What is Plica Syndrome?
Plica syndrome is a disorder that causes pain and discomfort by irritating or inflaming the plica, a fold of tissue in the knee joint. Usually caused by overuse or repetitive motions, it can cause symptoms like swelling, clicking, and knee pain.
Rest, physical therapy, anti-inflammatory medications, and in certain situations, surgery, may all be part of the treatment. For a precise diagnosis and suitable therapy, it’s critical to speak with a healthcare provider if you’re exhibiting symptoms.
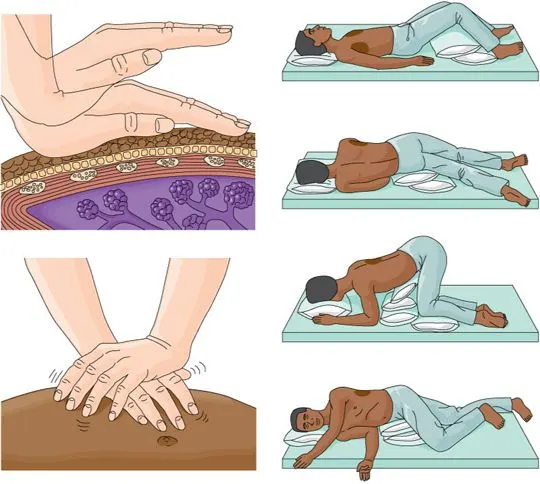
Clinically Relevant Anatomy of Plica Syndrome:
Types of Plica
The plicae in the knee joint can vary in size and structure; they can be longitudinal or crescent-shaped, fibrous or fatty, and depending on their anatomical location within the knee joint cavities, they can be classified as suprapatellar, mediopatellar, infrapatellar, or lateral plicae. The latter is rarely observed, so there is some debate about its existence or precise nature.
Suprapatellar plica
The plica synovialis suprapatellaris, superior plica, supramedial plica, medial suprapatellar plica, or septum are other names for the suprapatellar plica, which is a domed, crescent-shaped septum that typically sits between the knee’s tibiofemoral joint and suprapatellar bursa. It inserts above the patella after running downward from the synovium at the anterior side of the femoral metaphysis to the posterior side of the quadriceps tendon.
Under normal circumstances, its free border appears thin, wavy, crenated, or pointed. This kind of plica can surround an aperture known as a porta as a peripheral membrane or an arching membrane. It frequently becomes part of the medial plica. When the knee is moved, the suprapatellar plica, which is anteriorly connected to the quadriceps tendon, changes size and orientation.
Medial patella plica
The plica synovialis mediopatellaris, medial synovial shelf, plica alaris elongata, medial parapatellar plica, meniscus of the patella, and, after its first two descriptors, Iion’s band or Aoki’s ledge are other names for the medial patellar plica. It is located along the joint’s medial wall. It enters the synovium around the infrapatellar fat pad after attaching to the lower patella and lower femur and passing through the suprapatellar plica.
The look of its free border can vary.The medial plica also changes size and orientation during knee movement since it is connected to the ligamentum patellae and the synovium that covers the fat pad. Because of its anatomical placement, the medial plica is recognized to be the most frequently injured plica, and it is typically this plica that is implicated when describing plica syndrome.
Infrapatellar plica
Ligamentum mucosum, plica synovialis infrapatellaris, inferior plica, and anterior plica are other names for the infrapatellar plica. Starting from a narrow base in the intercondylar notch, this synovial fold extends distally in front of the anterior cruciate ligament (ACL) and inserts into the inferior of the infrapatellar fat pad.
Distinguishing the ACL from the infrapatellar plica is frequently challenging. It typically manifests as a thin, fibrous band that resembles a cord. The most prevalent plica in the human knee is thought to be the infrapatellar plica. Discussion is on-going whether this plica is structurally crucial to proper knee movement or whether it is superfluous.
Lateral plica
Other names for the lateral plica include lateral para-patellar plica and plica synovialis lateralis. It is 1-2 cm lateral to the patella, longitudinal, and thin. It extends inferiorly and inserts into the synovium of the infrapatellar fat pad, forming as a synovial fold along the lateral wall above the popliteus hiatus. Some authors question whether it originates from the parapatellar adipose synovial border or if it is a genuine septal remnant from the embryological period of development. This kind of plica is extremely uncommon, with an incidence far below 1%.
Epidemiology of Plica Syndrome:
The majority of synovial plicae are asymptomatic and have minimal clinical significance. However, when they are hurt or agitated, they may start to exhibit symptoms. Numerous conditions, including direct trauma or blow to the plica, blunt trauma, twisting injuries, repetitive knee flexion and extension, increased activity, intra-articular bleeding, osteochondritis dissecans, torn meniscus, chronic or temporary synovitis, and more, can cause this.
