Ankle Joint
Ankle joints are complex mechanisms that play important roles in allowing movement in the lower extremities and providing stability. Several ligaments support the ankle’s overall stability by joining the bones and ensuring optimal joint function.
The anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), and calcaneofibular ligament (CFL) comprise the lateral (outside) portion of the ankle joint. These ligaments contribute lateral support to the ankle by attaching the talus and calcaneus, two-foot bones, to the fibula, one of the two lower leg bones.
Ankle ligament overstretching or taking produces a sprain. Ankle sprains are a common problem that can either worsen or heal quickly.
Introduction Of Ankle Joint
Your shin bone (tibia), calf bone (fibula), and talus bone relate to the ankle joint. It attaches to your lower leg and foot. Further, your ankle comprises blood vessels, muscles, ligaments, cartilage, and nerves. You use your ankles when moving your feet and legs in two main ways.
The joint enables both plantarflexion and dorsiflexion of the foot, acting as a hinge.
The talus, tibia, and fibula bones interact to form the ankle joint, which is a hinged synovial joint. Ankle mortise is determined by these three boundaries.
- The bony protrusion on the lower fibula, known as the articular facet of the lateral malleolus, forms the longer side of the ankle joint.
- The lower tibia’s bony protrusion, the articular facet of the medial malleolus, establishes the joint’s medial border.
- The inferior articular surface of the tibia and the superior border of the talus combine to form the superior portion of the ankle joint.
The calcaneus and navicular articulate inferiorly and anteriorly, as well, with the talus.
- Ankle dorsiflexion and plantarflexion are allowed given the upper surface, defined as the trochlear surface, being rather cylindrical.
- The talus has a greater anterior diameter and a more posterior narrowing.
- The ankle is most durable in dorsiflexion when it forms a wedge that stands between the lateral and medial malleoli.
Anatomy of the Ankle joint
The 26 distinct foot bones that comprise the foot and ankle, as well as the long bones of the lower limb, join to form 33 joints. The talocalcaneal frequently referred to as a subtalar joint, the tibiotalar, formerly known as a talocrural, and the transverse-tarsal, also called a talocalcaneal navicular joint, comprise the ankle joint complex.
The subtalar joint
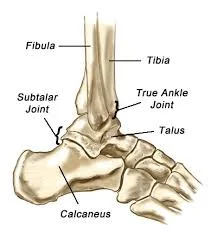
- The calcaneus, the biggest, strongest, and most posterior bone in the foot, connects to the Achilles tendon in the lower thighs.
- This is located inferiorly to the talus bone and joins the talus in the lower leg to form a tri-planar, uniaxial joint. The talus bone is maintained by the anterior part of the calcaneus bone.
- The facets for the articulation of the posterior talocalcaneal joint are concave on the inferior surface of the talus bone and convex on the superior surface of the calcaneus. On the superior aspect of the calcaneus bone, the two similarly articulated facets of the anterior talocalcaneal joint are concave and strong, while on the inferior aspect of the talus bone, they are convex and strong.
- The ankle may rotate in both directions due to its geometry, although this joint can also move in a different path. The two bony parts are attached by a multitude of ligaments.
- The interosseous talocalcaneal ligament, a strong, wide, and thick ligament that binds the superior aspect of the calcaneus bone to the articular facets of the inferior talus bone, is the most important ligament separating the two.
- Talocalcaneal ligaments, both anterior and lateral, provide additional support for the fixed position of the subtalar joint.
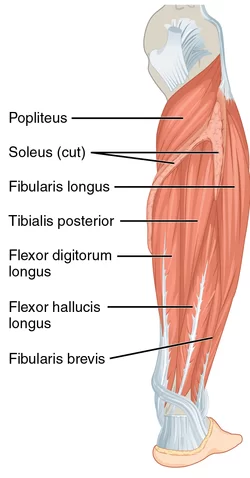
- The talocalcaneal joint is further stabilized by the lateral collateral ligament of the ankle joint and the interosseous talocalcaneal ligament. Additional support is offered by the long tendons of the flexor hallucis longus, tibialis posterior, peroneus longus, and flexor digitorum longus muscles.
The tibiotalar joint
- It is well-known for being a talocrural joint. The distal tibia and fibula bones of the lower leg and the talus bone of the foot collaborate at the tibiotalar joint, formerly referred to as the talocrural joint.
- Here, the weight is maintained via the tibial-talar interaction. The talus bone in the foot does not directly connect to the head, neck, or torso through muscles.
