Acute Pain
Acute pain is a fundamental sensation experienced by individuals as a result of injury, disease, or trauma. Unlike chronic pain, which persists over an extended period, acute pain typically has a sudden onset and is often temporary.
What is Pain?
When something hurts, it produces pain, which is an uncomfortable or unpleasant sensation. Pain is often a sign that something is not quite right. You are the best person to judge your pain.
Anatomy and Physiology of Pain
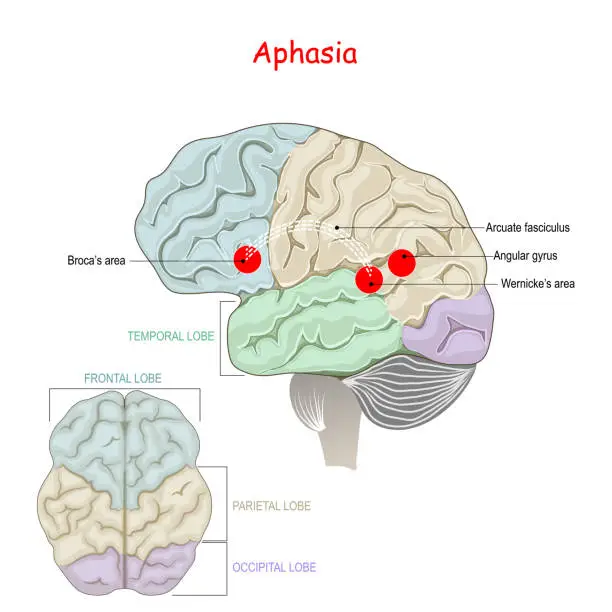
The experience of pain begins with specialized nerve endings called nociceptors. These nociceptors are found in the skin, muscles, joints, and internal organs throughout the body. They pick up on stimuli that might be dangerous, such as heat, cold, chemicals, or mechanical forces. When noxious stimuli activate the nociceptors, it causes the release of inflammatory molecules that convert the stimulus into electrical nerve impulses through a process called transduction.
These electrical impulses are then transmitted along peripheral nerves to the dorsal horn of the spinal cord. In the spinal cord, neurotransmitters like substance P activate second-order neurons that cross over or ascend along the spinothalamic tract toward the brain. This transmission and modulation of the pain signals up the spinal cord is carefully regulated by the central nervous system.
Once the pain signals reach the thalamus in the brain, they are relayed to several higher brain centers like the somatosensory cortex and limbic system. These areas are responsible for localizing and interpreting the pain signals to create the subjective, conscious experience of pain. The perception of pain is influenced by many factors including emotions, previous experiences with pain, and activation of descending inhibitory pathways that can modulate pain signals.
The central nervous system can modulate pain through these descending pathways involving opioid, serotonin, and norepinephrine signaling. This neurochemical regulation of pain is part of the body’s attempt to control the experience of acute pain in response to an injury or illness. In cases where pain persists beyond the normal healing period due to alterations in the peripheral and central nervous systems, it can transition into a chronic pain condition that is much more complex.
Types of Pain
The sensation of pain arises from the interaction among your nerves, spinal cord, and brain. Your pain can be acute, chronic, neuropathic, or nociceptive, with the last category further subdivided into visceral and somatic pain, depending on what is causing it.
As each individual perceives pain uniquely, expressing the specific type of pain you are experiencing may pose a challenge. It is possible to encounter multiple forms of pain simultaneously, complicating the situation further.
Familiarizing yourself with the distinct varieties of pain can facilitate communication with your healthcare provider and aid in articulating your symptoms more effectively. Explore the primary types of pain discussed here to gain insight into how they manifest physically.
Acute Pain
Short-term pain that occurs suddenly due to a specific reason, typically related to tissue damage, is known as acute pain. It usually lasts for less than half a year and disappears once the root cause is addressed.
Acute pain often begins as a sharp or intense sensation before gradually getting better.
Some common triggers of acute pain are fractures, surgical procedures, dental treatments, labor and delivery, lacerations, and burns.
Chronic Pain
Pain that lasts longer than six months, even after the initial injury has healed, is referred to as chronic pain.
This type of pain can continue for extended periods, varying in intensity from mild to severe each day. It affects approximately 50 million adults in the United States, making it quite common. Sometimes, chronic pain can occur without any clear cause.
If not properly managed, chronic pain can significantly reduce one’s quality of life. Those living with chronic pain may experience symptoms of anxiety or depression as a result.
