Edema
What is a Edema?
Edoema, sometimes written edema, is the buildup of fluid in soft tissues. Other names for it include swelling, hydropsy, dropsy, and fluid retention. Most often affected are the arms or legs. Among the symptoms are stiff joints, heavy spots, and the feeling of tight skin. Any other symptoms will depend on the underlying cause.
Some of the potential causes include angioedema, certain medications, liver disorders, low protein levels, heart failure, deep vein thrombosis, and lymphedema. It can also occur to those who are immobile because of a stroke, spinal cord injury, aging, or temporary immobility caused by prolonged standing or sitting, menstruation, or pregnancy. It is more harmful if the illness worsens quickly or if there is pain or dyspnea.
The fundamental reason determines the course of treatment. A diuretic and less salt may be ingested if sodium retention is the underlying cause. Support stockings and leg elevation may be beneficial for leg edema. More elderly people are frequently affected. The word “da edema,” which means “swelling” in Greek, is the source of the name.
Pathophysiology:
Edema is caused by anything that increases endothelial permeability, decreases oncotic pressure, raises capillary pressures, or hinders lymphatic drainage. A common cause of edema, including congestive heart failure, left ventricular failure resulting from pulmonary edema, and right ventricular failure, is elevated capillary pressure. The arterial pressure that is pressed onto the capillary is determined by the autoregulatory capacity of capillary hydraulic pressure, which permits variations in resistance at the precapillary sphincter.
On the other hand, the capillary’s venous end is poorly regulated, which causes variations in venous pressure to cause parallel variations in capillary hydraulic pressure. There are two ways to raise venous pressure. First, when the volume of blood is increased; second, when the venous end is blocked.Cirrhosis or right heart failure causes venous blockage, whereas heart failure and renal illness cause volume expansion, both of which eventually contribute to edema. In addition to causing deep vein thrombosis, external compression, and superior vena cava blockage, local venous obstruction can also raise capillary pressure.
Common causes of reduced oncotic pressure include diabetic nephropathy, lupus nephropathy, amyloidosis, minimal change disease, membranous glomerulonephritis, HIV-associated nephropathy, focal segmental glomerulosclerosis, IgA nephropathy, light chain associated renal disorders, chronic glomerulonephritis, and radiation nephropathy. Reduced oncotic pressure is usually caused by hypoalbuminemia and occurs in a number of diseases, including renal disease, where albumin is lost across the glomerulus (nephrotic syndrome). Reduced oncotic pressure and eventually edema can also result from hepatic diseases including cirrhosis and chronic liver disease caused by insufficient albumin synthesis, as well as malabsorption or malnutrition caused by insufficient albumin intake and synthesis, such as kwashiorkor.
Edema is caused by increased capillary permeability, usually as a result of vascular damage, for a number of reasons. Damage to vessels increases the capillary walls’ porosity, which in turn increases net filtration. Additionally, the difference between the oncotic pressure of the capillary and the oncotic pressure underneath the endothelium glycocalyx narrows when the coefficient of proteins across the capillary wall diminishes. Edema develops when the oncotic pressure gradient decreases. When histamine and oxygen free radicals cause microvascular damage and direct physical harm, capillary permeability usually rises in burn patients.
Capillary permeability is also increased by vascular endothelial growth factor or recombinant human interleukin 2 treatment (PMID:3495213, PMID:10836914). Edema, particularly pulmonary edema, is caused by an increase in pulmonary capillary permeability that happens in any situation when cytokines like interleukin 1 or tumor necrosis factor are released, as in respiratory distress syndrome. Some even contend that increased capillary permeability may contribute to edema in cases of diabetes mellitus or kwashiorkor.
Edema is caused by eating after three or more days of fasting. This is thought to be because re-feeding with carbs raises insulin levels, which improves sodium reabsorption.
Furthermore, one well-known cause of edema is lymphatic blockage; other common causes include tumors, fibrosis, inflammation, infection (e.g., Filariasis from Wuchereria bancrofti), surgery, congenital anomalies, and lymphedema. Interstitial albumin and other proteins build up in myxedema, which is usually caused by thyroid disorders. This results in an excess of interstitial fluid and protein without an increase in lymphatic movement. According to some theories, this occurs because filtering proteins attach to interstitial mucopolysaccharides and block the lymphatics’ ability to remove them. Although there are numerous causes of edema, the underlying cause determines the unique physiology.
Mechanism of Edema:
Edema can develop as a result of six factors:
- increased hydrostatic pressure,
- decreased colloidal or oncotic pressure in blood vessels,
- elevated tissue colloidal or oncotic pressure, increased permeability of blood vessel walls (including inflammation),
- blockage of fluid clearance in the lymphatic system, and modifications to the tissues’ ability to retain water.
- Increased hydrostatic pressure frequently indicates that the kidneys are retaining water and salt.
