Thenar muscle pain refers to discomfort or soreness in the muscles of the thenar eminence, the fleshy area at the base of the thumb. It can result from repetitive strain, overuse, poor ergonomics, or conditions like carpal tunnel syndrome.
Symptoms may include aching, weakness, or difficulty gripping objects. Proper rest, stretching, strengthening exercises, and ergonomic adjustments can help alleviate pain and prevent further strain.
What is a Thenar Muscle Pain?
Pain in the thenar prominence, a soft region near the base of the thumb, is referred to as “thenar muscle pain.” The thenar muscles are subject to strain, overuse, and nerve-related problems since they are essential for thumb movement and grip strength. Injuries, underlying medical disorders like arthritis, repeated activities, and nerve compression (as in carpal tunnel syndrome) can all cause this kind of pain. Maintaining hand function and avoiding increasing symptoms require accurate diagnosis and treatment.
The thumb’s mobility and grip strength are controlled by the thenar muscles, a trio of muscles at the thumb’s base. Several factors, such as overuse, strain, nerve compression, or underlying medical disorders, can produce the soreness, hurting, or pain that is commonly referred to as “thenar muscle pain.”
The soft, fleshy spot at the base of your thumb is known as your thenar eminence. Your thumb is opposable thanks to these four muscles. In other words, they enable your thumb to grasp and retain little items like a spoon, sewing needle, or pencil. You can also handle heavy bags, grasp and turn a doorknob, and text on your phone with an opposable thumb.
Many of your everyday activities are done using your thumb. These repetitive movements have the potential to overstress the muscles controlling your thumb over time, leading to pain and inflammation. To find out how to diagnose, treat, and prevent thenar eminence pain, continue reading.
What is the thenar muscle?
- Both hands have the thenar eminence, which is often called the “thumb pad.” The abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis are the three muscles that make up the thenar eminence.
- The thumb joint is stabilized by the tension in all three muscles; however, prolonged active tension in any one of these muscles can result in thenar eminence muscular pain.
Common Causes of Thenar Muscle Pain:
Overuse & Repetitive Motion: Prolonged holding of things, texting, or typing can all cause the thenar muscles to become strained.
- Carpal Tunnel Syndrome (CTS): Pain, weakness, and tingling in the thenar area can result from compression of the median nerve.
- Trauma or Injury: Excessive force, falls, or direct collision can all result in strained or damaged muscles.
- Arthritis: The thumb joint may be affected by osteoarthritis or rheumatoid arthritis, which can cause pain in the thenar region.
- De Quervain’s Tenosynovitis: Pain that radiates to the thenar muscles can be caused by inflammation of the tendons close to the thumb.
- Nerve Disorders: Pain and weakness may be caused by conditions that impact the nerves, such as peripheral neuropathy.
Symptoms of Thenar Muscle Pain:
- Aching, soreness, or a sharp ache at the base of the thumb are examples of pain and tenderness.
- Weak Grip Strength: The inability to hold or grip something securely.
- Swelling or Inflammation: The thenar area may appear swollen or sensitive.
- Pins-and-needles sensations, such as numbness or tingling, are frequently caused by nerve involvement (e.g., carpal tunnel syndrome).
- Thumb Movement Issues: Having trouble grasping, pinching, or using fine motor skills.
- Thumb mobility is restricted due to stiffness or limited range of motion, particularly after rest.
- pain that radiates past the thenar eminence to the hand or wrist.
- For an accurate diagnosis and course of therapy, it is advised to seek a medical assessment if these symptoms intensify or continue.
Diagnosis of Thenar Muscle Pain
A combination of a physical examination, medical history, and diagnostic tests are used to identify the underlying reason for thenar muscle pain.
Medical History & Symptom Assessment
- The length, severity, and type of the pain
- Any past medical issues, trauma, or repeated hand movements (e.g., arthritis, carpal tunnel syndrome)
- Related symptoms such as weakness, tingling, or numbness
Physical Examination
- Palpation: Examining the thenar area for soreness, edema, or muscular atrophy
- The Range of Motion (ROM) Test measures the stiffness and mobility of the thumb. The Grip & Pinch Strength Test evaluates the thumb and hand function.
