Tibial Nerve
Introduction
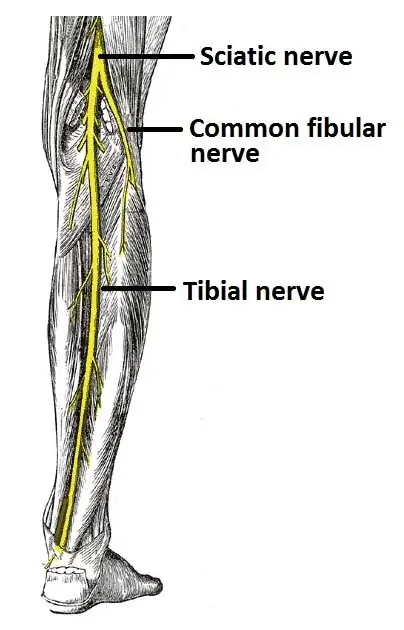
The tibial nerve is a major branch of the sciatic nerve and is part of the lumbosacral plexus. It originates from the L4-S3 spinal nerves and runs down the back of the leg.
From the popliteal fossa, the tibial nerve descends into the leg’s posterior compartment. Along with the posterior tibial vessels, it travels vertically into the deep layer of the leg’s posterior compartment and penetrates deep into the fibular and tibial heads of the soleus muscle, innervating the surrounding muscles.
The majority of the intrinsic muscles and skin are supplied by the tibial nerve, which leaves the posterior compartment of the leg near the ankle joint and enters the sole by going beneath the medial malleolus.
The tibial nerve has a root value of L4, L5, S1, S2, and S3, originating from the lumbosacral plexus. It is one of the two terminal branches of the sciatic nerve, contributing to motor and sensory functions of the lower leg and foot.
Structure
Popliteal fossa
With root values of L4, L5, S1, S2, and S3, the tibial nerve is the largest terminal branch of the sciatic nerve. It crosses the popliteal vessels from the lateral to the medial side and extends from the superior angle to the inferior angle of the popliteal fossa, placing it superficially (or posteriorly) to the popliteal vessels. It produces branches, as seen below:
Muscular branches: The distal portion of the popliteal fossa is where muscular branches originate. It provides blood to the gastrocnemius, soleus, plantaris, and popliteus muscles’ medial and lateral heads. To feed the deep (or anterior) surface of the popliteus, the popliteus nerve passes over the popliteus muscle, descends laterally, and coils around the bottom border of the popliteus. The tibia bone, the interosseous membrane of the leg, the superior tibiofibular joint, the tibialis posterior muscle, and the inferior tibiofibular joint are also supplied by this nerve.
Cutaneous branches: From the center of the popliteal fossa, the tibial nerve also releases a cutaneous nerve known as the medial sural cutaneous nerve, which leaves at the inferior angle. Up to the tip of the little toe, it provides blood to the skin of the lateral border of the foot and the lower portion of the back of the leg.
The superior medial genicular nerve, which is situated on the surface of the medial condyle of the femur, the middle genicular nerve, which pierces the posterior capsule of the knee joint to supply the structures located in the intercondylar notch of the femur, and the inferior genicular nerve, which runs along the upper border of the popliteus to reach the medial condyle of the tibia, are the three articular branches that emerge from the upper portion of the fossa.
Back of the leg
The tibial nerve enters the rear of the leg at the inferior angle of the popliteal fossa and travels deep to the soleus tendinous arch. Midway between the medial malleolus and medial tubercle of the calcaneum, it travels medially and downward in the leg to the posteromedial side of the ankle. It splits into medial and lateral plantar nerves to supply the foot, ending deep to the flexor retinaculum near the origin of the abductor hallucis. The rear of the leg is supplied by many branches of the tibial nerve:
Muscular branches: Provides the deep portion of the soleus, flexor digitorum longus, flexor hallucis longus, and tibialis posterior.
Cutaneous branches: The flexor retinaculum is punctured by the medial calcaneal nerve, which supplies blood to the back and lower heel skin.