The Starling equation’s forces govern the generation of interstitial fluid. Water tends to seep out of blood vessels into the surrounding tissue due to hydrostatic pressure. As a result, the protein concentrations in tissue and blood plasma differ. Consequently, the greater protein content in the plasma tends to suck water back into the blood vessels from the tissue due to the colloidal or oncotic pressure. The difference between the two forces and the vessel wall’s permeability to water, which establishes the flow rate for a particular force imbalance, determines the fluid leakage rate, according to Starling’s equation.
Capillaries and post-capillary venules, which have semi-permeable membrane walls that let water flow more easily than protein, are where the majority of water leaks occur. (The protein is said to be reflected, and a reflection constant of up to one indicates how effective the reflection is.) Permeability to water increases first if the spaces between the vessel wall’s cells widen, but as the spaces get bigger, permeability to proteins also rises while the reflection coefficient decreases.
By increasing the hydrostatic pressure inside the blood vessel, decreasing the oncotic pressure inside the blood vessel, or increasing the permeability of the vessel wall, changes in the variables in Starling’s equation can cause edemas to occur. The latter has two outcomes. By making it easier for protein to exit the vessel, it lowers the colloidal or oncotic pressure differential and permits water to flow more freely.
The lymphatic system, another group of vessels, functions as a “overflow” and has the ability to replenish the bloodstream with a significant amount of extra fluid. However, even the lymphatic system can get overloaded. If the lymphatic system is clogged or there is just too much fluid, the fluid will stay in the tissues and cause swelling in the legs, ankles, feet, belly, or any other portion of the body.
An increase in tissue colloidal or oncotic pressure; a decrease in blood vessel colloidal or oncotic pressure; or a rise in hydrostatic pressure. an obstruction of the removal of lymphatic fluid; an increase in the permeability of blood vessel walls (as in inflammation). Additionally, changes in the tissues’ own capacity to retain water. An rise in hydrostatic pressure usually indicates that the kidneys are retaining salt and water.
The Starling equation’s forces govern how much interstitial fluid is produced. The hydrostatic pressure in blood arteries causes water to tend to seep into the tissue. Consequently, the protein composition of tissue and blood plasma varies.
Consequently, the higher protein content in plasma tends to draw water from the tissue back into the blood vessels by oncotic or colloidal pressure. Starling’s equation states that the difference between the two forces and the vessel wall’s permeability to water determine the rate of fluid leakage for a given force imbalance.
Most water leakage happens in capillaries or post-capillary venules, which have a semi-permeable membrane wall that allows water to enter more easily than protein. (The protein is said to be reflected; the efficacy of reflection is indicated by a reflection constant up to 1.) As the gaps between the cells of the vessel wall expand wider, the permeability to water first increases. However, as the gaps get larger, the permeability to protein also increases, and the reflection coefficient decreases.
There are two basic processes in the production of edema. A change in capillary hemodynamics that promotes fluid flow from the vascular space into the interstitium is the first. Edema can also result from the kidneys retaining water and sodium that has been given intravenously or through diet. Initially, fluid enters the interstitium from the arterial space, which lowers tissue perfusion and plasma volume. The kidney keeps water and salt in response to these changes. The plasma volume recovers to normal, and some fluid remains in the vascular space. Edema is the outcome of retained fluid entering the interstitium due to this alteration in capillary hemodynamics.
Higher capillary hydraulic pressures or greater capillary permeability, endothelial glycocalyx rupture, decreased interstitial compliance, lower plasma oncotic pressure, or a combination of these can also cause edema. Because filtered fluids do not normally return to the systemic circulation, lymphatic blockage can also result in fluid accumulation. The lower extremities are especially vulnerable to fluid collection because edema can be localized or widespread and gravity is a major factor in fluid accumulation.
