Gout
Introduction
Gout is an inflammatory disease that causes joint pain and swelling, usually in flares that last a week or two before resolving. Gout flares typically start in your big toe or lower leg. Gout develops when excessive amounts of urate accumulate in your body over time, resulting in needle-shaped crystals in and around the joint.
This causes inflammation and arthritis of the joint. When the body produces too much urate or excretes too little, urate levels rise. Many patients with high serum urate levels do not develop gout.
Gout can affect the following areas of the body:
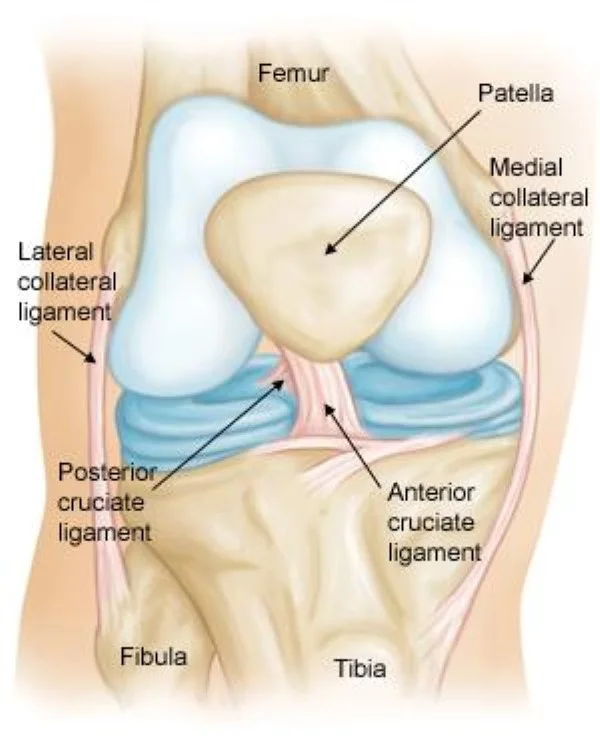
- Joints.
- Bursae are cushion-like sacs that connect bones and other soft tissues.
- Tendon sheaths are membranes that enclose tendons.
- Kidneys, since high levels of uric acid can produce stones.
- Gout is a disease that can progress through multiple stages:
Hyperuricemia occurs when there are elevated levels of urate in your blood for an extended period, as well as crystals in the joint, but no symptoms exist.
Gout flares are recurrent attacks of extreme pain and swelling in your joints.
Interval or intercritical gout refers to the interval between gout attacks when you do not experience any symptoms.
Tophi is a late stage of gout in which crystals accumulate in the skin or other parts of the body. Tophi, depending on their position, can cause lasting harm to your joints and other internal organs like the kidneys. Tophi can be prevented by proper therapy.
Gout is one of the most manageable kinds of arthritis when diagnosed early, treated, and lifestyle changes are implemented. Many patients prevent gout flares, reduce the severity of their symptoms, and even become gout-free.
Who is most likely to develop gout?
Many people get gout. It is mostly found in men than women. Gout typically develops in middle age. Women rarely develop gout before menopause, thus they develop the disease at a later age than men. Younger people are less likely to get the disease, but when they do, it is more severe.
Many people get gout. it if…
- Are male.
- Are older; it typically arises in middle age.
- Obesity occurs.
- Have certain medical conditions, such as:
- Heart failure.
- High Blood Pressure
- Metabolic Syndrome
- Chronic Kidney Disease
- Conditions that cause your cells to break down faster, such as psoriasis or multiple cancers.
- Rare hereditary disorders that contribute to high uric acid levels
- Have a family history of gout.
- Have an unhealthy diet and consume foods high in purines, such as red meat, organic meats, and some seafood.
- Drink booze.
- Consume a wide variety of fructose-containing meals and beverages.
Pathophysiology
Gout is a purine metabolic condition in which the ultimate metabolite, uric acid, develops into monosodium urate, precipitating and creating deposits (tophi) in joints, tendons, and surrounding tissues. Microscopic tophi may be walled off by a ring of proteins, preventing the crystals from interacting with cells and therefore avoiding inflammation.