Patients may experience no symptoms for a while after the initial injury has healed, but weeks or months later, they may suddenly develop anterior knee discomfort. Pilia syndrome is the term used to describe an internal disturbance of the knee that impairs normal knee joint function and is caused by inflammation or damage to the medial patellar, lateral plica, suprapatellar, or a combination of the three. Because of its anatomical placement, the medial plica is thought to be the most often injured plica.
The appearance of plica syndrome typically does not imply the presence of the infrapatellar plica. Because the plica syndrome is frequently caused by overuse of the knee, it is more common in people who perform exercises that require repeated flexion-extension motions.
Both the reported incidence of plica syndrome and synovial plicae exhibit significant variance. The primary causes of these discrepancies include variations in nomenclature and assessment methods, as well as interpretations by the individual researchers.
Pathophysiology:
Normal knee joint components called plicae unite during pregnancy. Although autopsy studies show that plicae are present in 50% of persons, plicae usually involute when the fetus is around 12 weeks old.
There are four types of normal plicae for the roughly 50% of persons who have one. They are medial, lateral, suprapatellar, and infrapatellar. Having several plicas is not unusual in patients.
The knee joint and the suprapatellar bursa are separated by the suprapatellar plica. The synovium surrounding the infrapatellar fat pad and the intercondylar notch are separated by the infrapatellar plica. The medial facet of the knee joint and the infrapatellar fat pad are separated by the medial plica. The most prevalent kind of plicae and the most likely to exhibit symptoms are medial plicae. The rarest plica is the lateral plica. It is situated between the lateral patellar facet and the infrapatellar region.
It is crucial to remember that not every plicae is painful. When normal plicae experience inflammation, they may become painful. When this inflammation causes impingement between the patella and femur, it might result in a tight, fibrotic plica that can cause symptoms during knee flexion.
Causes of Plica Syndrome:
The plica is a tissue remnant that arises during fetal development, and irritation or inflammation of the plica is usually the cause of plica syndrome. Although the precise origin of this irritation can vary, overuse, repetitive knee movements, or direct trauma to the knee are frequently linked to it.
The risk of developing plica syndrome may be increased by activities that require a lot of bending, crouching, or kneeling. A history of prior knee injuries or structural problems with the knee joint may also be contributing factors.
- Repetitive Motions: The plica may become irritated and inflamed as a result of frequent motions that require bending, straightening, or rotating the knee joint.
- Trauma: The plica may become irritated as a result of direct impact or trauma to the knee, causing inflammation.
- Overuse: Plica syndrome can develop as a result of activities that place an excessive amount of tension on the knee joint, particularly when there is inadequate rest or recuperation.
- Muscle Imbalances: Weak or unbalanced knee muscles can impact the stability and mechanics of the joint, which may cause plica discomfort.
- Infection or Inflammation: Scar tissue formation and plica irritation can occasionally result from infections or inflammatory disorders affecting the knee joint.
Symptoms of Plica Syndrome:
- Activity-Related Pain: Activities that require knee bending, such running, walking, or climbing stairs, may make the pain worse.
- Localized Tenderness: The inside side of the knee joint or the region surrounding the plica may feel tender to the touch.
- Knee Stiffness: After extended periods of inactivity or rest, people with plica syndrome may have stiffness in their knee joint.
- Sensation of Locking: When the inflamed plica becomes lodged in the joint, some persons may experience the sensation that their knee “locks” or becomes momentarily trapped in a particular position.
- Sensation of Giving Way: During motions that cause the plica to catch or fold, the knee may feel unstable or as though it will give way.
- Swelling: Localized swelling surrounding the knee joint may result from plica inflammation.
- Pain Along the Joint Line: Because the plica tissue is found along the inner side of the knee, pain may be felt there.
- Limited Range of Motion: Because of the discomfort caused by the inflamed plica, some people may find it difficult to fully bend or straighten their knees.
Risk Factors of Plica Syndrome:
- Anatomical Factors: Some people may have a larger or more noticeable plica by nature, which makes discomfort more likely.
- Improper Biomechanics: The knee joint and the plica may be subjected to additional stress due to poor alignment or mechanics during movement.
- Age: Adolescents and young adults are susceptible to plica syndrome.
- Employment: Jobs requiring a lot of kneeling or repetitive knee motions may increase the risk.
- Repetitive Motions: Activities that require kneeling, crouching, or bending repeatedly might aggravate the plica and raise the risk.
- Overuse: Running, jumping, and other activities that put undue strain on the knee joint can aggravate the plica.
- Knee Injuries: A history of trauma, surgery, or knee injuries may cause structural alterations in the knee joint, increasing its vulnerability to plica irritation.
- Muscle Imbalances: Pplica syndrome can be exacerbated by imbalances in the muscles surrounding the knee, which can change joint mechanics.
Diagnosis of Plica Syndrome:
A physical examination, medical history, and occasionally imaging tests are used to diagnose plica syndrome:
- Medical History: You will be asked to describe your symptoms, their onset, and any activities that may have caused them. Additionally, they will ask about any prior knee operations or injuries.