Signs and symptoms:
Specific area
Edema may arise in some organs due to tissue-specific mechanisms. Several instances of edema in various organs:
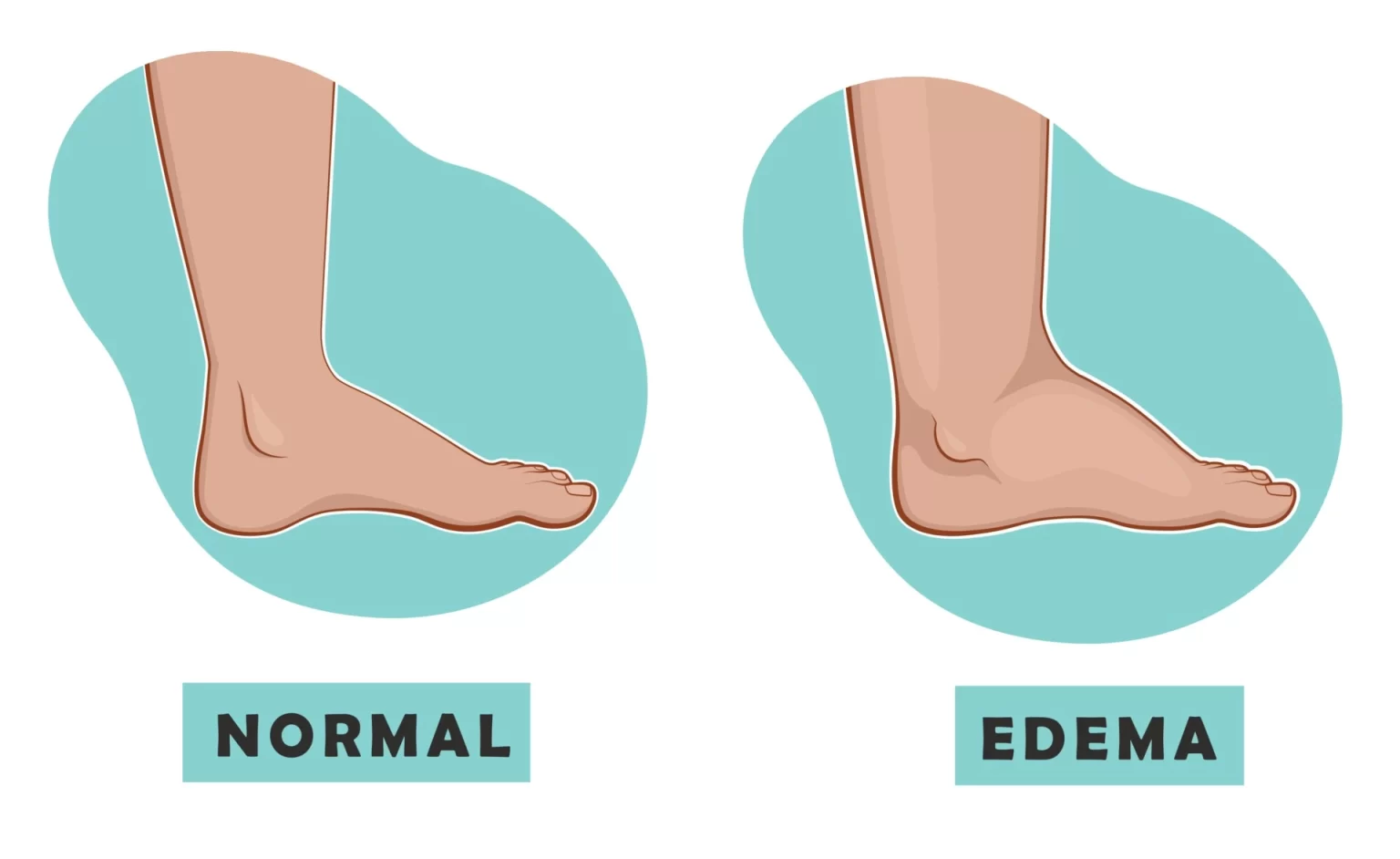
Peripheral edema
Peripheral edema, sometimes referred to as “dependent” edema of the legs, is a buildup of extracellular fluid in the lower extremities caused by gravity. It occurs when fluid accumulates in the hands, feet, or legs. This often occurs in immobile patients, such as paraplegics or quadriplegics, pregnant women, or otherwise healthy individuals, due to hypervolemia or extended standing or sitting.
Cerebral edema is the accumulation of extracellular fluid in the brain; it may occur under toxic or abnormal metabolic conditions, such as systemic lupus or low oxygen levels at high altitudes; it causes somnolence or unconsciousness, which leads to brain herniation and death; it can also occur in people with elevated hydrostatic venous pressure or decreased oncotic venous pressure; it can be caused by congestion in the lymphatic or venous veins draining the lower leg; it can also occur in people with elevated hydrostatic venous pressure or decreased oncotic venous pressure.
Pulmonary edema
When the pressure in the lung’s blood vessels rises, pulmonary edema occurs because of a blockage in the pulmonary veins. This is frequently caused by the left ventricle of the heart failing. Altitude sickness or the inhalation of toxic chemicals can also cause it. One sign of pulmonary edema is dyspnea. Pleural effusions may result from an accumulation of fluid in the pleural cavity.
Edema in the cornea of the eye can also result from keratitis, acute conjunctivitis, glaucoma, and following surgery. Bright lights could be surrounded by colored haloes for those who are impacted.
Periorbital edema, often known as swollen eyes, is the term used to describe an edema that encircles the eyes. The fluid’s gravitational redistribution in the horizontal posture may be the cause of the periorbital tissues’ most noticeable swelling just after awakening.
Common causes of cutaneous edema, sometimes called contact dermatitis, include mosquito bites, spider bites, bee stings (both wheal and flare), and skin contact with certain plants, like western poison oak or poison ivy.
Myxedema
Another type of cutaneous edema caused by an increased deposit of connective tissue is called myxedema. The tissue’s increased inclination to hold water in its extracellular space causes edema in myxedema and several other rare illnesses. This is caused by an increase in hydrophilic, carbohydrate-rich molecules, most likely hyaluronic, that are deposited in the tissue matrix in myxedema.