Naked crystals may break out from walled-off tophi as a result of minor joint damage, medical or surgical stress, or fast uric acid level changes. When they penetrate the tophi, they cause a local immune-mediated inflammatory response in macrophages, which is initiated by the NLRP3 inflammasome protein complex.
Activating the NLRP3 inflammasome activates caspase 1, which transforms pro-interleukin 1β into active interleukin 1β, an important protein in the inflammatory cascade. This disorder is frequent among humans and higher human beings due to an evolutionary loss of urate oxidase (uricase), which breaks down uric acid.
The mechanisms that cause uric acid precipitation are poorly understood. While it may break down at normal levels, the likelihood of doing so increases as levels rise. Cool temperatures, fast changes in uric acid levels, acidosis, articular hydration, and extracellular matrix proteins are all thought to be major triggers in acute arthritis.
The greater precipitation at low temperatures helps to explain why the joints in the feet are most frequently afflicted. Trauma, surgery, chemotherapy, and diuretics are all potential causes of rapid uric acid alterations. The use of urate-lowering drugs, especially febuxostat, can result in an acute onset of gout. Calcium channel blockers and losartan have a reduced risk of gout than other hypertensive medicines.
Epidemiology
Gout affects around 1-2% of persons in the Western world at some point in their lives and is getting more common. Approximately 5.8 million people were affected in 2013. Between 1990 and 2010, gout rates had nearly doubled. This surge is thought to be the result of increased life expectancy, dietary changes, and an increase in gout-related disorders such as metabolic syndrome and high blood pressure. Gout rates are affected by factors such as age, race, and the season. The rates for males over 30 and women over 50 are 2%.
Cause of Gout
Gout occurs when urate, a chemical found in your body, accumulates and produces needle-shaped crystals in your joints. This causes pain, swelling, redness, and alterations in the movement and function of the affected joint. However, not everyone with elevated urate levels develops gout.
Urate is derived from purines, which are filled in your body’s tissues and numerous meals. When purines degrade, they produce urate. Urate is normally excreted by the body through urine. However, when too much urate is produced or too little is eliminated, it accumulates in your blood and needle-shaped crystals form in your joints, triggering inflammation known as gout flares, which cause pain and swelling.
How genes and environmental factors contribute to the accumulation of urate in your blood. However, several variables may raise your chances of acquiring gout, including:
- Having elevated urate levels.
- A family history of gout.
- Being Male.
- Going through menopause.
- Increasing age.
- Drinking alcohol.
- Drinking sugary drinks, such as soda.
- An unhealthy diet includes eating foods high in purines (typically from animal sources), a chemical that degrades into urate.
The following health factors may raise your risk of developing gout:
- Overweight or obesity.
- Metabolic syndrome refers to a set of symptoms that include high blood pressure, excessive blood sugar, abnormal cholesterol levels, and extra body fat around the waist.
- Chronic renal disease occurs when your kidneys are damaged and unable to filter blood properly.
- High blood pressure.
- Psoriasis and certain malignancies are examples of conditions that produce fast cell turnover.
- Rare hereditary diseases (Kelley-Seegmiller syndrome or Lesch-Nyhan syndrome) cause elevated urate levels.
Some medications can raise your risk of acquiring gout. For example,
- Diuretics assist your body in suppressing extra fluid.
- Low-dose aspirin.
- When consumed in significant quantities, niacin, a vitamin, is effective.
- Cyclosporine is an immunosuppressant used in organ transplants and to treat some autoimmune disorders.
Symptoms Of Gout
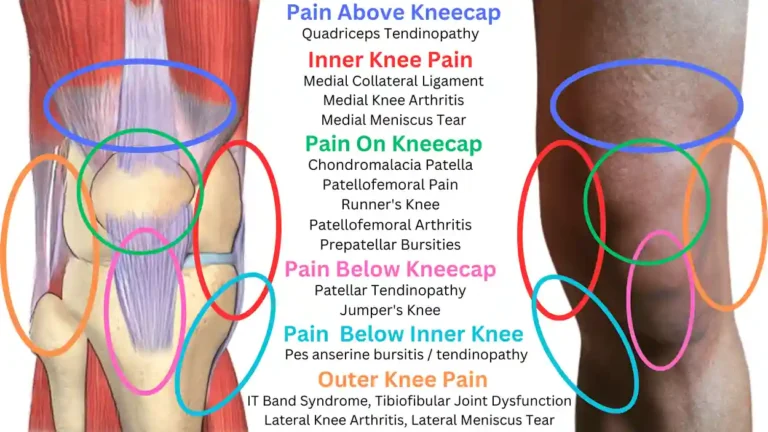
The most common gout symptom is discomfort in the affected joint. Many people experience their first bout of gout in one of their large toes, but it can affect other joints in the body. Gout flares frequently begin unexpectedly at night, and the acute pain may be enough to wake you up. Additionally, your joint may feel swollen, red, and warm.
