Heel Pain a Sign of Diabetes?
Introduction:
For diabetics, foot injuries can be an important issue. Although diabetic heel pain can strike anyone at any age, older persons with diabetes who have had the disease for a longer time are more likely to experience it.
Diabetic heel pain may result from problems such as peripheral neuropathy or impaired circulation, which are more common in older adults with diabetes. Furthermore, individuals who have uncontrolled blood sugar levels for a long time may also be more susceptible to diabetic foot issues, such as heel pain.
Up to 25% of diabetics report having foot pain, with heel pain being one of the most prevalent forms, according to a study published in the Journal of Foot and Ankle Research.
About 10% of diabetics have foot pain primarily connected to plantar fasciitis, a condition that can produce stiffness or throbbing pain in the foot and heel arch, according to another study published in the journal Diabetes Care.
Although there isn’t much information on diabetic heel pain specifically, diabetic foot problems are a typical consequence of diabetes, and heel pain can be a sign of several conditions related to diabetic foot difficulties.
Maintaining a healthy lifestyle, which includes controlling your blood glucose levels, is crucial for protecting your feet.
Taking appropriate care of your feet is essential to preventing foot injuries. This includes avoiding being barefoot, wearing supportive, well-fitting footwear, and often checking your feet for wounds, sores, and other injuries. If you do observe any problems, you should get medical help right away.
What Causes Heel Pain in Diabetics?
- Because neuropathy impairs nerve function, it can result in pain, tingling, and numbness in the heels. Usually, pain is greatest at night or after prolonged standing.
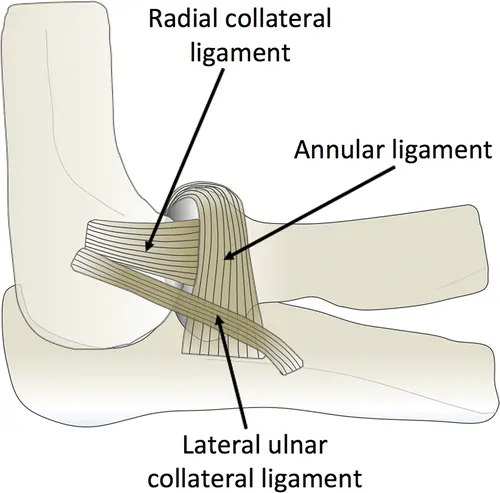
- Achilles Tendonitis: Diabetes can alter the Achilles tendon, resulting in tendonitis, heel pain, and inflammation. Inappropriate footwear, biomechanical problems, or repetitive strain on the tendon can all lead to Achilles tendinitis.
- Infections: Osteomyelitis, an infection of the bones, or cellulitis, an infection of the skin and tissues, can cause heel pain.
- Poor Circulation: Diabetes can result in poor circulation, which can cause pain in the heels and other parts of the body and hinder the body’s capacity to heal.
Symptoms of Heel Pain Are a Sign of Diabetes:
Depending on the type, diabetic foot issues might present with different symptoms. However, generally speaking, you should be aware of the following signs:
- Frequent bleeding.
- Discharge of fluid or pus.
- Foul smell.
- Pain.
- Skin discoloration.
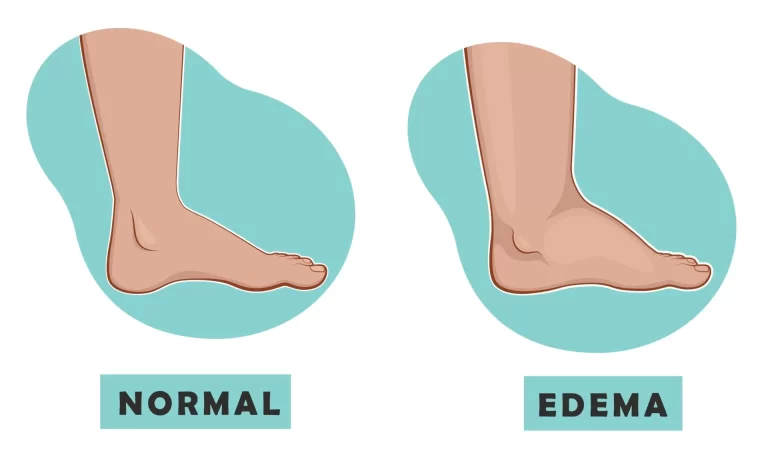
- Swelling.