The reason why edema in dependent areas is more common in older adults who sit on chairs a lot at home or on airlines is unknown. Estrogens change the water content of tissues, which has an impact on body weight. The transfer of water from tissue matrix to lymphatics may be hindered in a number of poorly understood situations due to changes in the hydrophilicity of the tissue.
Myoedema
Percussion, such as flicking a relaxed muscle with the thumb and fingers, can cause myoedema, a localized swelling of muscle tissue. A noticeable, hard, and non-tender mound is formed 1-2 seconds after the tactile stimulation, and it returns to normal in 5-10 seconds. It is a sign of a hypothyroidism-related myopathy, such Hoffmann syndrome.
Lymphedema
The failure of the lymphatic system leads to inappropriate clearance of interstitial fluid in lymphedema, which can be caused by blockage (e.g., pressure from enlarged lymph nodes or cancer), damage to the lymphatic channels from radiotherapy, or infection (e.g., elephantiasis) infiltration of the lymphatics, but it is most obviously caused by muscle weakness resulting from immobility in conditions such as multiple sclerosis or paraplegia.
It has been suggested that the edema that some people experience after taking cyclo-oxygenase inhibitors that function similarly to aspirin, such as ibuprofen or indomethacin, may be caused by the suppression of lymph heart activity.
Generalized edema
Hydrostatic pressure rises with heart failure. Osmotic pressure decreases in both liver failure and nephrotic syndrome.
Edema-causing factors that are generalized throughout the body may cause edema in different organs as well as peripherally. For example, severe heart failure can cause pulmonary edema, pleural effusions, ascites, and peripheral edema; the medical term for such severe systemic edema is anasarca.
The majority of physicians note that although a low plasma oncotic pressure is often cited as the cause of the edema associated with nephrotic syndrome, the edema may appear before any detectable proteinuria or a decrease in plasma protein levels. The biochemical and structural alterations in the basement membrane of the capillaries in the kidney glomeruli that cause most types of nephrotic syndrome also affect, albeit to a lesser extent, the vasculature in most other body tissues; if the other capillaries are also more permeable, the resulting increase in permeability that causes protein in the urine may help to explain the edema.
In addition to the previously mentioned symptoms, some women often experience edema in the later stages of pregnancy; this is more common in those with a history of poor circulation or pulmonary problems, and it is worse in women who already have arthritis. Women with pre-existing arthritic conditions are more likely to need medical attention for discomfort caused by excessive swelling. Pregnancy-related edema is usually found in the lower leg, usually from the calf down. A child with hydrops fetalis will have fluid accumulation in at least two different body compartments.
Other:
Edema can have a variety of reasons, and the appearance will vary depending on the cause. Edema typically manifests as swelling in the ankles, but it can sometimes spread higher. Malabsorption, protein calorie malnutrition, obstructive sleep apnea, nephrotic syndromes, liver illness (cirrhosis), allergic reactions (urticaria or angioedema), congestive heart failure, constrictive pericarditis, pregnancy, or adverse drug reactions are common causes. Venous thrombosis is suspected when edema is unilateral or asymmetrical. When determining the precise site of edema in heart failure, the specific cause is crucial. For instance, pulmonary edema but not peripheral edema are common in conditions like coronary heart disease, hypertension, or left-sided valvular disease.
Cor pulmonale, on the other hand, is characterized by edema in the limbs and is initially pure right ventricular failure. Cardiomyopathies cause the left and right ventricles to be equally involved, and they frequently result in peripheral and pulmonary edema at the same time. Heart failure is also strongly suggested by an S3 heart sound, particularly when pulmonary or widespread edema is present. A chest x-ray displaying enlarged pulmonary vasculature, cardiomegaly, and haziness of vascular borders, which suggest fluid overload, are classic indicators of congestive heart failure. Additionally, patients may exhibit pitting edema and dyspnea.
Cellulitis, chronic venous insufficiency, deep vein thrombosis, lymphedema, or May-Thurner syndrome are the most common causes of localized edema. Infectious and/or thrombotic reasons should be suspected when the patient’s vitals are unstable (febrile, tachycardic, or tachypneic) and the edematous area is warm.
Antihypertensives (calcium channel blockers, minoxidil, or hydralazine), antidepressants (trazodone and MAO inhibitors), antivirals (acyclovir), chemotherapeutics (docetaxel, cyclophosphamide, and cyclosporine), fludrocortisone, pramipexole, hormones (estrogens, progesterones, and anabolic steroids), thiazolidinediones, and non-steroidal anti-inflammatory medications (celecoxib and ibuprofen) are the most common medications that cause edema.
Increased intracranial pressure can also result from brain edema. If treatment is not received, this is frequently fatal. Numerous factors, such as widespread hypoxia, trauma, abscesses, or tumors, can result in intracranial edema.
Edema can also be clinically caused by fluid in the bodily cavities. Ascites (caused by cirrhosis, heart failure, or tumors), pericardial effusion (caused by inflammation or tumors), and pleural effusion (caused by heart failure, inflammation, or tumors) are among the etiologies. Abdominal distention, fluctuating dullness, and a fluid wave upon abdominal percussion are the usual symptoms of ascites.