- Physical Examination: The physician will check your knee for any strange sensations, such as clicking or catching, as well as any indications of swelling or soreness. To determine your knee joint’s range of motion and to pinpoint any particular painful spots, they might move it.
- Imaging Research: Imaging procedures such as MRI scans or X-rays can be performed to better evaluate the interior components of the knee and rule out other disorders, though they are not always required. By illustrating any inflammatory or anatomical problems with the plica, they can aid in diagnosis confirmation.
- Diagnostic Injections: In certain situations, administering a local anesthetic injection to the vicinity of the plica can assist ascertain whether the symptoms go better, which can confirm the diagnosis.
Physical Examination:
Getting a relevant history from the patient is one of the most crucial steps in detecting medial synovial plica disease.
The proximo-medial part of the knee and the patella’s border are frequently reported as having a dull discomfort. An internal hydrops and a perceptible string are common. Activity and overuse exacerbate the pain, which is especially painful at night. Because stair climbing, squats, and standing up from a chair put stress on the patello-femoral joint, the majority of patients complain about these activities.
After sitting for extended periods of time, the patient may also complain of pain. Approximately half of the patients inform us that they have been performing repetitive flexion and extension exercises. Although they are less common, injuries or excessive use of the other plica might result in the same problems.
The plica and mediopatellar plica stutter tests are unique physical examinations used to diagnose a medial plica. However, when the joint is inflamed, the plica stutter test will not function. The medial subluxation test, McMurray’s, Appley’s test for instability, and Cabot’s test are further testing techniques that could reveal the existence of a medial plica.
The patient is placed in a supine position with their knee extended during the MPP test. Next, using the thumb, manual force is given to the inferomedial portion of the patellofemoral joint to check for discomfort. The test is deemed successful if, upon applying the same manual force, this discomfort obviously decreases at 90° of flexion. This test has a diagnostic accuracy of 89.0% and a sensitivity and specificity of 89.5% and 88.7%, respectively, in comparison to arthroscopy.
The knee extension or flexion test are further provocation tests that can be used to detect medial plica syndrome. The active extension test involves rapidly extending the tibia in a manner similar to kicking. Because the quadriceps femoris muscle causes an abrupt stress on the plica, the test is deemed positive when it is uncomfortable. The tibia is swiftly swung from full extension into flexion and then stopped between 30 and 60 degrees of flexion to conduct the flexion test. When the plica is extended with an eccentric contraction of the quadriceps muscle, the test is once more positive.
To determine whether the medial plica is irritated, use the plica snap test. The patient rests supine on the examination table with both legs relaxed in order to palpate the medial synovial plica. The examiner rolls their fingers along the plica fold, which is between the adductor tubercle region of the medial femoral condyle and the medial border of the patella, to palpate the medial synovial plica.
The ligament will appear as a ribbon-like fold of tissue beneath the finger, which rolls directly against the medial femoral condyle underneath. When the test replicates the symptoms, like a slight pain, it is considered successful. Additionally, compare it to a normal knee to see if the level of pain is different. Because the synovium and medial joint are extensively innervated, it has been shown that it can cause significant discomfort in certain patients.
Clicking or popping sensations on the anterior part of the knee are common in patients with plica syndrome. One of the main symptoms of plica syndrome is anterior knee discomfort. Stairs, squatting, getting out of a chair, and other actions that put strain on the patellofemoral joint might cause pain. There may be no history of trauma or injury, or there may be a history of blunt trauma or a twisting injury. When getting a history, one should take into account secondary causes of plica. These include rheumatoid arthritis, intra-articular lesions, loose foreign bodies, and hemophilia-related hemarthrosis.
A taut band that is painful to the touch may be felt beneath the skin during a physical examination. If so, it is necessary to evaluate the contralateral knee to determine whether a plica is generating discomfort when palpated there as well. Tight quadriceps, hamstrings, and an effusion are possible additional physical examination findings.
There are two physical examination methods that can indicate plica syndrome. These assessments are the Hughston and Stutter tests. The diagnosis of plica syndrome should be suspected when both tests come back positive. Although it is less suspicious, plica syndrome should still be taken into consideration if only one of the two tests is positive. In order to administer the Stutter test, the patient must sit up straight and have their legs hang at a 90-degree angle off the edge of the examination table. The examiner touches the center of the affected leg’s patella with his or her index and middle fingers. The inspector then feels for a patella stutter as the patient extends the affected leg. A positive test result involves experiencing a stutter.
The patient extends their knee while lying supine in the Hughston test. With one hand wrapped around the plantar aspect of the patient’s heel and the other palm covering the patient’s patella, the examiner stands on the side of the injured knee. After that, the examiner takes the patient’s knee through flexion and extension while pushing the patella medially and inwardly rotating the tibia. When the patient feels discomfort or the practitioner notices popping during range of motion, the Hughston’s test is considered affirmative.