- The talus bone’s trochlea was developed to fit into the mortise formed by the distal ends of the long shin bones of the lower leg. The talus bone is constrained by the malleoli of the tibia and fibula bones, causing the joint to operate as a hinge joint. The main functions of this joint are to help the foot’s dorsiflexion and plantar flexion. However the joint’s geometry—the trochlear surface’s cone shape and the oblique rotation axis—indicates that it may not function as a hinge joint isolated.
- Dorsiflexion may improve joint stability because the talus is located in the anterior region. The greatest shape of the tibiotalar joint seems to have a bearing on the stability of the ankle joint. The soft tissue parts of the ankle joint provide stability when the ankle joint’s geometry alone isn’t sufficient for resisting eversion motion during the stance phase.
- A capsule connecting the talus bone inferiorly, the tibia malleoli, and the superior tibia bone control the diarthrosis that approaches the tibiotalar joint.
- Three ligamentous groups give stability to the ankle joint.
- To maintain stability between the tibia and fibula’s bone ends, the tibiofibular syndesmosis restricts movement between the tibia and fibula bones during regular activities.
- The anterior tibiofibular, posterior tibiofibular ligament, and interosseous tibiofibular joint are the three aspects of the syndesmosis. The medial collateral ligaments, formerly known as the deltoid ligaments, support the medial surface of the ankle joint and are mainly responsible for avoiding eversion motions and valgus stresses within the joint.
- The anterior and posterior tibiotalar ligaments, the talonavicular ligament, and the talocalcaneal ligament compose the fan-shaped deltoid ligament, referred to as the medial collateral ligament.
- By limiting varus a lot and decreasing rotation, the lateral collateral ligaments decrease the joint’s ability for inversion. This structure consists of the anterior and posterior talofibular ligaments, as well as the calcaneofibular ligament. Plantar flexion and dorsiflexion, respectively, provide significant strains to the anterior and posterior ligaments, respectively. These ligaments give stability to the lateral tibiotalar joint and are frequently damaged during inversion injuries, such as injuries of the ankle. The tibiotalar and subtalar joints are united by the calcaneofibular ligament, which is the only direct connective tissue.
Inferior tibiofibular joint
- In some literature, the inferior tibiofibular joint is considered an essential part of the tibiotalar joint, while it may be considered a distinct joint. The interosseous membrane and fibrous tissue connect the two distal parts of the fibula and tibia joints; it is not a synovial type articulating joint.
- Adding stability rather than facilitating bigger lower limb movement at the foot and ankle is the primary goal of the inferior tibiofibular joint. The tibia and fibula bones connect by the anterior, posterior, and interosseous tibiofibular ligaments, as previously stated.
- Ankle fractures and eversion injuries usually involve the ligamentous structure that reduces the joint, rendering it highly susceptible to damage.
Transverse tarsal joint
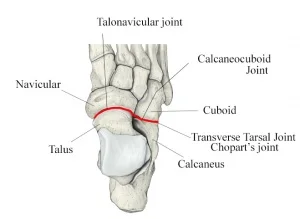
The talus and navicular bone junction, where the talar head articulates with the posterior surface of the navicular bone anteriorly, and the calcaneocuboid joint, which becomes the calcaneus and cuboid bones come together to form the transverse tarsal joint, also known as Chopart’s joint. As this joint and the subtalar joint share an axis for movement and both assist in the eversion-inversion action of the foot, they are considered to form the same functional unit.
Structure of ankle joint
- The ankle joint plays an essential part in ambulation as it responds to the walking surface.
- The ankle joint can move in any of these directions: dorsiflexion, eversion, inversion, and plantar flexion.
- It is known that the leg muscles have anterior, posterior, and lateral compartments.
Articulating Surfaces of the ankle joint
- Three bones contribute to the complex ankle joint: the trochlear surface of the talus (the foot bone), the lateral malleolus of the fibula (the leg bones), and the distal end of the tibia attached to the medial malleolus. Hyaline cartilage keeps an ankle joint’s articular surfaces in contact.
- The ankle joint consists mainly of three articulations:
- Tibiofibular ligaments, which are situated at the distal end of the lower leg, completely attach the tibia and fibula, or leg bones. The tibia and fibula join creating a socket with a bracket-like shape that is covered in hyaline cartilage. We describe it as a mortise (socket).