The etiology of widespread edema greatly influences the course of treatment. Treating the root cause is the first step in the therapy process. In some cases, such pulmonary edema, the illness can be fatal and needs to be treated very once. In some situations, it is possible to reduce interstitial fluids more gradually. Fluid removal with diuretics must be carefully controlled if retention results from compensatory factors, such as cirrhosis or heart failure, as treatment may impair arterial blood volume and, consequently, tissue perfusion. Edema fluid mobilization can happen quickly when edema is caused by heart failure, nephrotic syndrome, or sodium retention. In particular, two to three liters of fluid can be removed in a 24-hour period from a patient with anasarca without causing clinically noticeable changes in plasma volume.
Dietary changes can also assist minimize fluid overload. If hypoalbuminemia is present, consider increasing protein consumption to 1g/kg/dL and lowering sodium intake to 2 g/dL. Edema fluid can be decreased with diuretics, particularly loop diuretics like torsemide, bumetanide, and furosemide. Diuretics should be used with caution in individuals with liver cirrhosis and ascites who do not have peripheral edema or who have localized edema caused by lymphatic or venous blockage or cancer. After fluid levels drop in these situations, hypovolemia may result. The etiology determines the clinical profile of edema, and meticulous examination of the patient’s underlying illness maintains therapy.
Causes of edema:
Edema is common since it can be caused by a number of factors. Since minor cases of edema go away on their own, it is difficult to determine the exact rate of recurrence.
Heart
Healthy blood vessel pressure should be maintained in part by the heart’s ability to pump blood. However, if the heart begins to fail (a condition known as congestive heart failure), the pressure changes may cause very significant water retention. Although this sickness is most noticeable in the legs, feet, and ankles, water sometimes accumulates in the lungs, causing a chronic cough. This condition is usually treated with diuretics since, in the absence of them, water retention may make breathing difficult and increase cardiac strain.
Kidneys
Significant water retention can also be caused by renal failure, which occurs when the kidneys are unable to filter fluid from the bloodstream and convert it to urine. As with diseases like lupus or nephrotic syndrome, inflammation is often the initial indication of kidney disease. Ankle and leg swelling is a typical symptom of this type of water retention.
Liver
One common cause of the development of edema in the legs and abdomen is cirrhosis, or scarring, of the liver.
Veins
The most prevalent kind of edema (about 90%) is phlebetic lymphedema, also known as phlebolymphedema, which occurs in patients with untreated chronic venous insufficiency. Defective “leaky” veins that permit blood to backflow (venous reflux) and impede the return of blood to the heart (venous stasis) are the source of this combined venous/lymphatic illness. Standing causes a significant difference in the venous pressure in the legs when compared to lying down. The height of the individual determines the pressure; for an average adult, it is 8 mm Hg while they are laying down and 100 mm Hg when they are upright.
In order to evacuate the blood through the lymphatic system, venous stasis in venous insufficiency causes excessively high venous pressure (venous hypertension) and increased permeability of blood capillaries (capillary hyperpermeability). Since the lymphatic system is not as effective as an unimpaired circulatory system, swelling (edema) is evident, especially in the ankles and lower leg, even though it gradually drains extra fluid and proteins from the veins in the lower legs and transports them upward. An inflammatory reaction caused by the chronically elevated fluid in the lymphatic system and capillary hyperpermeability results in tissue fibrosis of the veins and lymphatic system as well as the opening of arteriovenous shunts, all of which exacerbate the condition in a vicious cycle.
Others:
Inactivity is another common cause of water retention in the legs. Exercise may improve the leg veins’ ability to defy gravity and pump blood back to the heart. If blood flows too slowly and starts to pool in the leg veins, too much fluid may be driven out of the capillaries in the legs and into the tissue spaces. Capillaries may burst, causing tiny blood spots to show beneath the surface. Veins themselves may be impacted by varicose veins, a condition that causes swelling, discomfort, and distortion. Muscle movement not only keeps the blood flowing through the veins but also aids the lymphatic system in carrying out its “overflow” function.
Long-term bed rest, lengthy travel, mobility-impairing conditions, etc., can all lead to water retention. Simple exercises like rotating your ankles and wriggling your toes will help reduce it.
Water retention is a common side effect of some drugs. These include beta-blockers, non-steroidal anti-inflammatory drugs, and estrogens, which also include hormone replacement therapy (HRT) drugs and oral contraceptives like the pill.
Pregnancy
Long-term bed rest, lengthy travel, mobility-impairing conditions, etc., can all lead to water retention. Simple exercises like rotating your ankles and wriggling your toes will help reduce it.
One of the most frequent adverse effects of several medications is water retention. Among these are estrogens, which also include oral contraceptives such as the pill or hormone replacement therapy. in addition to beta-blockers and non-steroidal anti-inflammatory drugs.
