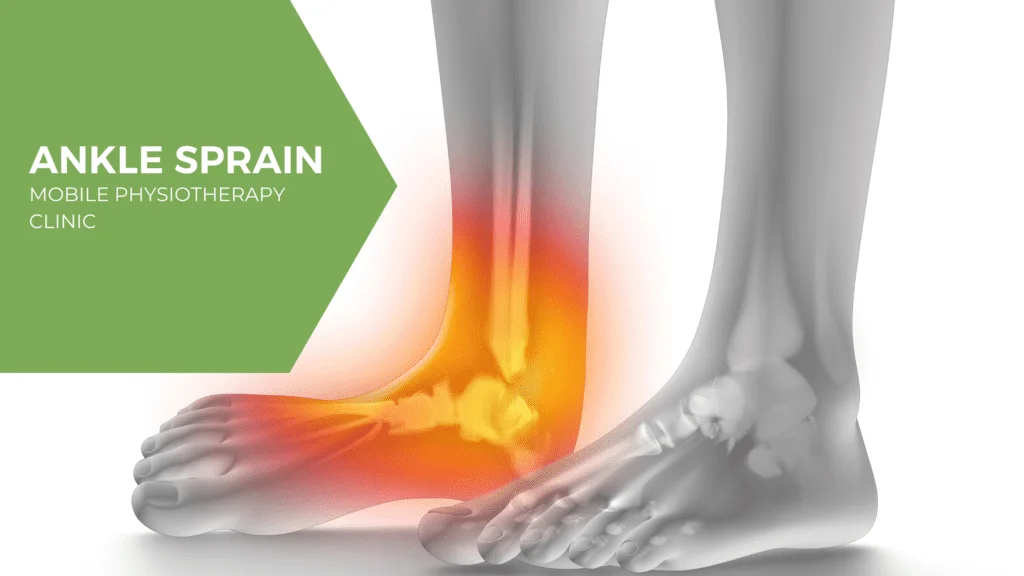
Ankle Sprain
Introduction
Ankle sprains are common musculoskeletal injuries caused by a partial or complete tear or stretch of the ankle’s ligaments. They mostly affect active and sports-related populations and arise when the ankle breaks away from its normal range of motion.
Epidemiology
The second most common joint that experiences an injury in sports is the ankle joint, which is prone to sprains.
Ankle sprains commonly occur as lateral ligament injuries, making up around 85% of all sprains; acute medial and syndesmotic sprains are less common. Females are more likely than males and children to get ankle sprains.
Anatomy with Clinical Significance
The Anterior Talofibular ligament is the ligament in the lateral ankle ligament complex that suffers damage the most frequently (ATFL). The act of forcefully twisting the movement of a foot that is plantar flexed can result in sprain injuries to the ATFL and CFL. In this case, it suggests that there is a decreased likelihood of harmful loads on the posterior talofibular ligament (PTFL) and the calcaneofibular ligament (CFL). Rarely is the PTFL harmed unless it is connected to a talus dislocation.
Forceful pronation and rotation movements of the hindfoot harm the strong, deltoid ligament complex on the medial side, which is made up of the posterior Tibiotalar (PTTL), anterior Tibiotalar (ATTL), calcaneal (TCL), and tibiinavicular (TNL) ligaments.
The stabilizers distal to the tibio-fibular syndesmosis is formed by the inferior transverse ligament, the anterior-inferior, posterior-inferior, and transverse tibiofibular ligaments, as well as the interosseous membrane and ligament. When the ankle’s dorsiflexion and the leg’s external rotation are coupled, a syndesmotic (high ankle) sprain results.
Mechanism of Injury
Lateral ankle sprains usually occur during a rapid shift of the body’s center of mass over the landing or weight-bearing foot. The lateral ligament stretches and tears as the foot twists inside and the ankle rolls outward. Rarely does a ligament’s previous strength and flexibility return to normal once it tears or is overextended. Some situations when a return to play is allowed too soon have been reported by researchers, affecting proper ligamentous repair.
