Asthma
What is Asthma?
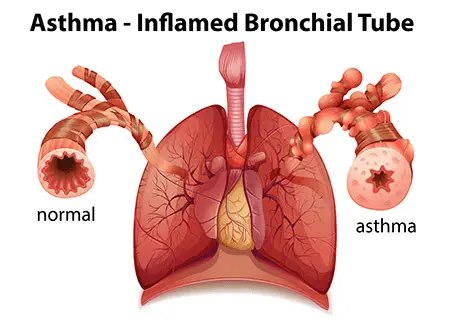
Asthma, often known as bronchial asthma, is a lung condition. Excess mucus causes your airways to swell, narrow, and become obstructed. These symptoms can be treated with medication. Since it is a chronic (ongoing) disorder, it requires constant medical attention.
Currently, about 25 million Americans suffer from asthma. Over 5 million youngsters are included in this total. If you don’t receive treatment, asthma can become fatal.
When irritants, dust, pollen, or other particles are breathed into the lungs, the bronchioles constrict and generate mucus, which in turn limits the supply of oxygen to the alveoli. It is distinguished by reversible airflow restriction, easily induced bronchospasms, and fluctuating and recurrent symptoms. Shortness of breath, chest tightness, coughing, and wheezing bouts are among the symptoms. A couple of times a day and a few times a week, these might happen. Depending on the individual, exercise or the night may exacerbate asthma symptoms.
It is believed that both environmental and genetic factors contribute to asthma. Allergens and air pollution exposure are examples of environmental influences. Medications like beta blockers and aspirin are also possible factors. Spirometry lung function testing, the pattern of symptoms, and the patient’s reaction to treatment over time are typically used to make the diagnosis.
The frequency of volume of forced expiration in a single second, or FEV1, symptoms and the maximum expiratory flow rate are used to categorize asthma. It can also be categorized as either atopic or non-atopic, with atopy denoting a tendency to experience an allergy 1 hypersensitivity reaction.
Related conditions
In addition to asthma, patients with asthma are more likely to have rhinosinusitis, obstructive sleep apnea, and gastroesophageal reflux disease (GERD). Additionally, psychological illnesses are more prevalent , with mood disorders accounting for 14–41% and anxiety disorders for 16–52% of cases.
Whether psychological issues create asthma or asthma causes psychological issues is unknown.
Increased mortality from heart disease, chronic lower respiratory tract disease, and all causes is linked to current asthma but not to past asthma. The occurrence of chronic obstructive pulmonary disease (COPD) is closely linked to asthma, especially severe asthma. People with asthma are more likely to experience radiocontrast responses, particularly if their condition is inadequately managed.
Pathophysiology
Over the last ten years, our knowledge of the pathogenesis of asthma has grown. The inflammatory component is crucial to the pathophysiology of symptoms in this bronchial hyperactivity disease.
Airway inflammation and an abnormal buildup of cells that are inflammatory in the bronchioles are the hallmarks of asthma. Increased tracheobronchial tree response to a wide range of stimuli, either alone or in combination, is linked to asthma. In addition to bronchospasm, inflammation of the airways, mucosa edema, and mucus plugging, there is an increase in expiratory resistance. Air trapping, more dead space, or hyperinflation result from this.
A personal or familial history of allergic conditions including urticaria, rhinitis, or eczema is often linked to extrinsic or allergic asthma. A personal or family history of allergies is not linked to nonallergic or intrinsic asthma. There is typically no external etiology identified for intrinsic asthma. Nonallergic asthma usually has normal serum immunoglobulin E type.
Various environmental allergens, dust mites, pollen, molds, animal dander, occupational substances, smoking, cold air, exercise, sinus diseases, emotional factors, widely upper respiratory infections, and medications like aspirin, nonsteroidal anti-inflammatory drugs, or beta blockers are some of the stimulation or triggers of asthma attacks.