Articular branches – Supplies the ankle joint.
Foot
The nerve splits into medial and lateral plantar branches near the foot’s end.
The tibial nerve’s bigger terminal branch is known as the medial plantar nerve. It splits into additional branches after passing between the flexor digitorum brevis and abductor hallucis. Its distribution is similar to the hand’s median nerve distribution. The flexor digitorum brevis, flexor hallucis brevis, abductor hallucis, and first lumbrical are all supplied by its muscular branches. The medial sole and medial three-and-a-half toes are supplied via the cutaneous distribution of the medial plantar nerve via four digital branches. To supply the nail beds on the dorsum, each digital branch produces a dorsal branch. To feed the tarsal and metatarsal bones, this nerve also produces articular branches.
The tibial nerve’s smaller terminal branch is known as the lateral plantar nerve. It travels forward and laterally until it splits into superficial and deep branches near the base of the fifth metatarsal bone. Its distribution is similar to that of the hand’s ulnar nerve. The flexor digitorum accessorius and abductor digiti minimi are two muscles that are supplied by the nerve’s primary trunk. The sole’s skin is likewise supplied by this nerve.
There are medial and lateral branches inside the superficial branch. Three muscles—the flexor digiti minimi, the third and fourth interossei, and the skin covering the lateral side of the toe—are supplied by the lateral branch. The skin across the fourth interdigital cleft is supplied by the medial branch, which also connects with the medial plantar nerve. The adductor hallucis, first and second plantar interossei, and the second, third, and fourth lumbricals are all supplied by the deep branch.
Tibial Nerve Root Value
The tibial nerve has a root value of L4, L5, S1, S2, and S3, originating from the lumbosacral plexus. It is one of the two terminal branches of the sciatic nerve, contributing to motor and sensory functions of the lower leg and foot.
Function
Motor
The gastrocnemius, soleus, plantaris, and popliteus muscles’ medial and lateral heads are supplied by branches of the tibial nerve at the popliteal fossa. The tibialis posterior muscle, superior and inferior tibiofibular joints, tibia, and the leg’s interosseous membrane are all supplied by the popliteus branch.
The deep section of the soleus, flexor digitorum longus, flexor hallucis longus, and tibialis posterior are all supplied by posterior branches of the tibial nerve.
Sensory
The following are sensory innervated by tibial nerve branches:
The skin on the lower back of the leg and the skin of the foot laterally to the little toe are supplied by the medial sural nerve.
The skin on the inferior and posterior surface calcaneus is supplied by the medial calcaneal nerve.
There are three articular branches to the ankle and knee joints.
Courses
As the bigger terminal branch of the sciatic nerve, the tibial nerve normally emerges around the top of the popliteal fossa in the lower part of the posterior thigh. Lateral to the popliteal vessels, the tibial nerve descends via the popliteal fossa from its origin. The nerve becomes medial to the popliteal vessels and travels deep to the gastrocnemius muscle heads as it gets closer to the distal side of the popliteal fossa. After that, it enters the deep posterior compartment of the leg by passing beneath the tendinous arch made by the soleus muscle heads. Together with the posterior tibial vessels, it descends as a neurovascular bundle on the surface of the tibialis posterior muscle.
The tibial nerve leaves the posterior compartment of the leg at the ankle, travels posterior to the medial malleolus, and then enters the sole through the tarsal tunnel (a fibro-osseous canal on the posteromedial aspect of the ankle) with the help of deep flexor tendons. There is a helpful mnemonic to remember the order of structures that pass through the tarsal tunnel (from anterior to posterior): Tibialis posterior flexor Digitorum longus Artery (posterior tibial) Vein (posterior tibial) Nerve (tibial) Flexor Hallucis longus
Muscle supplies
Region of the posterior thigh
The semitendinosus
- Origin: Ischial tuberosity
- Insertion: Pes anserinus, superior aspect of the tibia’s medial surface
- Actions: Hip extension, knee flexion
The semimembranosus
- Origin: Ischial tuberosity
- Insertion: The tibia’s medial condyle’s posterior side
- Actions: Hip extension, knee flexion
The long head of biceps femoris
- Origin: Ischial tuberosity
- Insertion: Lateral part of the fibula’s head
- Actions include extending the hip, flexing the knee, and laterally rotating it.