How Can Diabetic Heel Pain Be Treated?
Diabetic heel pain may be treated using the following options:
- Wearing the right shoes: Shoes that fit well and offer adequate support and cushioning can help ease pain and lessen pressure on the heels.
- Custom orthotics: By distributing weight more evenly across the foot, custom shoe inserts can lessen the strain on the heels.
- Physical therapy: Strengthening and stretching techniques can assist in increasing the range of motion and lessening pain.
- Medication: To assist in reducing inflammation and relieving pain, doctors may prescribe topical creams or nonsteroidal anti-inflammatory medicines (NSAIDs).
- Surgery: To address underlying foot abnormalities or other problems that are causing heel pain, surgery may be required in extreme circumstances.
- Laser Therapy: Laser therapy increases circulation, reduces pain, and speeds up healing. The procedure doesn’t hurt, and it can even relieve your pain right away!
- Pain management: Anti-inflammatory drugs and over-the-counter or prescription painkillers may be able to aid with heel pain. Since topical pain relievers don’t conflict with prescription drugs, they might be a better choice. It’s imperative to speak with a healthcare provider before taking any drug.
- Daily Foot Care Routine: Examine your feet. Heel pain can be reduced and complications can be avoided by establishing a regular foot care regimen that includes daily foot washing, drying, and moisturizing.
- Blood Sugar Control: Reducing the risk of problems, such as heel pain, requires appropriate diabetes control to maintain ideal blood sugar levels. Individuals who have superior blood sugar control recover from injuries faster.
Blood glucose control is particularly crucial because it might make diabetic heel pain worse. Frequent examinations of the feet are also necessary to spot any indications of foot issues, like infections or ulcers, which can aggravate or cause heel pain.
The most effective treatment for diabetic heel pain is a multifaceted strategy that includes medication, lifestyle modifications, and other interventions according to each patient’s needs.
Prognosis:
Your perspective is influenced by things like:
- The presence of an infection and its rate of transmission.
- Efficacy of treatment.
- Based on your particular circumstances, your healthcare professional will give you a clearer understanding of what to anticipate.
Prevention:
To try to prevent or postpone diabetes-related neuropathy and blood flow problems, it is crucial to properly manage your blood sugar and diabetes. For assistance with your diabetes treatment plan, consult your healthcare practitioner (such as an endocrinologist) frequently.
As your life changes, so will your pharmaceutical requirements. Additionally, inquire about any helpful developments in diabetes treatment technologies, such as continuous glucose monitoring (CGM).
- Daily foot check: Keep an eye out for any changes and remember to inspect between your toes.
- Maintaining the filing and trimming of your toenails: To avoid ingrown toenails, trim your nails straight across with clippers. Then, use a nail file to gently flatten any sharp edges.
- Wearing properly fitting shoes and socks: Verify that your shoes fit correctly and that your socks aren’t excessively tight. In order to help avoid ulcers or sores, some diabetics wear orthopaedics, or therapeutic shoes. Before putting on your shoes, be sure there are no stones or other things within.
- To prevent burns, keep your feet away from open fires and heaters. To keep your feet warm in cooler weather, wear insulated shoes and socks.
- Keeping your feet up when you sit and frequently wriggling your toes are two ways to maintain blood flow to your feet. Continue to be active, but pick more foot-friendly pursuits like swimming or walking.
- Daily foot washing and moisturization: Make use of warm water, not hot. After that, make sure to completely dry them, including in between your toes. Next, put lotion on your feet’s tops and bottoms, avoiding the space between your toes.