Gout flares typically occur in a single joint and can be caused by certain meals, alcohol, drugs, physical trauma, or diseases. Flares usually subside after a week or two, and there are no symptoms in the meantime. Some people experience flares regularly
If gout is not treated for an extended time, tophi can develop. A tophus is a collection of needle-shaped crystals that form hard lumps under the skin, in and around the joints, and in other organs. Tophi are normally painless but can become painful with time, causing bone and soft tissue damage as well as deformed joints.
Some gout patients may be predisposed to multiple illnesses or complications, particularly those involving the heart and kidneys. Common conditions include:
- High blood pressure (hypertension).
- Chronic renal illness.
- Obesity.
- Diabetes.
- Nephrolithiasis refers to kidney stones.
- Myocardial infarction (a heart attack).
- Congestive heart failure.
Some people have too much uric acid in their blood and just show no symptoms. This is known as asymptomatic hyperuricemia.
Acute gout symptoms appear quickly due to the accumulation of uric acid crystals in your joint and keep going for 3 to 10 days.
You will have extreme pain and swelling, and your joints may feel heated. Between gout attacks, you will not have any symptoms.
If not treated, gout can become chronic. Tophi, or hard lumps, can grow in your joints as well as the skin and soft tissue that surrounds them. These deposits might cause irreversible damage to your joints.
Prompt treatment is necessary to prevent gout from becoming chronic.
Diagnosis
Your doctor can diagnose gout after reviewing your medical history, physical exam, and symptoms. Your doctor is likely to base your diagnosis on:
- Describe your joint pain.
- Indicate the frequency of joint pain and the degree of redness or swelling.
- Your doctor may also prescribe a test for identifying uric acid buildup in your joint. A sample of fluid from your joint might reveal whether it contains uric acid. They may also want to perform an X-ray on your joint.
If you have gout symptoms, start by seeing your primary care doctor. If your gout is severe, you should consult an expert on joint problems.
Gout can be identified and treated without further testing in people who have hyperuricemia and the typical acute arthritis at the base of the great toe (known as podagra). If there is disagreement about the diagnosis, the synovial fluid investigation should be performed. Plain X-rays are frequently unremarkable and do not confirm an early gout diagnosis. They can show symptoms of chronic gout, such as bone degradation.
Synovial fluid
Synovial Fluid Analysis: The gold standard for diagnosing gout is still the identification of monosodium urate crystals. A flare-up of gout is identified by the direct observation of MSU crystals in synovial fluid from bursas that have been affected by the disease, using compensated polarized light microscopy.
The presence of monosodium urate crystals in synovial fluid or a tophus results in a conclusive diagnosis of gout. All synovial fluid samples acquired from undiagnosed inflammatory joints by arthrocentesis should be evaluated for these crystals.
They have a needle-like shape and produce high negative birefringence when viewed under polarised light microscopy. This test is difficult to complete and requires a professional observer. Temperature and pH affect solubility, thus the fluid should be analyzed as soon as possible after aspiration.
Blood testing.
Hyperuricemia is a hallmark of gout, yet approximately half of the time gout develops without hyperuricemia, and the majority of persons with elevated uric acid levels never get gout. Thus, assessing uric acid levels has limited diagnostic usefulness.
Hyperuricemia is defined as a plasma urate level above 420 μmol/L (7.0 mg/dl) in men and 360 μmol/L (6.0 mg/dl) in women. Other blood tests that are frequently conducted include white blood cell count, electrolytes, renal function, and erythrocyte sedimentation rate (ESR). However, even in the absence of infection, gout may cause an increase in white blood cells and ESR. White blood cell counts as high as 40.0×109/l (40,000/mm3) have been reported.