- Examining for nerve compression, such as carpal tunnel syndrome, using Tinel’s Sign and Phalen’s Test
Diagnostic Tests
- Electromyography (EMG) and nerve conduction studies (NCS) are used to evaluate nerve function and identify disorders such as carpal tunnel syndrome.
- X-ray – Recognizes problems with bones, like arthritis or fractures
- Examine soft tissues, muscles, and tendons for signs of inflammation, rips, or nerve entrapment using ultrasound and magnetic resonance imaging.
- Blood tests are used to look for autoimmune or inflammatory diseases such as rheumatoid arthritis.
- A correct diagnosis aids in choosing the most effective course of treatment, guaranteeing efficient pain control and recuperation. It is imperative to seek medical attention if symptoms intensify or continue.
Treatment of thenar muscle pain:
It normally gets better if you can quit the activity that’s generating the pain and irritation. Because it is a work activity, this is frequently not feasible. You might not want to give it up if it’s because of a sport or pastime.
Even if the offending behavior is not entirely stopped, medical interventions and home remedies can be beneficial. Usually, the best results come from combining the two groups.
Medical Treatment:
Therar eminence pain is frequently treated with a thumb splint. Your thumb becomes immobile as a result, preventing misuse of the muscles. Your muscles will have more time to recover and the pain will be lessened.
If the splint affects your ability to do your job, you may not be able to wear it all the time, but you should wear it whenever you can.