Part of the adductor magnus hamstrings (vertical fibers)
- Origin: Ischial tuberosity
- Insertion: Femur’s adductor tubercle
- Actions: Hip (vertical fiber) extension
- Note: The obturator nerve innervates the adductor magnus horizontal fibres, which aid en hip flexion and adduction.
superficial compartment of the back of the leg
- Origin: The lateral side of the femur’s lateral condyle
- The popliteal surface above the femur’s medial condyle is where the medial head originates.
- Insertion: Achilles/calcaneal tendon, posterior side of the calcaneus
- Activities: Plantar flexes the knee and ankle.
The Soleus
- Origin: The Soleil line of the tibia, the proximal side of the posterior fibula, and the posterior aspect of the fibula’s head
- Insertion: Achilles/calcaneal tendon, posterior side of the calcaneus
- Actions: Ankle plantar flexion
The plantaris
- Origin: Oblique popliteal ligament, lateral supracondylar line of femur
- Insertion: Achilles/calcaneal tendon, posterior side of the calcaneus
- Plantar flexes the weak ankle and flexes the weak knee.
Deep compartment in the back of the leg
Popliteus
- Origin: The lateral side of the lateral meniscus and lateral femoral condyle
- Insertion: superior to the sole line on the posterior tibia
- Actions: Flexes the knee (weak), and internally rotates the knee (unlocks the knee).
Posterior tibialis
- Origin: The proximal side of the posterior fibula, the interosseous membrane, and the posterior tibia inferior to the seal line
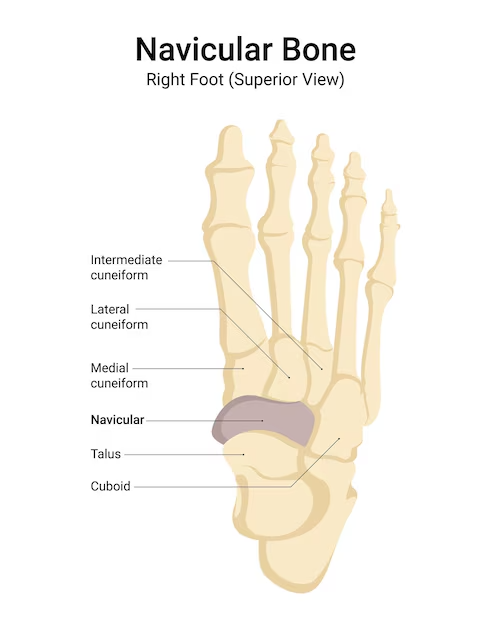
- Insertion: Medial, intermediate, lateral four cuneiforms, cuboid, base of the second through fourth metatarsals, and tuberosity of the navicular bone
- Actions: ankle inversion and plantar flexion
Flexor hallucis longus
- Origin: Interosseous membrane, a distal portion of the posterior fibula
- Insertion: Distal phalanx base of hallux
- Actions: Plantar flexes the ankle (weak), MTP, and Hallux IP
The medial plantar branch
Hallucis abductor
- Origin: Plantar aponeurosis and calcaneus tuberosity
- Insertion: Medial aspect of the proximal phalanx’s hallux base
- Abducts the hallux and flexes the hallux MTP
Flexor digitorum brevis
- Origin: Plantar aponeurosis and calcaneus tuberosity
- Insertion: middle phalanges number two through five
- Actions: MTP and PIP flexes second through fifth
Flexor hallucis brevis
- Origin: Lateral cuneiform plantar aspect, cuboid plantar aspect
- Insertion: Proximal phalanx base of hallux
- Flexes Hallux MTP actions
The first lumbrical (not called according to the numerals)
- Origin: Flexor digitorum longus tendon
- Insertion: Extensor expansion of the medial portion of the second phalanx
- Actions: Extends second DIP, PIP, and flexes second MTP
Lateral plantar branch
Plantae Quadratus
- Origin: The calcaneus plantar surface’s medial and lateral sides
- Insertion: Posterolateral side of the flexor digitorum longus tendon
- Activities: compensates for the obliquely orientated contraction of the flexor digitorum longus to aid in flexion.