Asthma has both a early and late response. In asthma, a trigger starts the inflammatory response in the airways. These triggers have the potential to activate local airway mast cells and induce immunoglobulin E cross-linking on a mast cell surface after inhalation. Histamine will be released as a result, and prostaglandins, leukotrienes, and other enzymes will be produced. At the same time, the lung will receive signals from other inflammatory cells and their mediators through cytokines produced by the mast cell.
Wheezing, bronchospasm, mucus secretion, increased vascular permeability, and airway inflammation are the outcomes. Because they happen in a matter of minutes, these occurrences are known called the early asthmatic reaction. Bronchospasm is a key element of the early reaction.
Hours pass before the late asthmatic reaction occurs. It is caused by numerous inflammatory cells that keep the inflammation going. T cells are a significant subset of inflammatory cells.
Chronically engaged T helper cells may be exposed to a range of allergenic antigens from antigen-presenting cells. The local inflammatory reaction is then maintained and exacerbated by the numerous cytokines secreted by these cells. The cytokines produced by the T cells will cause a response from numerous other inflammatory cells, such as mast cells and eosinophils. Cytokines, which are produced by these inflammatory cells, intensify the inflammatory reaction and the cellular response.
Inflammatory cells are migrating into the circulation into the submucosa of the airways and the pulmonary vasculature. The arachidonic acid pathway, which produces leukotrienes, is essential to both the inflammatory process and its management.
In order to treat asthma, it is clinically important to comprehend the differences between early and late asthma. At different stages of the disease process, other treatments might work better. Beta-2 agonists are expected to be most beneficial in the early response to asthma because they will stabilize mast cells. In the late asthmatic response, corticosteroids and leukotriene antagonists work better because of their anti-inflammatory properties.
Increased airway resistance, reduced maximum expiratory flow, air trapping, elevated airway pressure, hypoxemia, hypercarbia, pulsus paradoxus, and respiratory exhaustion and failure are all symptoms of airway blockage.
Forms of asthma:
- Asthma allergies
- Asthma that is not allergic
- Seasonal asthma
- Asthma at work
- Asthma induced by exercise
- Having trouble breathing
- Severe asthma
- Asthma eosinophilic
- Childhood asthma
- Adult-onset asthma
Asthma allergies
Allergens such as dust mites, pollen, and pets can cause allergic asthma. Atopic asthma is another name for it. Allergies affect about four out of five asthmatics.
To determine whether you’re allergic to any common allergens, a skin prick or blood test may be performed if you have been diagnosed with asthma. You will gain a better understanding of what triggers your asthma.
In addition to having allergy triggers for their asthma, many people also have non-allergic causes, such as cigarette smoke and chilly temperatures.
Asthma that is not allergic
Asthma that isn’t caused by an allergen, such as dust mites or pollen, is referred to as non-allergic asthma or non-atopic asthma. Compared to allergic asthma, it is less prevalent. Non-allergic asthma affects about 1 in 5 asthmatics. Asthma that is not allergic frequently appears later in life.
You may have non-allergic asthma if allergens such as dust mites, pollen, or dogs do not appear to trigger your asthma. The following can cause non-allergic asthma:
- colds,
- flu,
- chest infections,
- stress,
- recreational substances,
- cigarette smoke, and
- air pollution.
Asthma in season
Some people only have symptoms of asthma during specific seasons, such hay fever season or cold weather. This is sometimes called “seasonal” asthma.
It’s crucial to stick to your asthma action plan and use your preventer inhaler as directed, even if your symptoms only appear during specific seasons of the year.
Your doctor or nurse can recommend an AIR treatment plan if you only require assistance with managing your asthma during specific seasons of the year.
You can better control seasonal stressors like pollen and weather by following our suggestions.
Asthma at work
Asthma caused by exposures at work is known as occupational asthma. Occupational asthma affects roughly 10% of adults who acquire asthma.
You may have asthma related to your job if:
Your symptoms of asthma began when you were an adult, and they get better on the days when you’re not working.