- The talus’s body slides easily into the groove formed by the lower leg’s bones. The talus’s articulating component has a wedge-shaped shape that is expansive in front and thin in back.
- Dorsiflexion and plantarflexion of the foot are made possible by the ankle joint, which is connected to some inversion and eversion through the subtalar and midtarsal joints. Whenever the heel contacts the ground at the initial stages of walking, the ankle joint also serves as a shock absorber.
The joint capsule of the ankle joint
The superior capsule of the ankle joint connects to the articular surfaces of the medial malleolus of the tibia and the lateral malleolus of the fibula. The margins of the talar trochlear surface establish the capsule inferiorly. The ankle joint capsule is thin and somewhat fragile. strengthened laterally and medially, still by strong collateral ligaments. The synovial membrane continues into the distal tibiofibular joint and protects the interior of the ankle joint capsule up to the interosseous tibiofibular ligament.
Ligaments of the ankle joint
The ankle joint requires to be stabilized because it bears a lot of weight, but only to the extent that maximum movement is still allowed. The lateral collateral and medial collateral ligaments are the ligaments that help stabilize the ankle joint.
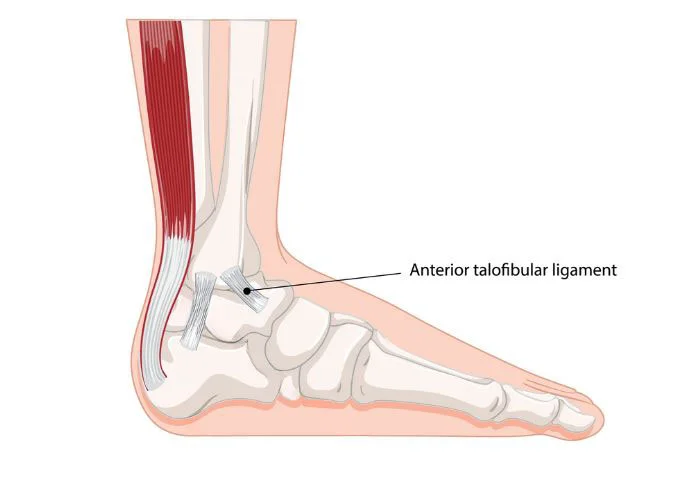
Lateral collateral ligament
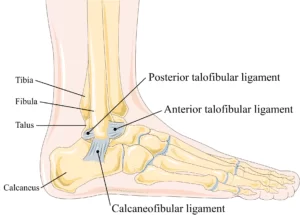
- The lateral aspect of the ankle joint is stabilized by the robust and broad lateral collateral ligament. It is built from three distinct brands:
- Anteromedially, the anterior talofibular ligament extends from the lateral malleolus of the fibula to the lateral side of the talus’s neck. It acts as a weak, flat band. The ankle joint ligament is often injured.
- Function: Protect the talus bone from moving anteriorly concerning the tibia and fibula bones. Refuses to Invert when performing plantarflexion.
- The posterior talofibular ligament is a muscular band that joins the lateral tubercle of the talus to the distal section of the lateral malleolar fossa on the fibula. It extends both medially and posteriorly. There is a tibial slip of fibers which links it to the medial malleolus. Ligaments are rarely damaged since the ankle’s dorsiflexion protects them from injury due to bone stability.
- Function: Forms the trochlear of the talus recipient socket’s posterior wall. Prevent talus bone posterior displacement.
- The calcaneofibular ligament is a strong, complex band that extends posteroinferiorly from the apex of the fibula’s lateral malleolus to a tubercle on the lateral side of the calcaneus.
- function: Provides help with talofibular stability during dorsiflexion. Limit the calcaneus’ inversion concerning the fibula. Avoid talar tilting into an inverted position.