According to a study on 94 young competitive volleyball and basketball players in Brazil, the likelihood of ankle sprains increased to 80.6% when the athlete had a dominant lower leg (left leg), a peroneus brevis electromyographic response time greater than 80 ms, they were wearing shoes without dampers, and they played in a particular position.
Additionally, the dominant leg is 2.4 times more likely to sprain than the non-dominant leg, according to a study on the epidemiology of unilateral ankle sprains. A less frequent mechanism of injury is a powerful deltoid ligament injury caused by an active eversion action at the ankle.
- Aspect – Lateral
- Mechanism of injury- Inversion and plantarflexion
- Ligaments- anterior talofibular ligament,
calcaneo-fibular ligament
posterior talofibular ligament
- Aspect- Medial
- Mechanism of injury: Eversion
- Ligaments: posterior tibiotalar ligament
tibiocalcaneal ligament
tibionavicular ligament
anterior tibiotalar ligament
- Aspect: High
- Mechanism of injury: External rotation and dorsiflexion
- Ligaments: anterior-inferior tibiofibular ligament
posterior-inferior tibiofibular ligamen
transverse tibiofibular ligament
interosseous membrane
interosseous ligament
inferior transverse ligament
Classification of Ankle Sprain
Ankle sprains can be categorized using some grading plans, each with unique advantages and disadvantages. For effective continuity of care, therapists use several systems that reflect the patient’s circumstances and educational background.
Ankle sprains can be categorized using a grading system that concentrates on one particular ligament:
- Grade I (Minimal stretching, no tearing): minor overstretching/damage to fibers
- Grade II (Partial tear): A partial tear of the ligament
- Grade III (Full tear or rupture): represents the complete rupture of the ligament
The use of a grading system created to describe the status of a single ligament may not always be straightforward unless it is certain that just one ligament is injured, as the ankle joint is covered by numerous ligaments. Other grading system based on the number of injured ligaments is used for ankle sprains. It is, however, hard to determine the exact number of ligaments torn unless there is clear high-quality radiographic imaging or surgical evidence.
An alternative system that may be used depends on how severe the sprain injury is:
Grade I: Mild impairment – Minimal swelling and tenderness with little impact on function, tenderness. Usually no bruising. No joint instability. No difficulty bearing weight. Recovery time is around 1–3 weeks
Grade II: Moderate swelling, pain, and tenderness with limited range of motion and ankle instability. Possible bruising. Mild to moderate joint instability. Loss of range of motion and function. Pain during weight-bearing activities and walking. Recovery time is around 3–6 weeks
Grade III: Severe injury with swelling, tenderness, loss of Ankle function, and marked instability. Unable to bear weight or walk. Recovery time Up to several months
Causes of Ankle Sprain
An ankle sprain is common when the foot flips or twists unexpectedly, causing the ankle joint to become malpositioned. Ankle twists can occur during physical exercise when there is an abrupt or unplanned movement. This may result in a tearing of one or more ankle ligaments.
These injuries cause swelling or bruises. Pain or discomfort may also be felt when you place weight on the injured area. Potentially injured blood vessels, tendons, and cartilage could result from the sprain.
Sports-related activities, uneven terrain, and even the wrong kind of shoes can result in this kind of injury.
When your ankle is forced to move from its natural position, one or more of the ligaments may stretch, partially tear, or rupture completely, resulting in a sprain.
It may result from the following:
- Twisting Ankle Movement
- During Jumping, landing awkwardly on your foot.
- Walking or exercising on an uneven surface
- Another person stepping or landing on your ankle during any activity or sports.
Clinical Symptoms
Ankle sprain indications and symptoms can vary depending on the kind and extent of the injury. Here are some examples:
- pain during weight-bearing activity on the affected foot.
- tenderness upon palpation of the ankle joint.
- bruising, edema, and swelling.
skin discoloration, stiffness
Ankle Stiffness and instability at the level of the joint.
Complains of paresthesia which could affect neurovascular. compromise of the peroneal nerve.
