Contrast bath therapy: what is it?
In contrast bath therapy, the entire extremity or body part is submerged in ice water for a few minutes after being submerged in hot water for physical therapy purposes. Then, this procedure of switching between hot and cold is carried out repeatedly. The circulation around the damaged tissue may be improved with the use of the contrast bath.
Muscle spasms, stiff joints, inflammation of soft tissues, edema, and pain in the upper and lower limbs are all treated by contrast bath therapy. Athletes are the ones who use contrast baths the most. Contrast baths are mostly used by athletes to relieve muscleaches and injury, as well as to hasten the healing process following injuries.
It may sound agonising to submerge your body in hot water for a while and then in an ice-cold bath for a while, depending on how tolerant you are of extreme temperatures.
For physical therapists, this is only one of numerous hydrotherapy treatment options that can help reduce pain and muscle spasms, increase muscular strength and range of motion, and enhance functional mobility.
The contrast bath’s mechanics:
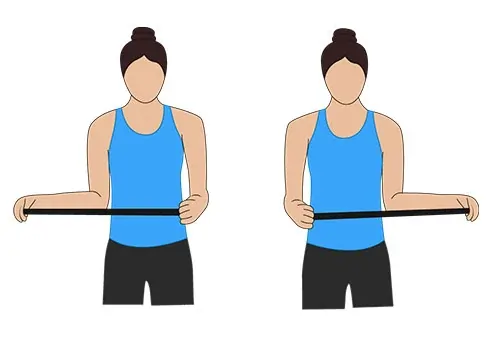
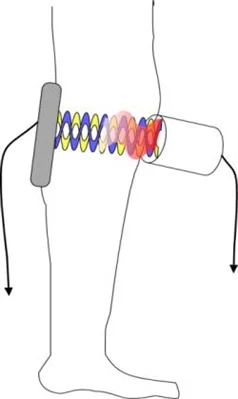
A limb is repeatedly dipped in hot and cold water as part of a hydrotherapy procedure called a contrast bath. This is completed at a specific speed, temperature, and movement. Blood vessel vasoconstriction and vasodilation may result from the frequent change between the two temperatures, producing a pump action. Some people think that doing this will speed up blood flow to all of the tissues in your body.
Despite being a popular therapy, there is no set protocol for the temperature of the water—warm or cold—or the duration of the treatment. To get the greatest outcome, different professionals could employ different temperatures and timings.
Moreover, the contras bath therapy quickens blood flow, which could result in blood oxygenation and enhance the healing process. It might also improve waste product transportation, which would alleviate edema. The hot water causes the generation of more oxygenation. It is believed that hot water alters haemoglobin, a blood protein involved in oxygen transport, making it easier for oxygen to reach the tissues.
The primary idea behind contrast bath therapy is the quick changes in the circulatory system that happen when you go from extremely hot to extremely cold water.
The tiny blood vessels called capillaries in your body shrink in response to the cold when you submerge a portion of it or the entire body in cold water. Vasodilation is the term for this method.
The opposite occurs if you submerge yourself in warm or hot water. Your blood vessels widen. It’s called vasodilation method.
The idea behind the use of contrast baths in physical therapy is that the body’s tiny blood vessel capillaries instantly expand and close as a result of the abrupt transition from warm to cold water. When it’s cold, these tiny arteries constrict, and when it’s warm, they dilate.
It is believed that the quick opening and closure of blood vessels close to the injury site will aid to minimise edema and inflammation surrounding the injury. Pain and mobility are enhanced by reducing edema and inflammation.
Treatment Objectives:
In the event that your physical therapist recommends using a contrast bath to address your injury, your treatment objectives will probably include:
- Reduced pain
- Restrained inflammation
- increased mobility
- Boost muscle regeneration following exercise
How Contrast Treatment Functions:
The mechanism by which contrast therapy works is by eliciting bodily responses to heat and cold. It functions according to the same ideas as cryotherapy (cold therapy) and thermotherapy (heat therapy). Blood arteries dilate (widen) when exposed to warmth, and constrict (narrow) when exposed to cold.
Swelling may be lessened by the pumping action that results from switching between cold and warmth. Consequently, this can aid in reducing discomfort and enhancing joint flexibility.
Contrast therapy is frequently used by athletes to improve their recovery after exercise, as well as to treat soft tissue or joint injuries. In the wake of orthopaedic surgery, it can also be utilised to expedite healing.
