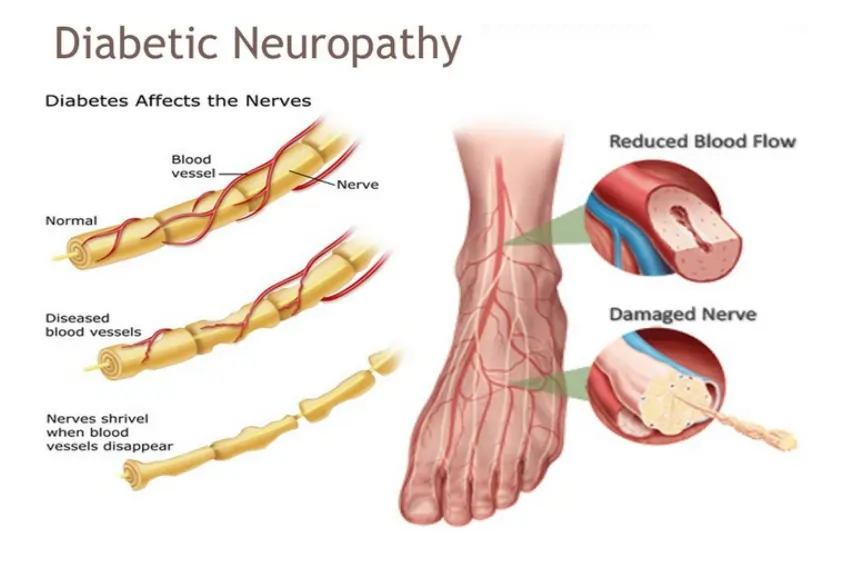
Diabetic Neuropathy
Diabetic neuropathy is a kind of nerve injury that can develop in persons with diabetes. It is caused by excessive blood sugar levels that accumulate over time and can harm nerves throughout the body.
Neuropathy refers to injury to the nerves of the peripheral nervous system. Diabetes is the leading cause of neuropathy. It most usually affects the nerves in the feet and hands, although any nerve can be affected, including those that regulate internal organs (autonomic nerves).
Up to half of all diabetics develop neuropathy during their illness. There is no cure. Management seeks to alleviate symptoms while lowering the risk of additional problems.
What is Diabetic Neuropathy?
- Diabetic neuropathy is a kind of nerve injury that can develop when you have diabetes. High blood sugar (glucose) can cause nerve damage throughout the body. Diabetic neuropathy often destroys nerves in the legs and feet.
- Diabetic neuropathy symptoms might include discomfort and numbness in the legs, feet, and hands, depending on the nerves involved. It can also have negative effects on the digestive system, urinary tract, blood vessels, and heart. Some people experience modest symptoms. Others, however, may have severe discomfort and disability as a result of diabetic neuropathy.
- Diabetic neuropathy is a significant diabetes complication that affects up to half of all diabetics. Still, diabetic neuropathy may usually be prevented or at least slowed down in progression with regular blood sugar control and a healthy lifestyle.
Causes of the Diabetic Neuropathy
Although the specific causes of diabetic neuropathy are unknown, there are many factors such as:
- High blood glucose levels. High blood glucose levels alter chemical changes in neurons, impairing their capacity to carry messages. It can also harm blood arteries, which transport oxygen and nutrients to the neurons.
- Metabolic considerations. In addition to glucose levels, high triglyceride, and cholesterol levels are linked to an increased risk of neuropathy. Patients who are overweight or obese have a higher chance of acquiring neuropathy.
- Factors that can be inherited. Some hereditary features may make certain persons more vulnerable to nerve illness than others.
- Inflammatory processes: Elevated blood sugar levels can activate inflammatory processes in the body, contributing to nerve damage.
While high blood sugar is the primary cause, several conditions might increase the chance of developing diabetic neuropathy, including:
- The duration of diabetes: The longer you have diabetes, the higher your chances of having neuropathy.
- Poor blood sugar control: Inconsistent blood sugar management considerably raises the risk of nerve injury.
- Some medical conditions: Conditions such as high blood pressure, high cholesterol, and renal illness can exacerbate neuropathy.
- Lifestyle Factors: Smoking, alcohol abuse, and obesity can all lead to nerve injury and aggravate neuropathy.
- Vitamin deficiencies: Deficiencies in some vitamins, notably vitamin B12, might raise the risk of neuropathy.
Symptoms of Diabetic Neuropathy
Symptoms of neuropathy can arise gradually. The nerves of the foot are frequently the first to be damaged. This might result in painful “pins and needles” in your feet.
