Stroke
What is a Stroke?
A stroke, also known as a cerebrovascular accident (CVA), occurs when the blood supply to part of the brain is interrupted or significantly reduced, depriving brain tissue of oxygen and nutrients. Without prompt treatment, brain cells begin to die within minutes.
Strokes are a major medical emergency that requires immediate attention.
Acute neurological dysfunction, such as stroke, brain attack, or cerebrovascular accident, is caused by a disruption in blood flow to the brain, which changes how the vascularly derived portion of the brain functions. The two most prevalent stroke kinds are the most well-known, even though there are many others. An ischemic stroke is represented as an insufficiency of 02 blood supply to the brain and infarction.
The blood should not be delivered to the brain with food and oxygen. a hemorrhagic stroke happens because of a sudden rupture of cerebral arteries consequence in bleeding into the extravascular regions of the brain which is secondary to an aneurysm, or trauma. Blood leaks harm brain cells by applying pressure on them.
Less than 90% of strokes are ischemic (caused by blocked blood arteries), with hemorrhagic strokes accounting for the remaining strokes. The location of the obstruction or bleeding in the brain determines the subsequent classification of strokes.
A stroke is a serious medical condition that results in death, irreversible brain injury, or extended incapacity.
A sudden, intense headache, unexpected weakness, vision problems, and difficulty speaking or understanding speech are possible additional symptoms. type 9-1-1 in the phone on the spot if you think someone is having a stroke. Avoid driving or allowing someone else to drive you to the hospital, for medical professionals to start life-saving treatment while en route to the emergency room, call for an ambulance. Every minute matters when having a stroke.
The hospital’s stroke team will assess your condition and manage your stroke with medicine, surgery, or another form of therapy. The severity of your stroke and the promptness of your treatment will determine how well you recover. Resuming your pre-stroke activities may be facilitated with a rehabilitation plan. Your chances of recovering from a stroke without any disabilities increase with the speed at which it is handled.
Causes for the Stroke
Depending on the etiology
strokes can have a variety of causes. Blood clumps are rarely the cause of ischemic strokes. These might appear for several reasons, including:
Embolic stroke
The arteries in the upper chest and neck or the heart are typically the sites where a blood clot forms. an artery transits via the bloodstream until attacks the clot. A clot cannot flow through an artery because it is too small. This results in a cerebral embolism, also known as an embolic stroke. It takes place during the day’s working hours. sometimes systemic disorders might generate septic, fat, or air emboli, carotid bruit is heard in case of embolic stroke
Thrombotic stroke
- Cerebral thrombosis, sometimes called thrombotic stroke, is brought on by a blood clot that develops at the fatty plaque inside the blood vessel. it generally ensues in the sleeping hrs and is of slow onset ( 6 to 8 HRS ).
- atherosclerosis.
- coagulation issues.
- irregular and fast heartbeat occurs when sleep apnea is the causality.
- abnormalities such as anomalies in the ventricular or atrial septal.
- Smaller blood arteries in your brain may become blocked due to microvascular ischemic illness.
A hemorrhagic stroke
Hemorrhagic stroke ensues when an artery in the brain splits or terminates blood. That artery’s blood damages brain tissues and cells by causing the skull to expand and create excessive pressure. Hemorrhagic strokes should also appear for multiple reasons, such as:
- Intracerebral hemorrhagic stroke (ICH) is the most ordinary type of hemorrhagic stroke. It occurs when an artery ruptures and blood fills the tissues encompassing the brain.
- Strokes that are subarachnoid hemorrhagic (SAH) are less frequent. It upshot in blood clots between encompassing tissues and the brain.
- high blood pressure, particularly if it has been present for a long time, is extremely high, or both.
- Hemorrhagic strokes can periodically result from brain aneurysms.
- tumors of the brain, including cancer.
- illnesses like moyamoya disease that weaken or alter the blood vessels in your brain in an odd way.
- accelerated ICP
- projectile vomiting
- giddiness
- nausea
- blurring vision
- papilledema
- altered sensation
- loss of consciousness
- convulsions
- coma
- bradycardia
- hypertension
Subarachnoid hemorrhage
it ensures because of bleeding into the subarachnoid space from a saccular or berry aneurysm
it results in elevated Icp, blood in CSF irritates the nerves supplying the neck, severe pain, and stiffness of neck muscles.
Depending on management categories
Transient ischemic attack (TIA)
it is the temporary interruption of blood supply to the brain in which episodes of neurological deficits are seen but recovered within 24 hours. The symptoms correspond to those of an entire stroke. But after the obstruction is removed and blood flow is restored, they usually go away in a few minutes or hours. A TIA is a caution sign that a stroke might appear, even though it isn’t a total stroke. It is therefore best to pay attention to it. Get emergency care and follow the same guidelines as if you were experiencing a severe stroke.
Having Trouble Speaking: trouble comprehending spoken language, slurred speech, or difficulty finding words.
Issues with Vision: Abrupt vision problems in one or both eyes, including double or fuzzy vision.
Lightheadedness or Unsteadiness: a sudden lack of coordination, dizziness, or difficulty walking.
A sudden and intense headache: an unexplained headache, albeit this is less frequent in TIAs than in complete strokes.
- occlusive episodes
- emboli
- decelerate cardiac output
- cardiovascular spasm
- subclavian steal syndrome
- reduced cerebral perfusion
primary or direct impairment of stroke
- Though not often nonexistent, the feeling is compromised on the hemiplegic side.
- abnormal sensation
- numbness, dysesthesia, hyperesthesia
- exaggerated response to stimuli
- paroxysmal spasm of pain by simply stroking the skin, pinprick, contact with heat, cold, pressure
- forced gaze deviation
- visual neglect, defect in spatial relation, depth of perception
- minor stroke
- major stroke
- deteriorating stroke
- young stroke
Depending on the vascular origin
Anterior cerebral artery syndrome LE > UE
Part of the internal carotid artery is the anterior cerebral artery.
it supplies the medial aspect of the cerebral hemisphere ( frontal and parietal lobe), basal ganglia, anterior fornix, anterior 4/5th corpus callosum.
- motor leg region involvement of arm zone: although uncommon, paralysis of the opposing foot leg and involvement of the opposing arm
- disappear cortical nerve perception in the arm and foot sensory zones
- Urinary incontinence caused by bilateral involvement of the superior frontal gyrus’ posteromedial region
- the mid surface of the back side frontal lobe: frontal tremor, response to external stimulus rigidity, stinking reflex, and unilateral grasp reflex severe frontal lobe infarction: memory loss and behavior impairment
- corpus callosum: apraxia, agraphia
- Another dominant hemisphere motor condition is aphasia.
- symmetrical muscle zone of leg: cerebral hemiplegia
homonymous hemianopia never occurs in ACA strokes.
Posterior cerebral artery syndrome
The basilar artery’s branch is this one.
it supplies: the occipital lobe, medial and inferior temporal lobe, upper brainstem, midbrain, posterior diencephalon ( thalamus)
- conditions conclude thalamus, Hemianesthesia, or contralateral sensory loss, thalamic sensory syndrome, or unpleasant hemibody sensation with spontaneous pain
- occipital cortex: vision loss( homonymous hemianopia), difficulty in recognizing things (visual agnosia), difficulty in recognizing faces and interpreting facial expressions (prosopagnosia)
- bilateral occipital cortex involvement: cortical blindness, dyslexia ( difficulty in reading, writing, color name )
- temporal lobe ischemia concludes amnesic syndrome with memory defect
- midbrain consists of hemiballismus, athetoid posture, skew deviation, involuntary movement, and postural tremor
- The cerebral peduncle embrace of Hemiplegia on the opposite side and oculomotor nerve palsy
- the motor tract between the vestibular and red nuclei includes the decerebrate incidents
- weakness (paresis) of upright eye activities, miosis, ptosis
- sluggish pupillary reflex
Middle cerebral artery syndrome UE, Face > LE
It delivers the cerebral hemisphere’s lateral view, which includes the frontal, temporal, and parietal lobes.
subcortical structures like the internal capsule, corona radiate, globus pallidus, caudate nucleus, and putamen
- the motor region of the arm, face, and fibers that descend from the leg portion to the coronal radiata, the opposite arm, leg, and face become paralyzed.
- somatosensory zone of face, arm, leg: sensory impairment beyond opposite side.
- problem with the muscles used for speech that makes it difficult to talk in Broca’s zone of the dominant hemisphere.
- The dominant hemisphere’s central language center and parietal occipital cortex include central aphasia, word deafness, anomia, jargon speech, alexia, agraphia, acalculia, and finger agnosia.
- Perceptual abnormalities such as unilateral neglect, anosognosia, unawareness of the hemiplegic side, apraxia, spatial disarray, homonymous hemianopia, and conjugate gaze loss to the other are all part of the nondominant parietal lobe.
- parietal lobe includes ataxia of opposite limbs.
- The bilateral frontal lobe comprises Brun’s ataxia or apraxia of walking.
- supramarginal gyrus or inferior parietal lobe includes loss or impairment of optokinetic nystagmus.
- The posterior limb of the internal capsule and adjacent corona radiates pure motor hemiplegia without sensory and visual involvement.
Lacunar syndrome
It is rendered by disorders of the small vessels deep in the white matter.
Its types are pure muscle lacunar stroke, pure sensory lacunar stroke, speech troubles(dysarthria) clumsy hand syndrome, ataxic hemiparesis, and dystonia.
Vertebrobasilar artery syndrome
vertebral artery is a subclavian artery branch that supplies the cerebellum and medulla oblongata.
basilar artery furnishes the pons, internal ear, and cerebellum.
clinical features
medial medullary syndrome
obstruction should emerge in the lower basilar artery, a branch of the spinal artery, or the artery itself.
Ipsilateral traits include atrophy and paralysis of half of the tongue, with the paralyzed side deviating when the tongue is protruded.
Contralateral characteristics include arm and leg paralysis, diminished sense of touch, and proprioception.
lateral medullary syndrome ( Wallenberg’s syndrome )
Blockage can arise in the basilar, posterior cerebellar, and spinal arteries.
ipsilateral features: decelerated pain, temperature sensation in the face, cerebellar ataxia, vertigo, nausea, vomiting, nystagmus, horner’s syndrome, diminished gag reflex, sensory impairment in ipsilateral UE, trunk, LE.
contralateral features: impaired pain and thermal sense over 50 percent body, face.