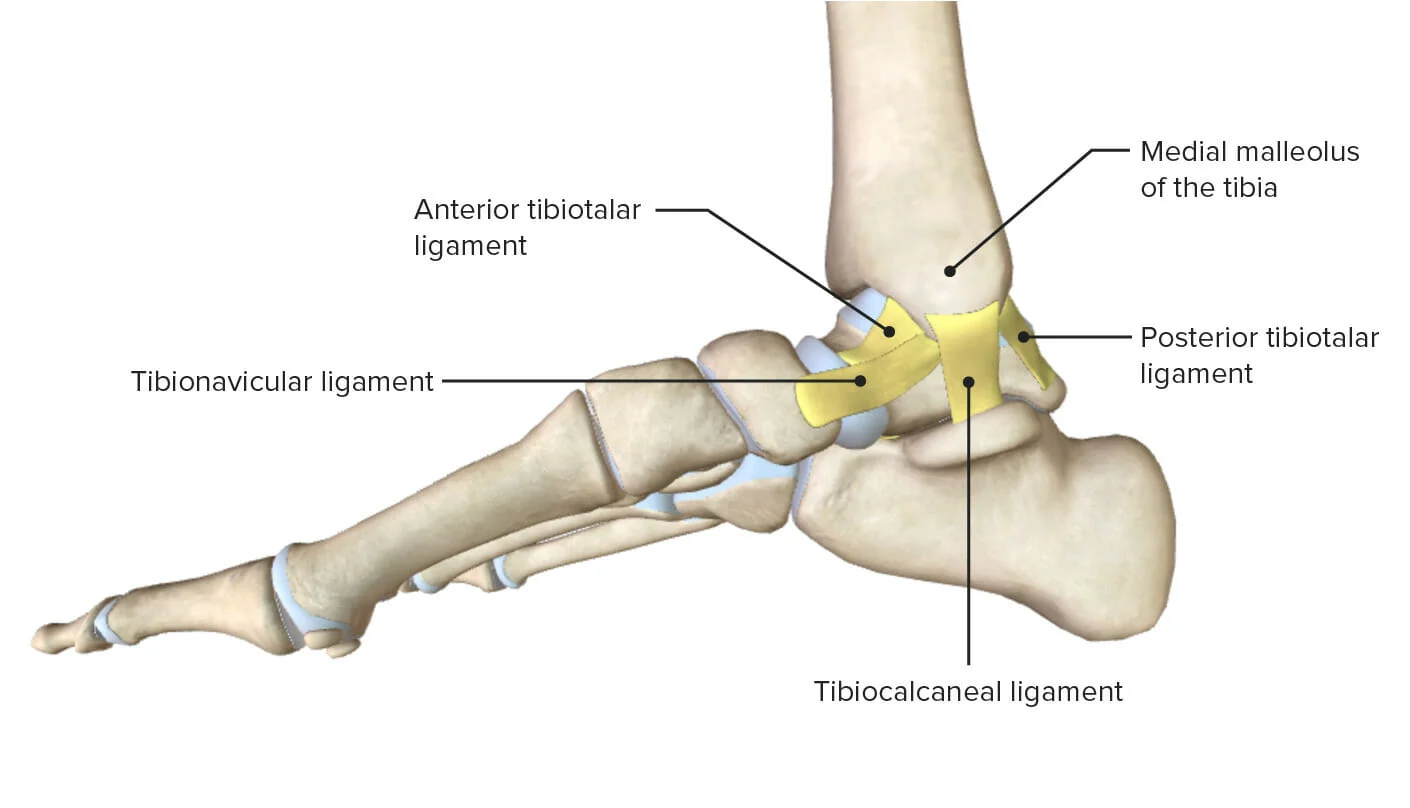
Medial collateral ligament
Another name for the medial collateral ligament is the deltoid ligament. The medial portion of the ankle joint is strengthened by this lengthy, robust, triangular band. Avoiding ankle joint dislocations (over-eversion) and stabilizing the ankle joint in eversion is important. The proximal ends of the medial malleolus and its apex are where the medial collateral ligament is tethered. The ligament then spreads outward to fasten to the foot’s talus, calcaneus, and navicular bones. The medial collateral ligament is typically divided into three continuous segments according to the distal attachment locations, however, the fact that it can be very variable and consist of three to six aspects ranging from the superficial to the deep parts:
- Tibionavicular ligament: The sum of the superficial fibers of the ankle joint’s medial collateral ligament that descend from the medial malleolus and attach distally to the foot’s navicular bone’s tuberosity. From the attachment site, the talonavicular ligament connects with the medial border of the plantar calcaneonavicular ligament.
- The talocalcaneal ligament is formed out of the intermediate region of the ankle joint’s medial collateral ligament, which originates from the medial malleolus nearly vertically downward and attaches to the sustentaculum tali.
- Tibiotalar ligament: This ligament is a structure made up of the medial collateral ligament’s deep section. Both an anterior and a posterior part are present. Both start at the apex of the tibia’s medial malleolus. From there, the posterior tibiotalar ligament joins to the non-articular posterior portion of the medial talar surface, while the anterior tibiotalar ligament descends to attach to the medial tubercle of the foot’s talus bone.