The following injuries respond well to contrast bath treatments:
- fractures of the ankle and leg
- Plantar fasciitis
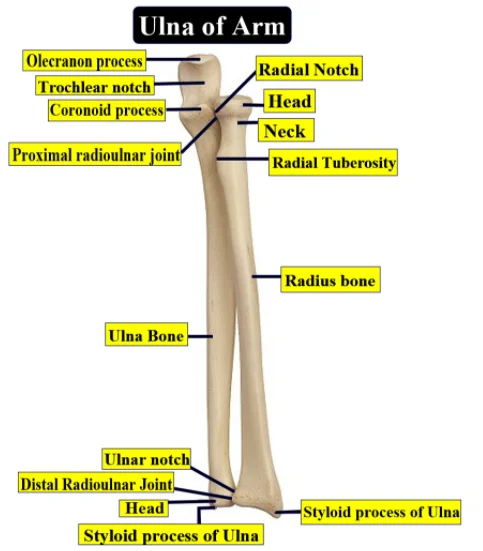
- displaced elbow
- arthritis in the hands and fingers
- Meniscus tear
- anterior cruciate ligament (ACL) injuries
The most common setting for contrast therapy is a temperature-controlled whirlpool bath. It is believed that the swirling action helps to further encourage pain relief and muscular relaxation.
Contrast bath therapy advantages:
lessens tiredness
Contrast bath therapy may help athletes feel less exhausted after a game.
The team athletes used contrast bath therapy, which entailed taking both cold as well as hot baths, to heal from tiredness 24–48 hours afterward the game.
The benefits of submersion in cold water were not the same. as immersion mixed with heated water
reduces pain in the muscles
Muscle fibres are harmed by intense activity. However, you might not experience any discomfort for a day. We call this technique delayed onset muscular soreness.
Elite athletes experiencing delayed onset muscle discomfort and weakness after intense exercises. When contrast bath therapy is used in place of passive relaxing alone, it decreases both irritation and weakening.
It is important to consider two variables.
- First, hot water temperatures below 104°F (40°C) produced the best outcomes.
- Second, contrast bath therapy was nearly twice as effective as other widely used therapies, like submerging the patient in cold water alone, for reducing symptoms of weakness and discomfort.
eliminates surplus lactic acid
Your body produces lactic acid when you workout vigorously. Although lactic acid secretion is natural, it can nonetheless cause fatigue and pain.
By resting, drinking water, taking a magnesium supplement, and adhering to a few other basic guidelines, you can lessen the symptoms that arise when lactic acid builds up in your body.
By lowering the amount of lactic acid in your body, contrast bath therapy can also aid in your body’s healing from the aches and exhaustion that come with vigorous activity.
reduces edema
White blood cells and fluids are sent to the wounded area as part of your body’s natural inflammatory reaction when you get hurt. This fluid’s growth may put pressure on the wound and hurt.
Three days after the accident, hundreds of patients with ankle sprains experienced less swelling thanks to contrast bath therapy.
Conditions targeted in the contrast bath:
Contrast bath therapy should be included as a routine component of rehabilitation for a variety of musculoskeletal ailments, particularly those caused by repetitive strain on the limbs. Any method for activating tissue without overstressing is beneficial for recovering from repetitive strain injuries, which typically require longer periods of rest. The most frequent users of the contrast bah are those who find it easier, more practical, and more successful to apply contrast to the limbs:
- fractures of the upper and lower extremities.
- arthritic hands and fingers, as well as other acute injuries to the extremities that require more than 72 hours to heal.
- disorders correlated with decreased blood flow.
- muscles that are overly taut, resulting in cramps or spasms.
- Behaviours that encourage that lead to carpal tunnel syndrome or other repetitive strain injuries.
- The chronic regional pain syndrome(CRPS).
- Shin splints and plantar fasciitis.
- tennis elbow
- Achilles tendonitis
Even though the knees are small joints, athletes can employ contras bath therapy to treat diseases including patellofemoral pain syndrome, iliotibial band syndrome, and runner’s knee with a little ingenuity.
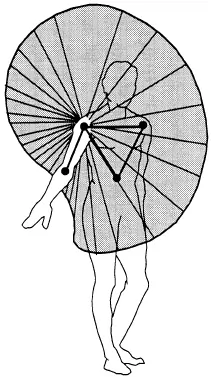
It is more difficult to regulate the temperature of the hips and shoulders for contrast bath therapy because they are wider, thicker, and frequently more fat-covered than the other body parts. Hips and shoulders are also more heavy to utilise. There is essentially no benefit to using a contrast bath for hip issues because the hip joint itself is most likely virtually entirely unaffected by its use. Naturally, contrast is much less pleasant or beneficial for conditions relating to the spine, such as back discomfort.