Complete basilar artery syndrome (locked-in syndrome )
it ensures bilateral infraction of ventral pons and basilar artery thrombosis.
it is sudden in onset.
clinical features
- hemiparesis progress to tetraplegia
- lower bulbar palsy
- cranial nerve palsy (5,6,7)
- anarthria
- dysarthria
- dysphonia
- impaired horizontal eye movement, vertical eye movement, blinking, sensation is intact
Internal carotid artery syndrome
- features of ACA and MCA
- The lower limbs are primarily affected by contralateral hemiparesis (upper limb spread).
- lack of contralateral hemisensory perception, primarily in the lower extremities
- urinary incontinence
- apraxia
- abulia ( akinetic mutism )
- problem in bi-manual tasks
- slowness and delay in motor action
- contralateral grasp reflex, sucking reflex
- UE- and face-related contralateral hemiparesis (LE spared)
- upper limb and opposite hemisensory loss of the face (LE spared)
- affect the ability to speak due to issues with the muscles or nervous system that control speech
- Broca’s or nonfluent aphasia
- affect the person’s ability to understand and say (Wernicke’s or fluent aphasia)
- low understanding and nonfluent speaking
- perceptual defects ( agnosia, unilateral neglect, spatial disorganization )
- incorrect and awkward fine motor movement particularly hand-in-learned tasks (limb kinetic apraxia)
- The condition is known as anosognosia, in which one side of the tongue lacks taste
- contralateral homonymous hemianopia
- loss of eye movement to the opposite side
- contralateral sensory ataxia
- edema
- herniation
- coma
- death
Associated conditions
Several additional circumstances and variables can influence a person’s risk of stroke. These consist of:
- disorder of alcohol usage
- Because high blood pressure can damage blood vessels, which increases the risk of stroke, it can affect strokes of all kinds, not just hemorrhagic kinds.
- elevated cholesterol levels, or hyperlipidemia
- People who suffer from migraines, particularly those with auras, are also more likely to experience a stroke at some point in their lives. Migraine headaches can also present with symptoms that are similar to those of a stroke.
- diabetes type 2
- smoking as well as using tobacco products in other ways, like smokeless tobacco and vaping
- misusage of medications, both specified and over-the-counter
Signs and Symptoms of a Stroke
Brain tissues are harmed when blood flow to the brain breaks off. Stroke symptoms manifest in the bodily parts that are governed by the affected brain region.
A stroke victim’s prognosis is likely to improve the sooner they receive treatment. due to this, being conscious of the signs of a stroke must assist you in quick action. Symptoms of a stroke may include:
- paralysis
- slurred speech
- mostly on one side of the extremity affected with weakness
- difficulty communicating or comprehending others
- focus, disorientation, or inability to respond
- abrupt alterations in behavior, particularly heightened agitation
- Visual issues include difficulty seeing in one or both eyes, hazy or darkened vision, or double vision
- trouble walking
- loss of balance or coordination
- dizziness
- strong headache that came on suddenly and for no apparent reason
- seizures
- nausea or vomiting
Keep in mind that BE FAST can help you spot the early warning signs of a stroke:
- B. Keep an eye out for an unexpected loss of equilibrium.
- E. Keep a lookout for sudden blindness in one or both eyes. Do they have double vision?
- F. Request a smile from the individual. Their face might drop on one or both sides, a sign of muscle weakness or paralysis.
- A stroke victim frequently develops weakness in one side of their muscles. Request that they lift their arms. If they have a one-sided weakness (and not previously), one arm will remain higher while the other sags and falls downward.
- S. People who have strokes frequently lose their ability to talk. They can have trouble choosing the appropriate phrases or slur their remarks.
- T. Don’t put off getting aid because time is of importance! If at all feasible, check a clock or your watch to recall the onset of symptoms. A healthcare professional can determine the best course of treatment for you if you tell them when your symptoms began.
Additional symptoms recognize stroke
instant confusion: Speech comprehension issues or unexpected difficulties with reasoning and comprehension may arise.
Unexpected Numbness: Numbness may be felt in various areas of the body, particularly on one side, in addition to the face and arms.
Immediate Changes in Vision: bilateral vision, unclear vision, and premature loss of vision in one or both eyes are all signs of a stroke.
Rapid difficulties Walking: This can include lightheadedness, unsteadiness, or poor coordination, which makes it hard to stand or move.
Terrible Headache: Particularly with hemorrhagic strokes, a severe headache that has no known explanation and is frequently referred to as the worst headache ever can happen.
Inability to Swallow: This can result in choking or a feeling that food is stuck, which is frequently linked to throat muscle weakness.
Mood or Behavior Changes: Unexpected emotional shifts can happen, such as heightened irritability or unexplainable fear.
Consciousness loss: Fainting or losing consciousness can happen to some people, especially when there is severe brain bleeding.
The Value of Quick Action
It’s critical to identify any of these symptoms as soon as possible and get medical help right away. When treating strokes, time is important; prompt action can improve results and lower the chance of permanent harm. Do not hesitate to contact emergency services if you or someone else displays these symptoms.
Diagnosis
To identify whether a stroke is ischemic or hemorrhagic and to inform treatment choices, prompt identification is essential when a stroke is suspected. Numerous diagnostic tests, including blood tests, MRIs, and CT scans, are frequently employed. Here is a summary of each:
Computed Tomography (CT) scans
Goal: When a stroke is suspected, a CT scan is frequently the first imaging test carried out. It can rule out other disorders and aid in the diagnosis of hemorrhagic stroke, a type of brain bleeding.
Technique: A giant circular device rotates a table on which the patient lies. Cross-sectional images of the brain are acquired utilizing X-rays.
Benefits include speed and accessibility.
efficient in identifying severe bleeding.
can aid in recognizing big strokes.
Limitations: Might miss early ischemia changes in minor strokes.
Magnetic Resonance Imaging, or MRI
Goal: An MRI offers more precise pictures of the brain and is especially helpful in determining the degree of brain damage and identifying ischemic strokes.
Procedure: The patient lies within a tube-shaped device that creates finely detailed pictures of the brain using radio waves and powerful magnets.
Benefits include increased sensitivity in identifying minute strokes and alterations in brain tissue.
can reveal details about any ischemia areas and the structure of the brain.
Limitations: It is more costly, takes longer than a CT scan, and might not be available in all emergencies
Examinations of the Blood
Goal: Blood tests are crucial for assessing general health and identifying stroke risk factors. They aid in measuring blood sugar, cholesterol, and clotting factors.
Typical Tests:
Complete Blood Count (CBC): Assesses general health and identifies anemia or infections.
Coagulation studies, such as PT/INR and aPTT, measure the effectiveness and speed of blood clots.
Checks for hyperglycemia or hypoglycemia, which may impact stroke treatment, are done using blood glucose levels.
The Lipid Profile aids evaluation of cholesterol levels and cardiovascular risk.
Benefits: Offers crucial details regarding the patient’s condition and possible risk factors for subsequent stroke
Extra Examinations
Ultrasound: To look for plaque accumulation in the carotid arteries, which might raise the risk of stroke, carotid ultrasonography may be done.
Cerebral Angiography: A specialized imaging exam that shows the brain’s blood arteries and can spot anomalies or obstructions.
Importance of Medical History and Physical Examination in Stroke Diagnosis
A thorough medical history and physical examination are essential components in the evaluation and management of stroke. These steps provide valuable insights that guide diagnosis, treatment, and prevention strategies. Here’s an overview of their importance:
Identifying Risk Factors
Medical History: Understanding a patient’s medical history helps identify risk factors for stroke, such as hypertension, diabetes, heart disease, smoking, and previous strokes or transient ischemic attacks (TIAs). Treatment and preventative actions can be guided by this knowledge.
Family History: Knowing about any family history of stroke or cardiovascular diseases can indicate genetic predispositions and help assess risk levels.
Assessing Symptoms
Symptom Onset: A detailed account of when symptoms began is crucial for determining the type of stroke and eligibility for certain treatments (e.g., thrombolytic therapy).
Nature of Symptoms: Describing the progression and characteristics of symptoms helps differentiate between ischemic and hemorrhagic strokes, as well as other potential neurological conditions.
Physical Examination
Neurological Assessment: A physical examination focuses on neurological function, evaluating muscle strength, coordination, reflexes, and speech. This assessment helps identify the extent of neurological impairment and localize the area of the brain affected by the stroke.
Vital Signs: Monitoring blood pressure, heart rate, and respiratory rate can provide immediate insights into the patient’s overall condition and potential complications.
Guiding Diagnostic Testing
Focused Testing: Information gathered from the medical history and physical examination helps determine which diagnostic tests (e.g., CT, MRI, blood tests) are necessary. This focused approach helps speed up the diagnostic process.
Interpreting Results: A comprehensive understanding of the patient’s background allows healthcare providers to interpret test results in the context of individual risk factors and symptoms.
Formulating a Treatment Plan
Personalized Care: The insights gained from medical history and physical examination enable healthcare providers to create tailored treatment and rehabilitation plans, addressing both immediate needs and long-term prevention strategies.
Identifying Comorbidities: Recognizing other health conditions that may complicate stroke treatment (e.g., atrial fibrillation, heart failure) is critical for managing patient care effectively.
Preventing Future Strokes
Education and Counseling: Understanding a patient’s history allows for targeted education on lifestyle modifications and risk factor management to prevent future strokes.
Regular Monitoring: Patients identified with high stroke risk can be monitored more closely, allowing for timely interventions to mitigate risk factors.
The function of neurologists and other medical specialists in stroke treatment
The management of stroke involves a multidisciplinary approach, with various healthcare professionals playing critical roles at different stages of care. Each member of the healthcare team contributes their expertise to ensure optimal patient outcomes. Here’s an overview of the roles of neurologists and other healthcare professionals in stroke care:
Neurologists
Diagnosis: Neurologists specialize in diagnosing and managing neurological conditions, including stroke. They interpret diagnostic tests (CT scans, MRIs) and assess symptoms to determine the type and severity of the stroke.
Treatment: They develop and oversee treatment plans, including administering thrombolytics for ischemic strokes and coordinating care for hemorrhagic strokes.