Differential diagnosis.
The most important differential diagnosis for gout is septic arthritis. This should be considered in people who show indicators of infection or do not recover after treatment. A synovial fluid Gramme stain and culture can aid in diagnosis.
Other disorders that may appear similar include CPPD (pseudogout), rheumatoid arthritis, psoriatic arthritis, palindromic rheumatism, and reactive arthritis. Gouty tophi, especially when not found in a joint, might be mistaken for basal cell carcinoma or other neoplasms.
Treatment of Gout
Gout Home Remedies
Some home remedies may help to reduce uric acid levels and avoid gout attacks. The following items of food and drink have been recommended for gout:
- Tart cherries
- Ingredients include magnesium,
- ginger, and diluted apple cider vinegar.
- Ingredients include celery,
- nettle tea,
- dandelion, and milk thistle seeds.
- However, these alone may not be sufficient to manage gout.
Acute gout attacks require immediate medical attention because they are painful and may be incapacitating. The best course of treatment is to reduce inflammation and pain.
Acute flare-ups: The goal of management is to reduce the pain that results from inflammation. To decrease the intensity and length of the flare-up, the doctor should begin the treatment within the first twenty-four hours of the onset. Colchicine, systemic glucocorticoids, or non-steroidal anti-inflammatory drugs can be used in combination with rest and topical ice application. To avoid rebound flare-ups, the treatments should be administered for a minimum of 7 to 10 days.
Urate lowering therapy (ULT) should be developed in patients with recurrent attacks, tophi, urate arthropathy, renal damage, or in symptomatic patients with extremely high serum uric acid levels. Long-term uricosuric medications (probenecid), uricase agents (pegloticase), or xanthine oxidase inhibitors (allopurinol or febuxostat) may be used to lower urate levels and stop more acute flare-ups.
Another treatment option for tophaceous gout is surgical removal of the affected lesions.
Pharmacological treatment
If left untreated, gout can progress to gouty arthritis, a more severe kind of arthritis. This painful disorder can cause irreversible joint injury and swelling.
Your doctor will propose a treatment strategy based on the stage and severity of your gout.
Gout medications act in one of two ways: they reduce pain and inflammation, or they lower uric acid levels, which prevents recurrent episodes.
Drugs for gout pain include:
- Nonsteroidal anti-inflammatory medicines (NSAIDs) include aspirin (Bufferin), ibuprofen (Advil, Motrin),
- Naproxen (Aleve),
- Colchicine (Colcrys, Mitigare),
- Corticosteroids.
Drugs used to prevent gout attacks include:
Xanthine oxidase inhibitors include allopurinol (Lopurin, Zyloprim), febuxostat (Uloric), and probenecid (Probalan).
In addition to medications, your doctor may suggest lifestyle adjustments to help manage your symptoms and lower your risk of future gout attacks.
r.advise To improve health, consider reducing alcohol use, losing weight, and quitting smoking if necessary.
Non-pharmacologic:
To avoid more attacks, gout patients are advised to change their lifestyles. Dietary recommendations include cutting back on alcohol, limiting foods high in purifies (seafood, meat, high fructose corn syrup, and sweetened soft drinks), and switching from higher-fat dairy products to lower-fat or nonfat dairy products. Losing weight and drinking enough water will also lessen the frequency of gout attacks.
Physiotherapy treatment
Any patient with a history of gout, hyperuricemia, or a septic joint presentation should be referred for a medical evaluation before beginning physical therapy, the physical therapist should be aware of this.
The physical therapist’s primary focus during acute exacerbations should be on strengthening the management program and protecting the affected joint(s) with splinting, orthotics, or other assistive devices.
According to research published in Rheumatology, cryotherapy may be useful in reducing the discomfort brought on by sudden attacks of gout.
Physical therapists can help maintain the range of motion, strength, and function during intercritical periods. In addition, the physical therapist can help the patient maintain a healthy weight and design an appropriate exercise program.