Symptoms vary according to the areas affected. Common symptoms of diabetic neuropathy include:
- Sensitivity to touch.
- Loss of touch.
- Walking coordination is challenging.
- Numbness as well as pain in the feet or hands.
- Feet burn, particularly at night.
- Muscular weakness or wasting.
- Bloating or fullness.
- Symptoms may include nausea, indigestion, and vomiting.
- Diarrhea or constipation.
- Dizziness upon standing up.
- Sweating can be excessive or reduced.
- Bladder issues include inadequate bladder emptying.
- Vaginal dryness.
- Erectile dysfunction.
- The inability to detect low blood glucose.
- Double vision is a type of visual problem.
- Increased heart rate.
Types of Diabetic Neuropathy
Neuropathy refers to a variety of nerve injuries. Diabetes patients might have four types of neuropathy.
Peripheral neuropathy
Peripheral neuropathy is the most common kind of neuropathy. Peripheral neuropathy mostly affects the feet and legs, although it can also affect the arms and hands. Symptoms vary from moderate to severe. They include:
- Numbness
- Tingling or burning feelings.
- Extreme sensitivity to touch and insensitivity to hot/cold temperatures.
- Symptoms may include severe pains, cramps, and muscular weakness.
- Loss of balance and coordination
Autonomic neuropathy
The second leading type of neuropathy among diabetics is autonomic neuropathy. The autonomic nervous system regulates other systems in your body over which you have no conscious control. It controls several organs and muscles, including yours.
- The digestive system
- Sweating glands, sexual organs, and the bladder.
- The cardiovascular system
Digestive difficulties
- Nerve injury to the digestive tract can lead to constipation, diarrhea, difficulty swallowing, and gastroparesis (slow stomach emptying into the small intestine).
- Gastroparesis causes a delay in digestion, which can increase with time, resulting in frequent nausea and vomiting. You’ll usually feel full too soon and be unable to complete your food.
- Delayed digestion makes it more difficult to manage blood glucose levels, which regularly fluctuate between high and low values.
- Hypoglycemic signs, such as perspiration and heart palpitations, can often go unnoticed in persons with autonomic neuropathy. This can include failing to notice low blood sugar, which increases the likelihood of a hypoglycemia emergency.
Sexual and bladder issues
- Autonomic neuropathy can also cause sexual issues like erectile dysfunction, vaginal dryness, and trouble attaining orgasm. Neuropathy in the bladder might result in incontinence or make it difficult to empty your bladder.
Cardiovascular issues
- Damage to the nerves that regulate your heart rate and blood pressure might cause them to respond slowly. When you rise from a sitting or reclining position or exert yourself, your blood pressure may drop and you may feel light-headed or dizzy. Autonomic neuropathy can also result in an excessively quick heartbeat.
- Autonomic neuropathy might make it harder to recognize some signs of a heart attack. When your heart does not receive enough oxygen, you may not experience chest discomfort. If you have autonomic neuropathy, you should be aware of the additional signs of a heart attack, including:
- Symptoms may include excessive perspiration, discomfort in arms, back, neck, jaw, or stomach, and, shortness of breath, nausea, lightheadedness.
Proximal neuropathy/Diabetic Amyotrophy
- Proximal neuropathy, or diabetic amyotrophy, is an uncommon kind of neuropathy. This kind of neuropathy is more frequent in persons over the age of 50 with type 2 diabetes, and men are more likely to be diagnosed.
- It often affects the hips, buttocks, and thighs. You may encounter sudden, intense pain. Muscle weakness in your legs may make it difficult to stand without help. Diabetic amyotrophy often affects just one side of the body.
- After the starting of symptoms, they normally worsen until gradually improving. Even if no therapy is given, most patients recover within a few years.
Focal neuropathy/Mononeuropathy
- Focal neuropathy, also known as mononeuropathy, occurs when one or more particular nerves are damaged, resulting in weakness in the affected region. This happens most frequently in your hand, head, chest, or leg. It arises unexpectedly and is generally quite painful.
- Most localized neuropathies, including proximal neuropathy, resolve within a few weeks or months and cause minimal long-term harm. The most prevalent kind is carpal tunnel syndrome.
- Although most people do not have carpal tunnel syndrome symptoms, around 25% of diabetics suffer from nerve compression at the wrist.
- Focal neuropathy symptoms include discomfort, numbness, tingling in fingers, difficulty focusing, double vision, and eye aches.
- Bell’s palsy.