Muscles of the ankle joint
Which muscles in the ankle generate plantarflexion at the ankle joint?
- Gastrocnemius
- Soleus
- Flexor hallucis longus
- Flexor digitorum longus
- Tibialis posterior
- Peroneus Brevis
- Peroneus longus
Which muscles in the ankle produce dorsiflexion at the ankle joint?
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
Gastrocnemius
- Origin: Above the lateral and medial condyles of the femur, on the lower posterior border of the femur bone.
- Insertion: The Achilles tendon descends into the posterior side of the calcaneus bone.
- Movement: Plantarflexion.
- Nerve supply: Tibial nerve.
Soleus muscle
- Origin: The upper third of the posterior fibula and the upper half of the posterior end of the tibia bone, along with the sole line.
- Insertion: Through the Achilles tendon at the ankle, the posterior side of the calcaneus bone is exposed.
- Actions: Plantarflexion.
- Nerve supply: Tibial nerve.
Flexor Hallucis Longus muscle
- Origin: The lower two-thirds of the posterior surface of the fibula bone.
- Insertion: The sole base of the first metatarsal’s distal, or farthest, phalange.
- Actions: Plantarflexion, Inversion, and Big Toe Flexion.
- Nerve supply: Tibial nerve.
Flexor Digitorum Longus muscle
- Origin: The bottom two-thirds of the tibia bone’s back surface.
- Insertion: Plantar (bottom) aspect of the base of the second, third, fourth, and fifth metatarsal phalanges, which are the farthest.
- Three movements: toe flexion, inversion, and plantarflexion.
- Nerve supply: Tibial nerve.
Tibialis Posterior
- Origin: Interosseous membrane, which stretches between the fibula and tibia bones. lower leg bones near to the interosseous membrane are the fibula and the posterior side of the tibia.
- Insertion: Second, third, and fourth metatarsal bones of the foot; cuneiforms; cuboid; navicular tuberosity of the navicular bone.
- The ankles are inverted and plantarflexed.
- Nerve supply: Tibial nerve.
Peroneus brevis muscle
- Origin: Its tendon approaches the lateral malleolus of the fibula by wrapping posteriorly and going upward from the distal 2/3 of the lateral fibula.
- Insertion: At the proximal end of the 5th metatarsal, on the styloid process.
- Nerve supply: Superficial Peroneal nerve.
- Action: Planterflexion and eversion.
Peroneus Longus muscle
- Origin: The upper second third of the fibula and the head of the bone.
- Insertion: The undersides of the cuneiforms and the base of the primary metatarsal.
- Actions: Eversion and Plantarflexion.
- Nerve supply: Superficial peroneal (fibular) nerve.
Tibialis Anterior Muscle
- Origin: Tibia bone (superior and inferior portions).
- Insertion: Foot’s medial cuneiform bone and first metatarsal beneath the surface.
- Action: Dorsiflexion and inversion.
- Nerve supply: Deep peroneal nerve.
Extensor Hallucis Longus muscle
- Origin: Midway on the inner surface of the fibula bone’s anterior two-thirds.
- Insertion: The first metatarsal distal phalanx.
- Actions: Inversion, dorsiflexion, and big toe extension.
- Nerve supply: Peroneal (fibular) nerve.
Extensor Digitorum Longus muscle
- Origin: The interosseous membrane (between the tibia and fibula), the head and anterior surface of the fibula, and the lateral condyle of the tibia bone.
- Insertion: The middle and last phalanges of the four outer toes are situated on the dorsal (top) surface.
- Actions: Dorsiflexion, eversion, and toe extension.
- Nerve supply: Peroneal (Fibular) nerve.
Blood supply of the ankle joint
The aortic arch and posterior fibular and tibial arteries deliver arterial blood to the ankle joint. To be able to supply the ankle joint, these arteries develop an anastomosis around the foot’s malleoli, separating into anterior, lateral, and medial regions. The similar veins around the ankle release venous blood.
Starting in Malleolar Branches of:
- Peroneal Artery
- Anterior and posterior Tibial Artery
Nerve Supply of the ankle joint
- Common Peroneal Nerve
- Tibial Nerve
Innervation of the ankle joint
The body’s lumbar and sacral plexus generate the sensory and motor materials that supply the ankle complex. Tibial, deep, and superficial peroneal nerves provide the muscles with the necessary motor supply, while the sural and saphenous nerves supply the muscles with their sensory supply. Also supplying the muscles with motor function are these three mixed nerves. It has been established that mechanoreceptors that contribute to proprioception are extensively innervated in the lateral ligaments and joint capsules of the talocrural and subtalar joints.