When it comes to treating gout, an inflammatory form of arthritis caused by elevated blood uric acid levels, physical therapy can be quite helpful. Physical therapy usually targets pain management and joint protection during a gout flare-up, which can cause abrupt and acute discomfort, inflammation, and redness in the joints. Physical therapy can help restore joint strength, function, and mobility after the flare-up has gone away to avoid more flare-ups.
The benefits of gout physical therapy:
- Pain relief: To help reduce pain and inflammation, physical therapists may use a range of modalities, including ultrasound, electrical stimulation, heat, and ice.
- Increased joint mobility: Gout may affect a joint’s range of motion and cause stiffness. You can learn exercises from physical therapists to help increase your range of motion and flexibility.
- Improved strength: By strengthening the muscles surrounding the affected joints, one may reduce the likelihood of further flare-ups by supporting and protecting the joints.
- Improved balance and coordination: You can reduce your risk of falls and other injuries by working with a physical therapist to improve your balance and coordination.
- Self-management and education: Physical therapists can instruct you on how to manage your gout, including making lifestyle adjustments that can lower your chance of flare-ups.
The best type of exercise for gouty people:
Exercise is important for controlling gout and lowering the chance of flare-ups in the future. Even though you should rest, ice, and elevate during a flare-up, exercising in between episodes can help you in several ways.
Advantages of Gout Exercise:
- Reduce uric acid levels: Frequent exercise will promote the excretion of uric acid through sweat and urine, which may help to build up and prevent flare-ups in the future.
- Keep a healthy weight: Being overweight increases the risk of developing gout. Exercise eases joint pressure and aids in weight management.
- Improve joint health: By improving the range of motion, strength, and flexibility around affected joints, low-impact exercises can help to improve joint health overall.
- Boost mood and general well-being: Engaging in regular physical activity can help manage gout by lowering stress, elevating mood, and improving general well-being.
Selecting the Proper Workouts:
Concentrate on low-impact activities: Reduce the strain on your joints. Choose to:
- Walking: Suitable for all fitness levels and excellent for beginners. Increase speed and distance gradually after starting slowly.
- Swimming is a great low-impact exercise that is easy on joints and provides resistance and buoyancy.
- Cycling: Without putting undue strain on the joints, stationary bikes or outdoor cycling are good for the heart.
- Elliptical trainer: Provides impact-free, low-impact cardiovascular exercise that simulates running.
- Water aerobics: Exercises increase strength and flexibility while buoyancy lowers stress.
- Yoga: For the benefit of joint health, gentle yoga points out flexibility and range of motion.
Additional Tips:
- Increase duration and intensity gradually after starting slowly.
- When your body tells you to rest, do so.
- Before, during, and after exercise, drink plenty of water.
- Before exercising, warm up, and after, cool down.
- Consult a physical therapist or your doctor before beginning a new fitness regimen.
What to look forward to from gout physical therapy:
A physical therapist will probably ask you about your medical history, your current symptoms, and your treatment objectives during your initial evaluation. After that, the physical therapist will examine you to determine your strength, balance, and range of motion.
The physical therapist will create a treatment plan based on your specific needs, which may include:
- Modalities: To help reduce pain and inflammation, try using ice, heat, ultrasound, or electrical stimulation.
- Exercises: To increase joint mobility, flexibility, and strength, perform range-of-motion, stretching, and strengthening exercises.
- Exercises for balance and coordination: These can help you avoid falls by improving your balance and coordination.
Gout surgery.
Gout can usually be cured without surgery. However, over time, this disorder can cause joint damage, tendon tears, and infections in the skin surrounding the joints.
Tophi, or hard deposits, can build up on your joints and in other locations, such as your ears. These lumps can cause pain and swelling, as well as long-term damage to your joints.
There are three surgical techniques for treating tophi:
- Tophi removal procedure
- Joint Fusion Surgery
- Joint Replacement Surgery
- Which of these surgeries your doctor advises is determined by the severity of the injury, the location of the tophi, and your personal preferences.
Diet for Gout
Foods to Like:
- Low-purine foods: These include fruits, vegetables (apart from spinach and asparagus), whole grains (brown rice, quinoa, and oats), nuts, seeds, eggs, low-fat dairy products, and coffee (in moderation) that have little effect on uric acid levels.