- Request that your doctor examine your feet each time: Request a visual examination of your feet from your healthcare physician. Get a comprehensive foot examination (also known as a diabetes foot exam) at least once a year, which should include a check of your feet’s sensation and pulse.
FAQs
Is there a permanent cure for diabetes?
No, there is no long-term cure for diabetes. There is presently no full and permanent cure, although it can be properly treated and put into remission with medical interventions and lifestyle adjustments.
How can I lessen pain in my heels?
To lessen pain and swelling, place an ice pack covered with a cloth over the affected area for 15 minutes, three or four times a day. Extend your arches. You can stretch your calf muscles, Achilles tendon, and plantar fascia easily with easy at-home workouts.
What is the source of heel pain?
Vitamin D and B12 deficits, as well as calcium shortages, can be linked to heel pain. These inadequacies can induce plantar fasciitis, which causes heel pain, or weaken bones, which can result in disorders like stress fractures.
Why is my heel hurting now?
Obesity, poorly fitting shoes, running and jumping on hard surfaces, irregular walking patterns, traumas, and certain condition are some of the common reasons for heel pain.
Why am I experiencing heel pain now?
Heel pain may arise from the thickening of the plantar fascia caused by abrupt or recurring stressors. Additionally, the heel bone and surrounding muscles may be affected.
How can diabetes be reversed?
Some people may be able to reverse type 2 diabetes by making major lifestyle changes, mainly losing weight and being more active. By using these techniques to bring blood sugar levels down to a healthy range, type 2 diabetes can be put into remission, although it is not a cure.
Why is my heel hurting now?
It happens when your foot’s fascia, which is the connective tissue that runs along the plantar surface, tears, strains, and becomes inflamed. Common irritants include treadmills and harsh surfaces (such as concrete) used for work or exercise.
Is it possible to heal diabetic foot pain?
Nerve damage in diabetics is known as diabetes-related neuropathy. Peripheral neuropathy is the most prevalent kind and frequently affects the feet. Diabetes-related neuropathy has no known treatment. However, you can control it with medicine, counseling, and stricter blood sugar control.
Does diabetic foot pain indicate diabetes?
Although there isn’t much information on diabetic heel pain specifically, diabetic foot problems are a typical consequence of diabetes, and heel pain can be a sign of several conditions related to diabetic foot difficulties.
How can I be active in Florida and avoid diabetic heel pain?
Avoid going barefoot (even at home or on the beach), wear supportive, breathable shoes, and look for redness or sores on your feet every day. Heel pain can also be avoided by controlling your blood sugar levels and maintaining an active lifestyle with low-impact activities like swimming.
What should I look out for in the early stages of diabetic heel problems?
Watch for redness, stiffness, burning, swelling, or heel pain in the morning. Always check your feet after a long day outside if you’re in Florida’s hot and muggy climate, since moisture can worses issues.
Why do diabetics frequently get heel pain?
Being active is a way of life in Florida’s warm climate, but diabetics may find foot care challenging. Because high blood sugar can impede blood flow and harm nerves (a condition known as peripheral neuropathy), your heels are more susceptible to pain, inflammation, and even severe injury.
References:
- Ankle, C. F. &. (2025, April 14). Heel pain and diabetes: causes, treatment, and prevention tips. Certified Foot & Ankle Specialists. https://certifiedfoot.com/heel-pain-diabetes-causes-teatment-prevention/
- Diabetes-Related foot Conditions. (2025, June 2). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21510-diabetic-feet
- Center, L. F. &. A. (2024, October 22). Soleful Struggles: Managing Heel Pain in Individuals Living with Diabetes — LIGHTHOUSE FOOT & ANKLE CENTER. LIGHTHOUSE FOOT & ANKLE CENTER. https://lighthousefootandankle.com/blog/2023/10/27/soleful-struggles-managing-heel-pain-in-individuals-living-with-diabetes
- Dpm, T. P., & Dpm, T. P. (2018, January 22). Diabetes and heel pain. Capital District Podiatry. https://capitaldistrictpodiatry.com/blog/diabetes-heel-pain/