Evaluation:
Though they are frequently normal even if plica syndrome is the diagnosis, anteroposterior (AP), lateral, and skyline radiographs should be taken when plica syndrome is suspected.
There is debate on the usefulness of magnetic resonance imaging (MRI) in the diagnosis of plica syndrome. On MRI, plicae are only sometimes visible. When there is an effusion, plica is easier to see on MRI. If plicae are seen, their signal intensity will be minimal. On MRI, symptomatic plicae can occasionally be distinguished from normal plicae due to their thick appearance and potential for synovitis. Normal plicae, on the other hand, could seem slender. Therefore, MRI is crucial for assessing additional possible reasons of knee pain and can be helpful in pre-operative planning.
Several studies that examined 492 knees and contrasted the sensitivity and specificity of physical examination with ultrasonography and MRI were found in a review of the literature. These findings showed that the MRI had 77% sensitivity and 58% specificity, the physical examination had 90% sensitivity and 89% specificity, and the ultrasound had 90% sensitivity and 83% specificity.
Differential Diagnosis of Plica Syndrome:
- Patellar femoral syndrome
- Patella bipartite
- Patellar maltracking
- Degenerative joint disease
- Hoffa syndrome
- Sinding-Larsen-Johansson disease
- Medial collateral ligament sprain
- Osteochondritis dissecans
- Pes anserinus bursitis
- Meniscal tears
Treatment of Plica Syndrome:
Medical Treatment of Plica Syndrome:
- Anti-Inflammatory Drugs: NSAIDs, or non-steroidal anti-inflammatory drugs, are medications that help reduce inflammation and pain. These, however, ought to be used under a doctor’s supervision.
- Ice and Elevation: You can relieve and lessen swelling in your leg by applying ice and raising it.
- Corticosteroid Injections: To lessen inflammation and discomfort, a corticosteroid injection into the knee joint may occasionally be advised.
- Pain management: To control discomfort, over-the-counter painkillers may be suggested.
- Rest and Activity Modification: You can lessen plica discomfort and inflammation by allowing your knee to rest and avoiding activities that exacerbate symptoms.
Physical Therapy Treatment of Plica Syndrome:
- By reducing discomfort, increasing joint mobility, and fortifying the muscles surrounding the knee, physical therapy is essential in the treatment of plica syndrome. The following is one possible technique to plica syndrome physical therapy treatment:
- Evaluation: A physical therapist will evaluate the strength, range of motion, and general function of your knee. In order to customize the treatment plan to meet your unique needs, they will also go over your medical history and symptoms.
- Hand Therapy: To increase joint mobility and lessen muscular tension, manual methods like soft tissue massage and joint mobilizations may be employed.
- Stretching: Mild stretching techniques can ease tension in the knee muscles and increase flexibility.
- Exercises for Strengthening: It’s critical to strengthen the muscles that support the knee joint. To improve knee alignment and stability, exercises may focus on the calf, hip, hamstring, and quadriceps muscles.
- Functional Training: To increase functional strength and stability, physical therapists frequently work on exercises that replicate your everyday motions.
- Biomechanical Corrections: By identifying and addressing any incorrect movement patterns that lead to plica irritation, the therapist can help you move more effectively and lessen the strain on your knee joint.
- Electrotherapy: To lessen pain and encourage healing, techniques like electrical stimulation or ultrasound may be employed.
- Home Exercise Program: To assist you maintain the improvement you make in sessions, your physical therapist will probably give you a series of exercises to perform at home.
- Education: You will be given instructions on how to move correctly, maintain good posture, and use self-management techniques for your symptoms.
- Progress Monitoring: To guarantee the best outcomes, your physical therapist will monitor your development over time and modify the treatment plan as necessary.
- Bracing: During activities, using a knee brace or support can assist stabilize the joint and offer relief.
- Activity Modification: Adjusting your activity to eliminate movements that increase symptoms can aid in recuperation.
Exercise of Plica Syndrome:
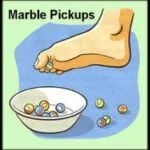
Indeed, a physical therapist may suggest the following exercises to assist control and lessen plica syndrome symptoms:
Quad Sets: The patient should sit on the floor with their legs straight. Press the back of your leg onto the floor while contracting your quadriceps, the muscles in your thighs. After a few seconds of holding, release the position. Repeat a number of times.
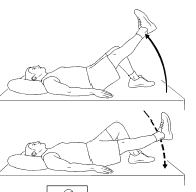
Straight Leg Raises: Place one leg bent and one leg straight on the patient’s back. Raise the straight leg a couple of inches off the floor, then hold it there for a few seconds before lowering it again. The quadriceps are strengthened by this exercise.
Hamstring Stretches: Stretching the hamstrings involves lying on the patient’s back and gently drawing one knee up to the patient’s chest. Maintaining the opposing leg flat, straighten the leg as much as you can. This should cause the back of your thigh to gently stretch.
