Sural neuritis, also known as sural neuralgia, is a painful disorder caused by irritation or damage to the sural nerve. The most common description of the pain is a burning feeling on the outside of the foot and ankle.
It can happen after surgery on the feet and ankles or if there is a nerve injury. Using an adverse massage method to desensitize the nerve, using oral drugs to reduce inflammation, and avoiding applying direct pressure on the nerve are examples of non-surgical therapy approaches.
In some cases, surgery may be necessary to remove the damaged nerve or relieve the surrounding scar tissue if the symptoms are severe.
What is the Sural Nerve?
- Your sural nerve is located in the posterior part of your lower leg, just below the skin’s surface (calf). It’s a part of your peripheral nerve system, which enables your body and brain to communicate.
- The outer heel, the back of your lower leg, and the skin on the outside of your foot are all sensed by the sural nerve. You can use it to sense touch, warmth, and pain in addition to foot position. Difficult nerve illnesses can be identified and treated with the help of the sural nerve.
Which type of nerve is the sural nerve?
As a sensory nerve, your sural nerve allows you to perceive and sense the following:
- Touch.
- Foot position.
- Temperature.
- Pain and vibration.
Anatomy Of the Sural Nerve
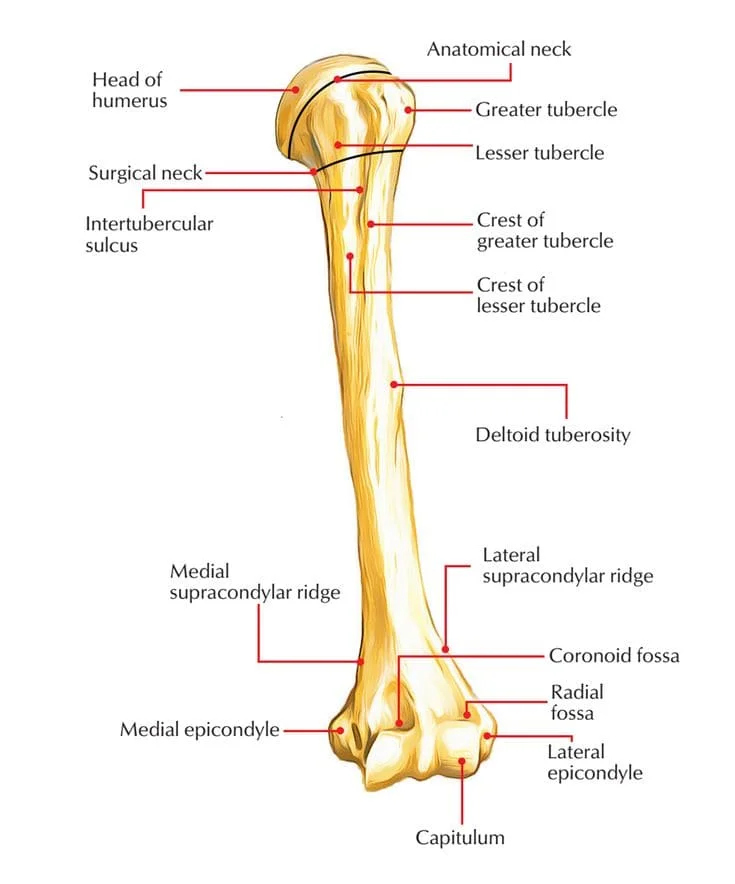
Your sural nerve begins where two nerves merge in your upper leg. It goes down the back of your leg, finishes right in front of your toes, and bends at the ankle.
Two nerves influence how your sural nerve forms:
- The tibial nerve supplies feeling and motor function to the back of your leg and foot.
- The common fibular nerve, also known as the common peroneal nerve, supplies sensation, and motor function to the tissue just behind your knee and surrounding leg muscles.
What composition makes up the sural nerve?
Your sural nerve is made up of tiny, string-like fibers called axons. The fatty material known as myelin connects them to form nerve bundles. These bundles connect to the spinal cord once they enter the body. Your brain receives and sends nerve information quickly thanks to this network of nerve tissue.
