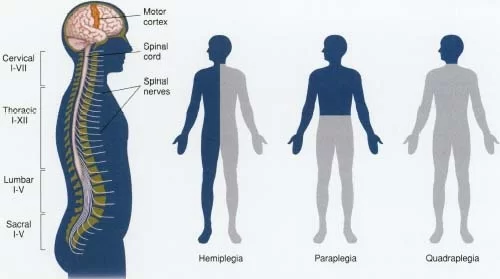
Hemiplegia is the medical term for one side of the body paralysis. It might impact the left or right side of the arms, legs, and facial muscles. It is a symptom of other disorders rather than a separate illness.
Hemiplegia can result from diseases such as brain tumors, traumatic brain injuries, and strokes. It could be either temporary or permanent, depending on the cause.
Treatments aim to treat the underlying disease and assist in restoring muscular mobility.
This article discusses hemiplegia’s types, causes, therapies, and other related topics.
What is Hemiplegia?
- Hemiplegia is paralysis or weakness on one side of the body. The word “hemi” is derived from the Greek word meaning half, signifying that just one-half of the body is affected by hemiplegia. Though there are several possible underlying causes, such as heredity, brain damage is the primary cause of hemiplegia.
- Hemiplegia is the paralysis of one side of the body’s lower face, arm, and leg muscles. Other cognitive, memory, and sensory deficits may also arise in addition to movement issues.
- Hemiplegia is most frequently caused by stroke, which affects one hemisphere of the brain’s corticospinal pathways. Brain tumors, infections, and trauma such as spinal cord injuries are among additional reasons for hemiplegia.
- One often uses the terms hemiplegia and hemiparesis interchangeably because they both produce similar symptoms. Hemiparesis is characterized by mild paralysis on one side of the body, whereas hemiplegia can cause full paralysis on one side of the body along with breathing or speech issues. It could be short-term or long-term, depending on the cause. It could be short-term or long-term, depending on the cause.
- Hemiplegia can develop in an individual or be present from birth. Up until the age of two years, doctors typically diagnose the disease as congenital hemiplegia if the brain injury happens before, during, or shortly after birth. Doctors may refer to an injury that happens later as acquired hemiplegia.
- Treatment for hemiplegia involves addressing the underlying cause and regaining motor function through various therapies. Physical therapy and mirror therapy in particular can help improve motor function in hemiparetic limbs.
- Treating hemiplegia may depend on how and why it occurs. Certain cases don’t require therapy, but others require urgent medical attention to address the hemiplegia’s underlying cause.
One of the most important indicators of a stroke, a potentially fatal medical condition, is hemiplegia. Stroke symptoms can be identified by keeping in mind to think FAST, where
- F stands for the face. Request a smile from the person. A droop on one or both sides of their face indicates muscle weakness or paralysis (facial hemiplegia).
- A-stands for the arm. A stroke generally results in muscular weakness or paralysis on one side. Ask them to lift their arms. If they develop new one-sided weakness or paralysis, one arm will remain up while the other will droop and fall lower or not lift.
- S-stands for speech. Strokes commonly cause people to lose their ability to speak. They may slur their speech or have difficulties choosing the right words.
- T stands for time. Don’t put off seeking assistance since time is of the essence. If possible, glance at your watch or a clock to recall when the symptoms began. Telling a healthcare physician when the symptoms started will help them choose the best therapy choices.
Hemiplegia results from difficulties with your central nervous system. Your central nervous system is made up of two parts: the brain and the spinal cord. Understanding how circumstances produce hemiplegia requires a basic understanding of how your central nervous system operates.
Anatomy of the Central Nervous System
- An important aspect of how your CNS functions is a notion known as “decussation.” This name is derived from the Latin word “discusses,” which stands for the Roman number “X.” Decussation occurs when nerves on opposite sides cross across each other (as in an X) and exchange sides. This occurs in your brainstem, right above where your skull and spine unite.
- Decussation explains why problems on one side of your brain frequently impact the opposite side of your body. Healthcare practitioners refer to this as “contralateral hemiplegia,” which means “opposite-side paralysis.” When you have hemiplegia on the same side, you have “ipsilateral hemiplegia.”
- The sole exception to decussation is when the afflicted nerves do not travel through the region of the brainstem where nerve fibers exchange sides. As a result, hemiplegia manifests variably depending on where in your CNS the problem originates.