Calf Stretches: For calf stretches, place the patient’s hands on the wall as they stand facing it. Keep one leg straight and take a step back. Feel the calf muscle stretch as you bend the front knee while maintaining the rear heel on the floor.
Inner Thigh Stretch: Place the soles of your feet together while sitting on the floor to perform an inner thigh stretch. To feel a stretch in your inner thighs, gently press your knees toward the floor.
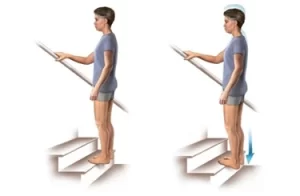
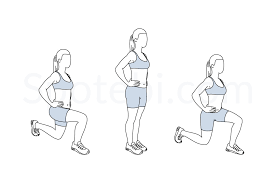
Step-Ups: Take a stance facing a low platform or a step. One-leg step up, followed by a step down. Before moving on to the second leg, perform a series of repetitions on the same leg.
Mini Squats: Place your feet hip-width apart to perform little squats. Straighten your knees after bending them slightly, as you’re reclining in a chair. The muscles surrounding the knee are strengthened by performing this little squat exercise.

Lateral Leg Raises: For balance, stand close to a wall or other support. Keeping one leg straight, raise it out to the side and then bring it back down. The hip abductor muscles are the focus of this leg lift exercise.
Bridges: Place your feet flat on the floor and bend your knees while lying on the patient’s back. Lift your hips off the floor with a gluteal squeeze, then bring them back down.
Wall Slides: Slide down into a squatting stance while leaning your back on a wall. Maintain your knees in line with your feet and the patient’s back against the wall. Before sliding back up, hold the position for ten to fifteen seconds.
Clamshells: Place your feet together and bend your knees while lying on the patient’s side. Raise your upper knee as high as the patient can without shifting your pelvis, while keeping their feet in contact. Put it back down. The hip abductor muscles are the focus of this clamshell exercise.

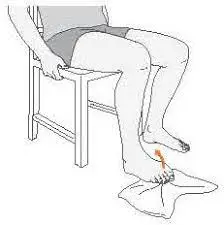
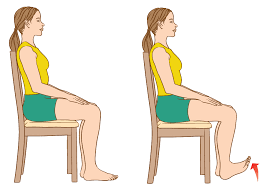
Seated Knee Extension: Bend your knees 90 degrees while seated in a chair. Straighten the patient’s knee and slowly extend one leg in front of them. Hold for a few seconds, then drop the leg back down.
Heel Slides: Keep your legs straight while lying on the patient’s back. Bend your knee and slide one heel up toward your buttocks, then back down. Knee mobility is improved by doing this exercise.
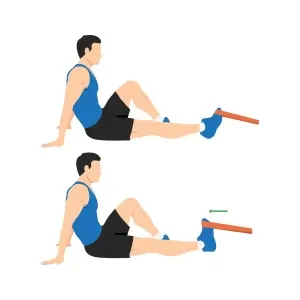
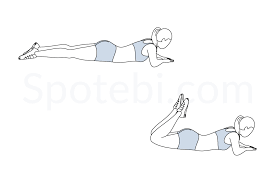
Hamstring curls: While lying on your stomach, fasten a resistance band around your ankle if you have one. To resist the pull of the band, bend your knee so that your heel is closer to your buttocks. Return your leg to its natural position slowly.
IT Band Stretch: Reach your arm over your head to the other side while crossing one leg in front of the other. Feel a stretch down the outside of your leg as you tilt your upper body sideways.
Calf Standing Raises: Place your feet flat on the floor and stand. Lift your heels off the ground and stand up onto the patient’s toes. Return the patient’s heels to the ground.
Isometric Quad Contractions: Bend your knees at a 90-degree angle while sitting on the edge of a chair. Using your quadriceps, press your knee against the chair. After ten to fifteen seconds of holding the contraction, release it.
Step-Ups with Knee Lift: This variation on the standard step-up involves raising the opposing knee toward your chest after stepping onto the platform and then stepping down.
Resistance Band Leg Abduction: Stand with your feet hip-width apart and wrap a resistance band around your ankles. Lift one leg out to the side against the band’s resistance while maintaining a straight posture.
Exercises with a Foam Roller: To assist relieve tension and increase blood flow, gently move a foam roller around the outside of your calf and thigh muscles.
Ankle Pumps: While lying on your back, slowly pump your ankles up and down. This lessens stiffness and increases circulation.

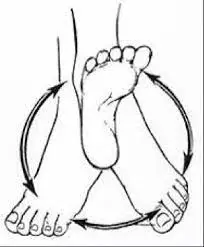
Quadruped Hip Circles: Get on your hands and knees and perform quadruped hip circles. Draw circles with the knee of the affected leg while keeping your back flat and your core stable.
