shallow, fast breathing
- Heart palpitations and sensations of suffocation or choking
- Coughing and wheeze
Dyspnea may indicate a dangerous medical disease if it happens quickly or if the symptoms are severe. Dyspnea emergency symptoms can include:
- Significant breathing difficulties,
- A heavy chest pain radiating to the arms, back, neck, and jaw, pale, blue, or gray lips or skin, and Sudden confusion
Causes of Dyspnea
A person’s health does not necessarily have a direct correlation with a dyspnea episode. When traveling to a high altitude or experiencing significant changes in temperature, a person may have dyspnea following vigorous activity.
Dyspnea, however, is typically associated with medical issues. Sometimes the symptoms are simply the result of inactivity, and exercise might help. Dyspnea, however, may indicate a more serious medical condition.
Shortness of breath is an acute case of dyspnea if it occurs suddenly.
Acute dyspnea may result from:
- Anxiety
- Asthma
- Pneumonia
- Heart conditions
- Airway obstruction by foreign items, allergic reactions
- Acute onset weakness, such as iron insufficiency, anemia, and exposure to harmful carbon monoxide levels
- Heart failure
- Low blood pressure is known as hypotension.
- A blood clot in an artery leading to the lung is known as a pulmonary embolism or collapsed lung.
- Multiple sclerosis and hiatal hernia
People who have a terminal illness also frequently experience dyspnea. A person is said to have chronic dyspnea if they have shortness of breath for more than a month.
Chronic dyspnea may result from:
- Asthma
- Chronic obstructive pulmonary diseases
- Obesity
- Heart problems such as pericarditis or cardiomyopathy
- Interstitial pulmonary fibrosis, which causes scarring of lung tissues
- Pneumonia
- Lung cancer
- Sarcodiosis
- Pulmonary hypertension
- Tuberculosis (TB)
- Blood clot
- Choking
- Partial or collapsed lung
Complications
- Low blood oxygen levels, or hypoxia or hypoxemia, can be caused by dyspnea. Reduced consciousness and other serious symptoms may result from this.
- A person may suffer from temporary or permanent cognitive impairment if they frequently experience hypoxia.
Prevention
Shortness of breath can be prevented by:
- Together with your provider, create a care plan and follow it to manage any underlying conditions.
- This covers the kind of drugs you should take methods of exercise, breathing techniques, and any other therapies your doctor may recommend.
- Stay away of substances like paint fumes and vehicle exhaust that might irritate your lungs.
- Using relaxation methods or breathing exercises.
- Not smoking.
- Keeping your weight within a healthy range.
- Avoid activities in extremely hot or cold temperatures or when there is a lot of humidity.
- Look for air pollution (ozone) alerts if you have lung disease; these are typically included in the Weather forecast.
- Stay clear of the outdoors during periods of heavy air pollution.
Scales for Dyspnea
Three scales are there:
- MRC Scale
- Modified borg scale or RPE
- American Thoracic Society(ATS)
The MRC Dyspnea Scale
The degree of baseline functional limitation by dyspnea is measured using the mMRC (Modified Medical Research Council) Dyspnea Scale.
When describing baseline dyspnea in individuals with respiratory conditions like COPD, it is helpful.
The scores are variably related to patients’ views of the burden of respiratory symptoms, even if they have a considerable correlation with other healthcare-associated morbidity, mortality, and quality of life scales (especially in COPD).
It is a part of the BODE Index, which forecasts negative outcomes like hospitalization risk and mortality. The scale is simple to use and effective.
The grades based on the mMRC breathlessness scale are 0–4.
MRC Dyspnea Scale
Description Grades
I only get breathlessness with strenuous exercise – 0
I get short of breath when hurrying on level ground or walking up a slight hill – 1
On level ground, I walk slower than people of my age because of breathlessness,
or I have to stop for breath when walking at my own speed on the level – 2
I stop for breath after walking about 100 yards or after a few minutes on
level ground – 3
I am too breathless to leave the house or I am breathlessness when dressing/
undressing – 4
Modified Borg Scale or Rating of Perceived Exertion (RPE)
An outcome measure scale called the Rating of Perceived Exertion (RPE) is used to measure exercise intensity without depending on physiological indicators like heart rate, lactate levels, or peak O2 uptake. Rehab specialists frequently utilize RPE to help prescribe exercises.