Rehabilitation Planning: Neurologists work closely with rehabilitation specialists to create personalized rehabilitation plans that address specific deficits and promote recovery.
Research and Education: Many neurologists are involved in stroke research and education, helping to advance knowledge and improve clinical practices.
Emergency Medicine Physicians
Initial Assessment: In the emergency department, emergency medicine physicians are often the first to evaluate patients with suspected strokes. They perform initial assessments, stabilize patients, and determine the need for further imaging and treatment.
Rapid Response: They play a key role in initiating immediate care and coordinating with neurologists for further management.
Radiologists
Imaging Interpretation: Radiologists specialize in interpreting imaging studies, such as CT and MRI scans, to identify stroke types and assess the extent of brain damage.
Guiding Treatment Decisions: Their findings are crucial for guiding treatment decisions and informing the healthcare team about the patient’s condition.
Nurse Practitioners and Nurses
Patient evaluating: In both acute and rehabilitation settings, nurses are essential in keeping an eye on patients’ vital signs, neurological conditions, and general state of health.
Patient Education: They provide education to patients and families about stroke symptoms, risk factors, and recovery processes.
Supportive Care: Nurses offer emotional and psychological support to patients and families during the recovery process.
Physical Therapists
Rehabilitation: Physical therapists assess and treat mobility and physical function impairments. They provide customized rehabilitation plans to assist patients in regaining their coordination, strength, and balance.
Goal Setting: They set functional goals to improve patients’ ability to perform daily activities and enhance their quality of life.
Occupational Therapists
Activities of Daily Living (ADLs): Occupational therapists focus on helping patients regain skills needed for daily living, such as dressing, bathing, and cooking.
Adaptive Strategies: They provide strategies and tools to promote independence and safety in everyday tasks.
speech-Language Pathologists
Communication and Swallowing: These professionals assess and treat speech, language, and swallowing difficulties resulting from stroke. They guarantee safe eating and assist patients in regaining their ability to communicate.
Cognitive-Communication Therapy: They may also address cognitive deficits that affect communication, such as memory and problem-solving skills.
Social Workers and Case Managers
Discharge Planning: Social workers assist with discharge planning, coordinating home care services, and ensuring access to community resources.
Emotional Support: They provide counseling and emotional support to patients and families, addressing psychological and social concerns related to stroke recovery.
Nutritionists/Dietitians
Nutritional Counseling: Nutritionists play a role in assessing dietary habits and providing nutritional counseling to help manage risk factors like obesity, diabetes, and hypertension.
Meal Planning: They can create tailored meal plans promoting heart health and supporting recovery.
Treatment for Stroke
Acute treatment for stroke is critical in minimizing brain damage and improving patient outcomes. The approach differs depending on whether the stroke is ischemic (caused by a blockage) or hemorrhagic (caused by bleeding). Here’s an overview of the acute treatment strategies for both types of strokes.
Ischemic Stroke
Thrombolytic Therapy
Medication: The primary treatment is the administration of thrombolytics (clot-busting drugs), such as tissue plasminogen activator (tPA). This is most effective when given within a specific window (typically within 3 to 4.5 hours of symptom onset).
The goal is to dissolve the clot and restore blood flow to the affected area of the brain.
Endovascular Treatment
Mechanical Thrombectomy: For larger vessel occlusions, a mechanical thrombectomy may be performed. During this treatment, the clot is directly removed by inserting a catheter through the blood vessels.
Indications: Typically indicated for patients who present within 6 to 24 hours of symptom onset, depending on the patient’s clinical condition and imaging results.
Antiplatelet Therapy: Following initial treatment, patients may be started on antiplatelet medications (e.g., aspirin) to prevent further clot formation.
stents to support weakened artery walls
surgery to remove plaque from your arteries
Hemorrhagic Stroke
Blood Pressure Management
Control Hypertension: Immediate management of high blood pressure is essential to prevent further bleeding and reduce intracranial pressure.
Surgical Interventions
Clipping or Coiling: For aneurysms, surgical clipping or endovascular coiling may be performed to prevent rebleeding.
Craniotomy: In cases of significant hemorrhage or hematoma, a craniotomy may be necessary to remove the blood and relieve pressure on the brain.
Supportive Care
Similar to ischemic strokes, supportive care includes monitoring vital signs and neurological status. Interventions may be necessary for patients to control intracranial pressure.
Rehabilitation Planning
Early assessment and planning for rehabilitation are essential to address potential deficits and promote recovery.
Preventive Measures
Long-term management may include medications to control risk factors and prevent further strokes.
Medications for Stroke
Medications play a crucial role in both the acute treatment and long-term management of stroke. The specific type of medication prescribed depends on whether the stroke is ischemic or hemorrhagic. Here’s an overview of the main categories of medications used in stroke care:
Ischemic Stroke Medications
Thrombolytics
Its purpose is to break up blood clots that are obstructing blood flow to the brain during acute treatment.
Examples: Tissue Plasminogen Activator (tPA): Must be administered within a specific time frame (usually within 3 to 4.5 hours of symptom onset).
Considerations: Risk of bleeding, so careful patient selection is essential.
Antiplatelet Agents
Purpose: Used for secondary prevention to reduce the risk of future strokes.
Examples:
- Aspirin: Often the first-line medication for long-term prevention
- Clopidogrel (Plavix): May be used alone or in combination with aspirin in certain cases.
- Dipyridamole: Sometimes combined with aspirin for additional protection.
Considerations: Monitoring for gastrointestinal bleeding and other side effects.
Anticoagulants
Purpose: Used for patients with specific conditions like atrial fibrillation to prevent the formation of blood clots.
Examples:
- Warfarin (Coumadin): INR levels must be regularly monitored when taking warfarin (Coumadin)
- Direct Oral Anticoagulants (DOACs): Such as dabigatran, rivaroxaban, and apixaban, offer easier dosing and do not require routine monitoring.
Considerations: Risk of bleeding; need for patient education on signs of bleeding.
Statins
Purpose: Used to manage cholesterol levels and reduce the risk of recurrent strokes.
Examples: Atorvastatin (Lipitor), and Simvastatin (Zocor).
Considerations: Keep an eye on liver function and adverse symptoms relating to the muscles.
Hemorrhagic Stroke Medications
Blood Pressure Medications
Purpose: Control hypertension to prevent further bleeding and manage intracranial pressure.
Examples: Beta-blockers (e.g., metoprolol), ACE inhibitors (e.g., lisinopril), and calcium channel blockers (e.g., nimodipine) are commonly used.
Considerations: Monitor blood pressure closely to avoid complications.
Anticonvulsants
Purpose: Used to prevent seizures, which can occur after a hemorrhagic stroke.
Examples: Levetiracetam (Keppra), Phenytoin (Dilantin).
Considerations: Monitoring for side effects and drug interactions.
Factor Replacement Therapy
Purpose: In cases of hemorrhagic stroke related to specific clotting disorders, factor replacement may be necessary.
Examples: Certain clotting factors based on the condition (for example, factor VIII in hemophilia.
Blood Pressure Management for Stroke
Blood pressure management is a critical component of stroke care, both in the acute phase and during recovery. Proper control of blood pressure can prevent further strokes, reduce complications, and improve overall outcomes for patients. Here’s an overview of the importance of blood pressure management in stroke care and the strategies involved.
Importance of Blood Pressure Management
Preventing Hemorrhagic Stroke: Effective management can help prevent the rupture of blood vessels in the brain.
Reducing the Risk of Recurrent Stroke: For patients who have experienced an ischemic stroke, maintaining blood pressure within a target range reduces the risk of future strokes.
Improving Outcomes: Proper blood pressure control in the acute phase of a stroke can help minimize brain damage and improve recovery chances.
Managing Complications: Fluctuations in blood pressure can lead to complications such as intracranial pressure increases, further bleeding, or additional strokes.
Strategies for Blood Pressure Management
Acute Phase Management
Monitoring: Ongoing observing of blood pressure is elementary in emergency and hospital settings.
Thresholds: Guidelines typically recommend careful blood pressure management during the acute phase, particularly in patients receiving thrombolytic therapy.
For those receiving tPA, blood pressure should be maintained below 180/105 mmHg during the treatment and for the first 24 hours afterward.
Medications: Antihypertensive medications may be administered to lower blood pressure as needed, including Labetalol, Nicardipine, and Esmolol.
Post-Acute Phase Management
Long-Term Control: After stabilization, patients are typically placed on antihypertensive medications to maintain blood pressure within recommended targets (generally below 130/80 mmHg).
Medication Options: Various classes of medications may be used, including :
- ACE Inhibitors (e.g., lisinopril)
- ARbs like losartan.
- Beta-blockers (e.g., metoprolol)
- Calcium Channel Blockers (e.g., amlodipine)
- Diuretics (e.g., hydrochlorothiazide)
Post-Stroke Rehabilitation
Post-stroke rehabilitation is a critical phase in the recovery process for stroke survivors. It desires to support individuals retrieve lost skills, maximizing their independence, and enhancing their quality of life. Rehabilitation often involves a multidisciplinary approach, incorporating various therapies and support systems tailored to the individual’s specific needs. Here’s an overview of key aspects of post-stroke rehabilitation:
Goals of Rehabilitation
Functional Recovery: Helping patients regain physical abilities, such as walking, balance, and coordination.
Activities of Daily Living (ADLs): Assisting patients in relearning daily tasks, such as dressing, eating, and personal hygiene.
Communication Skills: Increasing spoken and language skills to communicate more effectively.
Emotional and Cognitive Support: Addressing psychological aspects, such as depression and anxiety, and cognitive deficits like memory and problem-solving skills.
Components of Rehabilitation
Physical Therapy (PT)
on enhancing interaction, power, balance, and flexibility.
Therapists design individualized exercise programs to enhance physical function.
Use of assistive devices (e.g., walkers, braces) may be introduced as needed.
intends to improve one’s capacity to carry out everyday tasks.
Therapists work with patients on fine motor skills, hand-eye coordination, and adaptive strategies.
a focus on enhancing self-reliance in self-care activities.
Speech-Language Therapy
Addresses communication disorders (e.g., aphasia) and swallowing difficulties (dysphagia).
Therapists use exercises and techniques to improve speech clarity, comprehension, and cognitive communication skills.