Function Of The Sural Nerve
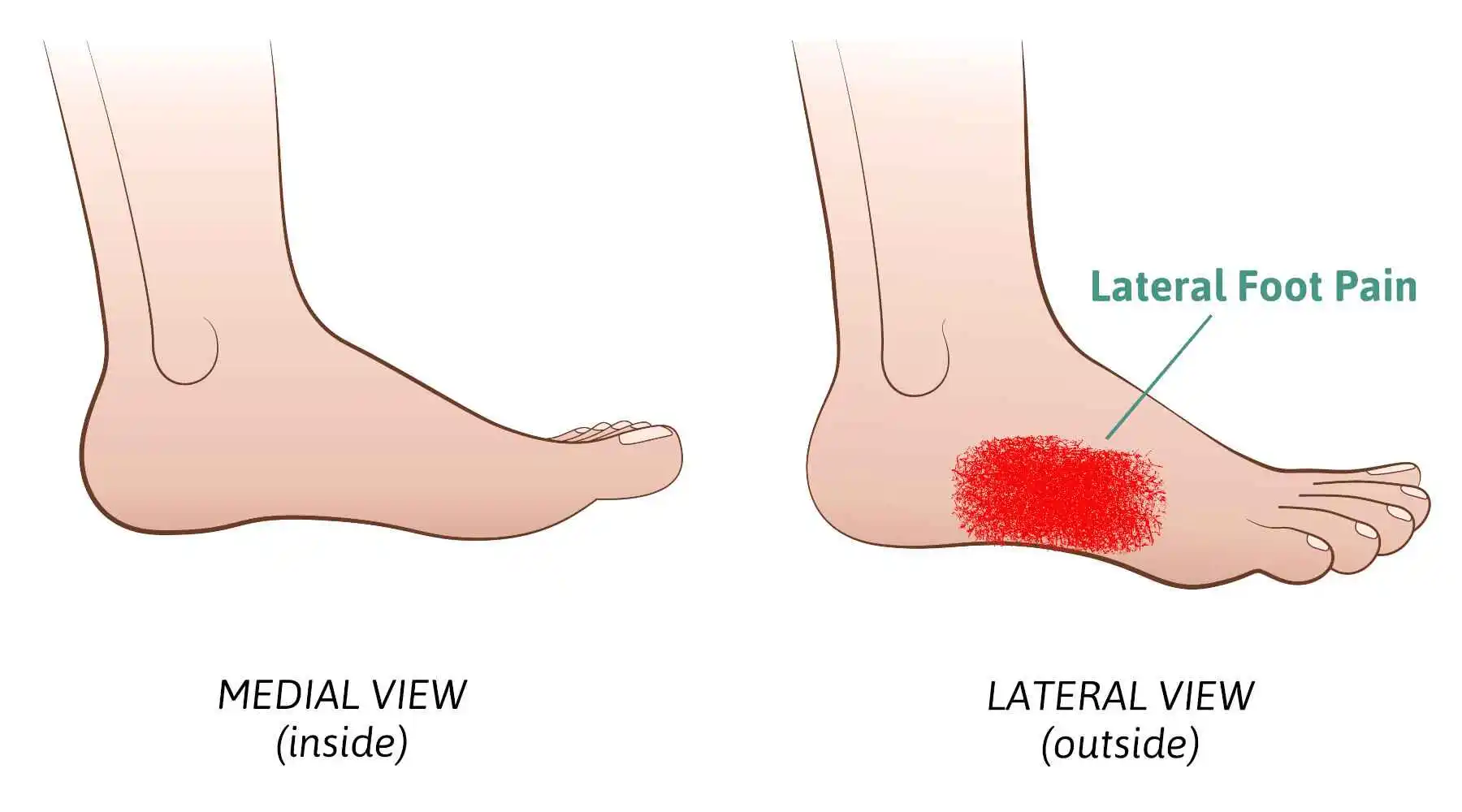
Your sural nerve detects skin color in the following regions:
- Below the knee and at the back of your leg.
- Your foot’s outside side.
- The outside of the heel.
- Ankle.
In addition to providing you with feeling, your sural nerve helps with balance when standing. To treat and diagnose a variety of nerve disorders, it can also be utilized as donor tissue.
What is Sural Neuritis?
- When a portion of the sural nerve becomes trapped, inflamed, or injured, it can cause sural neuritis, also known as sural neuralgia.
- All pain from an inflamed nerve is called neuritis. One of the five nerves that travel through the ankle and provide sensation to the foot is the sural nerve. The sural nerve senses only a small region on the outer edge of the foot and the fourth and fifth toes.
- Shoes with features like thick straps or seams pressing against the Achilles tendon outside the heel or foot might irritate the sural nerve. Sural neuritis can be caused by pressure or mechanical irritation because the nerve is just beneath the skin. This may cause burning, tingling, or numbness along the nerve’s path.