Numerous factors can contribute to occupational asthma. For instance, latex may be a trigger if you work in the medical field, while flour dust may cause symptoms if you work in a bakery.
Asthma caused by exercise
9 out of 10 asthmatics experience airway tightness as a result of exercise. We refer to this as bronchoconstriction. It can also happen to persons without asthma.
Bronchoconstriction symptoms may appear during or after physical activity. Among them are:
breathing difficulties, coughing, wheezing (a whistling sound made during breathing), and a constricted chest.
Having trouble breathing
Asthma that necessitates high dosages to manage symptoms is referred to as difficult asthma. Difficult asthma affects about 1 in 5 persons with asthma. It is sometimes referred to as difficult-to-treat or difficult-to-control asthma.
For the majority of patients, asthma symptoms can be reduced with proper management. This implies:
Using an asthma action plan and taking your preventer or MART inhaler as directed each day will help you know what to do in the event that you experience asthma symptoms. You should also have an asthma review at least once a year.
Severe asthma
Even with large dosages of medication, severe asthma is a form of problematic asthma whereby symptoms are challenging to manage. Severe asthma affects about 1 in 25 persons with asthma. A specialized asthma clinic is often where severe asthma is diagnosed and treated.
Asthma symptoms could be severe if:
You’ve had two or more asthma episodes in a year that required oral steroids, you’ve got one or more asthma attacks that required hospital treatment in a year, and your asthma symptoms are interfering with your ability to sleep, even with prescribed medicines.
Asthma eosinophilic
High concentrations of blood cells known as eosinophils within the airways are the cause of eosinophilic asthma. Inflammation is caused by these blood cells.
Eosinophilic asthma can coexist with other forms of asthma. Some people, for instance, suffer from severe eosinophilic asthma or allergic eosinophilic asthma.
Biologic therapy are frequently used to treat eosinophilic asthma when conventional asthma medications are ineffective. As a result, your airways contain less eosinophils.
Childhood asthma
The most prevalent chronic illness harming children in the United Kingdom is asthma. Asthma affects about 1 in 11 kids in the UK.
As they get older, some kids with asthma find that their condition gets better or goes away entirely. We call this childhood asthma. Later in life, asthma might occasionally resurface.
Read these tips to assist your child stay healthy if they have asthma.
Adult-onset asthma
Although asthma typically first manifests in children, some adults receive their first asthma diagnosis. We call this late-onset asthma or adult-onset asthma.
Adult-onset asthma has several causes, including:
occupational asthma, which is asthma caused by chemicals you are exposed to at work.
smoking, secondhand smoke, female sex hormones, and obesity.
Classification
What are the different stages of asthma?
The National Institutes of Health established the following guidelines to help doctors assess the severity of your child’s asthma:
Step 1: Mild intermittent asthma is characterized by symptoms that occur less than twice a week, have short flare-ups lasting a few hours to a few days, and experience nighttime symptoms less than twice a month.
Step 2: mild, ongoing asthma
More than twice a week, but not multiple times a day, symptoms
The flare-ups may have an impact on his or her activity levels.
Beyond twice a month, symptoms occur at night.
Step 3: Moderate persistent asthma in step three
Daily symptoms
take their life-saving medication every day.
has flare-ups at least twice a week.
The flare-ups can have an impact on his or her degree of activity.
has symptoms at night on multiple occasions a week.
Step 4: severe, chronic asthma
Persistent symptoms
has reduced their type of physical exercise
has regular flare-ups and frequently encounters symptoms at night.
Causes
- Allergies: Asthma risk might be increased by having allergies.
- Environmental factors: After being exposed to items that irritate the airways, people may acquire asthma. These contaminants include second- or third-hand smoking, fumes, poisons, and allergies. Infants and young children, whose immune systems are still growing, may be particularly vulnerable to them.
- Genetics: You are more likely to get asthma or other allergy disorders if your family has a history of them.