Because pregnant hormones encourage fluid retention, the body retains more water and salt than usual. The lower limbs, hands, feet, and face may swell.
Eclampsia, or elevated blood pressure that develops during pregnancy, can also cause edema. Bloating and breast discomfort are common symptoms of premenstrual water retention.
Conditions affecting the brain
Some causes of brain enlargement include the following:
- Head injuries: Fluid accumulation inside the brain may result from a head injury.
- Brain enlargement can result from severe strokes.
- Brain tumors: A brain tumor will produce a buildup of water around it as it develops new blood vessels.
Allergies
Edema of the face or skin can occur in those who are allergic to or sensitive to particular foods and insect bites. Severe swelling is one of the signs of anaphylaxis.
Swelling of the throat can obstruct the airway, making breathing impossible. There is a medical emergency.
Issues involving the extremities
Some causes of edema in the extremities include the following:
- Any obstruction, including a blood clot in a vein, can halt the flow of blood. When venous pressure increases, fluid leaks into the surrounding tissue, resulting in edema.
- Broken valves are frequently the cause of varicose veins. As internal pressure increases, veins start to expand.
- Furthermore, the pressure increases the possibility of fluids leaking into nearby tissue.
- Any bulge that presses up against a lymphatic duct or vein, whether it be a tumor, growth, or cyst, can cause edema. As pressure rises, fluids may leak into the surrounding tissue.
- When there is lymphedema, the lymphatic system helps to drain excess fluid from the tissues. Any disruption to this system, such from a tumor, an infection, or surgery, might result in edema.
Miscellaneous conditions
Other possible reasons for edema include:
- Long-term inactivity: Skin edema can develop in those who are not active for an extended period of time. Both fluid buildup in gravity-sensitive areas and the pituitary’s release of the antidiuretic hormone may cause this.
- High altitude: When combined with physical exertion, this may increase the risk of edema. Acute mountain illness can cause high-altitude brain edema or high-altitude pulmonary edema.
- Burns and sunburns: Burns cause the skin to retain moisture. Localized edema is the effect of this.
- In any tissue, swelling is a typical sign of inflammation or infection. This is usually most noticeable on the skin. The skin is typically where this is most obvious.
- Menstruation: Throughout the menstrual cycle, hormone levels change. In the days preceding menstruation, progesterone levels are decreased, which may cause fluid retention.
- Birth control pills: Any medication that contains estrogen has the potential to cause fluid retention. When people first start taking birth control tablets, they frequently gain weight.
- Menopause: Fluid retention may be caused by hormonal changes that occur during this time. Additionally, hormone replacement therapy may cause edema.
- Thyroid disease: Edema can result from hormonal abnormalities linked to thyroid issues.
Due to hydrostatic pressure
By increasing the hydrostatic pressure inside the blood artery, modifications to the variables in Starling’s equation can result in the development of edemas. enhancing the vessel wall’s permeability or reducing the oncotic pressure inside the blood vessel.
The latter yields two outcomes. By making it easier for proteins to exit the vessel, it increases water flow and reduces the colloidal or oncotic pressure differential.
Another blood vessel system called the lymphatic system acts as a “overflow” and has the capacity to return a sizable volume of excess fluid to the bloodstream. Even the lymphatic system, though, has its limitations. either the lymphatic system is blocked or there is simply too much fluid. Legs, ankles, feet, belly, or any other part of the body will enlarge as a result of the fluid remaining in the tissues.
Risk factors for edema:
- Edema is primarily caused by infections, but there are other variables that can raise your risk of getting it.
- Mild edema can result from a bad diet, particularly one that contains excessive amounts of salt. Additionally, a poor diet can exacerbate edema when paired with other illnesses.
- Low protein consumption combined with malnutrition can also result in hypoalbuminemia, which can cause edema.
- Edema can also result from prolonged standing and sitting, particularly during hot weather. Pregnancy and obesity are also linked to an increased incidence of edema.
- You may be more susceptible to edema if you have other medical issues. For instance, damaged or varicose veins in your legs may cause edema. Any procedure that removes lymph nodes has the potential to cause edema, depending on the site. Lymphedema is the term for this type of edema.
Types of Edema:
- Peripheral edema. Though it can also occur in the arms, this typically affects the legs, feet, and ankles. It can indicate issues with your kidneys, lymph nodes, or circulatory system.
- Pedal edema. This occurs when fluid builds up in your lower legs and feet. Pregnant women and older people are more likely to experience it. You can have less sensation in your feet, which might make it more difficult to move around.
- lymphedema. The most common cause of this swelling in the arms and legs is injury to the lymph nodes, which are tissues that aid in the removal of waste and pathogens from the body. Radiation and surgery used to treat cancer may be the cause of the harm. Additionally, the cancer itself may obstruct lymph nodes and cause fluid accumulation.
- Pulmonary edema. Pulmonary edema occurs when fluid builds up in the lungs’ air sacs. Breathing becomes difficult as a result, and it gets worse when you lie down. You might cough up a foamy spittle, occasionally including blood, feel smothered, and have a rapid heartbeat. If it occurs unexpectedly, dial 911.