Movements at the ankle joint
The tibia and fibula, which lie on the talus and calcaneus bones at the back of the foot, are situated in the ankle joint. There are twenty-six bones in the foot. The movements that are in evidence are:
- Plantarflexion: a rise of the toes. Range of motion normal: 0 to 50 degrees.
- Dorsiflexion is the action of elevating your foot. The normal range of motion is from 0 to 20 degrees.
- Inversion: The inward rotation of the foot’s sole. In a normal range of motion, 0 to 15 degrees.
- Eversion is the flattening or turning outward of the foot’s sole. The normal range of motion is from 0 to 10 degrees.
- It is uncommon to perform plantarflexion and dorsiflexion alone at the ankle joint; instead, they are usually combined with motions at the subtalar and midtarsal joints. That is to say, dorsiflexion is followed by abduction and eversion allowing the foot to lead, whereas plantarflexion generally follows by adduction and inversion allowing the foot to supinate.
- The ankle joint represents the 90-degree angle generated by the foot and the leg when one is standing. At a plantarflexion range of 0–10 degrees, this is the neutral, or dispersed, state for the ankle joint. Strong and wide muscular support is required posterior to the joint to preserve stability and prevent collapse or forward inclination when standing because the weight of the body acts through a vertical line that travels anteriorly to the joint. The soleus and gastrocnemius muscles are the main sources of this support. Ankle joints are most stable when they are packed together and at maximal dorsiflexion.
Clinical Significance of the ankle joint
Ankle Fracture
All ages are vulnerable to ankle fractures involving one or both malleoli. The fracture pattern indicates how stable the fracture is. Patients usually complain of ankle joint pain, edema, and trouble bearing weight. When healing stable fractures, a leg cast should be worn partially for four to six weeks. An open reduction and internal fixation (ORIF) is necessary for unstable fractures to rebuild a congruent mortise and fibular length.
Talus Fracture
This kind of injury usually occurs from a high-energy trauma, including a car crash or a fall from a height. There is a risk of avascular necrosis (AVN) in talus fractures due to its fragile blood supply.
Ligament Injury
Ankle sprains rank among the most typical musculoskeletal injuries. Indoor and court sports provide the largest risk of ankle sprains, with females more likely to receive one than males and children having a greater chance than adolescents and adults.
FAQs
Is the ankle a joint that hinges?
The talus, tibia, and fibula bones are defined to form the ankle joint, which is a hinged synovial joint.
What is the ankle joint play?
Plantar flexion, dorsiflexion, inversion, and eversion are the movements that can be accomplished at the ankle joint.
What’s the name of the ankle joint?
The joint that connects your foot to your lower leg has the name the ankle. Healthcare providers tend to refer to it as the talocrural joint or the tibiotalar joint. Your ankles participate in the skeletal system, just like any other joint. Additionally, your ankles are comprised of cartilage, muscles, ligaments, and nerves.
The ankle: is it a pivot joint?
The ankle does not have a pivot joint. However, the ankle can rotate in a way that is similar to a pivot joint’s actions.
Which four ankle joints move in these ways?
Ankle joints are hinge-type joints that may move in a single plane. Thus, the biggest movements at the ankle joint are dorsiflexion and plantarflexion. The other foot joints, especially the subtalar joint, are responsible for causing eversion and inversion.
References
- Prajapati, N. (2023, August 18). Ankle joint: Anatomy, Function, Movement, Exercise – Samarpan Physio. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/ankle-joint-anatomy-function-movement-exercise/
- Goriya, D. (2024, January 1). Ankle Joint Ligament: Anatomy its Function and Prevention. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/ankle-joint-ligament/
- Professional, C. C. M. (2024a, May 1). Ankle Joint. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24909-ankle-joint
- https://www.physio-pedia.com/Ankle_Joint.
- Image-https://www.google.com/url?sa=i&url=https%3A%2F%2Fwww.lecturio.com%2Fconcepts%2Fankle-joint%2F&psig=AOvVaw1FV2sbSX_KejYt4oWE_qhY&ust=1726122948776000&source=images&cd=vfe&opi=89978449&ved=0CBQQjRxqFwoTCNiNsbejuogDFQAAAAAdAAAAABAE.




32 Comments