- Pain in specific locations such as the front of the thigh, lower back, pelvic region, chest, stomach, within the foot, outside the lower leg, or weakness in the big toe.
Diagnosis of the Diabetic Neuropathy
- Patients with diabetic neuropathy have the highest chance of receiving appropriate therapy when diagnosed early. However, since not all pain in the foot or limbs is indicative of diabetic neuropathy, a precise diagnosis is necessary to guarantee the right course of care.
- However, since not all pain in the foot or limbs is indicative of diabetic neuropathy, a precise diagnosis is necessary to guarantee the right course of care.
- Diagnosing diabetic neuropathies involves a clinical examination, history, and relevant laboratory tests. Your physician might: Examine your reflexes and muscle strength.
- Assess the sensitivity of your muscles to temperature, vibration, posture, and light touch.
Ask for further testing, like:
- Use an ultrasound to assess the health of various urinary system components.
- To find out how muscles react to electrical impulses, use electromyography.
- Studies on nerve conduction monitor the passage of electrical electricity via a nerve.
- Skin biopsies to assess the innervation of the cutaneous nerve.
- Muscle and nerve biopsies for histological analysis.
A complete assessment, which includes a review of blood pressure, cholesterol, and blood glucose tests, along with more sophisticated screening, aids in the doctor’s ability to rule out alternative explanations and pinpoint the main issue.
Differential Diagnosis of the Diabetic Neuropathy
Although peripheral neuropathy is most commonly caused by diabetic neuropathy, it’s important to remember that other illnesses may have their symptoms. A differential diagnosis is also crucial to rule out other possible reasons and guarantee appropriate therapy. The following important conditions are taken into consideration while making a differential diagnosis of diabetic neuropathy:
Nutritional Deficiencies:
- Vitamin B12 shortage: This shortage mostly affects the hands and feet and can result in symptoms like numbness, tingling, and weakness.
- Additional vitamin deficits: Vitamin B1, B6, and E deficiencies may also be a factor in neuropathy.
The Toxic Neuropathy
- Abuse of alcohol: Prolonged alcohol use can harm nerves, resulting in neuropathy that resembles diabetic neuropathy in symptoms.
- Toxin exposure: Several substances, such as heavy metals and pharmaceuticals used in chemotherapy, can lead to neuropathy.
Conditions related to inflammation and immunity:
- GBS: Guillain-Barre syndrome is an autoimmune disease that targets the nerves, rapidly leading to numbness and paralysis.
- Chronic inflammatory demyelinating polyneuropathy (CIDP): The symptoms of this condition grow more slowly than those of GBS.
- Vasculitis: When blood arteries become inflamed, it can limit blood supply to nerves, resulting in harm and neuropathy.
Hereditary Neuropathologies:
- A collection of hereditary conditions known as Charcot-Marie-Tooth disease (CMT) damages the peripheral nerves, resulting in foot malformations, numbness, and weakness.
- Other hereditary neuropathies: Several different genetic disorders can result in neuropathy, each with its own set of signs and manifestations.
Additional Health Issues:
- A buildup of toxins in the bloodstream from kidney illness can result in uremic neuropathy, which can cause numbness, tingling, and weakness.
- Hypothyroidism: Signs of an underactive thyroid gland include weakness, exhaustion, and occasionally numbness, which can be misinterpreted as neuropathy.
- Neuropathy may result from HIV/AIDS, especially in the advanced stages of the infection.
Risk factors of the Diabetic Neuropathy
Here are some of the risk factors for diabetic neuropathy.
- Poor blood sugar control: Over time, high blood sugar levels can cause nerve damage throughout the body.
- Long duration of diabetes: The longer you have diabetes, the more likely you are to develop neuropathy.
- Age: The risk of neuropathy rises with age.
- Smoking causes blood arteries to constrict, reducing blood flow and damaging neurons.
- Obesity: Being overweight or obese raises your risk of neuropathy.
- High blood pressure can cause nerve injury.
- High cholesterol: High cholesterol levels might cause nerve damage.
- Kidney disease: Kidney illness can impair the body’s capacity to eliminate waste items from the blood, potentially damaging nerves.
- Alcohol consumption can harm nerves and exacerbate neuropathy symptoms.
- Prediabetes: Having prediabetes, which is characterized by higher-than-normal blood sugar levels but not high enough to be diagnosed as diabetes, increases your chance of getting neuropathy.
- A family history of neuropathy might further raise your risk.