Forceful eversion injury to the ankle.
Previous history of ankle injuries or instability.
Special tests: Anterior Draw, Talar Tilt, or Squeeze Test are Positive. (depending on the ligament affected).
It should be noted that the symptoms of a lateral ligament sprain should be replicated by passive inversion or plantar flexion with inversion, and the symptoms of a medial ligament sprain by passive eversion.
Outcome Measures
Lower Extremity Functional Scale (LEFS)
Foot and Ankle Ability Measure (FAAM)
Foot and Ankle Disability Index (FADI)
Star Excursion Balance Test
Diagnosis
Your doctor will check your ankle, leg, and foot during a physical examination. The physician will move your foot to evaluate your range of motion and determine which positions hurt or cause discomfort. They will also touch the area surrounding the injury to look for any painful spots.
Your doctor might suggest one or more of the following imaging tests if the injury is serious to rule out a broken bone or evaluate the extent of ligament damage specifically:
X-ray. Radiation passes through your ankle. Bone fractures may be confirmed with this test.
Magnetic resonance imaging (MRI). A powerful magnetic field and radio waves are used in MRI (magnetic resonance imaging) to create highly detailed 3-D or cross-sectional images of the soft internal ankle structures, such as ligaments.
CT scan. CT scans can provide more specific information about the joint’s bones. CT scans provide cross-sectional or three-dimensional images by combining X-rays taken from different angles.
Ultrasound. An ultrasound creates real-time images by using sound waves. These images may help your doctor assess the condition of a ligament or tendon when the foot is in different positions.
Clinical Examination
An ankle sprain involves various structures, therefore foot and ankle assessment is important. To help with the diagnosis, the evaluation of the injured ankle involves examining the patient’s past medical records to determine whether the injury was similar, different, or never happened. Following the collection of the patient’s past medical history, it’s important to observe the patient’s progress and posture, taking note of any deformities, malalignments, atrophy, swelling, or ecchymosis. After that, the patient’s passive and active range of motion must be evaluated. Palpating the affected structures is required to feel any pain over bony prominence, muscle, or even ligaments.
Special Tests
Anterior Drawer Test – tests the Anterior Talo-Fibular Ligament
Talar Tilt Test- tests the Calcaneofibular Ligament
Posterior Draw – tests the Posterior Talofibular Ligament
Squeeze test – tests for a Syndesmotic sprain
External rotation stress test (Kleiger’s test) – tests for a Syndesmotic sprain
Different Diagnosis
An Ankle fracture, tendon subluxation, tendinopathy, tendon rupture, and several other related conditions are associated with the differential diagnosis of an ankle sprain. The diagnosis is made based on the patient’s medical history, examination results, and the results of an ultrasound to determine whether a tendon damage has taken place. In chronic cases, when the Ottowa Rules do not apply, diagnostic imaging can be used to confirm the diagnosis.
Additional differential diagnoses to look out for:
- Impingement
- Tarsal Tunnel Syndrome
- Sinus Tarsi Syndrome
- Cartilage or osteochondral injuries
- Peroneal Tendinopathy or subluxation
- Posterior Tibial Tendon Dysfunction
Treatment
The severity of your injury determines how you should be treated for a sprained ankle. Reducing discomfort and swelling, improving ligament healing, and restoring ankle function are the objectives of treatment. If your injuries are serious, you can be referred to an orthopedic surgeon or a doctor who specializes in physical medicine and rehabilitation, who are specialists in treating musculoskeletal problems.
Self-care
After ankle sprain, use the R.I.C.E. method for self-care:
- Rest. Avoid painful activities.
- Ice. Use an ice pack for 10 to 15 minutes. Repeat every two to three hours. See your doctor before using ice if you have diabetes, vascular problems, or reduced feeling.
- Compression. Apply an elastic bandage to the ankle and squeeze it until the swelling decreases. Don’t wrap too tightly as this may prevent circulation.
- Elevation. Elevate your ankle above your heart to minimize swelling, particularly at night. Gravity drains extra fluid, which helps minimize swelling.