Abductor digiti minimi
- Origin: Plantar aponeurosis and calcaneus tuberosity
- Insertion: The fifth proximal phalanx’s lateral aspect of the base
- Actions: Fifth MTP flexes, fifth phalanx abducts
Flexor digiti minimi brevis
- Origin: Fifth metatarsal base
- Insertion: The fifth proximal phalanx’s lateral aspect of the base
- Actions: Shows off the fifth MTP
First through third plantar interossei (not named about digits)
- Origin: Third through fifth metatarsals’ medial surfaces and bases
- Insertion: Third through fifth proximal phalanges’ medial aspect
- Actions: Flexes third through fifth MTP and adducts third through fifth phalanges.
First through fourth dorsal interossei (not named about digits)
- Origin: The first through fifth metatarsals’ adjacent features
- First dorsal interossei insertion: The second proximal phalanx’s medial aspect
The second through fourth dorsal interossei are inserted: Extensor digitorum longus tendons and the lateral side of the second through fourth proximal phalanx - Action: Flexes the second through fourth MTP, stretches the second through fourth DIP, and PIP, and abducts the third and fourth phalanges.
No abduction of the second phalanx occurs when the first and second dorsal interossei oppose each other.
Second through fourth lumbricals (not named about digits)
- Origin: Flexor digitorum longus tendon
- Insertion: Extensor expansion of the medial portion of the third through fifth phalanx
- Actions include extending the third through fifth DIP and PIP and flexing the third through fifth MTP.
Adductor hallucis
- Origin of oblique head: base of the metatarsals, second through fourth
- Transverse head origin: MTP ligaments three through five
- Insertion: Proximal phalanx lateral aspect of hallux
- Adducts hallux are the actions
Branches
Muscular and articular branches emerge from the tibial nerve as they travel through the leg’s posterior compartment. All of the deep and superficial muscles in the leg’s posterior compartment are supplied by the muscular branches:
The gastrocnemius, plantaris, soleus, and popliteus are superficial muscle groups.
Tibialis posterior, flexor hallucis longus and flexor digitorum longus are deep muscle groups.
The superior and inferior tibiofibular joints, the ankle joint, and the knee joint are all innervated via the articular branches.
The sural and medial calcaneal nerves are two cutaneous branches originating from the leg’s tibial nerve.
Between the two heads of the gastrocnemius muscle, in the popliteal fossa, is where the sural nerve originates. The sural communicating branch of the common fibular nerve joins it as it passes distally on the stomach of the gastrocnemius, crossing the deep fascia halfway down the leg to reach the subcutaneous layer. It’s crucial to remember that some textbooks call the sural communicating branch the lateral sural cutaneous nerve and the primary branch from the tibial nerve the medial sural cutaneous nerve. The sural nerve is made up of these.
The sural nerve enters the foot through the calcaneus and lateral malleolus. Here, it produces the lateral dorsal cutaneous nerve and lateral calcaneal branches, which give the lower posterolateral surface of the leg, the lateral side of the foot, and the little toe cutaneous innervation.
The tibial nerve at the ankle gives birth to the medial calcaneal nerve, which extends onto the medial part of the calcaneus. This nerve supplies the skin on the heel’s sole and medial area.
The bigger medial plantar nerve and the smaller lateral plantar nerve are the two terminal branches of the tibial nerve that split off in the foot.