- It is critical to manage your diabetes properly to help avoid or decrease the growth of neuropathy. This involves managing your blood sugar levels, eating a balanced diet, exercising frequently, and quitting smoking. If you have any concerns regarding diabetic neuropathy, speak with your doctor.
Management and Treatment for Diabetic Neuropathy
Diabetes neuropathies are treated in two stages: with lifestyle modifications and, in rare cases, drugs to achieve optimal diabetes control, and with symptomatic pain and associated consequences.
Controlling blood glucose levels
- Controlling blood glucose levels cannot cure nerve damage, but it can prevent more damage from developing. Your doctor will assign you precise blood sugar targets. To manage these levels, consume a protein-rich, low-carbohydrate diet. When eating carbohydrates, aim to pick foods with more fiber and avoid chips and soda.
- Regular exercise can help maintain blood sugar levels by boosting insulin sensitivity, which means you’ll require less insulin each day. Getting enough sleep is also key since we tend to seek high-carb foods when we are fatigued.
Reducing Other Risk Factors
- Controlling blood glucose is vital, but it may not be sufficient. It is also critical to manage other risk factors such as excessive triglycerides or cholesterol, address high blood pressure, and stop smoking. Daily aerobic exercise has been demonstrated to help preserve nerves and improve neuropathy results. Losing weight is especially helpful for those who are obese or overweight.
Managing Pain and Other Complications
Diabetic neuropathy can result in chronic discomfort and consequences such as gastrointestinal issues, dizziness and weakness, and urinary or sexual difficulties. Treatment options include pain medicines.
- Anti-epileptic medicines.
- Antidepressants.
- Topical creams.
- Transcutaneous electrical nerve stimulation (TENS).
- Hypnosis.
- Relaxation training.
- Biofeedback training.
- Physical therapy.
- Acupuncture.
Treatment will depend on your unique symptoms and the degree of your neuropathy.
Check your feet frequently for ingrown toenails, blisters, and ulcers, especially if you have peripheral neuropathy. Because of the numbness associated with neuropathy, you may not notice when these diseases develop. Keeping your feet clean and protected can help protect them from harm and future concerns like infections.
Surgery
- If you have neuropathies caused by nerve pressure, such as tumor pressure, surgery may be necessary to relieve the pressure.
Physical Therapy for the Diabetic Neuropathy
Physical therapy can be a useful strategy in controlling diabetic neuropathy, assisting with:
Physical therapists can reduce pain and suffering using treatments such as manual therapy, electrical stimulation, and particular exercises.
- Improve balance and avoid falls: Neuropathy can impair your sense of sensation and coordination, increasing your risk of falling. Physical therapists can help you improve your balance and stability with gait training and particular exercises.
- Maintain or develop muscular strength: Nerve damage can cause weakness, which impairs your ability to perform daily tasks. Physical therapists can create a safe and effective training program to strengthen muscles and enhance function.
- Increase your flexibility: Neuropathy can be characterized by muscle and joint tightness and stiffness. Physical therapists can help you increase your flexibility and range of motion by teaching you stretching exercises.
- Promote wound healing: Neuropathy can impair feeling in your feet, leaving you more prone to undiscovered injuries. Physical therapists can teach you correct foot care and assist with wound healing if necessary.
The following are some of the particular methods utilized in physical therapy for diabetic neuropathy:
Exercise is an essential component of physical therapy for neuropathy. Exercises may include:
- Aerobic Activities: Moderate-intensity workouts such as walking, swimming, or cycling can help with blood sugar management, circulation, and general health.
- Strength training can help with balance, stability, and daily function.
- Flexibility exercises: Stretching regularly helps you maintain a healthy range of motion and minimize stiffness.
- Balance and gait training can assist improve coordination and stability while also preventing falls.
- Massage and mobilization are examples of manual treatment techniques that can enhance blood flow, relieve pain, and induce relaxation.
- Electrical stimulation: Using low-intensity electrical currents to relieve pain and enhance muscular function.
- Education: Physical therapists may teach you about self-care practices, basic foot care, and how to manage your condition efficiently.
- Assistive Device: Physical therapists may also suggest braces and/or splints to improve balance and posture. Splinting is frequently utilized in the treatment of compression mononeuropathies such as carpal tunnel syndrome.
Occupational Therapy
Occupational therapy can assist a patient deal with the functional, occupational, and social consequences of peripheral neuropathy by:
- Improving sensory-motor abilities.
- Teaching the patient how to prevent exposure to environmental or industrial pollutants.
- Teach self-care activities.