Hemiplegia and Hemiparesis: What’s the Difference?
- Similar to hemiplegia, hemiparesis is characterized by a substantial loss of strength and movement on one side of the body, but not total paralysis. Hemiplegia can sometimes emerge following a period of hemiparesis in certain individuals. Others who receive physical therapy may progress from hemiplegic to hemiparetic.
What Differences Exist Between Right and Left Hemiplegia?
- Hemiplegia is defined as a condition in which one side of the body is afflicted; hence, depending on the affected side, it can be referred to as either “left hemiplegia” or “right hemiplegia.”
- It is dependent upon the particular nerve injury that an individual has. As previously said, the brain’s left side governs the right half of the body, and the right side governs the left. Thus, left hemiparesis is more likely to occur from injury to the right hemisphere of the brain than from damage to the left (and vice versa for damage to the left hemisphere).
- Along with a host of other symptoms, a traumatic brain injury (TBI) of any kind can cause partial or total paralysis brought on by the trauma. Therefore, it’s critical to have a thorough medical evaluation after any significant head trauma or other nervous system-affecting incident.
Pathophysiology
- While the precise etiology of hemiplegia is not always clear, oxygen deprivation in the brain causes neurons to die. Damage to the corticospinal tract typically presents on the opposite side of the body
- Hemiplegia, for instance, affects the left side of the body when a person suffers a brain injury to the right. This occurs as a result of the motor fibers of the corticospinal tract, also known as pyramidal fibers, which originate in the brain’s motor cortex, crossing over to the other side in the lower medulla oblongata before descending into the spinal cord to feed the corresponding muscles. The degree of hemiplegia varies according to the location of the brain injury.
- A lesion at the cortex or subcortical level will result in varying degrees of weakness in one half of the body, whereas a lesion in the internal capsule, where all the motor fibers are concentrated in a tiny area, will induce dense hemiplegia, or the total loss of power in all the muscles of one half of the body.
Causes of the Hemiplegia
Conditions That Cause Hemiplegia
- Several illnesses and circumstances can induce hemiplegia. The most prevalent causes are strokes and transient ischemic attacks.
- Aneurysms and hemorrhages inside the brain.
- Concussions and traumatic brain injuries (TBI).
- Spinal Cord Injuries.
- Conditions such as hemiplegic cerebral palsy are caused by injuries sustained at birth or early infancy.
- Childhood alternating hemiplegia is an example of a congenital ailment (one that exists from birth).
- Conditions that cause facial paralysis include Bell’s palsy.
- Seizures with epilepsy.
- Bleeding between your brain’s outer layers (subdural hematomas or subarachnoid hemorrhages) or between your skull and the brain’s outer membrane (epidural hematomas).
- Brain tumors (including cancer).
Strokes
- Strokes are the major cause of hemiplegia in both children and adults. The level of muscular weakness you suffer might vary depending on the size and location of the stroke. Strokes in the womb are the leading cause of hemiplegia in offspring.
- In youngsters, the reasons for a stroke may remain undiscovered. Congenital cardiac disease and numerous hereditary blood coagulation abnormalities, which can result in embolism, thrombosis, or hemorrhage, are two of the most prevalent causes.
Brain infections
- A brain infection can permanently harm the cortex of the brain. The majority of illnesses are caused by bacteria, however, some might also be viral or fungal.
- Certain illnesses, such as meningitis, can cause significant brain damage.
Brain damage
- A quick hit to the head might result in lifelong brain damage. If the damage just affects one side of your brain, hemiplegia may occur. Car accidents, sports injuries, and assaults are among the most common causes of trauma.
- Brain damage can result from blunt force trauma. Falls, physical assaults, automobile accidents, and contact sports all have the potential to cause harm. Hemiplegia can result from damage to only one side of the brain due to trauma.
- In newborns, brain damage may develop in the pregnancy. This can be caused by premature birth, cognitive damage, or a lack of oxygen.
Genetics
- An exceedingly uncommon mutation in the ATP1A3 gene can cause alternating hemiplegia in children. It produces intermittent hemiplegia symptoms. About one million people are afflicted with this illness.
- AHC is an uncommon condition in which a kid has recurring periods of weakness or paralysis on one side of the body. The paralysis may alternate on both sides.
Brain Tumours
- Brain tumors can cause several physical difficulties, including hemiplegia. The symptoms of hemiplegia may worsen as the tumor develops.