Medications
For the most part, sprained ankle pain can be effectively treated with over-the-counter analgesics like ibuprofen (Advil, Motrin IB, etc.), naproxen sodium (Aleve, etc.), or acetaminophen (Tylenol, etc.).
Devices
Using crutches until the pain goes away can be necessary if you have a sprained ankle because walking could be uncomfortable. Your doctor may advise using athletic tape, an ankle support brace, or an elastic bandage to stabilize your ankle, depending on how severe your sprain is. If the sprain is severe, you might be required to immobilize the ankle with a walking cast.
Physical Therapy
Your doctor will have you start an exercise plan of exercises that will improve your ankle’s strength, flexibility, range of motion, and stability once the swelling and pain are completely reduced. The proper technique and workout progression will be explained by your physician or physical therapist.
Retraining the ankle muscles to play a role in supporting the joint and preventing recurrent sprains requires a special focus on balance and stability training. These activities, like standing on one leg, may present different types of balancing challenges.
Physical therapy plays an important part in the management of ankle sprains, particularly in athletes. It’s important to remember that the course of treatment differs based on the severity of the injury and whether the sprain is acute (lasting less than four weeks) or chronic (lasting more than four weeks).
The objectives of physical therapy are to strengthen the ankle joint and lessen pain and edema. A patient’s recovery typically takes five to fourteen days. Physical treatment aims to restore functional movement and stability while also lowering pain and edema in cases of chronic ankle sprains. A patient’s recovery often takes three to twelve weeks, or longer.
The PRICE (Protect, Rest, Ice, Compress, Elevate) therapy program is commonly used. It involves providing the injured ankle 72 hours of rest, protecting the ankle joint with crutches if needed, applying ice to reduce swelling and pain, applying a compress with a bandage or brace to stabilize the joint, and elevating the ankle to relieve pain and edema.
Exercise for ankle sprain
When to start ankle sprain exercise
If the injury is not too serious, most patients can start ankle rehabilitation activities three days following the accident. However, no timetable is set up. Take note of what your body tells you, and follow medical advice.
You should rest and apply an ice pack to your damaged ankle for ten to fifteen minutes every few hours during the first few days. Avoid touching your skin with the ice and avoid leaving it on for too long as this could cause burns.
The rest period is normally three days for most people. Following that, you can start a program of at-home workouts or physical treatment, and you can progressively increase the use of your ankle.
Types of exercises for a sprained ankle
- Range of motion exercises
- stretching exercise
- strengthening
- balance and control
Ankle range of motion exercises, stretching, and ankle strengthening: First 1–2 weeks
These easy exercises can help you keep your ankle’s flexibility and range of motion intact.
The Ankle alphabet
Take a seat on a comfortable chair. Stretch your leg wide and use your big toe to draw the alphabet’s letters in the air. 2 or 3 repetitions of this. These easy exercises help to improve your ankle’s movement.
Knee motion
Take a comfortable seat on a chair. Keep your foot on the floor and gently move your knee up and down for two to three minutes. This helps relax and stretch the ligaments that surround your ankle.
Towel and tissue scrunches
Sit in an uncomfortable chair and keep a little towel on the floor. Taking off your shoes and socks, use your toes to gently grip the towel, tear it up, and count backward from five. Next, remove the towel and carry on. Repeat 8 to 10 times.
Ankle stretching exercises
Your calf muscles and heel bone are connected by the Achilles tendon, which runs behind your ankle. Stretching your Achilles tendon is the next series of exercises that you should begin as soon as possible.
Towel stretch
With your leg extended in front of you, take a seat on the floor. Grip the ball of your foot with a strap or towel. Toes coming towards you, pull back on the towel. Stretch for a duration of 15 to 30 seconds. Avoid going overboard. Your calf muscle should only feel slightly to moderately stretched.
Standing calf stretch
Place your hands on the countertop or wall in front of you for support. Step back on your hurt ankle with your good foot forward. Keep your back heel level on the ground and flex the knee of your good leg progressively until you feel a slight stretch in the calf on your injured side. Repeat three times, holding this for thirty seconds each time.