- Respiratory infections: The developing lungs of young children may sustain harm from several respiratory infections, such as respiratory syncytial virus (RSV).
Although each person’s triggers are unique, some common ones are as follows:
- Dust mites: Although invisible, dust mites are present in our homes and can trigger an asthma attack if you have an allergy to them;
- Exercise: Exercise can trigger an asthma attack for some people; and air pollution: a variety of outdoor factors, such as factory emissions, vehicle exhaust, smoke from wildfires, and more, can trigger an asthma attack.
- Mold: If you have asthma, mold might be problematic since it grows in damp areas. To have an attack, you don’t even need to have allergic to mold.
- Pests: Asthma attacks can be caused by mice, cockroaches, and other household pests.
- Pets: Your animals may trigger asthma episodes. Inhaling pet dander, which is made up of dried skin flakes, can cause irritation to your respiratory system if you have an allergy to it.
- Tobacco smoke: You are more likely to get asthma if you smoke and someone in your household does. The best course of action is to give up smoking, though you should never smoke within enclosed spaces like your home or automobile. Your provider can assist you.
- strong odors or chemicals. Some people may have attacks as a result of these factors.
- specific exposures at work. At work, you may be exposed to a variety of substances, such as cleaning supplies, wood or wheat dust, and other chemicals. If you have asthma, any of these could be triggers.
Signs and Symptoms
- pressure, pain, or tightness in the chest.
- coughing, particularly in the evening.
- breathlessness.
- wheezing.
You might not experience every one of these symptoms during every flare-up of asthma. When you have chronic asthma, you may have various indications and symptoms at different periods. Additionally, symptoms may vary from one asthma attack to the next.
Who can get Asthma?
Asthma can strike anyone at any age. Asthma is more common in those who have allergies or have been around tobacco smoke. This covers secondhand smoke, which is when you are around someone else who is smoking, and thirdhand smoke, which is when you are around clothes or surfaces where someone has smoked.
Asthma is more common in women than in males. Furthermore, compared to other races, Black people are more likely to be impacted.
Diagnose
Physical examination
To rule out other potential illnesses, like a respiratory infection or chronic obstructive pulmonary disease (COPD), your doctor will do a physical examination. In addition, your doctor will question you about any other health issues as well as your symptoms.
Lung function tests
To find out how much air enters and exits your lungs during breathing, you could be subjected to lung function testing. These examinations could consist of:
Spirometry. By measuring how quickly and the amount of air you can exhale after taking a deep breath, this test calculates how small your bronchial tubes are.
maximum flow. A basic tool that gauges how difficult it is to exhale is a peak flow meter. Peak flow readings that are lower than normal indicate that your asthma may be worsening and that your lungs may not be functioning as effectively. You will receive instructions from your physician on how to monitor and manage low peak flow values.

Imaging examinations. Any diseases (such an infection) or structural anomalies that may cause or worsen breathing issues can be found with the use of a chest X-ray.
checking for allergies. A skin test or a blood test can be used for allergy testing. They identify any allergies you may have to dust, mold, pollen, or pets. Your doctor might suggest allergy injections if allergens are found.
Provocative testing for cold-induced asthma and exercise. Your doctor will measure your airway obstruction during these tests both before and after you engage in strenuous physical activity or inhale cold air multiple times.
Treatment
What asthma treatment choices are there?
You have alternatives to help manage your asthma. Your healthcare practitioner may prescribe drugs to control symptoms. These include:
Medical Treatment
These medications, known as bronchodilators, relax the muscles surrounding your airways. The airways can flow air because the muscles are loosened. Additionally, they facilitate the easier passage of mucus through the airways. These medications treat both chronic and intermittent asthma by reducing symptoms as they arise.
Anti-inflammatory medications: These medications lessen airway edema and mucus production. To manage or avoid your chronic asthma symptoms, your doctor could recommend taking these daily. When symptoms of severe asthma don’t go away with appropriate inhaler medication, biologic medicines are used.