- Brain tumors can cause hemiplegia, among other symptoms.
- As the tumor develops, it can cause damage to the brain, resulting in increased symptoms.
Types of Hemiplegia
Types of Hemiplegia include:
Facial Hemiplegia
- Facial hemiplegia causes paralysis of one side of the face’s muscles. Facial hemiplegia may also be associated with mild hemiplegia elsewhere in the body.
Spinal Hemiplegia
- Spinal hemiplegia is also known as Brown-Sequard syndrome. It includes damage to one side of the spinal cord, which causes paralysis on the same side of the body as the lesion. It also results in loss of pain and warmth on the opposite side of the body.
Contralateral hemiplegia
- This refers to paralysis on the opposite side of the body where brain injury has occurred.
Spastic Hemiplegia
- This kind of cerebral palsy primarily affects one side of the body. The muscles on the afflicted side are continually contracting or spasming.
Alternating hemiplegia of childhood
- Children under the age of 18 months are more likely to develop alternating hemiplegia. It results in periodic episodes of hemiplegia on one or both sides of the body.
Symptoms of Hemiplegia
Hemiplegia can occur on either the left or right side of the body.
If the left side of the brain is harmed, paralysis develops on the right side of the body, whereas injury to the right side causes symptoms on the left side.
Symptoms might vary in severity and affect individuals differently. They may include:
- Loss or Lack of Balance
- trouble walking and grasping stuff.
- Impaired coordination
- Muscle fatigue
- A person may also acquire symptoms that are specific to the traumatic brain injury. These might include symptoms like:
- Symptoms may include behavioral changes, speech difficulties, and seizures.
- Problems with focus, memory, attention, or thinking
- confusion, excitement, and restlessness.
- Children with hemiplegia may exhibit delayed walking, tiptoe walking, fisted hands, and favoring one hand over the other before the age of 12.
Diagnosis of Hemiplegia
A physical examination is used to assess hemiplegia and hemiparesis. Your healthcare professional will use a rubber reflex hammer to assess your reflexes and muscular strength. They may also push on your limbs while you try to resist their moves.
Additionally, your doctor may request the following imaging tests and diagnostic procedures:
- X-ray Computed tomography (CT scan) converts X-ray pictures into 3D images.
- Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to build a three-dimensional picture.
- Myelography, contrast dye, and an X-ray or CT scan are used to see the spinal canal.
- Electromyography (EMG) is a tiny needle electrode that monitors muscle activity.
- The nerve conduction study (NCS) analyses the speed of electrical impulses traveling through your nerves.
- A complete blood count (CBC) is a blood test that determines the quantities of blood cells and platelets.
- Weakness or loss of function in your limbs should always be treated immediately. If you have muscular weakness or paralysis, get medical treatment immediately.
Complication of Hemiplegia
Secondary conditions such as hemiplegia and hemiparesis may arise as a result of your weakness. Sometimes these issues are not apparent immediately. Instead, they may appear months after you initially experience weakness or paralysis.
Hemiplegia and hemiparesis can lead to the following complications:
- Bladder difficulties, such as not entirely emptying when you pee or peeing when you don’t want to (incontinence).
- Bowel control issues
- Deep vein thrombosis (DVT) occurs when a blood clot plugs a big vein.
- Autonomic Dysreflexia is a rapid increase in blood pressure.
- Depression
- Respiratory difficulties
- Heart illness.
- Sepsis is an infection in the bloodstream.
- Pressure wounds (also known as bedsores or pressure ulcers) are skin sores that arise when lying in bed.
- Tight, rigid, and inflexible muscles.
- Muscular atrophy (weakness)
Treatment of Hemiplegia
The treatment options for hemiplegia vary depending on the cause and severity of the symptoms. People with hemiplegia frequently get multidisciplinary treatment from physical therapists, rehabilitation therapists, and mental health experts.
Physical therapy
- Working with a physiotherapist assists patients with hemiplegia in improving their balance, strength, and coordination. A physiotherapist can also help you stretch tight and spastic muscles.
Modified constraint-induced movement therapy (mCIMT).
- Modified constraint-induced mobility treatment involves limiting the side of your body unaffected by hemiplegia. This therapy approach challenges your weaker side to compensate while attempting to enhance muscular control and flexibility.
- One tiny study found that using mCIMT in stroke rehabilitation may be more successful than standard treatments alone.
Assistive devices
- Even if you have hemiparesis or hemiplegia, mobility aids can assist you in living an independent and active life.