- Teaching patients about safety problems (e.g., paying closer attention to the ground when walking because slipping or tripping may constitute a danger for patients with PN)
- Teach the patient to pay attention to concerns involving automatic functions (for example, learning how to change positions smoothly to avoid a fast decrease in blood pressure and the danger of collapsing). If you have muscular weakness, exercising can help you move better. A wheelchair, walker, cane, or hand or foot braces can also be necessary.
Physical therapy for diabetic neuropathy should be tailored to your personal needs and the severity of your ailment. To ensure a safe and successful treatment plan, consult with a trained physical therapist who has expertise in managing diabetic neuropathy.
Remember, while physical therapy can provide considerable advantages, you should always check your doctor before beginning any new treatment program, especially if you have any concerns or other health issues.
Prevention for the Diabetic Neuropathy
Diabetic neuropathy, or diabetes-related nerve damage, can lead to a variety of consequences if not controlled properly. The following are several possible problems:
- Foot Ulcers and Amputations: Neuropathy can cause loss of feeling in the feet, making it harder to detect injuries such as cuts, blisters, or ulcers. These injuries are quickly infected and lead to severe ulcers. If left untreated, these ulcers can cause tissue death and, ultimately, amputation of the toe, foot, or even lower leg.
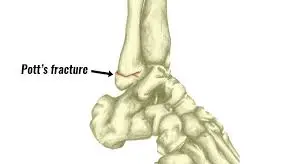
- Charcot foot: A rare but dangerous consequence of diabetic neuropathy affecting the foot’s bones, joints, and soft tissues. It can cause bones to weaken, fracture, or dislocate, resulting in deformity and discomfort.
- Digestive issues: Neuropathy can impair the nerves that regulate digestion, resulting in constipation, diarrhea, nausea, vomiting, and gastroparesis.
- Urinary problems: Nerve injury to the bladder and urinary system can cause difficulties emptying the bladder (urinary retention), frequent urination, and incontinence.
- Sexual dysfunction: Neuropathy can impair the nerves that control sexual desire and function, resulting in erectile dysfunction in males and vaginal dryness or reduced libido in women.
- Cardiovascular problems: Autonomic neuropathy, a kind of neuropathy that affects the nerves that govern automatic activities such as heart rate and blood pressure, might raise the risk of a heart attack, stroke, or sudden death.
- Pain: Chronic pain is a typical symptom of diabetic neuropathy that can hurt a person’s quality of life. The pain might be searing, tingling, stabbing, or throbbing, and it can affect the hands, feet, legs, and other parts of the body.
It’s crucial to realize that these are possible problems, and not everyone with diabetic neuropathy will have them. However, being aware of the hazards is critical for diabetics to efficiently regulate their blood sugar levels and seek medical assistance as soon as they notice any troubling symptoms. Early detection and treatment of diabetic neuropathy can help avoid or decrease the course of nerve damage, lowering the likelihood of complications.
Prevention for the Diabetic Neuropathy
While there is no 100% effective approach to avoid diabetic neuropathy, some treatments can dramatically lower your risk and perhaps halt its progression:
- Maintain proper blood sugar control: This is the most important preventive step. Aim to maintain stable blood sugar levels within your doctor’s suggested range. This may include nutrition, exercise, and medication management, as determined by your healthcare provider.
- Handle additional health issues: High blood pressure, high cholesterol, and obesity can all lead to nerve injury and aggravate neuropathy. Consult your doctor about ways to manage these diseases through lifestyle changes and, if necessary, medication.
- Stop smoking. Smoking dramatically reduces blood flow and oxygen availability to neurons, hastening nerve degeneration. Quitting smoking is critical for your general health and neuropathy prevention.
- Limit alcohol consumption: Too much alcohol can directly damage nerves and exacerbate neuropathy symptoms. Moderate alcohol intake is typically suggested, but please check with your doctor for particular advice.
- Maintain a healthy weight: Being overweight or obese increases your chances of having neuropathy. A balanced diet and consistent exercise are necessary to achieve and stay at a healthy weight.
- Eat a balanced diet. Choose a healthy diet high in fruits and vegetables, whole grains, and lean protein. Consume fewer saturated and harmful fats, processed meals, and added sweets. A healthy diet contains key nutrients that promote nerve health.
- Manage vitamin deficiencies: Vitamin B1, B12, and E deficits can all lead to nerve injury. Consult your doctor to check for deficiencies and consider taking supplements under their supervision.
- Practice appropriate foot care: Diabetics must check their feet daily. Check for cuts, blisters, and other injuries and treat them right away. Put on shoes that fit properly and offer sufficient support and cushioning.