- Cerebral edema. Fluid accumulates in the brain in this extremely dangerous illness. A severe blow to the head, a clogged or broken blood artery, a tumor, or an allergic reaction can all cause it.
- Macular edema. This occurs when fluid accumulates in the macula, a region in the middle of the retina, the tissue in the back of the eye that is sensitive to light. It occurs when fluid seeps into the retina from damaged blood vessels.
Diagnosis of Edema:
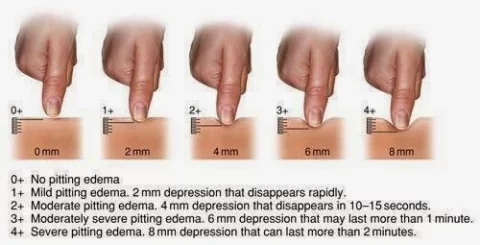
Grading of edema:
- Absent: Absent
- Mild: Both feet/ankles
- Moderate: Both feet,
plus lower legs,
hands or lower arms - Severe: Generalised
bilateral pitting edema,
including both feet,
legs, arms, and face.
Pitting and non-pitting edema
Pitting edema and non-pitting edema are the two primary types of edema. When pressure is applied to a small area and then released, an indentation is left behind, which is known as pitting edema. Water retention causes the most common type of peripheral pitting edema, as shown in the figure. In addition to systemic ailments and pregnancy in some women, it can be caused directly or indirectly by heart failure. Local illnesses including varicose veins, thrombophlebitis, insect stings, and dermatitis can also cause it.
Non-pitting edema is observed when the indentation disappears. It is associated with conditions including myxedema, lipedema, and lymphedema.
Edema caused by malnutrition is known as kwashiorkor, an acute form of childhood protein-energy malnutrition that manifests as edema, irritability, anorexia, ulcerating dermatoses, and an enlarged liver with fatty infiltrates.


Assessment of Oedema:
History – Should include:
- When did the edema start to occur? Acute compartment syndrome from trauma, cellulitis, ruptured popliteal cysts, deep vein thrombosis (DVT), or recent introduction of calcium channel blockers are more likely to cause acute swelling of a leg lasting less than 72 hours. The development or worsening of long-term systemic diseases such hepatic, renal, or congestive heart failure (CHF) is the cause of the persistent buildup of more widespread edema.
- Edema variations with position
- DVT, venous insufficiency, tumor-induced venous obstruction (such as iliac vein tumor obstruction), lymphatic obstruction (such as from a pelvic tumor or lymphoma), or lymphatic destruction (such as congenital vs. secondary from a tumor, radiation, or filariasis) can all cause unilateral edema. A systemic cause, such as CHF (particularly right-sided), pulmonary hypertension, chronic renal or hepatic illness (which results in hypoalbuminemia), protein-losing enteropathies, or severe malnutrition, may be the cause of bilateral or widespread swelling.
- Evaluation of systemic illnesses and medication history.
Physical Examination:
- Pitting, soreness, skin changes, and temperature are assessed during a physical examination.
- Pitting: Pitting and non-pitting edema are the two forms of edema. An indentation that persists in the edematous area following pressure application is known as pitting edema. Treatment response determines its location, time, and extent. It is mostly evaluated on the dorsum of the foot, the bony part of the tibia, and the medial malleolus. Myxedema, lipedema, and lymphoedema all exhibit non-pitting edema.
- Tenderness: Reflex sympathetic dystrophy, also known as complicated regional pain syndrome type 1, and DVT are linked to pain on palpation across the edematous area.On the other hand, palpating lymphoedema usually does not cause any pain.
- Alteration in skin temperature, color, and texture: Acute DVT and cellulitis are linked to warmth in the edematous region. Notable symptoms include redness, shiny skin, and ulcers. Venous insufficiency is characterized by yellow-brown hemosiderin accumulation.
Methods of Assess Oedema:
The following instruments are most frequently used to measure edema:
- Volume measurements (with a water volumeter)
- Girth measurements (with a tape measure).
- Pitting edema assessment.
Water Displacement ( Volume measurements)
The volumeter:
- Glisson introduced it to medicine in 1622.
- makes use of the same water displacement concept that was initially identified by the Greek mathematician Archimedes.
- This principle states that the volume of water displaced is equal to the volume of the item submerged in the water.
- Water is poured into a 13 x 5 x 9-inch clear acrylic rectangular box with a spout on one of the short sides until water shoots out of the spout.
- The patient places one foot in the volumeter once the water level is steady, and the displaced water is measured in a graduated cylinder. The volume of the foot, ankle, or hand is equal to the amount of water displaced in milliliters.
- The participant’s hand is inserted slowly into the volumeter with the forearm pronated, fingers adducted, and thumb facing the spout until the web of the middle and ring fingers rests on the stop dowel of the volumeter. The ankle can be tested using either sitting or standing, with the knees 90 degrees in the sitting position and the foot flat in the volumeter’s base.