For the purpose of rating exertion, dyspnea, and exhaustion during physical exercise—that is, the degree of difficulty of the activity as indicated by heart and respiratory rate, excessive perspiration, and muscle exertion—Gunnar Borg created the Borg RPE scale .
The scale is also used to track exercise habits and progress in patient populations, such as those recovering from neurological, pulmonary, and cardiac conditions.
The range of the original Borg scale is 6–20. It is highly correlated with one’s heart rate, and the training heart rate at the moment of scoring is obtained by multiplying each value by 10. The modified Borg Dyspnea Scale is a variant of the Borg CR-10 Scale, which was subsequently reconstructed to a category (C) ratio (R) scale of 0–10.
It is mostly used to evaluate the severity of musculoskeletal discomfort, chest pain, and dyspnea. The CR-10 scale works best when measuring a particular bodily sense, like muscle soreness or exhaustion, or pulmonary reactions, like tightness in the chest or dyspnea.
Throughout the activity, participants are asked to rate their level of exertion on a scale that accounts for physical stress and exhaustion. Leg discomfort or dyspnea are ignored in preference to concentrating on the overall impression of exertion.
This number indicates the activity intensity level, enabling the individual to increase or decrease their activity rate. The scale can be self-administered or delivered by a researcher before and after the person has exerted themselves. It takes a short while to finish.
- 0 Nothing at all
- 0.5 Extremely Slight
- 1 Very slight
- 2 Slight
- 3 Moderate
- 4 Somewhat severe
- 5 Severe
- 6
- 7 Very severe
- 8
- 9 Extremely severe
- 10 Maximal
Diagnosis
Your healthcare practitioner will conduct a physical examination, which includes taking your blood pressure and using a stethoscope to listen to your lungs in an attempt to determine what is causing your dyspnea. To measure the amount of oxygen in your blood, they will place a sensor on your finger.
They may also do other testing, like:
- Chest X-rays, CT scans, and other specialized imaging techniques. Your doctor can use photos of the inside of your chest to assess whether you have a lung issue.
- Blood examinations: Your healthcare provider may use blood tests to look for anemia or other illnesses.
- Tests of lung function: Tests that measure your respiratory health.
- Tests for cardiovascular exercise: For this test, your healthcare professional will have you use a stationary bike or treadmill. The tests can tell your doctor how much carbon dioxide you exhale and how much oxygen you breathe in when exercising.
Differential Diagnosis
One of the primary symptoms is dyspnea. Respiratory, cardiac, neuromuscular, psychogenic, systemic sickness or a mix of these are the four main groups from which it has emerged.
Respiratory conditions include aspiration, pneumonia, pulmonary embolism, lung cancer, asthma, pneumothorax, and acute or chronic exacerbation of congestive obstructive pulmonary disease (COPD).
Acute coronary syndrome, pulmonary edema, pericardial a blockage, valvular heart defect, pulmonary hypertension, cardiac arrhythmia, congestive heart failure, or intracardiac shunting are all signs of cardiovascular
Massive chest trauma with a fracture or instability Neuromuscular disorders include obesity, kyphoscoliosis, spinal cord or central nervous system (CNS) dysfunction, paralysis of the phrenic nerve, myopathy, and neuropathy.
Foreign body aspiration, vocal cord dysfunction syndrome, hyperventilation syndrome, and psychogenic dyspnea are examples of psychogenic causes.
Anaemia, abrupt renal failure, metabolic acidosis, thyrotoxicosis, liver cirrhosis, anaphylaxis, sepsis, angioedema, and epiglottitis are examples of systemic disorders.