Prone Hangs: Place your legs hanging off the edge of a table or bed while lying on your stomach. The front of the thigh can be gradually stretched in this way. Stretch your hip flexors by placing one foot in front of the other while kneeling on one knee. Lean forward to feel a stretch close to the front of the kneeling leg’s hip.
Seated Wall Slides: Bend your knees normally while sitting against a wall. Straighten your knees and slowly slide your feet away from the wall. Next, return your feet to a bent posture by sliding them up.
Quad Foam Rolling: Place a foam roller beneath your thighs while lying on your stomach. To massage the front of your thighs, gently roll from side to side.
Hip Hikes: Raise the opposing hip higher while standing on one leg. Repeat after lowering it back down. The hip muscles are strengthened by this hip hike workout.

Dynamic Hamstring Stretch: Reach for your toes with one leg out in front of you as you’re standing. Next, stretch your hamstrings by swinging the leg behind you while bending at the waist.
Seated Leg Extension with Resistance Band: Place a resistance band around your ankle while sitting on the edge of a chair. Despite the band’s resistance, extend your leg in front of you.
Single-Leg Balance: Try to keep the patient balanced while standing on one leg. This strengthens the muscles surrounding the knee and enhances stability.
Stationary Bike: Low-impact exercise on a stationary bike can help increase knee mobility and circulation.
Leg lifts while side-lying: Keep your legs straight while lying on the patient’s side. Raise your upper leg a couple of inches above the floor, then bring it back down. The hip abductor muscles are the focus of this side-lying leg lift exercise.
Wall Sit: Slide into a sitting position with your knees bent at a 90-degree angle while leaning against a wall. Before getting back up, hold the position for a predetermined period of time.

Active Knee Extension: Hang your legs down while sitting on the edge of a table or other elevated surface. Your knees should be gently extended and straightened before being lowered again.
Isometric Hip Adduction: Sit with a pillow or small ball between your knees. For a few seconds, squeeze your knees together, then let go.
Toe Taps: Place your feet on the floor while seated in a chair. One foot at a time, alternate tapping your toes on the ground in front of you.
Seated Heel Raises: Lifting your heels off the floor while maintaining the balls of your feet on the floor is known as a “seated heel raise.” Bring your heels back down.
Resistance Band Side-Lying Hip Abduction: Place a resistance band around your ankles while lying on your side. Raise the patient’s upper leg against the band’s resistance.
Resistance Band-Assisted Resisted Knee Flexion: Place a resistance band around your ankle while seated in a chair. To raise your foot off the ground against the band’s resistance, bend your knee.
Water Exercises: Low-impact mobility and joint support can be obtained by water exercises such as leg swings, water walking, and mild kicking if you have access to a pool.
Surgical Treatment of Plica Syndrome:
When conservative measures such as rest, physical therapy, and medication have failed to adequately alleviate symptoms and the condition substantially hinders your everyday activities and quality of life, surgery is usually considered for plica syndrome. This procedure, called a “plica resection” or “plica excision,” involves removing the irritated or inflamed plica tissue from the knee joint. Here are some things you should know about plica syndrome surgery:
Plica resection: Plica excision is a surgical operation performed to treat plica condition. It involves the removal or trimming of the irritated or inflammatory plica, which is a fold of synovial tissue in the knee joint. The procedure is frequently carried out arthroscopically, which is a minimally invasive method that involves tiny incisions and an arthroscope, a tiny camera that guides the surgeon’s tools. To ease discomfort and lower inflammation, the surgeon locates the troublesome plica and then carefully removes or trims it during the procedure. This can lessen the pain caused by the irritated plica and help knee function.
- Indications: When non-surgical treatments have failed, surgery is typically regarded as a last option. Based on your response to conservative treatments and the severity of your symptoms, your healthcare provider will evaluate your case and decide whether surgery is necessary.
- Procedure: To remove the irritated plica tissue, the surgeon will carefully make a small incision close to the knee’s affected area. Usually, minimally invasive techniques are used to perform this operation.
- Success Rates: Plica syndrome surgery generally has a good success rate in relieving symptoms; however, like any type of surgery, there are potential risks and complications that the patient’s healthcare provider will discuss with you beforehand.
- Recovery: Recovery time varies, but it usually involves a period of rest and rehabilitation. Physical therapy is commonly recommended post-surgery to help regain strength, flexibility, and mobility in the knee.
- Patient preparation: Prior to the procedure, the patient’s healthcare provider will give you instructions on how to prepare, which may include fasting and making plans for transportation and post-operative care.
- Post-Surgery Care: You must adhere to your surgeon’s instructions regarding physical therapy, pain management, and wound care after surgery. To prevent placing too much weight on the limb that was operated on, you might be told to wear crutches for a while.
- Consultation: It’s crucial to have a thorough consultation with an expert who can explain the procedure, any dangers, anticipated results, and the recovery period if surgery is being considered.
Home Advice of Plica Syndrome:
Indeed, the following self-care and home remedies can help you manage the symptoms of plica syndrome and aid in your recuperation:
- Rest: Give your knee enough rest, especially if your symptoms are getting worse. keep away of activities that make your pain worse.