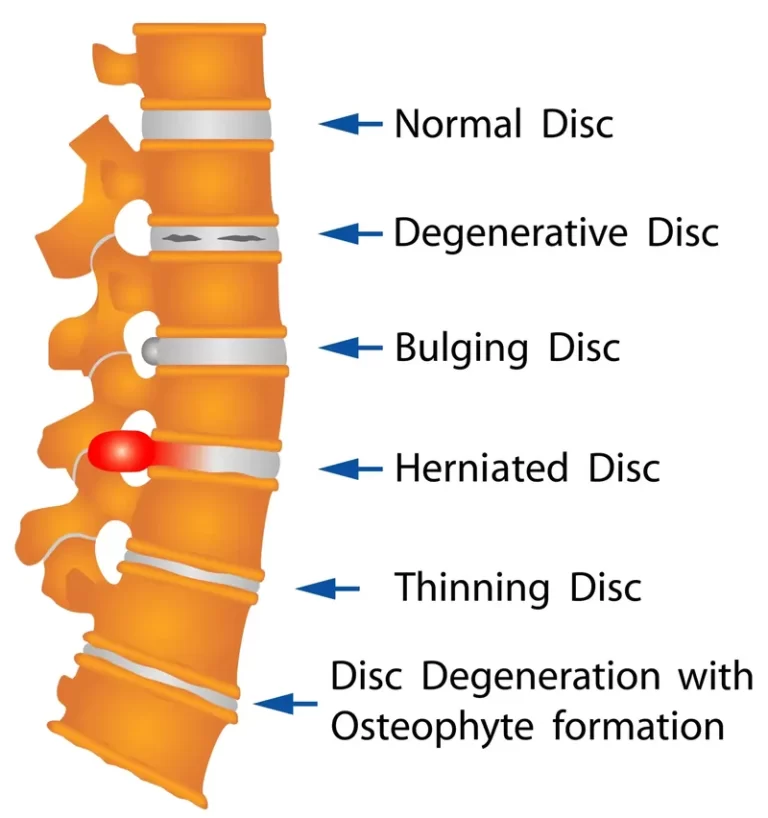
Chronic pain can often be accompanied by other symptoms including exhaustion, tight muscles, and reduced movement. Frequent headaches, pain connected to nerves, lower back pain, arthritis, and fibromyalgia are common instances of chronic pain.
Nociceptive Pain
Nociceptive pain, the most common type of pain, arises from the activation of nociceptors, which are receptors that respond to tissue damage. These nociceptors are distributed throughout the body, particularly in the skin and internal organs. When they detect potential harm, such as a wound or injury, they transmit electrical signals to the brain, resulting in the sensation of pain.
This type of pain is usually felt in reaction to inflammation or injury. Nociceptive pain may manifest as either acute or chronic and can be categorized as visceral or somatic based on its origin.
Visceral Pain (Internal Pain)
Internal pain arises from injuries or harm to your inner organs. It can be felt in the core of your body, encompassing the chest, abdomen, and pelvis. Pinpointing the exact source of internal pain is often challenging.
Internal pain is commonly characterized by feelings of pressure, aches, squeezing, or cramping. Additional symptoms may include nausea, vomiting, and changes in body temperature, heart rate, or blood pressure.
Causes of internal pain may include conditions such as gallstones, appendicitis, and irritable bowel syndrome.
Somatic Pain
Somatic pain arises from the activation of pain receptors in your body’s tissues rather than your internal organs, encompassing the skin, muscles, joints, connective tissues, and bones. Unlike visceral pain, somatic pain is typically easier to localize.
Somatic pain is often described as a persistent dull or nagging sensation and can be categorized as either deep or superficial. For instance, a tear in a tendon causes deep somatic pain, while a canker sore on the inner cheek results in superficial somatic pain.
fractures of the bones, tense muscles, disorders of the connective tissues including osteoporosis, cancers of the skin or bones, cuts, scratches, and burns on the skin, and joint discomfort such as arthritis, are a few examples of somatic pain. To learn more about the distinctions between somatic and visceral pain, continue reading.
Neuropathic pain
Neuropathic pain arises from nerve damage or dysfunction within the nervous system. This leads to the misfiring of pain signals by damaged or dysfunctional nerves, causing a sensation of pain seemingly without any specific trigger.
Individuals experiencing neuropathic pain may also encounter pain sensations in response to typically non-painful stimuli, such as exposure to cold air or contact with clothing.