It appears as though ligaments should have healed after a while, but ligament sprains heal very slowly and frequently become chronically uncomfortable. Contrasting may “increase healing” from sprains, but it’s unlikely that it would, therefore any therapy to speed up healing after the first swelling should be pursued in the hopes of a few tiny advantages.
Contraindications:
If you have any of the following conditions, you should avoid using a contrast bath:
- localised cancers
- peripheral vascular diseases (PVD)
- weakened feeling
- Both, severe irritation and bleeding.
- diabetic neuropathy
If the patient’s extremities have a strong pulse, people with diabetes and neuropathies may find benefit from a contrast bath; nevertheless, this procedure must be carried out under the guidance of a physical therapist.
Again, if you’re not sure if this treatment is good for you, speak with your doctor or physical therapist.
How can contrast bath therapy be applied?
- It takes two whirlpool tubs to complete a contrast bath. Transfer warm water into the first tub and cold water into the second. The ideal temperature ranges for the warm and cold tubs are 98–110 degrees Fahrenheit and 50–60 degrees Fahrenheit, respectively.
- Since some physical therapy facilities only have one tub, they usually utilise a bucket for cold water and the tub for warm water instead of a tube.
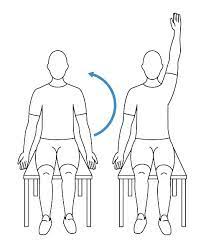
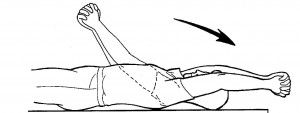
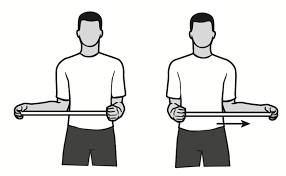
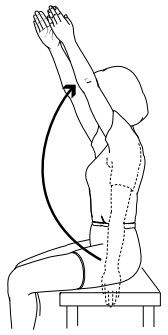
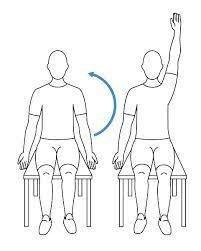
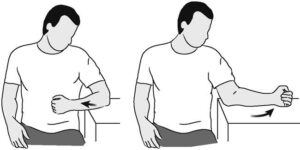
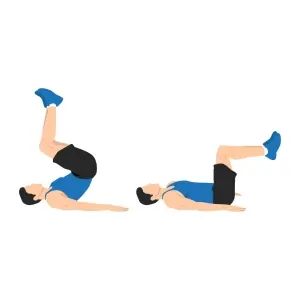
- Your damaged body part should be left in the warm whirlpool for three to four minutes by the therapist when both tubs have reached the proper temperature. Exercises involving mild motion may be required of you while receiving treatment.
- then quickly transfer the affected area to the bucket or cold tub. Be prepared since the change from hot to cold can happen quickly and dramatically.
- In overall, spend at least one minute in the water that is cold. Inform your physical therapist if you are unable to endure the low temperature for an extended period of time. They might have to put you back in the heated water.
- For twenty to thirty minutes, this pattern of going from hot to cold and back to heat is usually repeated. Make sure your physical therapist is keeping an eye on the water’s temperature as you receive treatment. To keep the baths comfortable, the temperature will frequently need to be adjusted by adding more ice or warm water.
- Your physical therapist should follow up with you after treatment to determine whether the results of the therapy were meaningful.
- must always keep in mind, to begin with hot water and finish with cold water, with the following exceptions:
- Rheumatoid arthritis: stop the hot water therapy and thoroughly dry the affected area.
Use only cold water on a joint that is really swollen and heated.
Apparatus for the contrast bath:
Two sufficiently large containers that suit the body portion that needs to be treated and have the right shape.
- A thermometer for a water bath
- Towels should be draped for drying.
- To remove the head bottle and add hot water, use a cold compress.
- This refers to heating water for cold compression and cold baths in the event that a tub or washbasin is unavailable.
Methods for applying contrast bath treatment:
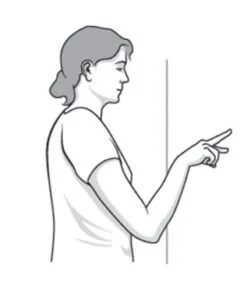
Numerous methods exist for heating and cooling the body. Keep in mind that, whenever achievable you should envelop the body part; immersion is always preferable to flow or spray. The primary temperature systems are:
- immersion: in bathtubs, buckets, or sinks
- draping: using cold packs, heating pads, or damp towels
- drizzling or the spraying: immersion from a valve in a stream, containers, and a detachable shower head.