Swallowing assessments are performed to ensure safety during eating and drinking.
Neuropsychological Support
emphasizes mental health recovery and emotional health.
Psychologists or neuropsychologists assess cognitive deficits and provide strategies for improvement.
Counseling may be offered to address emotional challenges, such as depression and anxiety.
Setting and Duration of Rehabilitation
Inpatient Rehabilitation: For patients with significant impairments, intensive rehabilitation is often conducted in a hospital setting. To deliver complete care, multidisciplinary teams collaborate closely.
Outpatient Rehabilitation: A large number of patients move to outpatient programs for ongoing therapy following inpatient care. Sessions are scheduled based on individual needs, often several times a week.
Home-Based Rehabilitation: Some patients may receive therapy at home, especially if they have mobility challenges or live far from rehabilitation facilities.
Home health aides or therapists can provide personalized support in familiar environments.
Family and Caregiver Involvement
Education and Training:
A consequential element of the rehabilitation team is the relative and protectors. They are educated about the patient’s needs and how to provide support effectively.
Support Groups: Encouraging participation in support groups can help families cope with the emotional and practical challenges of caring for a stroke survivor.
Monitoring and Evaluation
Regular Assessments: Ongoing evaluation of progress is crucial to adapt rehabilitation strategies as needed. Functional assessments help track improvements and set new goals.
Outcome Measures: Various standardized scales (e.g., Fugl-Meyer Assessment, Barthel Index) may be used to quantify progress in motor skills, ADLs, and overall function.
Community Reintegration
Support Services: Connecting patients with community resources and services can facilitate a smoother transition back to daily life.
Employment and Social Activities: Encouraging participation in social activities and potential vocational rehabilitation can enhance quality of life and promote independence
Physical Therapy for Stroke
A key element of stroke recovery is physical therapy (PT), which aims to increase general mobility, strengthen the body, and restore movement. The goals of physical therapy for stroke patients vary depending on the severity of the stroke and individual recovery needs, but the ultimate aim is to help patients regain independence and improve their quality of life. Here’s an overview of physical therapy in stroke rehabilitation:
Goals of Physical Therapy
- Restoration of Movement: Helping patients regain lost motor function and mobility.
- Strengthening Muscles: Focusing on building strength in affected limbs to facilitate movement.
- Improving Balance and Coordination: Enhancing stability to prevent falls and promote safe movement.
- Functional Independence: Aiding patients in performing daily activities, such as walking, climbing stairs, and transferring between surfaces.
Therapy Environment
- Inpatient Rehabilitation: For patients with significant impairments, intensive PT is often provided in a hospital or rehabilitation facility.
- Outpatient Therapy: After discharge, patients may continue therapy in outpatient settings, often participating in multiple sessions per week.
- Home-Based Therapy: For those unable to attend outpatient sessions, home therapy can be arranged, allowing personalized care in a familiar environment.
Adaptive Equipment and Techniques
- Assistive Devices: Introduction of tools such as walkers, canes, or braces to facilitate movement and support recovery.
- Adaptive Techniques: Teach patients methods to accomplish daily tasks safely, and adjust techniques to compensate for physical limitations.
The Role of Exercise in Stroke Prevention
Exercise
Regular Physical Activity: The heart is strengthened and circulation is improved by frequent exercise. Additionally, it might assist with controlling weight, better cholesterol, and decreasing blood pressure, manage weight, and improve cholesterol levels.
The American Heart Association instructs at least 150 minutes of moderate-intensity aerobic exercise (such as speedy walking) or 75 minutes of passionate exercise (such as running) per week.
Range of Motion Exercises: Passive and active exercises to maintain joint flexibility and prevent stiffness, improve circulation, and promote recovery.
Active Range of Motion (AROM)
Definition: Exercises performed by the patient independently, using their strength and control.
Passive Range of Motion (PROM)
Definition: Exercises performed by a caregiver or therapist without the patient’s active involvement, helping to move the joints through their range.
Leg Lifts: Gently lift the leg at the knee and move it through its range of motion.
Shoulder Rotation: Support the arm at the elbow and gently rotate the shoulder in circular motions.
Ankle Pumps: Move the foot up and down at the ankle joint while supporting the leg.
Upper Extremity Exercises
Shoulder Flexion and Extension: Extend the arm forward and overhead, then fall it back down.
Shoulder Abduction and Adduction: locomote the arm far from the body and then get it back towards the side.
elbow flexion and extension: flexing the arm towards and away from the biceps brachii muscle is known as elbow flexion or extension.
wrist flexion and extension: decrease the ratio between wrist and forearm is wrist flexion and opposite to that increase the ratio termed as wrist extension
Finger Flexion and Extension: Open and close the fingers, spreading them apart.
Lower Extremity Exercises
Hip Flexion/Extension: Lift the leg forward (flexion) and then extend it backward.
The process of reducing and expanding the angle developed between the thigh and lower leg is known as knee flexion as well as extension.
Ankle Dorsiflexion/Plantarflexion: Point the toes upward (dorsiflexion) and then down (plantarflexion).
Hip Abduction/Adduction: Move the leg out to the side and then back towards the midline.
Strength Training
Incorporating strength training exercises at least twice a week can enhance muscle strength and support metabolic health, which can help control blood sugar and weight. Exercises targeting specific muscle groups, using body weight, resistance bands, or weights.
Importance of Strength Training
Muscle Recovery: Helps rebuild muscle strength that may have been lost due to weakness after a stroke.
Functional Improvement: Improves the capacity to complete daily activities (ADLs) like getting dressed, bathing, and walking.
Balance and Stability: Strengthening core and lower body muscles can improve balance, reducing the risk of falls.
Overall Health: Supports cardiovascular health, bone density, and metabolic function
Upper Body Exercises
Seated Dumbbell Shoulder Press
Align your back and sit up straightforwardly. With your hand calmed, grab a small dumbbell at your side
locomote the dumbbells beyond the head and fall that back to shoulder level.
Repetitions: 8-12 times.
Bicep Curls
Assume a seated or standing posture and grasp a dumbbell.
Grasp the weight with your hand. bowed the elbow, bowing the weight upside towards the shoulder. Once the weight arrives on the shoulder, gradually straighten your arm to lower the shoulder back down to the starting position.
Repetitions: 8-12 times per arm.
Triceps Extension
thoroughly lengthen the arm upward, supporting the dumbbell with a straight arm.
After lowering the dumbbell behind your head with bent elbows, raise it back up.
Repetitions: 8-12 times.
Wall Push-Ups
Face the wall, hands flat against it.
Angle your body towards the wall, then exert force to return to your original stance.
Repetitions: 8-12 time
Lower Body Exercises
Sit-to-Stand
Employing the legs, get up from a comfortable chair and then return to the seat.
Focus on using your legs rather than pushing off with your hands.
Repetitions: 8-10 times.
Leg Press with Resistance Bands
snatches the end portion of a resistance band that is looped around your feet as you sit.
To overpower the resistance, force the feet away from the torso.
Repetitions: 8-12 times
Heel Raises
Stand tall with your feet shoulder-width apart. Position yourself near a chair or counter and lightly hold onto it for support.
Elevate your body weight onto the balls of your feet, and then slowly return to a flat-footed position.
Repetitions: 10-15 times.
Side Leg Lifts
Stand or sit and elevate one leg to the side while maintaining the body’s stable
Lower the leg back down.
Repetitions: 8-12 times per leg.
Core Strengthening
Seated Marching
Sit upright and lift one knee towards your chest, then alternate with the other knee.
During the seated marching, concentrate on employing the core.
Repetitions: 10-15 times per leg.
Torso Rotation
Holding a medicine ball or lightweight, thing when you can stand or sit.
The body should be rotated from side to side using the abdominal muscles.
Repetitions: 8-12 times per side.
Safety Considerations
Supervision: It’s advisable to perform exercises under the supervision of a physical therapist, especially for those new to strength training.
Modify as Needed: Adjust exercises based on individual abilities, focusing on safety and comfort.
Listen to the Body: Stop if there is pain or discomfort during exercises.
Gait Training
Focused on improving walking patterns. This might necessitate the use of walking assistance, parallel bars, or treadmills.
Techniques and Methods for Gait Training
Parallel Bars
Use: Ideal for initial gait training, providing support and safety.
Exercises: Patients practice stepping forward, sideways, or backward while holding onto the bars for stability.
Treadmill Training
Use: Makes it possible to practice walking repeatedly in a safe setting.
Assisted Treadmill Training: Some programs use body-weight support systems to help reduce the weight on the legs, making walking easier.
Benefits: Encourages consistent movement patterns and improves cardiovascular fitness.
Overground Walking
Use: Encourages natural walking in a real-world environment.
Techniques: Walking on flat surfaces, inclines, or uneven terrain to enhance adaptability and strength.
Use of Assistive Devices: Patients may use walkers, canes, or crutches to provide support during overground walking.
Gait Training Devices
Robotic Exoskeletons: These devices assist with movement and can provide feedback to help patients regain walking abilities.
Functional Electrical Stimulation (FES): Delivers electrical impulses to stimulate muscles during walking, improving movement patterns.
Progression of Gait Training
Beginning Patiently: Start with simple motions and, as the patient gets better, progressively increase their complexity and endurance.
Variety of Surfaces: Incorporate walking on different surfaces (e.g., grass, gravel) to improve adaptability.
Increase Distances and Speeds: Set goals to gradually increase the distance and speed of walking as confidence and ability improve.
Balance and Coordination Exercises
Static balance: Exercises that boost stability include standing on one leg and utilizing balance boards.
Dynamic Balance: Involves movements while standing or walking, like reaching for an object or turning while walking.
Flexibility and Balance Exercises
Activities like yoga or tai chi improve flexibility and balance, reducing the risk of falls and injuries, especially in older adults who may be at a higher risk for stroke.
Flexibility Exercises: Flexibility exercises should be gentle and focused on stretching major muscle groups. Here are some effective stretches for stroke survivors:
Neck Stretch
How to Do It: Take a comfortable seat or stand. Move your head slightly sideways to one side so that your ear is near your shoulder. Control for 10 to 20 seconds before transitioning sides.
Shoulder Stretch
Method: Utilize your other arm to hold it while crossing your first arm across your torso, after holding for 10 to 20 seconds, alternate sides.