- Cherries: Due to their anti-inflammatory qualities, studies indicate cherries may help lessen gout attacks. You can eat them frozen or fresh, but juice has more sugar than other foods.
- Water: Drink a lot of water throughout the day to stay hydrated. Aim for 8–10 glasses to stimulate the excretion of uric acid.
Foods to Avoid
Certain foods are naturally high in purines, which your body converts into uric acid.
Most people can tolerate purine-rich diets. However, if your body has difficulty releasing excess uric acid, you may want to avoid specific foods and drinks such as:
- Red meat,
- Organic meats,
- Some seafood,
- Alcohol.
Even if they do not include purines, sugar-sweetened beverages and foods high in fructose can be troublesome. Some foods help reduce uric acid levels in the body and are healthy choices for gout.
Additional Tips:
- Maintain a healthy weight: Carrying too much weight can raise the production of uric acid.
- Control your stress: Using calming methods like yoga or meditation can help prevent gout flare-ups.
- Examine food labels: Watch out for hidden purines in processed foods, and whenever possible, select low-purine options.
- Speak with a dietician: A registered dietitian can design a customized meal plan for you that is gout-friendly and meets your needs and preferences.
Gout and Alcohol
Alcohol, like red meat and seafood, contains large levels of purines. Your body makes uric acid as it breaks down purines.
More uric acid raises your chances of developing gout. Alcohol might also slow the rate at which your body eliminates uric acid.
Not everyone who drinks develops gout. However, excessive alcohol consumption (more than 12 drinks per week) can raise the risk, particularly among men. Beer is more likely than alcohol to influence risk.
In surveys, respondents stated that drinking alcohol causes gout flare-ups.
Gout triggers.
Certain foods, drugs, and situations can cause gout symptoms. You may need to avoid or limit foods and drinks that are high in purines.
- Red meat includes take and veal, as well as organ meats.
- Fish (e.g. cod, scallops, mussels, salmon), alcohol, sodas, and fruit juice are all options.
- Some drugs used to treat other disorders raise the quantity of uric acid in your blood.
Medications for decreasing blood pressure include diuretics, aspirin, beta-blockers, and angiotensin II receptor blockers.
Your health may also play a role in flare-ups. The following conditions have been related to gout:
- Obesity
- Diabetes or prediabetes.
- Risks include dehydration, joint injury, and infection.
- Congestive heart failure.
- High Blood Pressure
- Kidney disease.
Sometimes it can be difficult to determine which of these things is causing your gout periods. Keeping a diary might help you track your diet, medications, and health to figure out what’s causing your symptoms.
Here are some things you can do to help prevent gout:
- Limit how much alcohol you consume.
- Limit your consumption of purine-rich foods such as shellfish, lamb, cattle, animal, and organ meats.
- Consume a low-fat, non-dairy diet high in veggies.
- Maintain a healthy body weight.
- Avoid smoking.
- Exercise regularly.
- Stay hydrated.
If you have a medical condition or take medications that increase your risk of gout, consult your doctor about how to reduce your risk of gout attacks.
Prevention
The risk of gout attacks can be reduced by avoiding alcoholic beverages, limiting fructose consumption (e.g., high fructose corn syrup), and avoiding purine-rich animal meals such as organ meats and shellfish. Eating dairy products, vitamin C-rich foods, coffee, and cherries can help avoid gout episodes, as does decreasing weight. Gout may develop as a result of sleep apnea and the production of purines from oxygen-starved cells. Treatment for apnea can reduce the frequency of attacks
Gout with Tophus.
When uric acid crystals accumulate in joints over time, they form hard deposits known as tophi beneath the skin. Without treatment, these tophi can cause bone and cartilage degeneration, leaving the joints permanently deformed.
Tophi are swelling lumps near the joints that resemble knots on a tree trunk. They appear in joints such as the fingers, feet, and knees, as well as on the ears. Tophi themselves are not harmful, but the inflammation they generate can be uncomfortable.
Tophi can occur in connective tissue outside the joints.
Is gout painful?
Yes, gout can cause pain. Pain in the big toe is frequently one of the first symptoms reported. The discomfort is accompanied by more common arthritis symptoms, such as joint swelling and warmth.