- Some physical therapists may prescribe using a brace, cane, Manual and electric wheelchairs, or walker. Using an assistive device can aid with muscle control and movement. It is advisable to visit a healthcare practitioner to determine which device is appropriate for you. They may also propose house adaptations like higher toilet seats, ramps, and grab bars.
Occupational Therapy
- Occupational therapy is a sort of treatment that teaches people how to do practical tasks and daily activities including self-care. Occupational therapists may use modified constraint-induced movement therapy. This therapy consists of intense upper-limb muscular training to improve back function in the afflicted arm. Physical therapists may also employ this approach.
Mental imagery
- Imagining moving the paralyzed side of your body may assist engage the brain regions responsible for mobility. Mental imagery is frequently combined with other therapies and is seldom used alone.
- A meta-analysis of research indicated that mental imagery may be a useful therapeutic option for restoring strength when paired with physical therapy.
Electrical stimulation
- A medical expert can stimulate muscle action with electrical pads. Electricity permits muscles that cannot be moved consciously to contract. Electrical stimulation is intended to alleviate imbalances in the damaged side of the brain and increase brain plasticity.
Assistive Technology and Equipment
- Voice-activated devices, computers, telephones, and lighting systems all fall under the category of assistive technology. These are becoming increasingly accessible and practical to utilize. Furthermore, adapted equipment, such as specifically built gadgets for driving, eating, and personal hygiene, might be useful in everyday tasks.
Physiotherapy Treatment for Hemiplegia
Bed Positioning
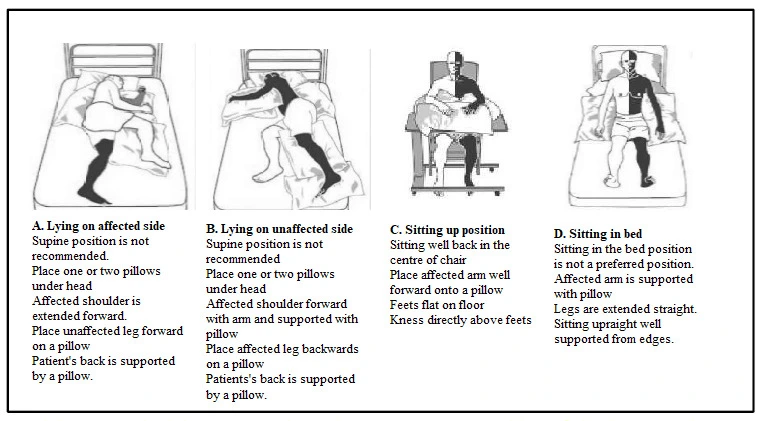
Sitting on The Affected Side:
- A head cushion or two.
- The affected shoulder is in a comfortable position.
- Lean forward on one or two cushions, untouched.
- Pillows behind or in front might provide support.
Sitting on The Unaffected Side
- A head cushion or two.
- hunched over and propped up on a pillow
- Reverse the affected leg on one or two pillows.
- Put a cushion behind.
Sitting in Bed
- Only brief periods are ideal for sitting in bed.
- Needs to be propped up with pillows and standing upright.
- Adding more support by placing pillows beneath the knees or arms.
- When lying on your back, arrange three pillows in a “triangle” to support your head and shoulders.
- Place the afflicted arm on the cushion.
- Maintain a neutral foot stance.
Loosen-up Neck Muscles
- Examine your left shoulder first, then your right.
- Place a hand on your right ear and then your left ear and left shoulder. (Bend your neck instead of raising your shoulder.)
- Raise your head back to an erect posture after bending it forward to place your chin against your chest.
Loosen-up The Shoulder Gardle Muscles
- With your hands in front of you and your elbows bent, sit at the table with your forearms and elbows resting on the surface. Verify that the table and chair don’t have any wheels.
- Sitting up straight and tall, raise your chest towards the table without moving your arms on the table. Then slouch with your chest away from the table. Keep going with this order.
- Place both hands on the table’s towel. Extend your hands straight before you, fully extend your elbows, and incline your head slightly forward.
- Sit up straight again by bringing your hands back in towards your chest. Continue in this order. Using your arms to slide slightly to the right, repeat the same movements. Using your arms to slide slightly to the left, repeat the same movements.
- Place both hands on the table’s towel. When both elbows are straight, slide your hands forward. Now, very slowly move your hands side to side, only as far as your shoulders will allow you to go.
