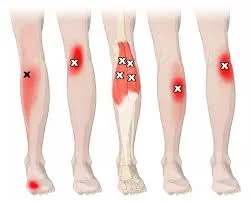
Trigger Points in Calf Muscle
Trigger points in the calf muscle are small, sensitive knots or tight areas within the muscle fibers, often causing localized pain, discomfort, and stiffness. These points, which develop from muscle overuse, strain, or poor posture, can create tension that affects mobility and contributes to pain in surrounding areas, sometimes radiating down to the ankle or up to the knee.
Understanding and treating trigger points in the calf muscles is essential for improving flexibility, enhancing circulation, and reducing pain, making it easier to perform daily activities and sports pain-free.
Trigger Points: What is it?
Throughout a muscle group, a trigger point is a tight band of skeletal muscle that can occasionally feel like tiny knots or marbles beneath the skin. They could experience pain and sensitivity at the trigger point location or in other body areas. They can limit the range of motion in addition to producing migraines, joint pain, visual issues, tinnitus, or a ringing sensation in the ears.
Like Charley’s horse, cramping is not the same as trigger points. Only a small percentage of the muscle spasms are due to the bothersome locations. Pain relief methods like “needling” and massage could be beneficial.
What are the calf muscles’ trigger points?
In the calf muscles, there are six trigger points, four of which are in the gastrocnemius muscle and two in the soleus muscle (one trigger point is extremely uncommon in this situation). The gastrocnemius muscle’s most frequent trigger point, which results in localized discomfort, Ankle, and sole discomfort can also result from trigger points in this muscle.
There are two primary trigger sites for the soleus muscles. These hurt the muscle’s midsection and radiate down to the heel and ankle. These trigger point pains might occasionally be confused with plantar fasciitis discomfort.
There are up to four trigger locations where the gastrocnemius might grow. There are two medial trigger points on the gastrocnemius muscle’s medial head. The lower trigger points are located an inch or two below the knee crease, while the higher trigger point is immediately below it. The two lateral trigger points in the lateral head are positioned similarly to the medial trigger points, with the exception that they are roughly half an inch more distal or towards the foot.
The soleus may consist of There might be up to three trigger sites in this muscle. The most prevalent trigger points are located along the inside of the muscle, right above the place where the Achilles tendon becomes palpable. A few inches under where the muscle attaches to the skull The upper trigger point is located at the head of the fibula bone in the upper outer quadrant. Infrequently occurring, the lateral trigger point is situated a few inches above the lower trigger point along the muscle’s lateral border.
The calf muscles’ anatomy:
Gastrocnemius Muscle
The gastrocnemius muscle is big and strong. The term “gastrosoleus” refers to the combined function of the gastrocnemius and soleus. The main calf muscle, the gastrocnemius, regulates the protrusion beneath the skin. The gastrocnemius’s two “heads” give it its diamond-like form.
Origin:
The medial head that emerges between the femur’s knee, joint, and medial condyle is called the gastrocnemius.
Insertion:
This muscle’s tendon joins the soleus tendon to produce the Achilles tendon, which is placed into the middle part of the calcaneum’s posterior side.
Nerve supply:
The tibial nerve serves as the gastrocnemius muscle’s nerve supply (S1, S2).
Action:
Together, the gastrocnemius and soleus muscles function as the foot’s plantar flexors at the ankle joint.
Thoroughly deep inside the gastrocnemius lies a multipennate muscle characterized by a sole form called the soleus.
Origin:
The soleus muscle’s domed origin may be traced back to:
Situated in the middle third of the medial border of the tibia shaft, the back of the head is the tendinous sole arch that connects the tibia and fibula.
Insertion:
This muscle’s tendon joins the gastrocnemius tendon to produce the Achilles tendon, which is placed into the middle part of the calcaneum’s posterior side.
Nerve supply:
The tibial nerve is the soleus muscle’s nerve supply (S1, S2).
Action:
Although the soleus muscle works less rapidly than the gastrocnemius, it is powerful.
Pain in the Calf Muscles:
Symptoms of trigger points in the gastrocnemius:
- cramping in the calves
- muscle soreness
- discomfort at the back of the knee when climbing or walking on an uneven surface
What leads to trigger points in the gastrocnemius?