Chest Stretch
How to Do It: Stand with your arms extended behind you and clasp your hands together. Maintaining a straight back, gently raise your arms upward. Continue for 15–30 seconds.
Seated Hamstring Stretch
how to accomplish: Straighten one leg while seated. Slowly flex forward from the hips so that the outstretched leg is in the way. After 10 to 20 seconds of holding, transition legs.
The process involves facing a wall with one leg in front of you and the other behind you. Push the heel into the base while bearing a straight back leg. After 10 to 20 seconds of holding, alter legs.
Balance exercises
Balance exercises can be performed standing or seated, depending on the individual’s ability. Here are some effective balance exercises:
Single-Leg Stand
strategy: Clutch a posture close to a wall or other stable object for stability. Raise one foot off the ground and hold it there for 15 to 20 seconds, or whatever long it feels comfortable. Switch legs.
Tandem Stand
Step-by-step instructions: Place one-foot heel to toe in front of the other.. Hold the position for 10-30 seconds, using a wall or counter for support if needed.
Heel-to-Toe Walk
Strategy: Walk in a perpendicular line with the sole of one foot instantly in front of the other foot’s toes. Focus on balance with each step.
Side Leg Raises
How to Do It: For support, place yourself near a wall or chair. One leg should be extended to the side and straightened. Lower it back down. Repeat 10-15 times for each leg.
Chair Stand
How to Do It: Sit in a sturdy chair and practice standing up without using your hands for support. Resuming your seat, repeat 8–10 times.
Safety Considerations
Use Support: Have a chair, wall, or other sturdy objects nearby for support during balance exercises.
Proper Footwear: Wear supportive, non-slip shoes to minimize the risk of falls.
Monitor Fatigue: Be aware of signs of fatigue and adjust the intensity or duration of exercises as needed.
Functional Training
Practicing activities of daily living (ADLs), such as sitting up, standing, or transferring from bed to chair.
Sit-to-Stand
How to Do It: Get positioned with your feet balanced on the base in a comfy chair.
Lean slightly forward and use leg muscles to stand up without using hands if possible.
Sit back down and repeat.
Repetitions: 8-10 times.
Step-Ups
How to Do It: arrange yourself in front of a lower platform or step.
Extend the other foot to meet the first as you take a stepper upward.
Pull each leg back, one at a time.
Repetitions: 10-12 times on each leg.
Heel Raises
How to Do It: Straighten up body, maintaining your hands on a work surface or chair for support.
elevate your heels off the base, standing on your toes, then lower back down.
Repetitions: 10-15 times.
Overhead Reaching
How to Do It: Use low weights or no weights while standing or sitting.
Reach overhead with both arms, extending fully, and then lower back to shoulder height.
Repetitions: 8-12 times.
Reaching Down
How to Do It: Whether you are seated or standing, set your feet shoulder-width away.
Bend forward at the hips to reach for an object on the ground while maintaining balance.
Return to standing position.
Repetitions: 8-10 times.
Walking with Purpose
How to Do It: Walk in a straight line or around a space, focusing on lifting your knees and maintaining a steady pace.
Incorporate changes in direction and speed as ability improves.
Duration: Aim for 5-10 minutes.
Carrying Objects
How to Do It: While walking, carry light objects (like a small bag or a book) to practice balance and coordination.
Focus on walking smoothly and maintaining good posture.
Duration: 5-10 minutes
Stress reduction training
Regular exercise has been shown to reduce stress and anxiety, both of which can contribute to high blood pressure and other risk factors for stroke.
Deep Breathing Exercises
How to Do It:
Find a comfortable seated position.
off your eyes and bring a deep inhale in via your nose for a hold of three.
For four counts, sustain your breath.
For a hold of six, relax the breath rhythmically through the mouth.
Repeat this cycle for several minutes.
Benefits: Deep breathing aids in lowering heart rate and blood pressure, encouraging relaxation.
Progressive Muscle Relaxation
How to Do It:
Sit or lie down in a pleased position.
trigger with your toes, tense the muscles for roughly five seconds, and then calm down.
Then repeat the procedure on the calves, thighs, belly, arms, and face.
Pay particular attention to how each muscle group differs between stress and calm.
Benefits: This technique helps relieve physical tension and promotes awareness of bodily sensations.
Mindfulness Meditation
How to Do It:
Find a quiet spot to rest.
Pay attention to your breathing and the way air comes into and goes out of your body.
If your ideas stay remain gradually fetch them back to your breathing.
Every day, make an effort to give five to ten minutes to practice.
Benefits: Mindfulness meditation reduces stress, enhances emotional regulation, and improves overall mental clarity.
Yoga
How to Do It:
Join a local class or follow an online yoga session tailored to beginners.
Focus on gentle poses that promote relaxation, such as Child’s Pose, Forward Bend, or Legs-Up-the-Wall.
Incorporate breath awareness into each movement.
Benefits: Yoga combines physical movement, breath control, and meditation, making it an effective stress-relief tool
Walking in Nature
How to Do It:
Go for jogging in a garden, park, or other natural area.
Mark your nearby atmosphere’s sights, sounds, and scents.
Make an effort to walk for at least fifteen to thirty minutes.
Advantages: Taking a nature walk might help you feel calmer, happier, and less stressed.
Visualization
How to Do It:
Sit or lie down comfortably.
Please close your eyes and guess a serene location, like a mountain, beach, or woodland.
Engage all your senses what do you see, hear, smell, and feel in this setting? Give yourself a few minutes to immerse yourself in this visualization.
Benefits: Visualization can help induce a state of relaxation and provide a mental escape from stressors
Tai Chi
How to Do It:
Partake in a Tai Chi session or observe an online video.
attention on gradual, intentional movements merged with deep breathing.
Practice regularly to build coordination and relaxation.
Benefits: Tai Chi promotes physical relaxation and mental clarity, reducing stress and enhancing well-being.
Community and Support: Participating in group exercise classes or community sports can provide social support, making it easier to stay active and committed to a healthy lifestyle.
Occupational therapy for stroke
When talking about stroke rehabilitation, occupational therapy (OT) is fundamental.
Basic ADLs
Dressing
Strategies: Use adaptive clothing with Velcro or elastic bands. Training dressing while sitting to preserve balance.
Exercises: Work on buttoning and zipping using a button board to improve fine motor skills.
Bathing and Personal Hygiene
Schedules: For safety, utilize grab bars or a shower chair. Consider using long-handled sponges or brushes.
Exercises: Practice reaching across the body or using both hands to simulate washing different body parts.
Eating
Strategies: Use adaptive utensils with thicker handles or plates with high edges to make scooping easier.
Exercises: Practice grasping and releasing utensils or using a stability board to improve hand control.
Toileting
Strategies: Install grab bars near the toilet and consider using a raised toilet seat for ease of use.
Exercises: Work on standing up from a seated position to build strength and stability.
Instrumental ADLs
Meal Preparation
Strategies: Use pre-cut ingredients or meal kits to simplify cooking tasks. Focus on one-step tasks to build confidence.
Exercises: Practice pouring liquids or stirring with one hand to improve coordination.
Housekeeping
Strategies: Break tasks into smaller steps, such as dusting one surface or picking up items from the floor.
Exercises: Practice reaching and bending safely to enhance mobility and strength.
Managing Finances
Strategies: Organize bills and payments into a clear system. Use apps or tools that simplify budgeting.
Exercises: Practice counting money or using a calculator to maintain cognitive skills.
Shopping
Strategies: Create a shopping list and practice navigating a store with a family member or therapist.
Exercises: Work on carrying lightweight bags or using a shopping cart to enhance strength and endurance.
Tips for ADL Practice
Start Simple: Focus on one task at a time, gradually increasing complexity as confidence builds.
Use Visual Aids: Checklists or picture guides can help with sequencing tasks.
Encourage Independence: Allow the individual to attempt tasks with minimal assistance to promote self-confidence.
Recuperation takes time, and improvement may be slow. Celebrate small achievements along the way.
Practicing ADLs regularly with the guidance of an occupational therapist can lead to significant improvements in independence and daily functioning for stroke survivors.
Speech therapy for stroke
Speech therapy is vital for stroke survivors who may experience difficulties with speech, language, or swallowing. Here are some common speech therapy exercises and activities:
Speech and Language Exercises
Articulation Practice
Sounds and Syllables: Practice pronouncing individual sounds (e.g., “s,” “m,” “b”) and syllables (e.g., “ma,” “ba”).
Tongue Twisters: Start with simple tongue twisters and gradually increase difficulty to improve clarity.
Word Retrieval
Naming Objects: Use pictures or real objects and practice naming them to improve vocabulary.
Categories: Practice naming items within a specific category (e.g., fruits, animals) to enhance word retrieval skills.
Sentence Formation
Phrase Repetition: Start with simple phrases and gradually move to more complex sentences.
Sentence Completion: Begin a sentence and ask the individual to finish it (e.g., “The cat is on the…”).
Conversation Practice
Role-Playing: Engage in role-playing scenarios (e.g., ordering food) to practice conversational skills.
Topic Discussion: Choose a familiar topic and encourage the individual to share their thoughts to build confidence.
Swallowing Exercises
Lip Closure
Lip Pursing: Practice tightly closing the lips and then relaxing to strengthen lip muscles.
Tongue Exercises
Tongue Lateralization: By thrusting the tongue laterally, you can enrich your strength and control.
Tongue Thrusting: Force the tongue against a tongue depressor or the interior of the cheek.
Swallowing Techniques
Chin Tuck: Tuck the chin slightly down while swallowing to help protect the airway.
Mendelsohn Maneuver: Practice holding the swallow for a few seconds to strengthen swallowing muscles.
Cognitive-Communication Activities
Following Directions
Multi-Step Commands: Start with simple commands and gradually increase complexity (e.g., “Pick up the pen and put it on the table.”).
Sequencing Activities: Arrange pictures in a logical sequence (e.g., steps in making a sandwich).
Memory Games
Recall Tasks: Show a set of items for a few seconds, then ask the individual to recall them.
Story Retelling: Read a short story and have the individual retell it in their own words to enhance comprehension and memory.
Tips for Effective Practice
- Consistency: Regular practice is key. Aim for short, frequent sessions.
- Positive Support: Promote and celebrate improvement to create trust.