- Place both hands on the table’s towel. Using your hands to slide the towel, create a little circle on the tabletop. Draw a circle that is the width of your shoulders.
Range Of Motion Exercises for Shoulder, Elbow and Wrist
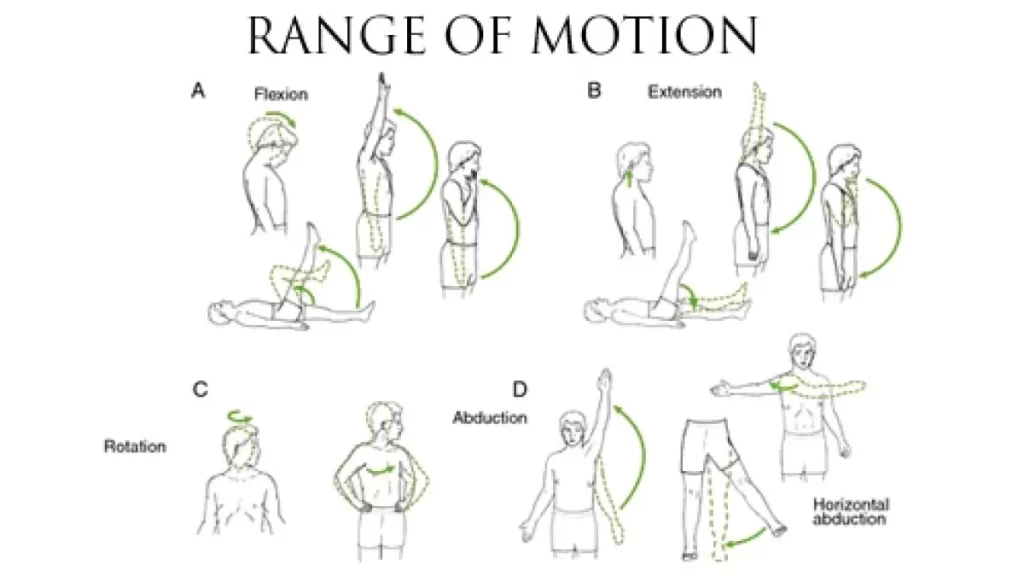
- Place the afflicted hand within the unaffected hand. While maintaining your hands at shoulder or chest level, extend your arms forward to straighten your elbows. Put your two hands back on your chest. Repeat.
- Raise your hands to shoulder or eye level, keeping your elbows straight and your hands together. Repeat.
- Reach your arms between your knees towards the floor while maintaining a straight elbow stance. Next, repeat over your left knee, then your right.
- Place your hands together on the same knee as you sit. Keeping your hands together, bring the back of your right hand to your right knee and the back of your left hand to your left knee. Repeat.
- Keeping your hands together, bend your elbows to bring your hands to your left shoulder; then, straighten your elbows to bring your hands to your right knee. After that, turn around and bring your hands to your left knee, then your right shoulder. Repeat.
- Bend your wrists to the left and then the right while keeping your forearms flat on the table and your thumbs facing up.
- Gently bend your fingers into your palm while your forearm is lying on the table, and then straighten them. You may gently spin your thumb in a full circle while holding the base of your thumb.
Improving Motor Control
Neuro facilitatory techniques
- Bobath: Berta and Karel Bobath’s neurofacilitatory techniques aim to modulate reactions from impaired postural reflex mechanisms. The emphasis is on altered input facilitation and typical movement patterns.
- Rood: Emphasize the usage of developmental sequences, sense stimulation, and muscular work categorization. Cutaneous stimuli including icing, tapping, and brushing are used to assist tasks.
Proprioceptive Neuromuscular Facilitation (PNF)
- Knott and Voss proposed using peripheral cues such as stretch and resistance to enhance existing motor responses.
- Treatment involves the use of whole movement patterns that are followed in a developmental sequence. It was demonstrated that the commutative action of PNF is advantageous to stroke patients.
- Comparing the effectiveness of PNF, Bobath’s technique, and conventional exercise revealed that no one strategy is better than the others.
learning Theory Method
- Conductive Education: In Hemiplegia Physical Therapy, conductive education is used to treat neurological diseases, including hemiplegia.