- Muscle strain from prolonged plantar flexion
- prolonged muscular contraction, shortening, or immobility
- Walking on a sloping surface or a steep slope
- Riding a bike with the seat too low or jogging uphill
- Ankle or lower leg injury that necessitates the use of a cast
- Leaning forward while standing for extended periods, such as when doing dishes, wearing heels, or working at a desk
- Long-distance driving
- Reduced blood flow
- A robust strip of flexibility at the highest point of long socks
Characteristics and warning signs for soleus trigger points
- Tenderness that indicates heel discomfort
- Nighttime pain
- ankle and foot swelling
- restricted ankle dorsiflexion
- Walking uphill or downstairs might be challenging.
Why do soleus trigger points occur?
- Utilization from too much toe-off
- Running
- Wearing footwear that causes sliding forward, such as high heels
- direct injury to the region
- Not using ankle support when skating or skiing
- Reduced blood flow
- Differences in leg length
Calf Trigger Points:
Among the most common concerns about calf trigger points are:
Gastrocnemius:
- Posterior Leg (Calf) Pain
- Posterior Knee Pain
- Lateral Leg Pain
- Plantar Midfoot Pain
- Upper/Lower Leg Cramps
- Restless Leg Syndrome
Soleus:
- Posterior Leg (Calf) Pain
- Posterior Knee Pain
- Posterior Ankle Pain
- Heel Pain
- Plantar Midfoot Pain
- Buttock Pain
- Restless Leg Syndrome
- Teeth Grinding (Bruxism)
Locations of Calf Trigger Points:
Trigger sites in the medial gastrocnemius:
The most frequently implemented gastrocnemius activation point can be found regarding the medial border of the medial gastrocnemius head, directly distal to the knee. It is a discomfort that originates in the foot’s instep and can spread to the knee, posterior thigh, medial part of the back of the leg, through the heel, and into the bottom of the foot. Because it alludes to discomfort in certain places, this gastrocnemius trigger point might resemble the symptoms of Achilles tendonitis and plantar fasciitis.
The second gastrocnemius trigger point is located in the proximal, medial region of the muscle and is responsible for localized discomfort in the medial region of the rear of the knee.
Trigger points for the lateral gastrocnemius:
Trigger point #3 for the gastrocnemius: This is the second most frequent trigger point. In the belly of the gastrocnemius’ lateral head, is situated distal to the lateral knee. It alludes to discomfort near the trigger point.
The fourth gastrocnemius trigger point is located in the proximal, lateral part of the muscle and is responsible for localized discomfort in the lateral region of the rear of the knee.
Locations of Soleus Trigger Points:
Trigger Points for Soleus:
The most prevalent soleus trigger point is found in the lower medial region of the soleus muscle and causes discomfort in the distal Achilles tendon and posterior plantar area of the heel. may result in instep and heel discomfort.
The second soleus trigger point is situated in the lateral and proximal regions of the cause and is responsible for localized upper calf discomfort.
How can a calf muscle trigger point be identified?
To identify the trigger point, four primary criteria are used.
- The part of that tight ring of tissue that is responsive to pressure.
- When you lightly push on the muscle, you experience pain or feeling radiating.
- This is an example of how the point relates to pain or sensation in other regions.
- A dry needle is gently pushed against the muscle’s twitch reaction.
Management:
Treating a trigger point should ideally involve applying pressure that is just enough but not too much. You must sort of sense it. It might be challenging to do this for yourself at times. You may work the trigger points back and forth, hold them, or rub them in a circular motion in either direction. Depending on the circumstances, one approach could yield a better outcome than the other. The point that causes the pain should be rubbed out or pressured for at least 10 to 15 seconds. Continue treating that area until there is no more discomfort if it is getting better. Additionally, the trigger point may occasionally “wash away” beneath your touch and vanish.
To treat a trigger point, some practitioners employ a modality and a few instruments, such as injections, laser treatment, electrostimulation, mechanical vibration, dry-needling, and spoon-shaped devices made of metal or wood. Using your hands as much as possible is preferred since it allows you to feel the region, even if some of these might be helpful. you are working on, and it’s common to feel the trigger point relax or dissipate.
Another benefit of using a hands-on method is that it reduces the possibility of pushing too hard and causing further injury or bruising, as well as pressing too little or too long and producing insufficient results. For those who are unable to reach a suspected trigger point or have weak hands, tools such as a foam roller, tennis or golf ball, Thera Cane, and/or The Stick may be useful.