- The pain associated with a nerve injury may also radiate or shoot up the back of the leg, or out to the fourth and fifth toes. Additionally, it may result in pain along the outer surface of the heel bone.
Causes of the Sural Neuritis
- Trauma to the leg is the most frequent cause of damage to the sural nerve, but it can also occur following surgery if scar tissue ends up trapping part of the nerve.
- The most frequent causes of nerve injury include a severe ankle sprain, a violent fall, an athletic collision, and a can accident.
Symptoms of the Sural Neuritis
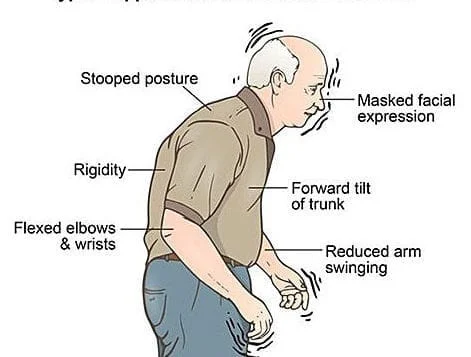
- Ankle or foot pain on the outside.
- The feeling of discomfort can be as burning.
- Localized hypersensitivity.
- Numbness.
- Swelling.
- Some types of footwear might make pain worse since pressure on the affected area aggravates symptoms.
Diagnosis of the Sural Neuritis
Physical Examination
The diagnosing process relies heavily on physical examination. When you tap on a nerve, you will experience an “electrical” sensation known as the Tinel, which is especially noticeable in areas where the nerve is damaged. Along the nerve’s path, there may also be localized edema and discomfort on the outer surfaces of the foot and ankle.
Imagine Test
Simple X-rays are rarely useful in surgical neuritis diagnosis. Since it is a soft tissue structure, an x-ray will not reveal the nerve. Furthermore, an MRI is not likely to be helpful because the sural nerve is too small to be seen. However, some information about prior surgeries or other injuries to the area that might be connected to the current symptoms may be obtained from these imaging investigations.
Treatment for the Sural Neuritis
Whether it’s scar tissue or a sprained ankle, treating sural neuritis entails treating the underlying root cause of nerve injury.
Conservative treatment
The majority of sural neuritis cases either get better with time or can be effectively managed without surgery. For sural neuritis, there are numerous non-operative therapeutic options available:
- Medicine. Two drugs called gabapentin and pregabalin may assist in stabilizing the irritated nerve.