- Motor Relearning Theory: Carr & Shepherd, both Australian physiotherapists, established this method in 1980. It highlights the need for patients to relearn real-life activities as well as practice functional tasks. It is critical to understand learning principles and conduct biomechanical analyses of motions and activities.
- There is no compelling evidence to support the superiority of one sort of exercise program over another. However, the goal of the therapeutic approach is to promote physical independence and enable motor control of skill learning, and there is good evidence that rehabilitation improves functional independence and reduces mortality.
Functional electrical stimulation (FES):
- Functional electrical stimulation (FES) involves delivering a brief electrical current to the hemiplegic muscle or nerve.
- In Hemiplegia Physical Therapy, FES has been shown to improve motor control, and spasticity, and reduce hemiplegic shoulder discomfort and subluxation. It has been determined that FES can improve acute stroke patients’ upper extremity motor recovery.
- FES may relieve spasticity in stroke patients. A recent meta-analysis of randomized controlled trials found that FES increases motor strength.
- FES can enhance arm function, electromyographic activity of the posterior deltoid, and range of motion, and reduce the severity of subluxation and hemiplegic shoulder discomfort.
Biofeedback
- Biofeedback is a technique that uses visual or aural cues to help individuals recognize electromyographic activity in specific muscles or joint positions. Biofeedback experiments in Hemiplegia Physical Therapy have produced disputed results.
- A meta-analysis of eight randomized controlled trials of biofeedback therapy found that electromyographic biofeedback improved motor function in hemiplegic patients.
- Another meta-analysis research on EMG found that EMG biofeedback is better than conventional treatment alone for increasing ankle dorsiflexion muscular strength. It is also shown that biofeedback might enhance early postural control to correct poor seated balance.
Tone Management
- Tone management is an objective of hemiplegia. Physical therapy approaches have aimed to “normalize tone to normalize movement.” Stretching, extended stretching, passive manipulation by therapists, weight-bearing, ice, contraction of muscles antagonistic to spastic muscles, splinting, and casting are some of the therapy techniques used to reduce tone.
- Manually stretching finger muscles, using pressure splints, and taking dantrolene sodium do not appear to enhance motor control over time.
- Dorsal resting hand splints decreased spasticity more than volar splints, however, the effect on motor function is unclear, whereas TENS stimulation improved chronic spasticity in the lower limbs.
Sensory Re-education
Bobath and other therapeutic techniques suggest using sensory stimulation to help hemiplegic individuals restore their sensory function.
Gait-Training
Hemiplegic Gait Intervention seeks to improve walking performance by preventing adaptive changes in lower limb soft tissues.
- They are inducing voluntary activation in major lower-limb muscle groups.
- Improving muscular strength and coordination.
- Increasing walking speed and endurance.
- Maximizing talent means improving flexibility.
- Increasing cardiac fitness.
The primary focus in walking training is on:
- Support for the body mass across the lower limbs.
- Propulsion of the body mass.
- Balance of body mass as it moves through one or both lower limbs
- Controlling knee and toe pathways for foot clearance and placement
- Optimizing rhythm and coordination.
Conventional Gait Training
Conventional gait training involves practicing certain gait components before walking. It comprises
- Symmetrical Weight-bearing training.
- Weight shifting
- Stepping training (swinging and clearing)
- Heel strike.
- Standing on only one leg
- Push off / Calf raise.
The next phase is circuit training, which includes sitting and standing exercises, step-ups, heel lifts, isokinetic strengthening, walking over obstacles, and up and down hills.
Traditional treatments for stroke rehabilitation rely on neurofacilitation or neurodevelopmental techniques (NDT) to reduce excessive tone, promote muscular activation if hypotonia exists, and enable normal movement patterns using hands-on procedures.
Berta Bobath’s framework remains the major physical therapy approach to stroke victims in the UK, as well as in Canada, the United States, Europe, Australia, Hong Kong, and Taiwan. The Bobath framework has expanded from its basic principles; nonetheless, therapists who questioned the fundamental Bobath aspects continue to emphasize normal tone and the need for normal movement patterns in performing functional activities. Strength training for better walking abilities. Task-specific training to enhance walking ability.
Treadmill Training
Treadmill training was a pioneering method for gait rehabilitation following hemiplegia, utilizing body weight support.
Prevention of Hemiplegia
Hemiplegia typically occurs unexpectedly. As a result, there is no permanent solution. However, you may lower your chances of developing hemiplegia by avoiding factors or situations that can lead to it.