Medical care:
Aspirin, ibuprofen, and naproxen are examples of NSAIDs (nonsteroidal anti-inflammatory medicines) that can help with milder types of pain. In addition to relieving muscular pain and stiffness, NSAIDs also lessen inflammation (swelling and irritation), as may Tylenol (acetaminophen).
trigger point injection (TPI):
When a calf’s trigger point is treated with trigger point injection (TPI), a tiny needle is inserted into the patient’s active trigger point. This injection may contain a corticosteroid in addition to saline or a local anesthetic. Usually, a short course of therapy will provide long-lasting relief. A doctor administers the injections, which usually take a few minutes. In a single visit, several sites might be injected. No medicine can be utilized in the dry needle procedure if the patient has a drug allergy.
Physiotherapy treatments:
Physical therapy with gentle stretching and exercise may help restore the full range of motion and motor coordination. Exercises to strengthen the muscles can begin once the trigger points have been removed, promoting the long-term well-being of the local muscular system. A physical therapist can design a plan to help you feel better based on your symptoms and telling signs. If you visit your doctor as soon as symptoms appear, before trigger points are formed, your therapy for a calf muscle trigger point will be more effective.
Your healthcare professional may likely mix many therapies to manage your discomfort and restore damaged muscles. physical treatment to relax, stretch, and strengthen muscles. Myofascial release (MFR) techniques and trigger point therapy can help you with your muscle knots and trigger points. It is believed that myofascial release can assist in correctly aligning the fascia that surrounds your muscles. This might enhance your muscles’ natural range of motion and circulation.
Trigger point therapy involves your physical therapist pushing and holding on to the muscles’ trigger points. A tissue’s circulation is momentarily stopped as a result. A substance known as “nitric oxide” is elevated in the tissue as a result of this circulation restriction. The body opens micro capillaries in response to nitric oxide, which increases blood flow and breaks a pain spasm pain cycle.
Everyday elements that cause a TrPs (Trigger Point) to appear should be reduced or avoided if at all feasible.
Postural instruction and lifestyle and posture education,
Occasionally during the day, perform foam roller and passive stretching.
Self-massaging, perhaps once a day, and particularly deep-stroke massage, which is rhythmic and unidirectional,
Strength training: start with only isometric exercises, then go on to isotonic ones,
Ischaemic Compression Technique: This phrase refers to a therapy wherein ischemia is created in the TrPt zone with the application of continuous pressure. However, this idea is dubious because the TrP’s nucleus naturally exhibits significant hypoxia.
The goal of this method is to release the sarcomeres that have constricted inside the trigger point. Without producing pain, the pressure should be just enough to cause the tension in the Trigger Point zone to gradually release. However, following therapy, both methods replicate a notable increase in the range of motion.
Avoid trying to get rid of your trigger points by going to a physical therapist for trigger point therapy. Instead, concentrate on developing coping mechanisms for unpleasant trigger locations. You can control your discomfort with the aid of physical therapy exercises for muscular knots. and assist in identifying the underlying bodily mechanics that could be causing the pain from the muscle knots.
Double leg calf raise
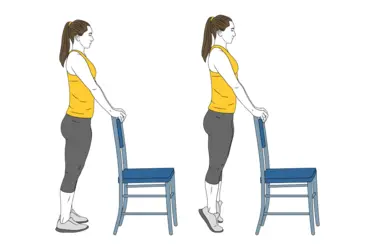
The traditional calf-strengthening exercise is the calf raise. They tone and strengthen your soleus and gastrocnemius muscles using your body weight.
- To start, the patient stands near a wall for balance and places his feet hip-width apart.
- Instruct the patient to elevate their body by applying pressure to the balls of both feet.
- Instead of moving the body forward or backward, keep the abdominal muscles taut so that it travels straight upward.
Downward dog position
Pressing the heels towards the floor is the secret to achieving a calf stretch in this traditional yoga stance.
- Start in a high plank position by placing your hands directly behind your shoulders.
- Shift body weight back to bring the butt to the ceiling by pressing through the fingers and palms, forming an inverted V with the body.
- The calf stretching will be more extensive the more the heels are pulled down towards the floor.
- Continue pressing the heels towards the floor while bending the knees slightly to stretch the bottom portion of the calves.
Seated calf stretch with resistance band

A towel, a yoga strap, or anything like can be used in place of a resistance band if one is not available.
- Make sure your legs are wide enough to sit on the ground.
- Using your hands, grasp both sides of one foot while you loop a resistance band—or any other tool—around it.
- To make the calf feel stretched, slowly bring the toes up to the shin.
- Continue on the opposite side.
Lunging calf stretch

The stretch will be in the gastrocnemius, the big calf muscle, if the rear leg is straight.
- Take several steps away from a wall and turn to face it. You may also perform this with your hand on your hips if there isn’t a wall around.