Common descriptors for neuropathic pain include feelings of burning, freezing, numbness, tingling, shooting, stabbing, and electric shocks. Various factors can contribute to neuropathic pain, including diabetes, chronic alcohol consumption, accidents, infections, facial nerve issues like Bell’s palsy, spinal nerve inflammation or compression, shingles, carpal tunnel syndrome, HIV, central nervous system disorders such as multiple sclerosis or Parkinson’s disease, radiation, and chemotherapy drugs.
What divides acute pain from chronic pain?
Acute pain typically flares up quickly and has a specific cause. It has a clean quality. Typically, acute pain decreases after six months. When the pain has no more underlying cause, it goes away. Acute pain can be brought on by:
- Surgery
- Shattered bones
- Dental procedures
- Wounds or burns
- The Birth Process and labor
You can get back to your normal activities after the acute pain subsides.
Persistent pain is defined as pain that persists for more than six months. Even after the disease or injury that initially caused it has healed or disappeared, this kind of pain may persist. For weeks, months, or even years, pain signals in the nervous system are still active. Even in the absence of apparent physical damage or prior injuries, some people experience chronic pain.
Chronic pain is linked to the following conditions:
- Ache
- Arthritis
- Cancer
- Neural pain
- Pain is in the back
- The fibromyalgia
When you experience chronic pain, stress has an impact on your body and can lead to physical conditions such as:
- Tight muscles
- Restricted mobility
- An absence of vigor
- Alterations in appetite
Additionally, the emotional effects of chronic pain include:
- Depression
- Anger
- Fear and anxiety
- dread of getting hurt again
Your ability to resume work or leisure activities may be restricted by this fear.
What is Acute Pain?
Acute pain is felt right away or shortly after suffering an injury, such as a bone fracture, fall, or auto accident. It is your body’s way of telling you that you have been hurt. The pain subsides when the wound heals.
Pain is experienced by patients after they sustain an injury or trauma. Depending on the injury, the pain may be either dull or intense.
For as long as the injury is present, the symptoms may persist. This means that although acute pain may only last a short while, its duration usually reflects the severity of the injury and it may take weeks or months for it to go away completely.
Causes of Acute Pain
Acute pain can be caused by physical injury. Acute pain can have several causes, such as:
- Fracturing a bone
- Acquiring an infection as a result of an open wound
- Receiving a burn
- Cramping during one’s menstruation
- Possessing kidney stones
- Giving birth
- Tumbling
- Striking a body part that is hard against a surface
- Pulling a muscle
The severity of the injury or its cause determines the range of pain that an individual can experience with acute pain.
Signs & Symptoms of Acute Pain
Acute pain’s most typical indications and symptoms include:
- Tingling
- Weakness
- Burning
- Stabbing
- Sharp pain
- Numbness
Complications and Risk Factors of Acute Pain
Acute Pain Risk factors
It might appear like acute pain is worse if you:
- Are female
- Are more seniors
- possess genetic alterations that impact pain perception.
Acute pain complications
- After an injury or illness has healed, acute pain usually goes away. A day or several months may pass while in pain.
However, pain turns into chronic pain if it lasts more than three to six months after you get better.
How do doctors diagnose acute pain?
Pain perception varies from person to person, posing a challenge in diagnosing conditions accurately. Individuals must share their complete medical history with healthcare providers.
The healthcare provider will rely on the individual’s description of their pain to determine the underlying cause. They will encourage the patient to explain their pain by inquiring about:
- Triggers that worsen the pain
- Intensity of pain
- Patient’s interpretation of the pain
- Impact of pain on mood and daily activities
- Location of pain in the body and its extent
You might be asked to rate your pain on a scale from 1 to 10 by your doctor.
To determine the cause of your pain, they might also prescribe the following tests:
- Blood examinations
- CT scan
- MRI
- Ultrasonic
- X-ray
Tests for electrodiagnosis If there are issues with the way your nerves are communicating with your brain, let your doctor know.
How to Treat Acute Pain?
The management of sudden pain relies on the root cause. approaches to treating sudden pain may involve:
- Rest
- Medications like aspirin, acetaminophen, ibuprofen, and naproxen
- Heat or cold therapy
In certain situations, a doctor may prescribe more potent pain medications based on the intensity of the sudden pain. For instance, opioids are utilized to address severe sudden pain resulting from significant surgeries, cancer, or fractures.