- Visual and Auditory Aids: Use visual aids, such as pictures or written prompts, and auditory aids, like recordings, to enhance learning.
- Tailor Activities: Adapt exercises based on the individual’s specific needs and abilities.
The Role of Diet in Stroke Prevention
Diet and exercise play critical roles in reducing the risk of stroke and improving overall cardiovascular health. Both are key components of a healthy lifestyle and can significantly influence many modifiable risk factors associated with stroke, such as hypertension, diabetes, obesity, and cholesterol levels.
Heart-Healthy Diet
A diet that emphasizes whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, can help maintain cardiovascular health.
The DASH (Dietary Approaches to Stop Hypertension) and Mediterranean diets are particularly beneficial for stroke prevention. These diets focus on reducing sodium intake and incorporating more nutrient-rich foods.
- Reducing Saturated and Trans Fats: Limiting saturated fats (found in red meat and full-fat dairy products) and avoiding trans fats (found in many processed foods) can help manage cholesterol levels and prevent atherosclerosis.
- Emphasize Fruits and Vegetables: Aim for at least five servings of a variety of fruits and vegetables each day. These foods are rich in mandatory vitamins, minerals, and antioxidants.
- Increasing Omega-3 Fatty Acids: Consuming foods rich in omega-3 fatty acids, such as fatty fish (salmon, mackerel), flaxseeds, and walnuts, has been shown to promote heart health and may reduce the risk of stroke.
- Managing Sodium Intake: Reducing sodium intake is vital for controlling blood pressure. Concentrating on fresh, natural meals can assist because packaged and processed meals often contain high salt. For people with high blood pressure, aim for fewer than 2,300 mg daily, or even less (1,500 mg).
- Maintaining a Healthy Weight: A balanced diet that helps achieve and maintain a healthy weight can reduce the risk of obesity-related conditions like hypertension and diabetes, both of which are significant stroke risk factors.
- Hydration: remain well-hydrated is elemental for overall health. Dehydration can lead to increased blood viscosity, which can contribute to clot formation. Drink plenty of water throughout the day. Limit sugary beverages and excessive caffeine.
- Moderate Alcohol Consumption: If consuming alcohol, do so in moderation up to one drink per day for women and two for men.
- Whole Grains: Prefer whole grains over unmixed grains. Options include whole grain bread, brown rice, quinoa, and oatmeal, which provide fiber and nutrients that support heart health.
- Healthy Fats: Incorporate sources of healthy fats, such as avocados, nuts, seeds, and olive oil, while limiting saturated and trans fats found in processed foods and red meats.
Smoking Cessation
Quitting smoking is one of the most efficacious routes to diminish stroke chance. The following are methods to help people quit smoking:
- Set a Quit Date: Choose a specific date to quit smoking and prepare mentally and physically for this change.
- Seek Support: Engage with support groups, counseling, or smoking cessation programs to gain encouragement and strategies for success.
- Consider Nicotine Replacement Therapy: Options such as patches, gum, lozenges, inhalers, or prescription medications can help manage withdrawal symptoms.
- Identify Triggers: Recognize situations or activities that trigger the urge to smoke and develop strategies to cope with these triggers.
- Stay Busy: Keep your hands and mind occupied to distract from cravings, consider hobbies, exercise, or engage in activities that you enjoy.
- Celebrate Your Progress: To reward yourself for achieving goals, like quitting smoking for a week or a month, you can strengthen your optimistic behavior.
Risk factors for stroke
Lifestyle and health-related factors that people can alter or control to lower their risk of stroke are known as modifiable risk factors. By addressing these factors, the chance of having a stroke can be considerably reduced. The following are the main risk variables that can be changed.
modifiable risk factors
Hypertension, or elevated blood pressure
Unbearably high blood pressure is the biggest risk factor for stroke. Risk can be considerably decreased by controlling blood pressure with medication, diet, and exercise.
Smoking
The risk of stroke is increased by tobacco usage because it destroys blood vessels and encourages atherosclerosis. Giving up smoking lowers the incidence of stroke and enhances general vascular health.
Diabetes
High blood sugar levels brought on by poorly controlled diabetes can eventually harm blood vessels. It is crucial to control it properly with food, exercise, and medicine.
Elevated cholesterol
An increased risk of ischemic stroke can result from plaque accumulation in arteries caused by elevated levels of low-density lipoprotein (LDL) cholesterol. Medication and dietary adjustments can help control cholesterol levels.
Being overweight
excess body fat is associated with stroke hazards such as diabetes, elevated blood pressure, as well as elevated cholesterol. Risk can be reduced by preserving a healthy weight through diet and exercise.
Lack of Physical Activity
The risk of numerous chronic illnesses that contribute to stroke is increased by a sedentary lifestyle. Frequent exercise aids in weight management and cardiovascular health maintenance.
Unhealthy Diet
The hazards of stroke can be accelerated by diets high in saturated fats, trans fats, cholesterol, and sodium. It is advised to have a well-balanced diet full of lean proteins, whole grains, fruits, and vegetables.
Consuming too much alcohol
High blood pressure and other health problems that raise the risk of stroke can result from heavy drinking. Moderate alcohol consumption is recommended, with women consuming no more than one drink and men up to two per day.
Fibrillation in the Atrium
The danger of blood clots, which can result in ischemic stroke, is increased by this erratic pulse. This risk can be decreased with appropriate management and care.
Anxiety
Chronic stress can lead to bad lifestyle choices and elevated blood pressure. Effective stress-reduction methods including relaxation, exercise, and mindfulness can be helpful.
Apnea in Sleep
This disorder, which is characterized by breathing problems while you sleep, can raise your risk of stroke and high blood pressure. CPAP machines and lifestyle modifications are two possible treatment options.
Non-modifiable risk factors
The traits or circumstances that people cannot alter or control are known as non-modifiable risk factors for stroke. Understanding these characteristics might help people and healthcare providers concentrate on addressing modifiable risks, even while they cannot be changed. The following are the main stroke risk factors that cannot be changed.
Age: As people age, their risk of stroke rises dramatically. Individuals over 55 are more vulnerable, and the chance keeps increasing every ten years.
Gender: Generally speaking, men are more likely than women to have a stroke, particularly when they are younger. After menopause, however, women are typically more at risk.
Family History: An individual’s risk is increased if there is a family history of stroke. Stroke risk factors like diabetes, heart disease, and hypertension can be influenced by genetic predisposition.
Ethnicity: Strokes are more common in some ethnic groups than in Caucasians, including Native Americans, African Americans, and Hispanics. Genetic, environmental, and behavioral variables may all play a role in ethnicity.
Prior Stroke or TIA: People who have previously experienced a transient ischemic attack (TIA) or a stroke are far more likely to get another one.
Specific Medical illnesses: Regardless of lifestyle choices, certain chronic illnesses, such as heart disease, sickle cell disease, and atrial fibrillation, might raise the risk of stroke.
Additionally, many illnesses can raise your risk of stroke, such as:
- previous history of TIA coupled with elevated levels of blood pressure
- excessive weight, diabetes, high cholesterol, and cardiac conditions such as coronary artery disease
- malformations of the heart valves
- irregular heartbeats and enlarged heart chambers
- Sickle cell disease
- Blood clotting disease, diabetes, and patent foramen ovale
Complications of stroke
Depending on whether areas of the brain have sustained significant damage, stroke consequences can differ.
Among these issues are:
- seizures
- lack of bladder and intestinal control
- Cognitive impairment, including dementia; difficulty speaking and swallowing; decreased range of motion, mobility, or control over specific muscle movements
- depression
- alterations in mood, emotions, or conduct
- Pain in the shoulders and bed sores
- Changes in perception or feeling
Regular Health Screenings for Stroke Prevention
Regular health screenings are compulsory for the determination of risk factors associated with stroke, granting early intervention and management. These screenings can help detect conditions that may lead to stroke, such as high blood pressure, high cholesterol, and diabetes. Here’s an overview of important health screenings and their significance in stroke prevention.
Blood Pressure Monitoring
Why It Matters: High blood pressure (hypertension) is the leading risk factor for stroke.Blood sugar monitoring aids in diabetes management and problem avoidance.
Recommended Duration: Adults should have blood pressure conducted at least twice annually.. Those with a history of high blood pressure should monitor it more frequently, as advised by a healthcare provider.
Cholesterol Levels
Why It Matters: Heightened cholesterol can cause to growth of plaques in arteries, accelerating the risk of stroke.
Required Frequency: At least every four to six years, those 20 years of age and beyond should have their cholesterol levels examined. More frequent screenings may be necessary for people with risk factors for heart failure.
Blood Sugar Testing
Why It Matters: Strokes are much more likely to occur in people with diabetes. Blood sugar tracking helps control diabetes and avoid problems.
It is advised that those 45 years of age and older undergo a diabetes screening every three years. Individuals with risk factors (such as obesity or a family history of diabetes) should be tested more often.
Body Mass Index (BMI) and Weight Management
Why It Matters: Obesity is an influential hazard factor for stroke. constantly estimating BMI aids in determining weight management necessities.
Recommended Frequency: BMI should be calculated during annual health check-ups. To lower the risk of stroke, it is essential that you keep a healthy weight.
Electrocardiogram (EKG or ECG)
Why It Matters: An EKG can detect irregular heart rhythms (such as atrial fibrillation), which can increase stroke risk.
Recommended Frequency: Individuals with risk factors for heart disease or stroke should discuss EKG screening with their healthcare provider, especially as they age.
Carotid Artery Ultrasound
Why It Is Important: The carotid arteries, which provide blood to the brain, are examined for constriction or blockages using this imaging technique.
Recommended Frequency: High-risk individuals (such as those with a history of stroke or TIA, or significant risk factors) should discuss this screening with their doctor.
Lifestyle Assessments
Why It Matters: Understanding lifestyle factors (such as diet, exercise, smoking, and alcohol use) is essential for identifying areas for improvement in stroke prevention.
Recommended Frequency: Lifestyle assessments can be part of regular health check-ups, allowing healthcare providers to offer tailored advice and support.
Education and Awareness Campaigns for Stroke Prevention
Education and awareness campaigns are critical components in the fight against stroke. These initiatives aim to inform the public about stroke risk factors, symptoms, and the importance of prevention strategies. By elevating awareness, communities should empower individuals to grab proactive steps in handling their health. Here’s an overview of key elements in effective stroke education and awareness campaigns.