- Exercise regularly: Regular physical exercise helps blood sugar regulation, circulation, and nerve function. Strive to get in at least 30 minutes of moderate-intensity activity most days of the week.
- Manage stress: Chronic stress can exacerbate pre-existing health issues, including diabetes and associated consequences, such as neuropathy. Practice stress-reduction strategies such as yoga, meditation, and deep breathing exercises.
Remember that early detection and treatment of diabetes are critical for avoiding neuropathy and related consequences. If you have any concerns regarding diabetic neuropathy, talk to your doctor. They can evaluate your risk factors, suggest suitable preventative actions, and monitor your status for early symptoms of nerve damage.
Summary
Diabetes-related neuropathy is nerve damage induced by high blood sugar. If you do not manage your diabetes properly, you are more prone to develop diabetes-related neuropathy. Smoking, heavy drinking, and high blood pressure are all risk factors.
If you have diabetes-related neuropathy, your doctor may prescribe pain relievers. You should also regulate your blood sugar with healthy eating and exercise. Many persons with nerve injury may experience depression or discouragement.
Consult your healthcare practitioner about your mental health. You may choose to start treatment or join a support group for persons who have diabetes-related nerve damage.
FAQs
What are the symptoms of diabetic neuropathy?
Numbness or a decreased capacity to sense pain or temperature fluctuations.
Tingling or burning sensation.
Sharp aches or cramps.
Muscular weakness.
Extreme sensitivity to touch for some people, even the weight of a bedsheet can be unpleasant.
Ulcers, infections, and bone and joint damage are all serious foot disorders.
How can you prevent diabetic neuropathy?
Maintain a weight appropriate for your height. Stop smoking. Reduce your blood pressure and lipid (fat) levels by making dietary and lifestyle adjustments, as well as taking medication as necessary. If you have symptoms like pain, numbness, or tingling in your hands or feet, see your doctor right away.
Is it possible to recover from diabetic neuropathy?
Although there is no cure for diabetic neuropathy, these therapies can help with unpleasant symptoms and avoid complications. Controlling blood sugar levels is an important part of treating diabetic neuropathy.
What are the early signs of diabetic feet?
A change in the color and warmth of your feet. The toenails are thickened and yellow. Fungus infections, such as athlete’s foot, occur between the toes. An ingrown toenail, blister, sore, ulcer, or infected corn.
What is the primary cause of neuropathy?
Nutritional or vitamin deficiencies, drunkenness, and exposure to pollutants can all harm nerves and create neuropathy. Vitamin B12 insufficiency and excess vitamin B6 are the most common vitamin-related causes. Several drugs have been shown to infrequently produce neuropathy.
Can you live a long life with diabetic neuropathy?
Although peripheral neuropathy is often fatal it can cause major problems if not treated. Neuropathy patients might expect to live a normal life with proper care. Addressing the underlying causes and treating symptoms via lifestyle modifications is critical for overall health.
Can neuropathy heal itself?
The peripheral nerves have a remarkable ability to repair. Recovery is possible, even if it takes many months. However, in certain cases, neuropathy symptoms may improve but not entirely resolve. Radiation-induced nerve damage frequently fails to heal.
What is the initial therapy for diabetic neuropathy?
Anticonvulsants such as pregabalin and gabapentin are favored as first-line treatments, followed by amitriptyline, duloxetine, and venlafaxine. Topical medicines like capsaicin and isosorbide dinitrate are also effective in treating DPN and may be used as a second or third-line therapy.
References
- Diabetic neuropathy – Symptoms & causes – Mayo Clinic. (2022, April 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/symptoms-causes/syc-20371580
- What is diabetic neuropathy? (2023, February 28). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/what-is-diabetic-neuropathy
- What is diabetic neuropathy? (2001, October 24). WebMD. https://www.webmd.com/diabetes/diabetes-neuropathy
- Brazier, Y. (2019, March 19). What to know about diabetic neuropathy. https://www.medicalnewstoday.com/articles/245310#takeaway
- Duggal, N. (2023, May 19). Diabetic neuropathy: Can it be reversed? Healthline. https://www.healthline.com/health/diabetes/can-diabetic-neuropathy-be-reversed#additional-causes
- Diabetic neuropathy. (2020, August 18). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/diabetic-neuropathy-nerve-problems
- Professional, C. C. M. (n.d.-f). Diabetes-Related neuropathy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21621-diabetic-neuropathy


4 Comments