- To improve your health, try eating a balanced diet and maintaining an appropriate weight.
- Many circulatory and heart-related disorders, including stroke, can induce brain injury, resulting in hemiplegia. Preventing strokes and other related diseases is an important method to lower your chance of getting hemiplegia.
- Manage your medical problems. Chronic illnesses such as Type 2 diabetes, high blood pressure, and epilepsy increase your chance of developing hemiplegia. Managing these circumstances is critical for reducing your likelihood of acquiring this symptom. Managing illnesses that might cause progressive damage to your brain or spinal cord over time, such as multiple sclerosis, is also critical.
- Do not overlook infections. Infections, particularly those affecting your eyes and hearing, can result in hemiplegia if they travel to your brain. Getting immediate treatment for infections, and then adhering to treatment instructions as strictly as possible, might lower your chances of this occurring.
- Wear safety equipment. Protective equipment, particularly helmets and safety restraints (such as seat belts), can help you avoid head, neck, and back injuries that could result in hemiplegia.
Summary
Hemiplegia and hemiparesis are two disorders that result in weakness on one side of the body. Hemiplegia occurs when a weakness causes paralysis, whereas hemiparesis is a partial weakness.
These diseases are caused by a variety of factors, but they are typically the result of an injury or sickness to the spinal cord or brain. Physical and occupational therapy can occasionally help persons regain their mobility. Mobility aids and assistive technologies enable people to stay independent and active.
FAQs
Can you have a regular life with hemiplegia?
For others, hemiplegia symptoms may be temporary (or improve with time). Others may live with all of their symptoms for the remainder of their life. Symptoms may be mild, with the hemiplegic having little control over the weakest side of the body.
Which pill is most effective for a brain stroke?
Antiplatelets also keep platelets from adhering together, which prevents clots from forming. Aspirin is the most well-known example. If you’ve had an ischemic stroke or TIA, you may need to take aspirin or other antiplatelet medications for the rest of your life.
Who develops hemiplegia?
Falls, physical assaults, automobile accidents, and contact sports all have the potential to cause harm. Hemiplegia can result from damage to only one side of the brain. In fetuses, pregnancy may cause brain injury. This can be caused by premature birth, cognitive damage, or a lack of oxygen.
Can stress induce hemiplegia?
Certain meals, odors, intense light, little or excessive sleep, physical effort, stress, or mild head trauma are all potential triggers for hemiplegic migraine.
What is the difference between hemiplegia and hemiparesis?
Hemiplegia refers to total paralysis, whereas hemiparesis refers to partial weakening.
How does one cure a hemiplegic stroke?
Some stroke survivors may take a blood thinner to lower their risk of blood clots, which might lead to another stroke. Stroke survivors can also benefit from physical therapy, occupational therapy, and speech and language therapy to aid with hemiplegia management.
Is it possible to cure hemiplegia?
Hemiplegia may be addressed based on how and why it occurs. In some situations, no therapy is required, while others require quick medical attention to reverse the source of the hemiplegia. Hemiplegia is a major indicator of a stroke, which is a life-threatening medical emergency.
References
- SpinalCord.com. (2020, December 22). Living with Hemiplegia and Hemiparesis: Causes, Treatment + Coping. Spinal Cord, Inc. https://www.spinalcord.com/hemiplegia,
- Professional, C. C. M. (n.d.-h). Hemiplegia. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/23542-hemiplegia
- Yetman, D. (2020, January 27). Hemiplegia: causes and treatments for partial paralysis. Healthline. https://www.healthline.com/health/hemiplegia#treatment
- Hemiplegia. (n.d.). Physiopedia. https://www.physio-pedia.com/Hemiplegia
- Fletcher, J. (2022, October 6). Everything you should know about hemiplegia. https://www.medicalnewstoday.com/articles/hemiplegia#treatment
- Vega, J., MD Ph.D. (2022, August 7). What are hemiplegia and hemiparesis? Verywell Health. https://www.verywellhealth.com/information-about-hemiplegia-3146139

[…] Hemiplegia is one of the symptoms of cerebral vascular disease (CVD). There is a foot drop in this presentation. Additional indications of involvement of higher motor neurons include hyperreflexia, circumduction of the lower extremities while walking, and elevated muscular tone. Depending on where the ischemia occurs, aphasia may manifest. […]
[…] therapy (NDT), is a widely recognized idea for the rehabilitation of stroke patients with hemiplegia in several […]