Gout pain can be severe. Pain in the big toe might be severe at first. Following the intense episode, it may become dull and painful.
The pain, swelling, and other symptoms are caused by the immune system’s response to uric acid crystals in the joints. This attack causes the release of particles called cytokines, which increase severe inflammation.
Gout Essential Oils
Essential oils are plant-derived chemicals used in aromatherapy. Some oils are thought to have anti-inflammatory, analgesic, and antibacterial properties.
Some of the essential oils used to treat gout are:
- Lemongrass oil
- Celery Seed Oil
- Yarrow oil extract
- Olive leaf extract.
- Chinese cinnamon
Consult your doctor before using any essential oils. Remember that the Food and Drug Administration (FDA) does not monitor the purity or quality of essential oils, so study the brand.
When using essential oils, remember to take the following safety precautions:
- Avoid applying essential oils straight to your skin. It is important to dilute them first with a carrier oil like coconut oil or jojoba oil. For a 3% dilution, use 20 drops of essential oil and 6 teaspoons of carrier oil.
- Do not put essential oils in your mouth because they are not safe to consume.
- Store essential oils and carrier oils in a cool, dark place away from direct sunlight and heat.
Is Gout hereditary?
Gout is at least partly hereditary. Researchers have discovered thousands of genes that boost the susceptibility of individuals to gout, including SLC2A9 and ABCG2. Gout-related genes affect how much uric acid the body stores and releases.
Gout is passed down across families due to genetics. People who have a parent, sibling, or other close family with gout are more likely to develop the ailment themselves.
It is likely that genes only pave the way for gout. The condition is caused by environmental factors, such as food.
Risk factors
- Diet: Eating a lot of purines, which are present in seafood, red meat, organ meats, sugar-filled food, and alcohol, can raise your risk of developing gout. The body breaks down purines into uric acid, and excessive uric acid levels can cause urate crystals to form in the joints, which can result in gout attacks.
- Obesity: A higher risk of gout is associated with being overweight or obese. This is because being overweight can cause your body to produce more uric acid and make it harder for your kidneys to remove uric acid from your blood.
- Medical conditions: You may be more likely to develop gout if you have high blood pressure, heart disease, kidney disease, sleep apnea, or any of these conditions. These diseases may have an effect on how your body makes or releases uric acid.
- Medication: Several drugs, including cyclosporine, low-dose aspirin, and diuretics, can raise your risk of developing gout. Your body’s reaction to uric acid may be affected by these medications.
- Genetics: A family history of gout raises your chance of getting the illness. This is because some genes may increase your risk of developing gout.
- Age and gender: Men are more likely than women to develop gout, and the likelihood of developing gout rises with age. Age-related changes in kidney function and hormone levels are probably the cause of this.
Complication
- Joint deformity and damage: Chronic phases of gout can permanently harm the affected joints, resulting in stiffness, deformity, and severe discomfort. This may have a major effect on your mobility and standard of living.
- Tophi: Urate crystal deposits that look like chalk can develop under the skin in the areas surrounding joints, ears, and other body parts. Although they usually don’t hurt, they can enlarge and look ugly, and in certain situations, they can even erode bone and tissue.
- Kidney stones: If left untreated, kidney stones can be very painful and cause additional problems. High uric acid levels can also raise your risk of developing kidney stones.
- Chronic kidney disease: Gout can strain your kidneys and eventually result in chronic kidney disease, which can be fatal if your uric acid levels are constantly high.
- Risk of cardiovascular disease is elevated: Research has connected gout to a higher risk of heart attacks, strokes, and other cardiovascular issues. The common risk factors, like obesity and high blood pressure, are probably to blame for this.
Prognosis
Prognosis Without therapy, an acute gout attack typically disappears in five to seven days; however, 60% of patients experience a second attack within a year. Gout patients are more likely to develop hypertension, diabetes, metabolic syndrome, renal and cardiovascular disease, all of which raise their risk of death.
It is unknown whether urate-lowering drugs reduce the risk of cardiovascular disease. This could be related to its connection with insulin resistance and obesity, but some of the increased risk appears to be independent.