The abductor hallucis muscle is deeply connected to the medial plantar nerve. It ends close to the metatarsal bases as three common plantar digital nerves, which further split into proper plantar digital nerves to toes I–IV. Distally, it gives birth to the medial proper digital nerve to the great toe. The abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and first lumbrical are the four intrinsic muscles of the foot that are supplied by the medial plantar nerve. Like the median nerve in the hand, the medial plantar nerve is cutaneously distributed to the anterior two-thirds of the medial sole and medial three-and-a-half toes, including the nail beds on the dorsum.
One may efficiently remember the muscles that are supplied by the abductors by using the mnemonic “LAFF muscles” (First Lumbrical, Abductor Hallucis, Flexor digitorum brevis, and Flexor hallucis brevis) medial plantar nerve.
The abductor hallucis muscle is also deeply connected to the lateral plantar nerve. It travels over the sole between the quadratus plantae and flexor digitorum brevis muscles before splitting into the superficial and deep branches in the lateral compartment of the sole. The quadratus plantae, flexor digiti minimi brevis, adductor hallucis, dorsal and plantar interossei, three lumbricals, and abductor digiti minimi are all motorly supplied by the lateral plantar nerve. Similar to the ulnar nerve’s cutaneous distribution in the hand, the nerve supplies cutaneous innervation to the anterior two-thirds of the lateral sole and lateral one-and-a-half toes.
Examination
When tarsal tunnel syndrome is suspected, plain radiography is a good place to start assessing the general anatomy of the foot and find any possible fractures or osteophytes. Lower extremity magnetic resonance imaging (MRI) and computed tomography (CT) can be used to search for particular mechanical reasons for tibial nerve injury, such as bone spurs, mass lesions, or local inflammation. Compared to CT, MRI is very useful in detecting tumors or tenosynovitis.
Particularly in situations when tarsal tunnel syndrome is suspected, ultrasound might offer a quick, dynamic investigation at the patient’s bedside to help with the diagnosis. Additionally, it helps rule out other possible causes of the symptoms, like plantar fasciitis. Plantar fasciitis may be indicated if the plantar fascia is hypoechoic and thicker than 4.6 cm. The tibial nerve is hyperechoic and visible at the level of the medial malleolus. The tibial vein and artery should be identified with the use of a color Doppler. Anisotropy distinguishes the flexor digitorum longus and posterior tibialis tendons.
To diagnose tibial neuropathy, electrodiagnostic testing using nerve conduction studies (NCS) and electromyography (EMG) is essential. Mixed or sensory examinations of the lateral and medial plantar nerves are also necessary. NCS will show reduced sensory nerve action potentials (SNAPs) in these nerves. Studies of these nerves are sometimes difficult to come by. Since their potentials frequently have modest amplitudes, they need to be averaged.
Unobtainable medial and lateral plantar nerve tests in healthy persons are fairly uncommon. Therefore, in every suspected case of tibial neuropathy, side-to-side comparisons are crucial. Reduced compound motor action potentials (CMAPs) in the tibial motor nerve will also be seen by NCS. It is crucial to compare the distal latencies of the abductor digiti minimi and abductor hallucis brevis muscles side by side to assess the medial and lateral plantar nerves. Tibial and peroneal F responses, together with Hoffmann reflexes, should be compared side to side.
The tibial innervated muscles distal to the injury site will exhibit anomalies on the EMG. The foot’s plantar muscles will be impacted by tarsal tunnel syndrome. This comprises the quadratus plantae, lumbricals, interossei, flexor digitorum brevis, abductor hallucis, and adductor hallucis. The medial and lateral gastrocnemius muscles may exhibit denervation if the tibial nerve is injured more proximally above the ankle. The chronicity of the damage can also be diagnosed with the use of EMG. While polyphasic potentials and motor potentials with a long duration and big amplitude may be observed in chronic injuries, fibrillation potentials, and positive sharp waves may be present in acute tibial nerve damage.