Additional medical interventions consist of:
- Using kinesiology tape to immobilize your thumb and nonsteroidal anti-inflammatory medications like naproxen and ibuprofen
- injections of steroids
- Dry needling, acupressure, or acupuncture
- Apply cold therapy for more recent pain and warm therapy for more chronic pain. Ice the region for ten minutes, three to four times a day.
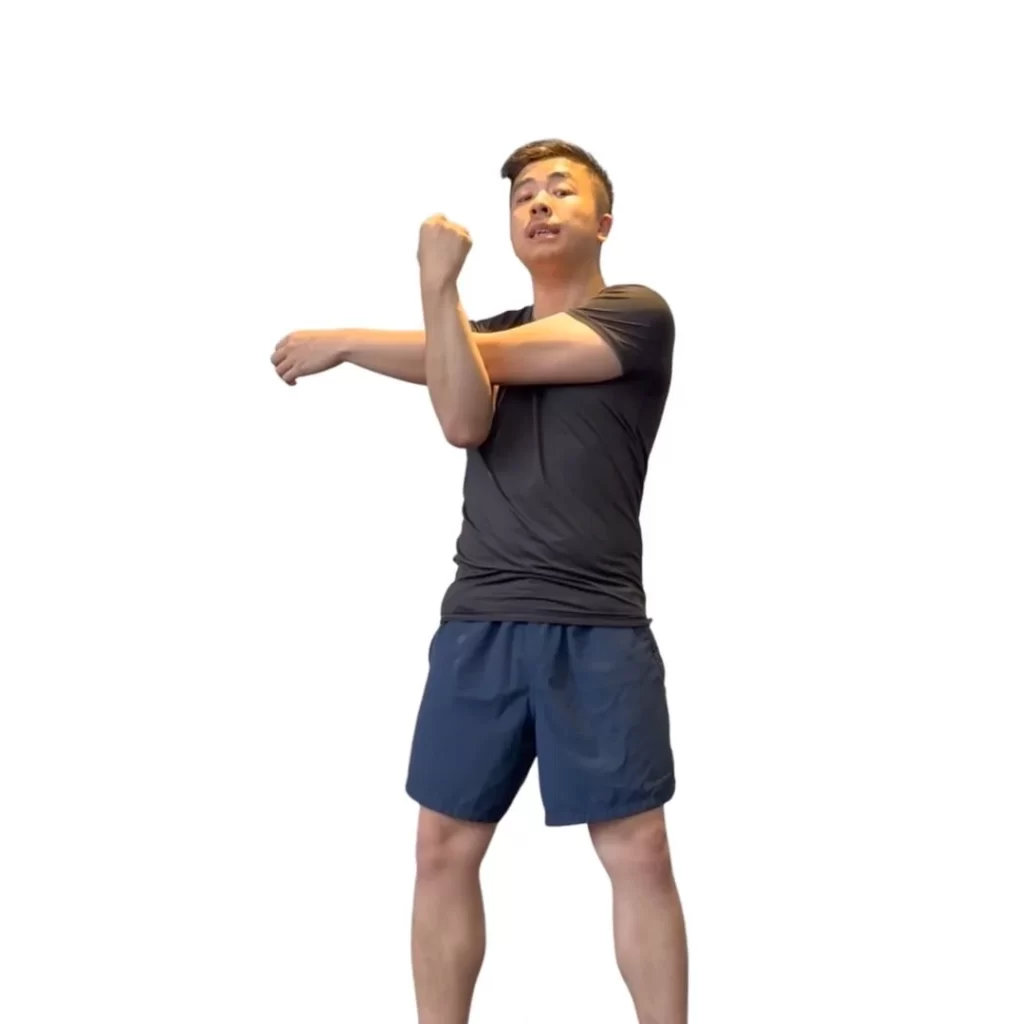
- Stretch your hands and thumbs and massage the area.
Home remedies for thenar muscle pain:
Rest
Avoid spending a lot of time on activities that cause your thenar eminence pain, such as sewing, weeding, or texting. To prevent these prolonged postures that are aggravating your pain, take rests in between tasks. For chores like texting, you might try switching hands.
Heat therapy
Put some heat on your thenar eminence. You can also soak your hands in a warm water bath or wash them in warm water. The heat promotes blood circulation in the area and relaxes your muscles, facilitating recovery. To prevent irritating the skin or giving this area superficial burns, use caution while applying excessive heat. Applying heat for 10 to 15 minutes at a time is often advised.
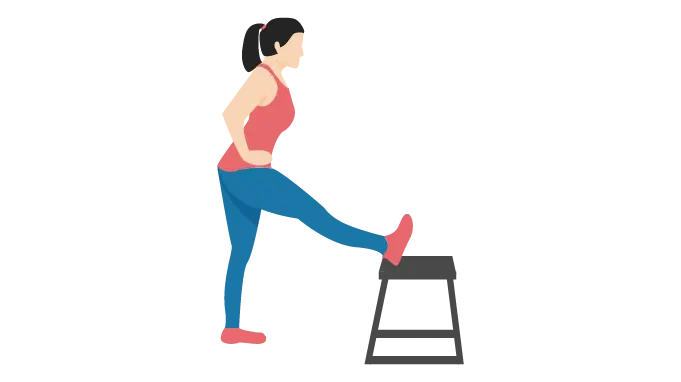
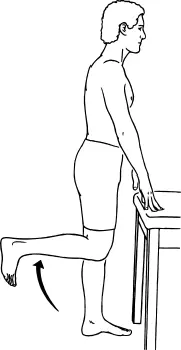
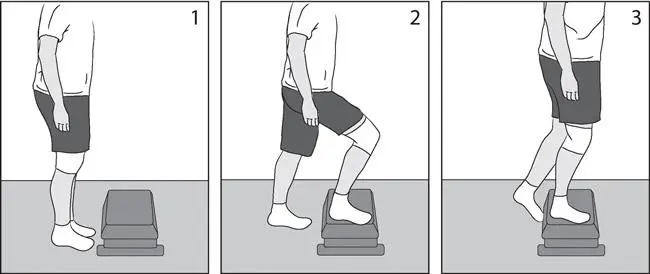
Stretches
Press your palms down and spread your thumb and index finger as widely apart as you can against a level surface. A diamond (or L and reverse L) should form between your two hands as a result of this stretch. You may also perform this stretch at the bottom of a warm water sink. The muscles will further relax if you use warm water.