- Injection of corticosteroids. To reduce pain and inflammation and break up the scar tissue surrounding the nerve, a targeted corticosteroid injection may be helpful.
- Wear comfortable shoes. Selecting the appropriate footwear can prevent direct pressure on the injured nerve region. The cushioning to the affected area can also reduce discomfort and decrease symptoms.
- Desensitization. When direct massage is applied to an irritated nerve, the intention is to desensitize the nerve and break up any surrounding scar tissue. Desensitization is uncomfortable at first, but it usually gets better with time.
Physical Therapy
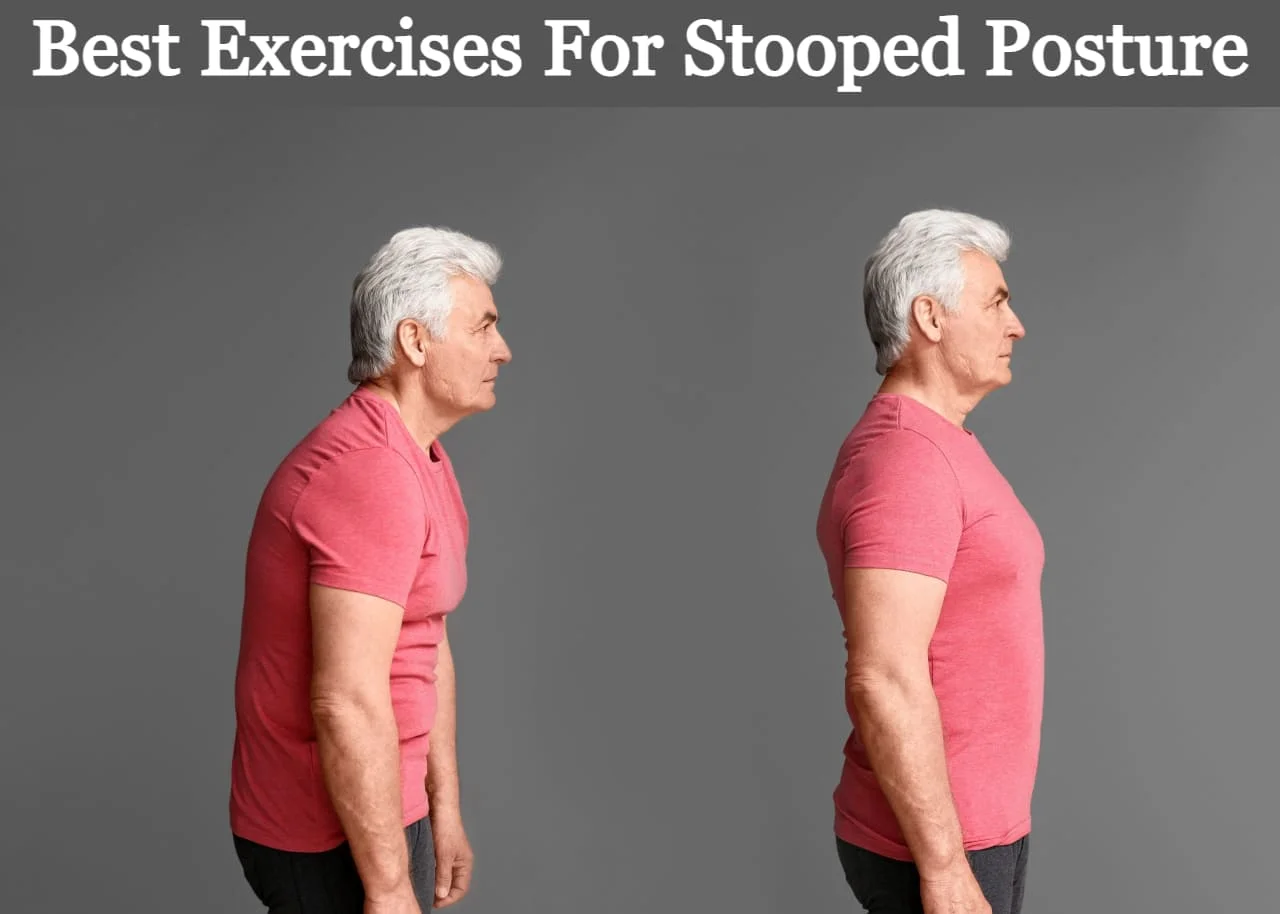
Physical therapy can be a very effective therapy for sural neuritis because it helps to treat underlying causes of nerve compression by reducing nerve pain and inflammation, improving nerve mobility, and preventing future recurrence.
A physical therapist will treat sural neuritis using a combination of techniques, such as:
- Electrotherapy: Inflammation and pain can be lessened with the use of ultrasound therapy. Pain can be decreased and nerve function can be improved by electrical stimulation.
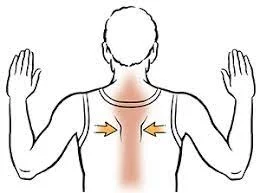
- Manual therapy: To help reduce inflammation and improve nerve gliding, this can include massage, friction massage, and nerve mobilization treatments.
- Taping: Taping can reduce pain and support the calf and ankle.
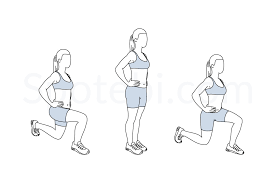
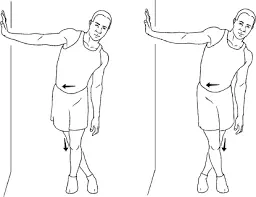
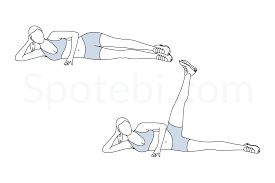
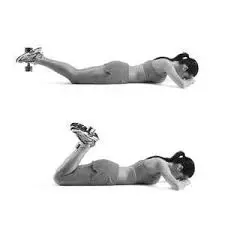
- Exercises: An essential component of physical therapy for sural neuritis is exercise. Stretches, strengthening exercises, and nerve-gliding activities are a few different exercises.
Exercises for sural Neuritis
Ankle Circle:
- To begin, slowly rotate your ankle in circles, starting from the left and moving towards the right.
- It might even appear easier to try drawing the letters while standing on your tiptoe. Point the path with your big toe.
- Try to move as little as possible and focus on using your foot and ankle alone, not your entire leg.
- Turn your ankle slowly, in one direction at first, then the other.