Goals of Education and Awareness Campaigns
Increase Knowledge: Educate the public about the signs and symptoms of stroke, enabling quicker recognition and response.
Promote Healthy Lifestyles: Encourage individuals to adopt lifestyle changes that reduce stroke risk, such as healthy eating, regular exercise, and smoking cessation.
Highlight Risk Factors: Raise awareness about modifiable and non-modifiable risk factors associated with stroke.
Encourage Regular Screenings: Emphasize the importance of routine health check-ups and screenings to monitor blood pressure, cholesterol, and diabetes.
Foster Community Engagement: Create a supportive environment where individuals can share resources, experiences, and encouragement for making health improvements.
Key Components of Effective Campaigns
Targeted Messaging
Tailor messages to specific populations, considering factors such as age, gender, and cultural background.
Use simple, clear language to ensure the information is accessible to everyone.
Multi-Channel Outreach
Utilize various platforms to reach diverse audiences, including:
Social Media: Leverage platforms like Facebook, Twitter, and Instagram to disseminate information quickly and widely.
Webinars and Workshops: Host online and in-person educational sessions to discuss stroke prevention and management.
Print Materials: Distribute brochures, flyers, and posters in healthcare facilities, community centers, and schools.
Partnerships and Collaborations
Collaborate with local healthcare providers, non-profit organizations, and community groups to expand reach and credibility.
Involve local influencers or celebrities to enhance visibility and engagement.
Community Events
Plan health fairs, screenings, and educational seminars to give the public access to information and resources.
Host fun runs or walks to raise awareness while promoting physical activity.
Examples of Successful Campaigns
American Stroke Association’s “Stroke Fast” Campaign: This campaign emphasizes recognizing stroke symptoms using the acronym FAST (Face drooping, Arm weakness, Speech difficulties, Time to call emergency services).
World Stroke Day: Celebrated annually on October 29, World Stroke Day raises awareness of stroke early detection and treatment, as well as the importance of prompt intervention.
Local Initiatives: Many communities have implemented programs that offer free blood pressure screenings and educational workshops to engage residents in stroke prevention.
Evaluating Campaign Effectiveness
Surveys and Feedback: Collect data from participants before and after campaigns to assess knowledge gained and behavior changes.
Engagement Metrics: Monitor social media interactions, attendance at events, and distribution of educational materials to evaluate outreach success.
Health Outcomes: Track changes in local health statistics related to stroke incidence and risk factor prevalence as a long-term measure of impact.
Living With stroke
Impact of Stroke on Daily Life and Relationships
A stroke can have profound effects on an individual’s daily life and their relationships with family, friends, and caregivers. Understanding these impacts is crucial for providing appropriate support and fostering effective coping strategies. Here’s an overview of how a stroke can influence various aspects of life:
Physical Impact
Mobility Issues: Stroke survivors may experience paralysis or weakness on one side of the body, making it difficult to walk, perform daily activities, or maintain independence.
Speech and Communication: Aphasia, a common result of stroke, affects the ability to speak, understand language, read, or write, creating barriers in communication.
Fatigue: Many stroke survivors experience chronic fatigue, impacting their ability to engage in activities or maintain a regular schedule
Emotional and Psychological Impact
Depression and Anxiety: The experience of having a stroke, along with changes in physical abilities and lifestyle, can lead to feelings of sadness or anxiety.
Mood Swings: Emotional lability, or sudden changes in mood, can occur, affecting interpersonal interactions and emotional stability.
Coping Mechanisms: Individuals may struggle to adapt to their new reality, which can lead to frustration and a sense of loss.
Impact on Daily Activities
Activities of Daily Living (ADLs): Tasks such as dressing, bathing, cooking, and cleaning may become challenging or impossible without assistance.
Work and Financial Strain: Many stroke survivors may be unable to return to work, leading to financial difficulties and a sense of loss of purpose.
Rehabilitation and Therapy: Ongoing therapy and rehabilitation require time and commitment, which can disrupt daily routines.
Impact on Relationships
Family Dynamics: Stroke can change family roles, with caregivers taking on more responsibilities. Stress, caregiver exhaustion, and resentment might result from this change.
Social Isolation: Individuals may withdraw from social activities due to physical limitations, communication difficulties, or feelings of embarrassment, leading to isolation.
Changes in Communication: Communication challenges can create misunderstandings or frustration between stroke survivors and their loved ones, impacting relationships.
Reevaluation of Relationships: Stroke may prompt individuals to reassess their relationships, leading to strengthened bonds with supportive friends and family or strained connections with others who may not understand their experience.
Long-Term Implications
Adaptation and Resilience: Over time, many stroke survivors and their families learn to adapt, finding new ways to connect and communicate.
Support Systems: Engaging in support groups or rehabilitation programs can foster community and help individuals share experiences, reducing feelings of isolation.
Improved Awareness: Relationships may deepen as family members gain a better understanding of the survivor’s needs, leading to increased empathy and support.
Coping Strategies for Stroke Survivors and Caregivers
After a stroke, both survivors and those who care for them may discover it difficult to manage. Developing effective coping strategies is essential for managing the physical, emotional, and social impacts of stroke. The following tactics are specific to both groups:
For Stroke Survivors
Embrace Rehabilitation:
Stay Engaged: Actively participate in physical, occupational, and speech therapy to regain skills and independence.
Specify Realistic Purposes: Break rehabilitation into effortless objectives to follow the improvement and celebrate small victories.
Establish a Routine:
Daily Structure: Create a consistent daily schedule to provide a sense of normalcy and predictability.
Include Activities: Incorporate enjoyable activities into the routine, such as hobbies, social interactions, or gentle exercise.
Practice Mindfulness and Relaxation:
Mindfulness Techniques: Engage in mindfulness meditation, deep breathing, or yoga to reduce anxiety and improve emotional well-being.
Visualization: Use visualization techniques to imagine positive outcomes and coping scenarios.
Maintain Social Connections:
Stay Connected: Keep in touch with family and friends, even if it’s through phone calls or video chats.
Join Support Groups: Participate in stroke support groups to share experiences and gain encouragement from others who understand the challenges.
Seek Professional Help:
Counseling: Consider therapy or counseling to address feelings of depression, anxiety, or frustration.
Medical Support: Regular check-ups with healthcare providers to monitor health and discuss any concerns.
For Caregivers
Educate Yourself:
Understand Stroke: Learn about stroke, its effects, and the rehabilitation process to better support the survivor.
Recognize Signs: Be aware of signs of complications or emotional distress in the survivor.
Practice Self-Care:
Prioritize Your Well-being: Make time for your own physical and emotional health through exercise, hobbies, and relaxation.
Set Boundaries: Establish boundaries to prevent caregiver burnout and allow for personal time.
Build a Support Network:
Reach Out: Connect with other caregivers for shared experiences, support, and advice.
Utilize Resources: Explore community resources, including respite care services, to take breaks when needed.
Communicate Openly:
Encourage Dialogue: Foster open communication with the stroke survivor about their needs and feelings.
Listen Actively: Be an empathetic listener to help them express their frustrations and fears.
Adapt to Changes:
Be Flexible: Understand that routines and plans may need to change based on the survivor’s abilities and needs.
Focus on Progress: Celebrate small improvements in the survivor’s recovery to maintain a positive outlook.
Seek Professional Help:
Assistance Groups: To go through your feelings and acquire coping mechanisms for the role of carer, think about getting counseling for yourself.
Support Groups: Participate in caregiver support groups to exchange stories and learn from people going through similar things.
Support Resources for Stroke Survivors and Caregivers
For those who have had strokes and those who care for them, having access to assistance resources is crucial. Various organizations and support groups offer education, community, and assistance to help individuals navigate the challenges that arise after a stroke. Here’s a list of valuable resources:
National Organizations
American Stroke Association (ASA)
Website: stroke.org
Overview: A division of the American Heart Association, ASA provides information on stroke prevention, treatment, recovery, and support. They offer educational materials, online resources, and connections to local support groups.
National Institute of Stroke and Neurological Disorders ( NINDS)
Website: ninds.nih.gov
Description: NINDS provides evidence-based information about stroke, including tools for prevention and rehabilitation. Their site includes publications and information on ongoing research.
Stroke Support Organizations
Website: Various regional and national organizations focused on stroke recovery and support.
Overview: These organizations often provide resources, advocacy, and local support group information tailored to specific communities.
Local and Regional Support Groups
Local Stroke Support Groups
Overview: Many hospitals and rehabilitation centers host stroke support groups where survivors and caregivers can share experiences, gain support, and receive educational resources. Check with local healthcare providers or stroke recovery programs.
Community Centers
Overview: Local community centers may offer support groups, activities, and educational workshops focused on stroke recovery and wellness.
Online Support Groups and Forums
Stroke Network
Website: strokenetwork.org
Overview: An online platform for stroke survivors and caregivers to connect, share experiences, and find resources.
PatientsLikeMe
Website: patientslikeme.com
Overview: An online community where individuals with various health conditions, including stroke, can share their experiences and find support.
Caregiver Support Resources
Family Caregiver Alliance (FCA)
Website: caregiver.org
Overview: FCA offers resources for family caregivers, including educational materials, support groups, and online forums specifically focused on caregiving challenges.
AARP Caregiving Resources
Website: aarp.org/caregiving
Overview: AARP provides tools, resources, and support for caregivers, including articles on managing stress and finding local support services.
Educational Resources
National Stroke Association (NSA)
Website: stroke.org
Overview: Offers educational resources and information for stroke survivors, caregivers, and healthcare professionals.
Local Health Departments and Nonprofits
Overview: Many local health departments and nonprofit organizations provide workshops, seminars, and resources related to stroke awareness and recovery.
How should you take care of yourself?
If you have experienced a stroke, your healthcare provider will discuss your recuperation schedule and rehabilitation plan with you. They might also suggest therapeutic choices, provide prescriptions for drugs, and more. It’s crucial to discuss the reasons behind and potential benefits of these with your healthcare physician.
It’s critical that you adhere to the treatment plan as strictly as possible after you and your clinician have finalized it. You’ll have the best chance of recovering as much as possible if you do that. Additional actions you can take involve :
- Take your prescription drug. After a stroke, taking some medications can help you avoid having another one.