Because isolating the distal parts of the tibial nerve can be challenging, electrodiagnostic testing for tibial neuropathy can sometimes be technically challenging, especially in cases with tarsal tunnel syndrome. This is especially noticeable in elderly people. Asymptomatic patients may have abnormal EMG results in their foot’s intrinsic muscles. Diagnosing distal tibial neuropathy when superimposed polyneuropathy is present is quite challenging. To prevent overdiagnosing instances of tibial neuropathy, it is crucial to match electrodiagnostic results with clinical history and physical examination.
Clinical Importance
Tarsal Tunnel Syndrome
Similar to the more well-known carpal tunnel syndrome of the wrist, tarsal tunnel syndrome is caused by compression of the tibial nerve within the tarsal tunnel. The tibial nerve passes via the tarsal tunnel into the foot after traveling anteromedially through the leg. Since this compartment is very small at baseline, the tibial nerve may be compressed by any cause of elevated pressure in this area. It is common practice to divide aetiologies into extrinsic and interior origins. Hypertrophic tendinopathies, peri-neural fibrosis, and aberrant growths (such as ganglion cysts, osteophytes, osteochondromas, and schwannomas) are examples of intrinsic causes. Trauma (ankle sprains, scars from surgery), edema, obesity, and tight shoes are examples of extrinsic causes.
The plantar surface of the foot and toes is frequently hot, numb, or tingly when patients first arrive. Radiation to the medial calcaneal nerve, which branches proximal to the tarsal tunnel, may also cause symptoms in the heel. Prolonged standing and physical pressure on the medial side of the ankle frequently cause the most severe discomfort. In more than half of cases, the final sign—a tingling sensation following percussion of the nerve—is positive. Patients may suffer from muscular weakness and atrophy in extreme situations.
For extrinsic reasons (weight loss, changing shoes), management includes lifestyle changes; for other situations, it involves initial conservative therapy. This covers the use of corticosteroid injections as well as resting the foot and ankle. Unless the condition is the result of acute damage or previous surgery, conservative therapy should be tried for six months before undergoing surgery. To surgically decompress the tibial nerve, the flexor retinaculum and abductor hallucis brevis fascia are frequently manipulated.
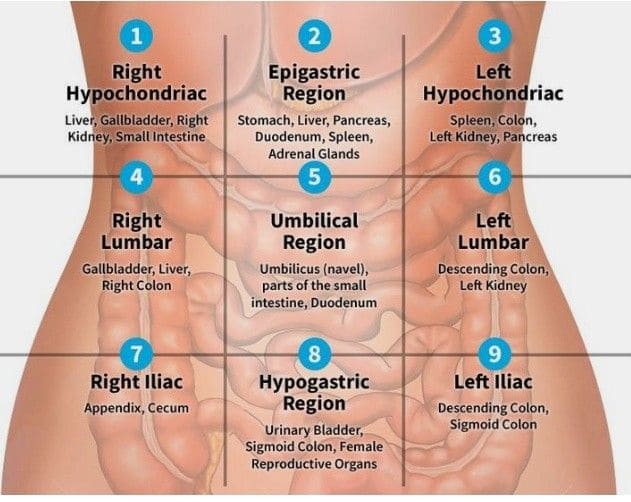
Compartment Syndrome
Fascial membranes wrap several muscle groups in the human extremities. The anterior, lateral, superficial, and deep posterior fascial envelopes or compartments comprise the leg. An acute or long-term rise in pressure inside a fascial compartment that compromises the blood flow to the compartment’s tissues is known as compartment syndrome. Although all four compartments may be affected, anterior compartment syndrome is the most prevalent. The most frequent cause of compartment syndromes after trauma is increasing limb swelling, which raises the compartment’s pressure and leads to venous hypertension and tissue ischemia.
If the deep posterior compartment syndrome is left untreated, tibial nerve ischemia may cause motor and sensory deficiencies in the foot and ankle. Plantar foot paresthesias and weakness in toe and plantar flexion are examples of deficiencies. The main therapy for symptomatic individuals is fasciotomy, which entails making an incision in the surrounding fascia to lower the pressure inside the compartment. Decompression must be done right away in acute instances to prevent irreparable tissue necrosis.