- Ice: Applying ice to the affected area for 15 to 20 minutes several times a day can help reduce inflammation and provide pain relief.
- Elevation: To help minimize swelling and promote blood circulation, elevate your leg while you’re at rest.
- Over-the-counter Pain Relief: If your doctor has given the go-ahead, you may use over-the-counter pain relievers (like ibuprofen or acetaminophen) to manage pain and inflammation.
- Compression: Using a knee compression sleeve or bandage can help support the joint and reduce swelling.
- Stretching: To avoid stiffness, perform mild range-of-motion exercises. keep away of motions that hurt or make you uncomfortable.
- Low-Impact Activities: If your doctor has given the all-clear, participate in sports like cycling or swimming that are less taxing on the knee joint.
- Shoes: To lessen the impact on your knees, choose shoes with adequate cushioning and arch support.
- Appropriate Footwear: keep away of shoes with low support and high heels as these might exacerbate knee alignment issues.
- Eat a nutritious, well-balanced diet to promote the general health of your joints.
- Hydration: To keep your body properly hydrated and to support joint function, drink a lot of water.
- Weight management: To lessen undue strain on the knee joint, keep your weight within a healthy range if needed.
- Being aware of your posture will help you distribute your weight evenly and avoid putting undue strain on your knees.
- Supportive Seating: When sitting for long periods of time, place a cushion or other support beneath your knees.
- Orthopedic Supports: To support your knee as you sleep, think about using orthopedic pillows or cushions.
- Pain Diary: To find trends and triggers that either aggravate or lessen your symptoms, keep a journal of your activities and symptoms.
- Stress Reduction: Using relaxation methods like meditation and deep breathing can help you deal with stress and pain.
- Gradual Return to Activity: As your symptoms subside, progressively resume your routines, exercises, and motions while monitoring your knee’s reaction.
Complication of Plica Syndrome:
Even though plica syndrome is generally thought to be a benign condition, if the symptoms are not adequately managed or if the condition is left untreated, complications may occur. Some possible complications of plica syndrome include:
- Chronic Pain and Discomfort: If plica syndrome is not treated, it may result in chronic pain and discomfort that affects everyday activities and quality of life.
- Knee Instability: Knee joint irritation of the plica may cause feelings of instability or “giving way,” which may raise the risk of falls or injuries.
- Secondary Issues: Pain-induced compensatory movements may cause muscle imbalances and changed movement patterns, which may eventually lead to other musculoskeletal problems. Inflammation: Prolonged irritation of the plica tissue may cause persistent inflammation in the knee joint.
- Decreased Range of Motion: If left untreated, plica syndrome may result in restricted knee joint mobility and trouble bending or completely extending the knee.
- Functional Limitations: People may find it difficult to engage in sports, physical activities, or even daily duties when their symptoms develop.
- Development of Scar Tissue: Prolonged irritation and inflammation can cause scar tissue to grow around the plica, which can worsen symptoms and impair joint function.
Prevention of Plica Syndrome:
While plica syndrome can often be tough to prevent fully, there are things you can take to lower your risk of getting the condition or experiencing recurrent episodes:
- It’s crucial to fully warm up before engaging in any kind of exercise. Your muscles and joints can be better prepared for the exercise with the use of mild dynamic stretches and movements.
- Gradual Progression: Increase the intensity of your workouts or begin a new fitness routine gradually. keep away of abrupt activity increases that could put strain on your knee joint.
- Cross-training: To prevent overusing the same muscles and joints, mix up your program with other exercises and activities.
- Correct Technique: To prevent putting undue strain on your knee joint, make sure you’re exercising with the right form and alignment.
- Listen to Your Body: Keep an eye out for any pain or ache in the patient’s knees; if you notice any unusual sensations, it’s best to address them early rather than pushing through.
- Maintain a Healthy Weight: Carrying too much weight can put additional strain on the knee joint; choosing shoes that provide enough support and cushioning for your feet and knees, especially during physical activities, can help prevent joint strain and irritation.
- Stay Hydrated: Staying properly hydrated can help prevent stiffness.
- Balanced Muscles: Include strength training exercises that focus on all major muscle groups, supporting balanced muscle development and joint stability.
- Flexibility and Mobility: Maintaining appropriate joint range of motion and lowering the chance of stiffness can be achieved with regular stretching and mobility exercises.
- Rest and Recovery: Allow your body to recuperate in between workouts. An increased risk of injuries, including plica irritation, can result from overtraining.
- Pay Attention to Experts: If you’ve had a previous knee injury, or surgery, or are prone to knee issues, work closely with a physical therapist or healthcare provider to develop a safe exercise plan.
Prognosis:
The prognosis for plica syndrome is favorable after it is treated adequately. At a median follow-up of 27.5 months, 10% of the 969 patients in one trial had not reacted to treatment, while 26% had improved and 64% were symptom-free.