Physical Therapy Treatment
- The majority of patients suffering from asthma will seek physical therapy for dyspnea and hyperventilation. Physical therapist treat asthma in different ways to improve breathing techniques.
- Physical therapy techniques for asthma are in addition to medication and should never be used as a replacement for prescribed medication, however may reduce the dosage required.
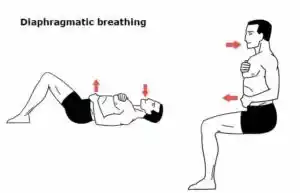
Techniques for Breathing Retraining
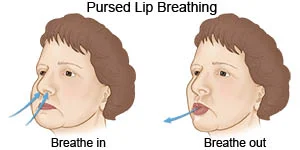
For mild-to-moderate asthma, breathing strategies might be more beneficial. By stabilizing respiratory rate and boosting expiratory airflow, breathing retraining aims to restore normal breathing patterns. The following elements are included in the physical therapist’s instructions on how to perform this technique:
- Taking fewer breaths (lowering the respiratory rate)
- Lowering Tidal Volume by Taking Smaller Breaths
- Deep breathing (diaphragmatic breathing using the lower thoracic chest movement and abdominal muscles)
- Nasal breathing, or breathing through the nose
- Relaxation (calm, steady breathing)
- Reduced expiratory flow due to pursed lip breathing is known as decreasing air leaving.
- These retraining methods aid in breathing control and lessen anxiety, hyperinflation, fluctuating breathing patterns, and airflow turbulence.
The Buteyko Breathing Method
Another breathing retraining method that is tailored to lowering hyperinflation is the Buteyko breathing technique. It was created on the premise that all asthmatic symptoms are caused by hyperventilation, which lowers PaCO2 and causes asthmatic bronchospasm. The air hunger caused by the constricted airways causes a shift to mouth breathing and an elevated respiratory rate, which ultimately results in hyperinflation. Buteyko thinks that bronchoconstriction is a result of this hyperinflation. In order to treat asthma and other respiratory conditions, the Buteyko approach attempts to decrease ventilation and, consequently, lung volume. The patient must be trained by a qualified practitioner.
The Method of Buteyko
- For two to three minutes, breathe normally through your nostrils.
- Breathe out normally, seal your nostrils with your fingers, and hold
- Keep track of the seconds.
- Release your nose and resume nasal breathing when you need to breathe for the first time (Control Pause).
- Hold off for three minutes.
- Hold your breath as long as you can while repeating (Maximum Pause).
Exercise
When taking the right measures, physical training is recommended for those with asthma and shouldn’t be avoided. For asthmatics, the American College of Sports Medicine (ACSM)
Guidelines offer advice and safety measures for safe exercise.
Physical Therapists should recommend physical exercise to asthmatics in order to improve their quality of life, decrease symptoms such as dyspnea, and enhance fitness and cardiorespiratory function. Exercise can cause asthma, chest tightness, and dyspnea, which discourages patients from exerting themselves. Fear can result in anxiety and sadness, which can also worsen physical health and quality of life. Physical training is an important therapeutic approach for asthmatics because it has been demonstrated to enhance illness symptoms and quality of life.
According to a study protocol, a behavior modification program that emphasizes physical exercise may help manage asthma and improve quality of life.
Increased endurance and less dyspnea are two benefits of aerobic exercise.
Resistance training: Enhances your balance and helps you build stronger muscles.
Training of the Respiratory Muscles
Increased lung volume from hyperinflation in asthma results in changed inspiratory muscle mechanics. Shortening of the inspiratory muscles causes a contraction’s length-tension connection to be less than ideal. When breathing, there is a reduced ability to generate tension, which leads to the use of accessory muscles of inspiration.
In order to make breathing exercises more challenging, an external device is used. Breathing becomes easier in daily life as a result of strengthening the inspiratory muscles.