- Contrasting should adhere to the fundamental framework below three to six cycles of cooling and heating.
- More adjustments may become ineffective at some point.
- Less than three times is most likely not worth the annoyance.
- If it’s feasible, increase the contrast’s intensity as you get hotter and colder. With certain techniques, it’s simple.
- after heating for around two minutes, comfortably warm
- Cooling for approximately a minute—not freezing, just cool enough to make your skin feel tight
- Heats up in around two minutes: hotter
- after cooling for roughly a minute: cooler
- Heating for about two minutes, or as hot as you can stand it
- Cool for approximately one minute, as cold as you can stand it.
- Many people think that cold is terrible, but you might be surprised at how bearable it is if you have a properly pre-warmed alternative option in place in case water baths are impractical or unavailable for the area that needs to be treated.
The affected area should be covered with a warm compress or heating pad, which should be left on for three to four minutes. - For one (1) minute, switch between using an ice pack covered in a towel, a frozen washcloth, or a towel.
Three more times, follow the previously stated instructions.
Some advice on contras bathing:
Remain warm. Generally speaking, you should apply the heat more slowly: for at least one minute, but possibly up to five, depending on how well your heating technique works. More comfortable and calming than cooling is heat, and the most common mistake people make when using contrast bath therapy is underheating the water.
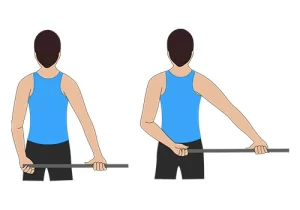
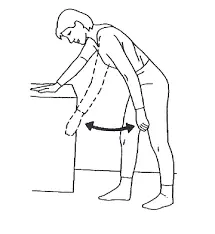
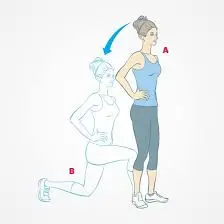
Stretch while the hot water is being treated. Stretching is caused by a fracture of the healing part, therefore avoid using it. If stretching is necessary, do it after heating. Before going on to the cold, reheat after stretching if you need to stop heating to begin the stretch.
Adjust as you go. It’s lovely, but the difference doesn’t always get stronger as you receive treatment—the hot gets hotter and the cold gets colder.
Since contrast has little effect on the deeper tissue, leave the contrast bath empty.
the temperatures in the gastrocnemius calf muscle after receiving cold contrast treatment for 30 minutes and warm water treatment for 30 minutes The deep calf muscle did receive some mild heat from the hot tub, ranging from a few degrees for hot to several degrees for cold with several fluctuations.
Nevertheless, during the contrast therapy, the temperature four cm below the skin’s surface rarely fluctuated; the calf’s depths looked to remain largely undisturbed. After the leg has warmed up, spend a minute dipping it in cold water.
It is incomprehensible that the physiological impacts suitable for the variations
Empty tissues may have a stronger effect; however, measurements were not made. Just because the temperature doesn’t change doesn’t indicate that the joints and connective tissues aren’t being meaningfully stimulated. In fact, the joints and connective tissues may react rather differently.
However, it does imply that applying a contrast bath to target empty tissues increases the likelihood of its being beneficial.
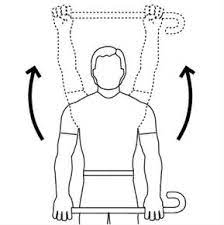
Comparing various body parts:
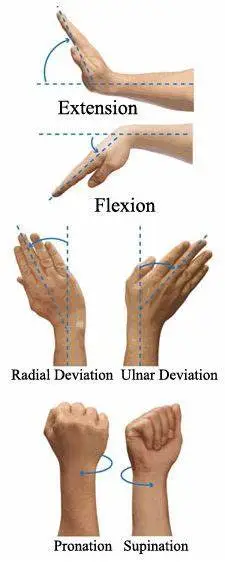
You can usually apply the contrast bath most easily to your wrists, forearms, and elbows. This comes in particularly handy if you have two sinks. Just fill one washbasin with hot water and another with cold water, then take a step back.
A water flow from the valve is an acceptable substitute if you only have one washbasin; just change the flow from hot to cold water.
A valve might not be as effective as wrapping forearms in damp towels, ice packs, or heating pads. Few people own ice packs big enough for wrapping, although big ones are reasonably priced and accessible at most medical supply stores. Towels that are wet are untidy.
In general, lower legs are harder. A pair of deep buckets requires a lot of setup work and specific buckets that are readily available; most users don’t utilise deep buckets since they are unaware of this optimal solution.