- Bend your front leg while maintaining a straight back leg as you step one foot back into a short lunge, holding your hands on the wall for support.
- Press the rear heel down until it is flat on the floor while leaning against the wall. There is more stretch when there is more distance between the feet.
- Continue on the opposite side.
Calf trigger points can be lessened with physiotherapy, which may involve:
Treatment for myofascial trigger points can be divided into two categories. Non-invasive methods include TENS (Transcutaneous Electrical Nerve Stimulation), low-level laser treatment, and therapeutic ultrasound.
Pain control
Cold laser and low-level light treatment:
Lasers are used to trigger the release of molecules that reduce pain. A cool laser is a type of low-level light treatment that exposes the trigger site to near-infrared light.
Ultrasound treatment
When a trigger point in the calf muscles affects soft tissues, ultrasound treatment may help them recover by using sound waves to improve blood circulation and warmth.
Transcutaneous electrical nerve stimulation, or TENS
Transcutaneous electrical nerve stimulation uses electrodes affixed to your skin to deliver low-voltage electric signals to the painful location.
Massage treatment:
Myofascial trigger points can be relaxed by certain massage techniques. These consist of:
- passive rhythmic release
- active rhythmic release
- shiatsu (acupressure)
- trigger point pressure release
Massage treatments warm muscles and improve blood flow. Consequently, pain and stiffness may be reduced. By applying pressure to your trigger points, your therapist will increase your discomfort and subsequently relieve the tension in your muscles. To help you feel better, a physiotherapist could massage the affected muscle.
To relieve tension, a physical therapist may apply pressure to particular muscle groups or move your hand along your muscles for extended periods. Short-term pain alleviation may also be achieved using massage treatment that employs trigger-point release methods. The condition could become better with massage.
One of the quickest methods for inactive trigger sites is the dry needling technique. A tiny needle will be inserted by the physician into and around your trigger point, moved about, and poked in and out during dry needling. A needle is inserted into many locations within and surrounding the trigger site in the dry-needling procedure. Although it helps release tense muscles and may be extremely painful, it’s one of the best methods to deactivate a trigger point and lessen discomfort.
Some persons with this trigger point also seem to benefit from acupuncture. Some therapists employ acupuncture needles, which are smaller and less painful than hypodermic needles. Acupuncture and dry needling vary in a few significant ways. inserting tiny needles into the trigger point to soothe pain, improve blood flow, and lessen stiffness. According to a systematic review, dry needling for the treatment of this lower back pain condition seems to be a helpful supplement to conventional therapy; but, because the published trials were few and of poor quality, a firm recommendation could not be given.
A sterile, disposable, solid filament needle is inserted into the muscle and skin at a myofascial trigger point in order to perform trigger point dry needling. This is the first step in ending the pain cycle, which, according to research, will lessen muscle contraction, lessen chemical irritation, increase flexibility, and lessen pain. Multiple contraction knots that are linked to the initiation and maintenance of the pain cycle make up myofascial trigger points.
Techniques for stretching (such as spray and stretch)
To assist relieve the pain in your affected muscle, a physiotherapist could guide you through mild stretching exercises. The physiotherapist may apply a numbing solution to your skin if you experience trigger point pain during stretching. Many people who have calf muscle trigger points find that stretching helps. Before guiding a patient through stretches, some physiotherapists apply a cold, numbing spray to the affected muscle region. To lessen discomfort, you may also attempt some easy stretches and exercises at home.
“Stretch and spray” technique: This method entails first applying a coolant spray to the muscle and trigger point, followed by a gradual physical stretching of the muscle.
Heat: Applying heat, such as with a hot pack or a hot shower, helps relax discomfort and release tense muscles.
A cold pack
Acupuncture and relaxation techniques, such as biofeedback and cognitive behavioral therapy, are also effective in lowering anxiety and enhancing sleep.
Training for posture
Myofascial discomfort, especially in the neck muscles, might be alleviated by improving your posture. You may avoid overworking any one muscle by doing exercises that build strength in the muscles around your trigger point.
exercises to assist in altering your body’s movement and posture.
Using kinesiology tapes
Numerous manual and physical treatment methods, including,
- Post-isometric relaxation
- Active Release Techniques
- Trigger point pressure release
- Muscle energy techniques
Additional alternatives for therapy include:
Modifications to the diet to lower inflammation and avoid substances that appear to cause
- discomfort
- Warmth
- changes in posture, exercise, yoga, meditation, sleep patterns, and workstation arrangement are examples of behavior change.