According to a 2020 study review, cannabis may be an effective treatment for acute, short-term pain, particularly when injected directly into the muscle Nonetheless, the writers highlight that the supporting evidence is of poor quality.
Treat acute pain with medications
For immediate relief, consider over-the-counter options such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs).
If you’re in severe pain, your doctor might suggest:
- Anti-seizure medications to alleviate numbness and tingling from nerve damage.
- Corticosteroid injections are given directly into the injured area to reduce inflammation.
- Muscle relaxants to ease tension in muscles.
- Prescription opioids for intense acute pain. Discuss potential addiction risks with your doctor before using these medications.
Massage Therapy for Acute Pain
In case your physician recommends, massage therapy can in:
- Easing acute pain following an injury or surgery.
- Promoting relaxation.
- Increasing the range of motion in your muscles and joints.
Massage therapy can be an effective complementary treatment for various types of acute pain. The therapeutic manipulation of soft tissues helps reduce muscle tension, improve blood flow, and promote relaxation. Some key ways massage may alleviate acute pain include:
- Releasing muscle spasms and knots that often accompany acute injuries
- Increasing range of motion and flexibility in affected areas
- Reducing inflammation through manual lymphatic drainage techniques
- Encouraging the body’s painkillers, endorphins, to be released
- Interrupting the pain-spasm cycle that can prolong acute pain conditions
Massage strokes like effleurage, petrissage, and frictions are commonly used. Techniques are tailored based on the type and location of acute pain being treated. For example, lighter Swedish massage is often used for acute low back pain, while deeper myofascial or trigger point therapy may help acute neck or shoulder pain.
Physical therapy for Acute Pain
A physical therapist can assist in reducing discomfort in the injured area by:
- Engaging in stretching exercises.
- Performing strengthening exercises.
- Giving you exercises to perform on your own time at home.
When it comes to treating and managing acute pain disorders, particularly those resulting from accidents, surgeries, or musculoskeletal problems, physical therapy is essential.
Key ways PT can address acute pain:
- Rehabilitation-focused exercises to increase strength, flexibility, and range of motion
- Manual therapies like joint mobilizations to improve mobility
- Pain management techniques such as electrical stimulation, ultrasound, and dry needling
- Patient education on proper body mechanics, postures, and movements
- Guidance on activity modification to allow healing while staying active
The physical therapist will do an assessment in order to create a customized treatment plan that addresses the cause of acute pain as well as any associated functional deficiencies. Early, appropriate PT can help decrease pain levels, restore normal movement patterns, and prevent acute conditions from becoming chronic.
Topical Treatment for Acute Pain
- Your doctor might employ either cold or heat therapy to address sudden pain in the affected region.
- Alternatively, you can utilize ointments or gels containing medication to alleviate the pain.
Topical analgesics offer localized pain relief options that can be used alone or in combination with other medications or therapies for acute pain conditions. Common topical treatments include:
- Salicylates like methylsalicylate creams or ointments
- Menthol or camphor-based rubs that create a cooling/warming sensation
- Topical NSAIDs like diclofenac gels or patches
- Lidocaine patches that numb the painful area
- Capsaicin creams made from chili peppers deplete pain neurotransmitters
The advantages of topical treatments are that they bypass the systemic circulation to deliver pain relief directly to the affected area. They might not have as many adverse effects as pills. The drawbacks are they only work for localized, superficial pain.
Topical analgesics are often used for acute musculoskeletal pains like sprains, strains, arthritis, or neuropathic pain conditions. Proper application instructions should be followed as some may cause skin irritation with overuse.
When to seek medical attention
- Severe, Unbearable Pain: If you are experiencing excruciating, unbearable acute pain, it’s time to get evaluated. Severe pain that rates 8 or higher on a 10-point scale merits having a doctor examine the underlying cause.
- Sudden, Intense Pain: Any sudden onset of intense pain, especially in the abdomen, chest, or head should prompt seeking emergency medical care right away. This could signal a serious condition like appendicitis, kidney stones, heart attack, or aneurysm.
- Injury with Severe Pain: Injuries like fractures, dislocations, deep cuts, burns, or crush injuries that cause severe acute pain require prompt medical evaluation and treatment.
- Pain After Surgery/Procedure: If you have severe uncontrolled pain following a surgery, procedure, or medical treatment, you should contact your doctor, as this could indicate a complication.