Heel raise
Place your hands in front of you and lean them on a countertop, wall, or the back of a chair for balance. Step up and down on your toes slowly while keeping your feet shoulder-width apart. Increase to at least 20 of these over time, starting with about 10. Remember that you want no pain, only a small stretch. When the toes on the injured side are comfortable, you can switch to utilizing them alone.
Balance on one leg
Raise your normal leg behind you so that the leg with the injured ankle supports your weight, with your hands on a wall or chair. For 20 to 30 seconds, try to hold this. As you get stronger, try doing it with just one or two fingers. Continue doing this till you reach a stronger point.
Exercises to strengthen your ankles
It’s proper to move on to strengthening exercises after you can bear weight on your sprained ankle easily and have a good range of motion. A resistance band will be needed for these exercises.
You can get this simple elastic band online, via a physical therapist’s clinic, or from a sporting goods store.
Elastic band push
Take a seat on the ground. To keep your heel off the ground, prop up your ankle with a swimming noodle or rolled-up towel. Hold the ends of the elastic band while circling the of your foot. Now, gradually extend your ankle forward as though you were pointing a toe. Then return it gradually. Ten times over, repeat this. If your ankle looks unstable or if there is any pain, don’t use the band.
Elastic band tug
Use your resistance band to secure it around an important item, like a desk or table leg. wrap your toes and upper foot with the thera-band while seated on the floor. Now, carefully raise your foot back up to your body and straighten it out. Ten times over, repeat this.
Ankle out
Wrap your resistance band around something heavy. wrap the inside of your foot into the band’s end in a seating or standing position. Step your foot back and forth slowly. Increase the number of repetitions to 20 from 10 at the beginning.
Ankle in
Encircle a substantial object with the resistance band and insert your instep into it. Now, move your foot inward against the resistance band and slowly draw it back. Repeat ten times, then increase to twenty repetitions.
Basic balance
Raising the other foot off the ground behind you, try to keep your balance while standing on the damaged foot. At first, try holding this for a few seconds. Then, if you can, increase to 30 and 1 minutes.
Balance with eyes closed
Now close your eyes and practice the basic exercise of balance. This is more harder because you can’t rely on visual clues to help you balance. Ensure that you have a rescue strategy. See if you can reach thirty-one minutes once more.
Pillow balance
Do the same basic balance practice while standing on a pillow. This is much harder. Even if your ankle is not hurt, you will constantly need to adjust your balance because your foot will be wobbling a lot. Aim for between 30 and 60 seconds. Stop if you begin to have ankle pain.
Surgery
In rare cases, following prolonged physical therapy and rehabilitative activity, surgery is necessary if the injury does not heal or if the ankle does not become stable. Surgery could be done to:
Repair a ligament that won’t heal
Reconstruct a ligament with nearby ligament or tendon.
Consult your doctor about when you can return to your activities if you injured your ankle while working out or playing a sport. In order to assess how well your ankle operates, your doctor or physical therapist may ask you to perform certain movement and activity tests if you participate in sports.
Rehabilitation of an ankle sprain
The aim is to improve your:
- Developed Muscles around the Ankle
- Stability in the Ankle joints
- Balance, and coordination
Your doctor will go over specific rehabilitation objectives with you if an ankle sprain is the diagnosis. However, the broad timeframes in question are:
1-2 weeks. a reduction in edema and improved mobility. Walking and standing up should get simpler.
two to four weeks. Walking normally again now. Nearly 100% movement and a decrease in edema.
8–12 weeks. Your routine tasks are starting to become more easier for you to complete.
Each soft tissue injury is unique, so you may need more time or less time than this estimate to heal.
Risk Factors
Athletes who experience chronic ankle instability are prone to both internal and external risk factors.
- Extrinsic factors: A history of sprains is one example of an external cause that can harm sensory nerve fibers and reduce stabilizer strength and integrity.