Treatment
The following are the treatment:
Medical Treatment
- Medicine: Asthma and COPD patients are offered bronchodilators, which are inhaled medications that relax the airways. Breathlessness may be improved by taking medication for pain or anxiety.
- Oxygen treatment: Your doctor will prescribe additional oxygen if your blood oxygen level is extremely low. Through a tube or mask, it enters your nose..
Physical Therapy Treatment
Exercise: Regular exercise will lessen the strain on your heart and lungs if you exercise often.
Relaxation techniques: You and your healthcare practitioner can practice breathing techniques and relaxation techniques. These can alleviate anxiety and dyspnea caused by underlying respiratory disorders.
- Walking
- Cycling
- Aerobic exercise
- Diaphragmatic Breathing
- Training using resistance exercises( Upper and lower limb)
Patients with a flat diaphragm may benefit from poses that use pressure from the abdominal contents to dome the muscle. Many breathless people find that self-posture helps them breathe.
In order to maximize accessory muscle function, the arms are best supported without tension or active fixation.
Pursed lip breathing improves physical function and exertional dyspnea over time while also relieving dyspnea and boosting exercise tolerance.
Dyspnea relieving position:
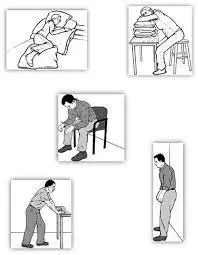
- High side-lying.
- Many people find that sitting up straight in a chair with arms to support them makes breathing easier than lying in bed.
- While some people prefer to lean forward slightly to expand the diaphragm, others prefer to lean back for support.
- Leaning forward from the waist, with feet on the floor and arms resting on table pillows
- Standing comfortably, arms resting on a support, such a window wall, and bending forward.
- Standing calmly, legs slightly apart, leaning back against a wall.
- If the auxiliary muscles require assistance, stand comfortably with your arms in your pockets and lean sideways against a wall.
- Sometimes the pressure of the contents of the abdomen against the diaphragm makes lying flat helpful. Some people may benefit from a small head-down tilt.
FAQs
What is dyspnea’s primary cause?
Acute myocardial ischemia, heart failure, cardiac tamponade, bronchospasm, pulmonary embolism, pneumothorax, pulmonary infection in the form of pneumonia or bronchitis, or upper airway blockage due to aspiration or allergy are the most frequent causes of acute dyspnea.
Is dyspnea fluctuating?
Dyspnea is the medical word for breathing difficulties or shortness of breath.. It is a sign of numerous respiratory system-related disorders.
Is it possible to treat dyspnea?
Treating the underlying illness or condition is the first step in treating dyspnea. For instance, removing fluid from the chest can lessen dyspnea if it is caused by a pleural effusion. Dyspnea may occasionally be treated with medicine or surgery, depending on the underlying reason.
Does oxygen help with dyspnea?
We observed that breathing difficulties can be somewhat relieved by oxygen. Oxygen must be administered during exercise in order to be effective. The majority of research assessed oxygen administered in a lab setting during exercise testing. Daily oxygen therapy did not significantly alter the quality of life of patients and had unclear effects on dyspnea.
Which neurological conditions can produce dyspnea?
The breathing mechanism is affected differently by various disease conditions of the nervous system since the respiratory center is located in the brain. Stress, anxiety, strokes, panic episodes, tumors, traumas, encephalitis, and impaired cerebral circulation are among the conditions that frequently cause dyspnea.
For shortness of breath, is there an inhaler available?
One class of medication known as a bronchodilator includes salbutamol. It facilitates easier breathing by relaxing the muscles that control the lungs’ airways.
References
- Dresden, D. (2025, January 27). What is dyspnea? https://www.medicalnewstoday.com/articles/314963
- Professional, C. C. M. (2024a, May 1). Dyspnea. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/16942-dyspnea
- MRC Dyspnea Scale | Primary Care Respiratory Society. (n.d.). https://www.pcrs-uk.org/mrc-dyspnoea-scale







3 Comments