Popliteal fossa region.
Injury might result from, for example:
A lesion that occupies space
Laceration damage
knee dislocation in the posterior
Entrapment in the soleus arch: Sports that place particular strain on the calf muscles may result in soleus arch entrapment neuropathy. The popliteal artery, vein, and tibial nerve may be compressed by the tendinous arch of the soleus muscle due to swelling and hypertrophy. The nerve may sustain long-term mechanical injury as a result, and the vein and artery may be obstructed. This has a favorable consequence and has to be released surgically.
tibial and fibular fractures.
localized injury to the lower leg’s back.
The sole:
Morton’s neuroma, also known as metatarsalgia, can result from abnormal pressure near the ball of the foot irritating the first plantar digital nerve.
Surgical Importance
The tibial nerve has important motor and sensory functions, hence it is crucial to properly identify and protect it during any surgical treatment. Within the popliteal fossa, the tibial nerve is the most superficial structure proximally. In the majority of knee surgery techniques, the nerve is protected by its somewhat posterior location. The most popular anterior midline incision for total knee replacement, for example, includes an anterior dissection and arthrotomy, which securely removes the tibial nerve from the operative field.
A posterior approach to the knee may be necessary in some clinical situations (such as tibial plateau fractures and injuries to the posterior cruciate ligament). Cutting down the medial gastrocnemius and then bending laterally along the knee’s flexion crease is how the posteromedial approach to the knee is executed. The dissection is continued until it reaches the fascia covering the medial gastrocnemius, at which point it is split. The tibial nerve, various neurovascular systems, and the medial head of the gastrocnemius are then securely retracted laterally.
A similar curved incision is created in the middle of the back of the knee with the posterior approach. The tibial nerve can then be located and linked to the medial sural cutaneous nerve. This makes it easier to recognize and safeguard the neurovascular structures. Depending on the clinical circumstance, the neurovascular structures may be dissected separately to reach the posterior side of the knee capsule or the medial gastrocnemius may be separated and reflected laterally to safeguard them.
The tibial nerve may usually be securely retracted and protected posteriorly, as it is located posterior to the medial malleolus. Although the use of the posterolateral and posteromedial ankle portals during ankle arthroscopy may theoretically endanger the tibial nerve, cadaver studies have shown that proper portal placement places the tibial nerve at a safe distance from the surgical tools.
FAQs
What are the symptoms of tibial nerve damage?
Pain, numbness, tingling, weakness, and burning in the foot, ankle, leg, or toes are signs of injury to the tibial nerve. You might also experience difficulty moving your foot or leg.
Symptoms
Ankle, toe, or bottom of the foot pain
Burning or tingling in the toes or bottom of the foot
Weakness in the muscles that move the toes
Difficulty lifting your foot or toes
Foot dragging or slapping the ground when you walk
How to test the tibial nerve?
The plantarflexion/inversion test is carried out by putting the foot in its maximum position, maintaining it there for ten to fifteen seconds, and then bringing it back to neutral. If a patient experiences pain or paraesthesia in the posterior tibial nerve’s distal branches, the test is deemed successful.
Can you walk with tibial nerve damage?
The tarsal tunnel, a small opening between the bones and ligaments in your ankle, is where your tibial nerve passes through after beginning at your knee. TTS, also known as tibial nerve dysfunction, can make it challenging to stand or even walk.
How long is tibial nerve recovery?
Spend one to three weeks typically off your feet.
After surgery, tibial neuropathy symptoms go away right away, however, some discomfort from the treatment could linger for a few weeks. Complete healing from nerve damage might take a year or longer.
References
- Tibial nerve. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/tibial-nerve
- Wikipedia contributors. (2024, August 4). Tibial nerve. Wikipedia. https://en.wikipedia.org/wiki/Tibial_nerve
- Tibial nerve.(2023, August 14).StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK537028/


7 Comments