- Attend treatment or rehabilitation sessions. These consultations are essential to your recuperation. Your recovery from a stroke can be greatly impacted by attending these appointments and giving it your all.
- look at you’re helpless or hopeless, ignoring them can make recovery more difficult. If you experience these emotions, discuss them with your healthcare professional. They can suggest treatments that can prevent mental health issues from impeding your healing.
- Try your best to implement the suggested lifestyle adjustments. Your recuperation from a stroke may be impacted by health issues such as your blood pressure, blood sugar, and cholesterol. You can prevent another stroke in the future by managing these. Giving up tobacco products of any kind, including vaping items, can also be quite beneficial.
How should you lower your chance of having a stroke or avoid one completely?
There are numerous strategies to lower your risk of stroke. This can reduce your risk of having a stroke, but it does not guarantee that you can avoid one. below are some key points mentioned
- Make your lifestyle better. Your health can be enhanced by eating a balanced diet and doing regular exercise. Additionally, you should make sure that you receive enough sleep seven to eight hours is the suggested number.
- Steer clear of dangerous lifestyle choices or alter your habits. Alcohol abuse, recreational drug usage or prescription drug abuse, smoking, and tobacco use, including vaping, can all raise your risk of stroke. Stopping or never starting them is crucial. It’s crucial to speak with your healthcare physician if you experience any of these difficulties. You can adjust your lifestyle to prevent these behaviors with the help of your provider’s advice and tools.
- Control your risk factors and medical conditions. Your chance of having an ischemic stroke can be increased by several disorders, including obesity, irregular cardiac rhythms, sleep apnea, high blood pressure, Type 2 diabetes, or high cholesterol. It’s critical that you take all necessary steps to control any conditions you may have, particularly by taking prescription drugs as directed by your doctor, such as blood thinners. You can prevent serious stroke-related issues later in life by doing that early.
- Make an annual well-being check-up or session with your primary medical physician. Long before you have any symptoms, annual wellness exams can identify health issues, particularly those that increase the risk of stroke.
Conclusion
Stroke is a serious medical incident that can have a big effect on survivors’ and caregivers’ lives. Effective management and support require an understanding of the complexity of stroke, including its causes, symptoms, treatment, and recovery, as well as the significance of prevention techniques.
To cope with the aftermath of a stroke, one must address the emotional and social ramifications in addition to the physical difficulties. Coping strategies can promote resilience and adaptation while assisting survivors and caregivers in adjusting to their new circumstances.
Enhancing the quality of life for stroke victims requires having access to support services, such as online communities, local support groups, and national organizations. These tools offer essential knowledge, consolation, and a sense of belonging that can lessen feelings of loneliness
In the end, increasing knowledge about stroke and encouraging education can enable people to take proactive measures to lower their risk and enhance their chances of recovery. We can assist stroke survivors and their caregivers to thrive despite the obstacles they encounter by creating an atmosphere of understanding, assistance, and proactive health management.
FAQs
Who is impacted?
Everyone should have a stroke, whether they are young or old, although some people are more susceptible than others. Strokes are more familiar in later life; adults over 65 for almost two-thirds of all should have strokes. The risk of stroke is also increased by several medical problems, such as hypertension, hyperlipidemia, Type 2 diabetes, and individuals with a history of stroke, heart attack, or abnormal heart rhythms, such as atrial fibrillation.
How frequently do strokes occur?
Strokes happen frequently. Strokes are the 2nd ultimate cause of death worldwide. Stroke ranks as the sixth most prevalent cause of mortality in the US. Another major source of impairment in the world is strokes.
What physical effects might a stroke have on a patient?
In the brain, strokes are comparable to heart episodes.The impacted brain cells become oxygen-starved and cease to function normally in the absence of oxygen. Your brain cells will die if they are left without oxygen for too long. If sufficient brain cells in a particular area die, the damage is irreversible, and you can lose the skills you formerly possessed in that area. Restoring blood flow, however, might stop that kind of harm or at the very least lessen its severity. For this reason, when treating a stroke, time is of the essence.
How should you handle the symptoms or look after yourself?
You should never attempt self-diagnosis or self-treatment for a stroke because it is a potentially fatal medical emergency. The first thing you should do is dial 911 (or the nearest emergency room number) if you or anybody you are with is experiencing stroke symptoms. The danger of death or irreversible brain damage increases with the length of time it takes to start stroke treatment.
How quickly will you feel better following treatment?
Numerous factors influence both the healing period and the time it takes to feel better following therapy. The best person to advise you on what to anticipate and when you might expect to recover is your healthcare professional.
What is the duration of a stroke?
A stroke persists for as long as a portion of your brain is not receiving enough blood. If therapy is not received, a stroke will persist until the brain cells in the impacted regions of your brain die, resulting in irreversible harm. It’s normal for the consequences of a stroke to persist even after treatment. It will typically take weeks or months for most people to fully recover. The majority of recovery progress occurs over the first six to eighteen months (roughly) following a stroke. After that, more advancement is possible, but it can be more difficult or take longer.
With this situation, is there anything I should avoid eating or drinking?
Your doctor might advise altering your diet to prevent blood pressure spikes if you are at risk for any type of stroke. Here are some instances of this:
foods with high sodium or salt content, which might raise blood pressure.
foods like fried dishes that are heavy in saturated fats, etc.
Cocaine, amphetamines, methamphetamine, and other recreational stimulants, as well as alcohol.
References
- What Is a Stroke? | NHLBI, NIH. (2023, May 26). NHLBI, NIH. https://www.nhlbi.nih.gov/health/strokeroke was and how quickly you were treated. A rehabilitation plan may help you get back to what you used to do before you had a stroke.
- Stroke. (2024, September 9). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/5601-stroke
- Stroke – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113




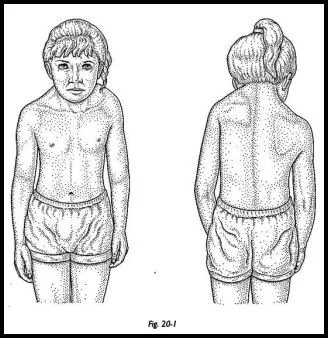
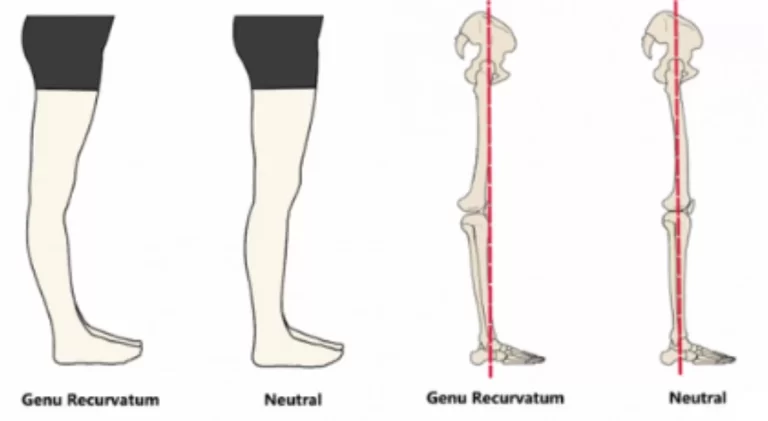
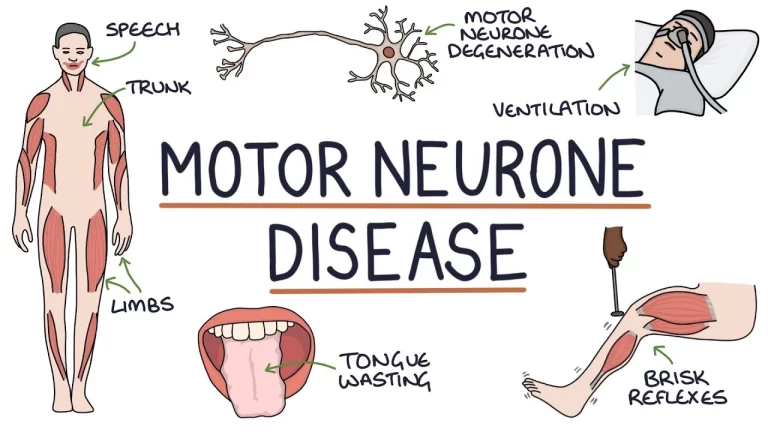
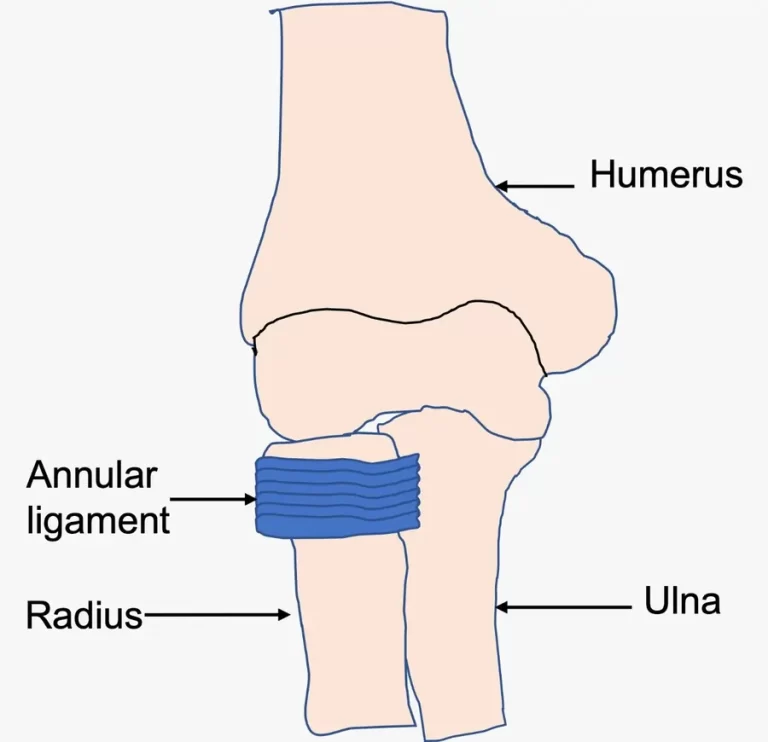
71 Comments