- When necessary, physiotherapy may involve posture realignment exercises.
- The use of acupuncture
Home Guidance
Learning to self-manage the disease is one of the greatest ways to deal with the trigger spots. Using trigger point methods for self-massage treatment may be part of this. Included are these treatments:
- Pressing through the tennis ball
- The muscles are covered with foam to help smooth out fascial tissue.
- When it comes to treating trigger points, active therapy programs that incorporate movement and posture correction are unquestionably superior to passive ones. For a comprehensive assessment of your problem and to learn self-care strategies for managing your trigger points, consult a physical therapist.
- You may also perform these treatments at home, such as:
- As in a heating pad, heat. Ice or cold packs help some folks.
- Exercise, particularly aerobic activities to increase oxygen delivery to the muscles, stretching exercises to assist muscles to stretch, and weight-bearing exercises to help strengthen muscles.
- NSAIDs
- Relaxation techniques include yoga, meditation, and breathing exercises to strengthen muscles, ease tension, and stretch.
- dietary adjustments Steer clear of recognised inflammatory foods.
Immersion in warm water. - massages.
It could disappear with therapy in a day or a few weeks, but other people may need more time. The following variables affect how quickly this discomfort goes away:
- your overall wellness.
- diet.
- quantity and quality of sleep.
- Take good care of yourself if you have this trigger point in your calf muscles. Maintaining your physical well-being via self-care practices may help you focus on managing your discomfort.
How Can Calf Muscle Trigger Points Be Avoided?
Pain treatment techniques are also included in a few of the avoidable recommendations to adhere to:
- Observe good sleep hygiene.
- Decrease your tension.
- Get moving.
- Avoid hurting your muscles. For example, if your shoulder bag or handbag is overly heavy, this can help prevent muscular pain.
- Use relaxing techniques.
- Consume a balanced, healthful diet, such as the Mediterranean diet.
Inflammation is caused by certain meals. and myofascial pain is exacerbated by inflammation. Foods to stay away from include:
- fried meals, such as French fries.
- dairy goods (yogurt, cheese, and milk).
- processed carbs and refined flour-based meals, including white bread, pizza, spaghetti, pastries, and morning cereals.
- Olive oil, margarine (butter).
- sugar-filled meals and drinks, such as soft drinks.
Red meat (steaks, burgers). - “No sugar added” goods, “diet” soft beverages with no calories, and processed meals like fruit, ice cream, and candy are examples of artificial sweeteners and general additives.
FAQs
How can a calf trigger point be released?
Find any stiff or painful spots by massaging the calf from top to bottom. Once you’ve located it, push it down steadily and hold it for 30 seconds.
How can calves with knots be released?
Heat and ice. Heat and ice are effective treatments for the majority of muscular soreness.
massage of trigger points. Firm pressure might occasionally cause your muscles to relax.
expert massage. Getting a massage from a qualified massage therapist might be beneficial.
Why do calves get trigger points?
Trigger points are regions of taut muscular fibers that develop in muscles. Trigger points are probably caused by overuse of the muscles, usually with bad form, muscular damage, and mental tension.
How can trigger points be massaged?
Using your thumb or finger, apply pressure to the tight area, which frequently feels like a marble.
While taking deep breaths, press hard for 30 to 90 seconds.
For three to five minutes, repeat.
Is massaging your calves beneficial?
By enhancing tissue suppleness and releasing tense muscles, a calf massage improves flexibility.
References
- PainWhisperer.com | Trigger Point Therapy for Calf, Ankle, and Foot Pain. (n.d.). Pw. https://www.painwhisperer.com/trigger-point-calf-ankle-foot-pain
- Ccsp, A. B. D. (2022, October 7). Trigger Point Dry Needling the Calf. Behm Muscle & Joint Clinic. https://www.behmmjc.com/blog/trigger-point-dry-needling-the-calf
- Levarda, T. (2024, May 23). Acupuncture for Calf Trigger Points — Morningside Acupuncture NYC. Morningside Acupuncture NYC. https://www.morningsideacupuncturenyc.com/blog/acupuncture-for-calf-trigger-points#:~:text=Trigger%20points%20in%20the%20calf,cramps%2C%20and%20restless%20leg%20syndrome.
- Dr.Esha Patel. (2023a, January 26). Trigger point calf – Cause, Symptoms, Treatment | Mobile Physio. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/trigger-point-calf-muscle/
- Physiotherapist, N. P.-. (2024, January 15). Calf Muscle: Origin, Insertion, Innervation & Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/calf-muscle-details-and-exercise/