Conclusion
Gout is typically successfully treated and managed. Your doctor may recommend drugs to help you lower your uric acid levels while also reducing inflammation and pain.
Your doctor or nutritionist may also recommend dietary adjustments to help you avoid flare-ups. Gout can be effectively managed with a balanced diet and healthy lifestyle practices.
FAQs
What are the ten foods that cause gout?
Gout (Low Purine) Diet: Best Foods to Eat and Avoid
The top ten drinks and foods that cause gout are:
Drinks with sugar and sweets.
High-fructose corn syrup.
There is alcohol.
Organ and game meats.
Some seafood, including herring, scallops, mussels, codfish, tuna, trout, and haddock. Red meats include beef, lamb, animal, and bacon.
Turkey
Which foods can help reduce uric acid?
Apples have a high dietary fiber level. This helps to lower your uric acid levels. Fibre absorbs uric acid from the bloodstream and removes it from the body. Apples are also high in malic acid, which assists in combating the effects of uric acid in the body.
What are the first-aid treatments for gout?
Applying an ice pack to the affected joint may help to reduce pain and inflammation. Wrap a pack (a bag of crushed ice or frozen peas would suffice) in a dishcloth and apply to the affected area for 20 to 30 minutes at a time, multiple times per day. Call your doctor. Inform your doctor about what is going on immediately.
Which tablet is the best for uric acid?
Drugs like allopurinol (Aloprim, Lopurin, Zyloprim) and febuxostat (Uloric) help your body produce less uric acid. Allopurinol side effects might include fever, rash, hepatitis, and kidney issues. Febuxostat side effects include rash, nausea, and decreased liver function.
Does rice cause gout?
A study discovered that lowering the glycemic index reduced uric acid levels in subjects. Limiting foods with a high glycemic index, such as white bread, pasta, and white rice, may help reduce uric acid levels and maybe avoid gout onset or flares.
How do I check my gout at home?
In these kits, a drop of blood is drawn from a finger stick, applied to a test strip, and the level of uric acid is measured using a handheld meter. At-home testing cannot diagnose gout and is not a substitute for medical care or testing authorized by a doctor or rheumatologist.
Is gout serious?
Without therapy, gout bouts may become more frequent and prolonged, increasing your risk of chronic joint damage. In the most severe cases, surgery may be necessary to repair or replace a damaged joint.
What organs does gout affect?
Tophi is a late stage of gout in which crystals accumulate in the skin or other parts of the body. Tophi, depending on their position, can cause lasting harm to your joints and other internal organs like the kidneys. Proper treatment can avoid the development of tophi.
What is the end stage of gout?
Stage Four.
If uric acid levels are not effectively regulated during the interval stage, gout may develop to the most severe form, chronic tophaceous gout. Chronic gout is characterized by the buildup of urate crystals known as tophi, which can show as lumps or nodules under the skin.
Does gout worsen at night?
Purines are compounds found in all diets, but particularly in red meats, seafood, organs, and alcohol. if you know why or how you got gout, you’re more likely to experience a painful attack in the middle of the night. The chance of a gout attack is 2.4 times greater at night than in the morning or day.
Do tomatoes contribute to gout?
Tomatoes are generally considered a low-purine food that is good for gout sufferers. They also contain anti-inflammatory substances like vitamin C. However, substances like glutamate and phenolic acid found in tomatoes have been shown to cause gout in certain individuals.
Does salt cause gout?
Blood pressure diets may be used to control flare-ups of gout.
Uric acid levels peaked during the DASH diet’s low-sodium phase and decreased during the medium- and high-sodium diets. These modifications brought on by salt consumption were minor but noteworthy. However, the authors do not advise gout sufferers to begin consuming more salt in their diet
References
- Gout. (2024, January 30). Wikipedia. https://en.wikipedia.org/wiki/Gout
- Branch, N. S. C. A. O. (2023, December 21). Gout. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/gout
- Kinman, T. (2023, March 8). Gout: Symptoms, Causes, and Treatments. Healthline. https://www.healthline.com/health/gout#takeaway
- Gout. (n.d.). Physiopedia. https://www.physio-pedia.com/Gout





19 Comments