With your palm facing up, use your other hand to grasp your thumb and gradually drag it to the ground. After 30 seconds, switch to the other hand and hold this stretch.
How to prevent thenar muscle pain:
- Avoiding repetitive thumb movement activities is the greatest approach to prevent thenar eminence pain from developing or returning.
- Sometimes you are unable to cease these actions because they are essential for your job or because you wish to carry on with the activity that is causing them. In this situation, you should relax the muscles that control your thumb by taking frequent rests.
- There are other ways to complete the task that don’t need to use your thumb excessively.
- Another way to keep your hand and thumb muscles from being stiff is to stretch them. The following stretches are beneficial for your thenar eminence:
- Spread your other fingers apart and gently slide your thumb back toward your forearm.
Keeping your thumb and index finger as far apart as possible, press your palm down against a level surface.
With your palm facing up, place your hand on a level surface. Then, use your elbow to gently lean into your thenar eminence and move it around the area.
FAQs
What’s causing my thenar pain?
Overuse syndrome, which is caused by repetitive thumb movements, is typically the cause of thenar eminence pain. Usually, a mix of home remedies and medical therapies helps it get well. Avoiding activities that involve repetitive thumb movements can help prevent thenar eminence soreness.
What makes my thenar muscle so large?
Pseudohypertrophy or genuine hypertrophy associated with spontaneous activity, increased effort of remaining fibers, and fiber stretching 2, 3 can cause thenar hypertrophy. The probability of real thenar hypertrophy is increased by spontaneous activity on needle EMG and chronic denervation.
Why do thenar muscles deteriorate?
The median nerve innervates the thenar muscles, which might exhibit atrophy in Carpel Tunnel Syndrome (CTS), if median nerve impairment occurs. Other CTS tests, such as the Tinel’s test and the Phalen’s sign, should be performed if indicated.
How is the thenar stretched?
The muscles will relax even more if you use warm water. Hold onto your thumb with your other hand and gradually pull it to the floor, palm facing up. After 30 seconds of holding this stretch, switch to the other hand.
For thenar pain, what is the differential diagnosis?
In conclusion, for baseball players who need manual power to hold a baseball and grip a bat, thenar pain can be a major functional constraint. When a baseball player experiences thenar pain, osteocartilaginous, ligamentous, vascular, and musculotendinous reasons are among the potential diagnoses.
What is the function of the thenar muscles?
The thumb’s intrinsic muscles are composed of the four thenar muscles. These consist of the flexor pollicis brevis, opponens pollicis, adductor pollicis, and abductor pollicis. These intrinsic muscles work together to provide thumb mobility.
How is the thenar muscle massaged?
Work your way outward from the palm’s center, beginning with the palmar fascia and moving layer by layer deeper until you reach the thenar eminence.
How can the thenar muscle be stretched?
Wrap your hand with a rubber band so that it rests at the base of your finger joints. Move your thumb as far away from your other fingers as you can with gentleness. After 30 to 60 seconds of holding this position, let go. With each hand, repeat ten to fifteen times.
What is causing the thenar muscle pain?
Overuse syndrome, which is caused by repetitive thumb movements, is typically the cause of thenar eminence pain. Usually, a mix of home remedies and medical therapies helps it get well. Avoiding activities that involve repetitive thumb movements can help prevent thenar eminence soreness.
References
- The Healthline Editorial Team. (2024, January 27). How to Diagnose, treat, and prevent thenar Eminence Pain. Healthline. https://www.healthline.com/health/thenar-eminence-pain
- Posts, V. M. (2020, November 18). 4 Tips for thenar muscle pain relief. Urban Health HQ. https://urbanhealthhq.com.au/2020/11/18/4-tips-for-thenar-muscle-pain-relief/
- Seladi-Schulman, J., PhD. (2019, May 28). Thenar Eminence overview. Healthline. https://www.healthline.com/health/thenar-eminence#nerves