A breathing apparatus creates a load against which to breathe. Air is only released upon inspiration if sufficient force is applied to open the device’s valves. By making the respiratory muscles work harder, they become stronger, which makes diaphragmatic breathing easier and lowers hyperinflation.
Techniques for breathing
Diaphragmatic breathing opens your airways and allows you to breathe more comfortably.
Pursed lip breathing: Lessens breathing issues and helps you distribute air more evenly in your lungs.
Breathing exercises that promote relaxation can help you regulate your breathing rate and lower the volume of your breaths.
Elimination of secretions
- Shaking Percussions
- Postural Drainage
- vibrations, and
- Productive coughing
Exercises for range of motion
- Exercises intended for hospitalized people.
- Learning
- Concerning the state
- When taking a bronchodilator along with any other drugs
- By enabling the chest to expand properly and the lungs to operate at their best, proper standing and sitting posture helps manage asthma attacks.
Prevention
How may an asthma attack be prevented?
You must determine what causes an asthma attack if your doctor diagnoses you with the condition. You can prevent an attack by avoiding the triggers. However, asthma is something you cannot avoid.
What is asthma control?
Controlling symptoms is the aim of asthma treatment. Controlling your asthma allows you to: Do the things you want to do at home and at work. have little to no symptoms of asthma. Use your relief medication (rescue inhaler) infrequently. Avoid having asthma disrupt your sleep.
- Able to carry out your desired tasks both at work and at home.
- Have little to no symptoms of asthma.
- Use your relief medication (rescue inhaler) infrequently.
- Avoid having asthma disrupt your sleep.
How are the symptoms of asthma tracked?
- You should monitor the symptoms of your asthma. It’s a crucial component of disease management.
- A peak flow (PF) meter may be recommended by your healthcare professional.
- The speed at which air may be expelled from your lungs is measured using this apparatus. It can assist your doctor in changing your prescription.
- Additionally, it indicates whether your symptoms are worsening.
FAQs
What does asthma mean?
A long-term illness that causes the bronchial airways in the lungs to swell and shrink, making breathing challenging.
What is asthma’s primary cause?
Typical triggers consist of: indoor allergens, including mold, dust mites, and fur or dander from pets. allergens found outside, like mold and pollen. stress on an emotional level.
Is asthma a dangerous condition?
Asthma sufferers may require emergency care and hospitalization for treatment and observation if their symptoms are severe. Asthma can be fatal in the worst situations.
Can asthma be completely cured?
You will have asthma for the rest of your life because it is a chronic ailment that can be managed. Unfortunately, asthma cannot be cured. Because of this, you could have symptoms of asthma when you are among triggers.
Is asthma worse with age?
Background. Patients with severe asthma are more likely to be older adults. We postulated that aging, rather than the length of asthma, is the primary cause of older people’s increased risk for severe asthma.
Does steam help people with asthma?
Inhaling steam can help clean the airways and facilitate breathing by releasing this mucus. It has also been discovered that respiratory steam therapy and asthma increase lung blood circulation. Improved blood flow can help promote healing and lessen airway inflammation.
Reference
- Asthma. (2025b, February 9). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/6424-asthma
- Wikipedia contributors. (2025, February 3). Asthma. Wikipedia. https://en.wikipedia.org/wiki/Asthma
- Types of asthma. (2024, June 30). Asthma + Lung UK. https://www.asthmaandlung.org.uk/conditions/asthma/types-asthma#allergic-asthma
- Types of asthma | Children’s Hospital Pittsburgh. (n.d.). UPMC Children’s Hospital of Pittsburgh. https://www.chp.edu/our-services/pulmonology/services/asthma/resources/type
- Asthma – Diagnosis and treatment – Mayo Clinic. (n.d.). https://www.mayoclinic.org/diseases-conditions/asthma/diagnosis-treatment/drc-20369660



16 Comments