- Intrinsic factors: Intrinsic factors include limb dominance, postural sway, foot architecture, height, weight, and sex.
- Other external factors include the type of shoe type, the duration of the competition, bracing, taping, and exercise intensity.
Complication
- Chronic ankle instability (CAI): This is the most common complication of ankle sprains. Your ankle may feel loose and unsteady as a result of the ligaments in your ankle being stretched or damaged.
- Arthritis: Repetitive sprains of the ankle joint may damage the cartilage over time, eventually resulting in arthritis. Ankle discomfort, stiffness, and edema can all be symptoms of arthritis.
- Reflex sympathetic dystrophy (RSD): This is a complex condition that can cause pain, swelling, and stiffness in your ankle and foot. It is an uncommon side effect of sprained ankles.
- Peroneal tendon injuries: The peroneal tendons run along the outside of your ankle and help to stabilize your ankle joint. These tendons may be injured if you sprain your ankle.
- Neurovascular injury: There is a slight chance that a severe ankle sprain may damage the blood vessels or nerves that run along your ankle. Your foot may become weak, uncomfortable or numb as a result of this.
Prevention
While there is no way to completely prevent the possibility of suffering an ankle sprain, there are things you may do to greatly lower your risk.
Strengthening and Flexibility:
Regular Stretching: Stretching your ankles, hamstrings, and calves regularly helps to maintain their flexibility and reduces the tension that may give rise to sprains.
Exercises for Ankle Strengthening: Exercises that focus on the muscles surrounding your ankle joint improve support and stability.
Balance Training:
Balance exercises: Activities like single-leg stands or wobble boards improve proprioception, and your body’s awareness of joint position, which helps maintain ankle stability.
Footwear:
Supportive Shoes: When participating in activities that increase your risk of rolling your ankle, wear shoes that fit properly and offer sufficient ankle support.
Replace Worn-Out Shoes: Uneven or worn-out treads might affect stability. It is advisable to regularly replace your athletic shoes.
Warming Up and Avoiding Uneven Surfaces:
Warm Up Before Activity: Before engaging in any type of activity or sports, warm up your muscles with a gentle jog or dynamic stretches.
Mind Your Footing: Take care when running or walking on uneven surfaces, such as cluttered areas, loose gravel, or hiking trails.
Other Advice:
Gradual Increase in Activity: To prevent overloading it, if you’re beginning a new fitness program, gradually increase the duration and intensity of your workouts.
Pay Attention to Your Body: If you feel any pain in your ankles, take care of it and avoid activity accordingly.
Ankle braces or taping may be recommended by a doctor if you have a history of ankle sprains in order to provide additional support during high-risk activities.
Conclusion
Ankle sprains are common, but with proper care, they typically heal well within a few weeks. This is an overview:
Healing Timeline: The majority of sprains heal in 4-6 weeks, at which time rest, edema reduction, and following strength and mobility restoration are priorities.
Complications: Repeated sprains or poor healing can lead to tendon problems, arthritis, and chronic instability, though these are rare.
The Key Is Prevention: The risk of sprains is greatly decreased by regular stretching, strengthening exercises, balance training, and wearing supportive shoes.
Listen to Your Body: Recognise when anything hurts and modify your activity accordingly. Early medical evaluation guarantees a correct diagnosis and a treatment plan that will help recovery and reduce side effects.
References
- Recovering from an ankle sprain. (2024, March 28). Harvard Health. https://www.health.harvard.edu/pain/recovering-from-an-ankle-sprain
- Hecht, M. (2019, February 15). 15 Exercises for Your Sprained Ankle. Healthline. https://www.healthline.com/health/sprained-ankle-exercises#takeaway
- Ankle sprain | NHS inform. (2024, February 5). NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints/conditions/ankle-sprain/
- Sprained ankle – Diagnosis and treatment – Mayo Clinic. (2022, August 11). https://www.mayoclinic.org/diseases-conditions/sprained-ankle/diagnosis-treatment/drc-20353231






8 Comments