Ankle Pump:
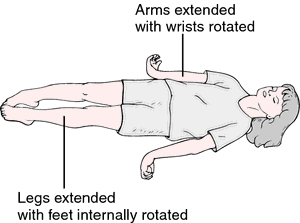
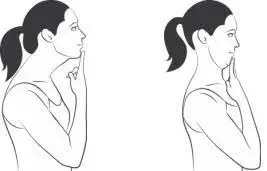
Point your toes down after bringing them up toward your head while sitting or lying on your back. Ten repetitions of this exercise should be performed on both ankles at the same time, once an hour.
Toe stretches:
Wrap your toes in a towel and settle into a chair. Pulling back on the cloth gently will stretch the top of your foot.
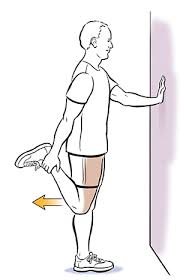
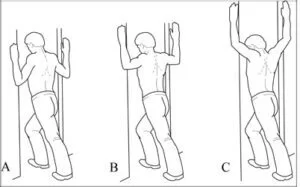
Calf Stretching:
Stretch your calf by standing facing a wall and placing your hands shoulder height on the wall. Until your calves start to stretch, lean forward. Repeat after 30 seconds of holding.
Operative Treatment
Surgery could be necessary if there is nerve discomfort that is not relieved by non-surgical means, if the nerve has been extensively scarred, or if the hardware inserted during the surgical process is irritating. Typically, sural neuritis surgery entails one of two things:
- Releasing the nerve. Surgery to remove any aggravating structures (such as residual metal) or to release the nerve from the surrounding scar tissue may also be beneficial. Scar tissue, though, frequently reappears. Therefore, collagen nerve wrapping may help stop the growth of scar tissue recurrence.
- Nerve Resection. It is frequently preferable to remove the sural nerve if the nerve is too severely injured due to previous scarring or if the symptoms are severe. Since the sural nerve primarily provides feeling to the outside of the foot and ankle, its resection results in numbness along its entire course without affecting motor function.
Complication
Complex regional pain syndrome is a potentially severe illness and a potential problem with sural neuritis, yet inconceivable.
Prevention for the Sural Neuritis
You can take the following actions for prevention of the Sural Neuritis
- If you have diabetes, make sure your blood sugar levels are within a healthy range.
- Choosing and replacing well-fitting sporting footwear when it becomes worn out.
- Giving up smoking and other tobacco products.
- Maintaining the health of your nerves by eating a balanced diet that includes foods high in vitamin B12 and vitamin D.
FAQs
What is the cause of sural neuritis?
The most often specified causes of sural neuropathy in research include accidental damage, repetitive or prolonged external ankle compression, and nerve trauma from ankle fracture.
How much time does it take for damage to the sural nerve to heal?
Your nerve should heal in six to twelve weeks if it is swollen or injured but not cut. Following four weeks of “rest,” a cut nerve will grow by 1 mm per day.
How is the sural nerve tested?
The patient’s clinical symptoms can be replicated using the sural nerve neurodynamic test. One can also use point tenderness over the nerve or a positive Tinel sign as clinical indicators of disease. If there is discomfort, plantar flexion and/or foot inversion may make it worse.
What is the treatment for sural neuritis pain?
Conservative treatments for sural neuralgia, which is a very uncommon sickness, frequently work. These include bed rest, physical therapy, massage therapy, anti-inflammatory drugs, tricyclic antidepressants, gabapentin, serotonin and norepinephrine inhibitors, and calcium channel blockers.
What early symptoms indicate damage to the nerves?
The following are the most typical signs of a nerve disorder: burning, tingling, or numbness in your extremities or limbs. unexplained weakness, paralysis, or loss of muscle strength. a persistent headache that seems “different” or appears out of the blue.
References
- Professional, C. C. M. (n.d.-u). Sural nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22323-sural-nerve
- FootEducation. (2019, November 6). Sural Neuritis – FootEducation. http://www.footeducation.com/sural-neuritis/
- Silverman, L., MD. (2021, May 10). Treating sural neuritis. Silverman Ankle and Foot Edina Orthopedic Surgeon. https://www.anklefootmd.com/treating-sural-neuritis/
- Segler, C. (2018, May 3). Sural Neuritis. DOC. https://www.docontherun.com/sural-neuritis-3/
- Silverman, L., MD. (2018, March 6). Diagnosing and treating severe nerve problems. Silverman Ankle & Foot – Edina Orthopedic Surgeon. https://www.anklefootmd.com/diagnosing-and-treating-sural-nerve-problems/