The most useful shower valves for contrast are detachable ones, but the effect is not as potent as immersion—especially with a low-flow shower head.
Generally speaking, bathtub valves provide enough water instead of a stream, which is nearly as pleasant as immersion, especially for the feet.
Knees are simple to use but challenging to submerge. Large pails are undoubtedly the best choice, but they should only be used by those who are short in stature and are simple to erect. The best course of action is usually to pour water over the knee joint, especially if you also bathe your lower legs and feet in smaller buckets.
Although the thighs and hips are especially difficult to employ contrast on, the effect was achieved by combining a hot bath with a sizable container of cold water used as a sitz bath. simple to assemble,
Although it’s not the best use for the process, contrasting the back of the spine can be done quite easily in the shower. Applying a large amount of cold water to the back of the spine might be challenging for many people.
Consequences of the contras bath at risk:
- open injuries.
- cardiac problems.
- elevated blood pressure
- deep venous thrombosis
- localised cancers
- Peripheral Vascular Disease (PVD)
- weakened feeling
- Severe bleeding and inflammation
- diabetic neuropathy
- Diabetes and neuropathies can benefit from a contrast bath if their upper and lower limb pulse rates are both healthy, but they must do it under a physiotherapist’s supervision.
- burns from overheated water
- Skin injury resulting from excessively cold water
- The easiest method to reduce these dangers is to make sure the water you use for contrast baths is at the proper temperature.
- Contrast bath therapy must be administered in pure, uncontaminated water. Infections could arise from contaminated water. An infection may be more likely to occur in the patient receiving therapy with tainted water. Adequate safety measures must be taken prior to using the contrast bath.
Safety Measures for Contrast Bathing:
- It is not recommended to use contrast baths on recently injured areas.
- It is not advisable to start treatment until 48 hours have passed after the injury.
- Contrast baths are a little less effective in colder rooms.
FAQs
How frequently are contrast baths possible?
For a maximum of fifteen minutes, the water is submerged alternately, the first and last times being in cold water. The contras baths should ideally be taken three times a day.
What is the recommended duration of submersion in cold water during contrast water therapy?
In contrast, during contrast water therapy, some athletes like to alternate between submersion in warm and cold water. Many individuals either immerse themselves in an ice bath for five to ten minutes, or occasionally up to twenty minutes, or alternate between an ice bath and moderate water immersions, lasting one to five minutes each.
Do contrast baths lessen edoema?
A typical thermal intervention used by physicians, physiotherapists, athletic trainers, and athletes to aid posttraining recovery and minimise pain, edoema, and inflammation in the upper and lower limbs is the contrast bath.
What is the duration of contras baths in your system?
Under monitoring, contraceptives are safe to use, and when you urinate or have a bowel movement, your body naturally gets rid of them in a day or two.
Can you receive contrast therapy every day?
You can utilise contrast bath therapy almost anytime, and many individuals even include it into their everyday regimen. For the best results in reducing inflammation and discomfort after a strenuous workout, contrast treatment sessions should be used right after.
A contrast bath: what is it?
A contrast bath consists of periodically immersing a limb in hot and then cold water for a predetermined duration, length, and temperature.
What is a contrast bath known by another name?
One type of hydrotherapy is a contrast bath. It’s sometimes referred to as hot/cold immersion treatment. When there may be a decrease in blood flow, it entails applying hot and cold water to the damaged area to encourage circulation and minimise discomfort.
Which conditions don’t apply to contrast baths?
These conditions preclude using a contrast bath:
Insomnia Perspiration
Skin coldness
ulcers on the legs
skin conditions.
Are baths with contrast safe?
Contrast treatment is a great, simple, safe, and inexpensive option for mending injuries when done appropriately. The idea is to get your tissues moving again after the sudden alterations, which means a lot of metabolic and circulatory activity.
Referance
- Vastralphysiotherapyclinic. (2023b, November 15). Use of Contrast Bath in Physiotherapy. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/use-of-contrast-bath-in-physiotherapy/#Contraindications
- Pt, B. S. (2024, May 3). Benefits of Hot and Cold Contrast Therapy Baths. Verywell Health. https://www.verywellhealth.com/contrast-bath-in-physical-therapy-2696628
- What Is a Contrast Bath? (2023, July 7). WebMD. https://www.webmd.com/pain-management/what-is-a-contrast-bathCopy
- Mandaliya, D. (2023a, December 13). Contrast bath therapy – Benefits, Indication, Contraindication. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/contrast-bath-therapy/#Risk_factors_of_the_contras_bath