- Fever and Pain: When acute pain is accompanied by a fever over 102°F, it could be a sign of infection or an underlying illness that needs treatment.
- Neurological Symptoms: Seek prompt care if acute pain is accompanied by concerning symptoms like confusion, dizziness, vision changes, numbness, or weakness, as this may indicate a neurological issue.
- Persistent Pain: Any severe acute pain that persists for more than a few days despite treatment or worsens over time instead of improving should be evaluated.
- Difficulty Functioning: If acute pain is so severe that it prevents you from being able to sleep, work, walk, or carry out normal activities, medical care may be needed.
Summary
Acute pain is a type of pain that typically comes on suddenly and is caused by something specific. Unlike chronic pain, acute pain is a normal sensation that alerts us to possible injury or illness. Acute pain goes away once the underlying cause has been treated or healing occurs.
Some common causes of acute pain include injuries like sprains, fractures, cuts, and burns. It can also result from medical conditions or procedures like surgery, labor and childbirth, dental work, or acute illnesses like appendicitis or kidney stones. The severity can range from mild to severe agonizing pain.
In most cases, acute pain is a protective mechanism – it makes you immobilize the injured area and rest it to avoid further harm. However, severe acute pain requires treatment to make it more manageable and allow healing. Treatment options include over-the-counter medications like acetaminophen or NSAIDs, prescription pain relievers, nerve blocks, steroid injections, or other interventions depending on the underlying cause.
While acute pain is unpleasant, it is typically short-lived once the injury or condition resolves. Chronic pain that persists for weeks or months is different and often more difficult to treat. If acute pain doesn’t improve with treatment or lasts longer than expected for the condition, it’s important to follow up with a doctor.
Managing acute pain effectively not only increases comfort during recovery but can also support better healing and prevent the transition to chronic, persistent pain.
FAQs
What is acute pain?
Acute pain is a type of pain that comes on suddenly and is caused by a specific injury, illness, or event. It acts as a warning sign that something is wrong in the body.
How does acute pain differ from chronic pain?
Acute pain starts suddenly and is temporary, going away once the underlying cause is treated or heals. Chronic pain persists over a longer period, lasting more than 3-6 months.
What are some common causes of acute pain?
Common causes include injuries like sprains, fractures, burns, cuts, and bruises. It can also result from medical conditions or procedures like surgery, dental work, childbirth, kidney stones, or appendicitis.
How severe can acute pain be?
The severity can range from mild to agonizing and disabling. Things like bone fractures or severe burns often cause extreme acute pain.
What treatments are used for acute pain?
Over-the-counter medications like acetaminophen, NSAIDs, or prescription painkillers are common treatments. Other options include nerve blocks, steroid injections, immobilization, ice/heat therapy, etc.
How long does acute pain typically last?
Acute pain is temporary, usually going away within days or weeks once the underlying condition is treated and healing occurs. If it persists for months, it may become chronic pain.
Are there any risks with acute pain?
Severe, uncontrolled acute pain can lead to complications like inability to sleep, anxiety, depression, poor healing, and an increased risk of developing chronic pain.
When should I see a doctor for acute pain?
You should see a doctor if you experience sudden, severe pain, if pain persists for more than a week or two despite treatment, or if pain disrupts your daily activities.
References
- Acute Pain – International Association for the Study of Pain (IASP). (2023, January 12). International Association for the Study of Pain (IASP). https://www.iasp-pain.org/resources/topics/acute-pain/
- Acute Pain Causes, Symptoms, and Treatments | UPMC. (n.d.). UPMC | Life Changing Medicine. https://www.upmc.com/services/pain-management/conditions/acute-pain
- Crna, R. N. M. (2021, June 15). Pain Relief Basics. Healthline. https://www.healthline.com/health/pain-relief
- Johnson, Q., Borsheski, R. R., & Reeves-Viets, J. L. (2013). A Review of Management of Acute Pain. Missouri Medicine, 110(1), 74-79. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6179627/
- Santos-Longhurst, A. (2018, November 29). Types of Pain: How to Recognize and Talk About Them. Healthline. https://www.healthline.com/health/types-of-pain#other-considerations
- Pollock, D. M. (2023, March 31). What is the difference between acute and chronic pain? https://www.medicalnewstoday.com/articles/acute-vs-chronic-pain#summary
- Clinic, O. (2023, October 10). What is Acute Pain? The Orthopedic Clinic. https://orthotoc.com/what-is-acute-pain/





3 Comments