Conclusion:
The condition known as plica syndrome is caused by irritation or inflammation of the knee’s synovial plica, which frequently results in pain, swelling, and discomfort, particularly when moving. It frequently affects athletes or those who move their knees a lot.
Clinical evaluation and imaging studies are usually used to make the diagnosis, and conservative measures including rest, physical therapy, and anti-inflammatory drugs are used as treatment options. To ensure a full recovery and avoid long-term consequences, early detection and management are crucial.
FAQs
What is the average healing time for a plica?
Physical therapy or an exercise regimen at home are effective treatments for the majority of plica syndrome sufferers. These often entail quadriceps strengthening and hamstring stretches. Within six to eight weeks of beginning an exercise or physical therapy program, the majority of people begin to feel better.
How is plica neuropathica treated?
Dermatoscopy revealed matting and honey-colored concretions entwining the hair shaft, giving the appearance of a “wrangled mesh of wires.” In order to prevent recurrence, plica neuropathica is treated by removing the matted hair and assessing any underlying mental health conditions.
Is there a cure for plica syndrome?
The middle of your knee will hurt and swell if you have plica syndrome. Usually, stress or overuse is the culprit. Although some patients may need surgery, plica syndrome is typically successfully treated with medicine and physical therapy.
Is it possible to massage Pica?
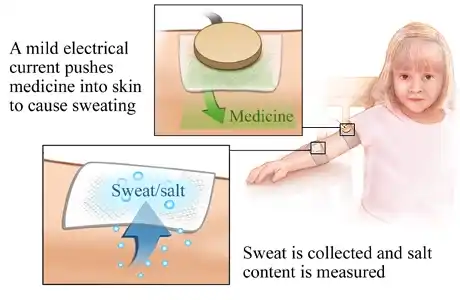
In order to reduce plica inflammation, we could also use therapies like friction massage and ultrasound. Iontophoresis is a technique we occasionally utilize in our therapy sessions to apply anti-inflammatory medication to the sore spot using a moderate electrical current.
What occurs if treatment for plica syndrome is not received?
What occurs if treatment for plica syndrome is not received? You run the danger of making your knee condition worse if you don’t get enough sleep and keep doing things. One can anticipate cartilage degradation and a progressive worsening of pain.
Which exercises are appropriate for people with plica syndrome?
To protect your lower back, lie on your back with one knee bent and the other straight. To maintain your knees straight and lock out your knee, bring your toes closer to you. Raise your leg straight slowly while locking it at a 60-70 degree angle. Hold for one second.
How is suprapatellar plica treated?
In most cases, knee plica issues resolve without surgery. You’ll need to apply ice and rest your knee for a bit. Your doctor might advise extending your leg muscles, particularly your quadriceps and hamstrings, and using anti-inflammatory pain relievers such ibuprofen or naproxen.
Does plica syndrome benefit from physical therapy?
By addressing all of the contributing causes, including discomfort and any lack of strength, flexibility, or body control, physical therapy aids in the rehabilitation from plica syndrome.
What side effects might untreated plica syndrome cause?
Chronic discomfort, knee instability, changes in movement patterns, inflammation, decreased range of motion, and functional restrictions are some examples of complications.
What at-home self-care activities can I do for Plica syndrome?
Resting, using ice, elevating your leg, using over-the-counter painkillers (if permitted), practicing mild movements, wearing appropriate footwear, and maintaining a healthy weight are all things you may do at home.
What side effects might untreated plica syndrome cause?
Chronic discomfort, knee instability, changes in movement patterns, inflammation, decreased range of motion, and functional restrictions are some examples of complications.
What is the Plica syndrome treatment?
Rest, physical therapy, ice, anti-inflammatory drugs, and in certain situations, corticosteroid injections are available as forms of treatment. If conservative measures are inadequate, surgery may be considered.
How is a diagnosis of Plica syndrome made?
A combination of the patient’s medical history, physical examination, and occasionally imaging tests like MRIs or X-rays are used to make the diagnosis. In certain situations, the diagnosis may also be confirmed by diagnostic injections.
Which factors lead to plica syndrome?
Overuse or repetitive knee motions, like bending, squatting, or kneeling, are frequently the cause of plica syndrome. Anatomical issues, prior knee operations, or injuries may also play a role.
Plica syndrome: what is it?
The illness known as “plica syndrome” is characterized by inflammation or irritation of the plica, a fold of synovial tissue inside the knee joint, which results in symptoms like clicking, swelling, and knee pain.
References
- Patel, D. (2023b, September 5). Plica syndrome – cause, symptoms, treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/plica-syndrome/
- Plica Syndrome. (2024, May 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21705-plica-syndrome
- Plica Syndrome: Effective Physiotherapy Management. (2023, July 17). https://arunalaya.com/news/details/154/Plica-Syndrome-Effective-Physiotherapy-Management