Advantage: It is the most reliable instrument for determining edema.
Disadvantages: In a clinical context, these approaches have a number of drawbacks.
- Because the water level must be steady, it must be set up several minutes prior to the test, which takes time.
- Once filled with water, it becomes difficult to move.
- It calls for specific equipment.
- It is undesirable for some patient populations since it is untidy and requires the patients to submerge their hands in water.
Girth measurements (with a tape measure)
Circumferential Method
Among the methods for measuring girth is the circumferential method. Each lower or upper extremity is identified by a semi-permanent marking at a certain location in relation to the bony prominences for consistent measurements.
Figure-of-Eight method
It is among the methods for measuring girth as well. Because it covers a larger region, it is more dependable than the circumferential technique. When measuring edema, a tension-controlled measuring tape is better than regular tape since it may be wrapped around the hand, foot, or ankle. When it comes to hand and ankle swelling, the figure of eight approach is typically recommended. For consistency, it makes its own unique points.
Pitting edema
Evaluation: Firmly press each extremity with your thumb for at least two seconds.
- above the foot’s dorsum
- Behind the malleolus medialis
- Above the medial malleolus in the lower calf
The depth of the pit and the recovery time the amount of time it takes for the skin to return to its pre-injury state are noted.
Pit depth (visually evaluated) and recovery time are used to grade edema from grade 0 to 4. The severity is rated using the scale, and the results are as follows:
- Grade 0: No edema in the body
- Grade 1: Minor pitting (2 mm depth) that instantly bounces back and shows no signs of deformation.
- Grade 2: Rebounds in less than 15 seconds, with a slightly deeper pit (4 mm) and no obvious distortion.
- Grade 3: The dependent extremity is full and bloated, with a noticeable deep pit (6 mm) that takes up to 30 seconds to recover.
- Grade 4: The dependent extremity is severely deformed and takes more than 30 seconds to recover from a very deep pit (8 mm).
Treatment of edema:
- The face of a man was swollen.
- edema of the face caused by venous obstruction during sleep.
- The same person who has no facial edema
- After being upright all day, the swelling subsides.
- The underlying problem is typically addressed as part of treatment. Diuretics are commonly used to treat heart or kidney problems.
During treatment, the affected body parts may need to be positioned to improve drainage. For example, sitting with the feet raised on cushions or reclining down in bed may help reduce ankle or foot swelling. Intermittent pneumatic compression can be used to pressurize tissue in a limb, causing fluids such as lymph and blood to drain from the compressed area.
Complications of edema:
If edema is not addressed, it may cause:
- Itchy, stretched skin infection at the area of edema and scarring between tissue layers with inadequate blood flow reduction in joint, artery, and vein suppleness uncomfortable edema with increasing stiffness, discomfort, and difficulty walking.
- Ulcerations on the skin.
- An underlying ailment needs to be treated to prevent it from getting worse.
Prevention:
Compression stockings help reduce swelling and pain associated with edema.
A few self-care techniques can help reduce or prevent edema.
These consist of:
- Reducing salt intake, losing weight if needed, exercising frequently, raising the legs to increase circulation, wearing support stockings bought online, avoiding extended standing or sitting, getting up and moving around a lot when traveling, and avoiding hot baths, showers, and saunas.
- When it’s cold, wearing warm clothes
A physical therapist or massage therapist may help remove the fluid by using strong strokes toward the heart. The use of oxygen may be beneficial for certain types of edema. For example, a person with cardiogenic pulmonary edema may need extra oxygen if they have problems receiving enough of it.
According to an earlier 2004 study, oxygen delivered via the nose may improve vision impairment caused by diabetic macular edema. However, a particular study suggests that hyperbaric oxygen therapy may raise the risk of pulmonary edema.
Prognosis:
If you have swelling or edema in your body, it’s critical that you see your doctor. Your skin may become stretched by edema, which could worsen and lead to major health issues if left untreated.
Depending on what causes it, edema may be a temporary or permanent condition. You can make easy lifestyle adjustments to lessen swelling and fluid accumulation in your body, or you can get treatment to help manage any underlying illnesses that may be the cause of your edema.
When is edema an emergency?
Even though edema symptoms usually go away with rest and at-home care, they can indicate more serious health issues such renal or heart failure.
In more specific cases, breathing difficulties may be a sign of pulmonary edema, therefore you should get medical help immediately. Additionally, if you get abrupt edema during pregnancy, let your doctor know immediately since it may be a sign of problems.
Summary
Each person with edema has a different etiology, which affects how severe their condition is. If you are pregnant, it is normal to experience swelling as your due date draws near. You might have mild edema, which normally resolves on its own. There are options for therapy and medication if your disease is more severe.
Make an appointment for a check-up with your physician if you notice unexpected swelling in a particular area of your body and you are not pregnant. Early identification and treatment of any underlying medical condition that edema may be a sign of may lead to the best prognosis.
FAQs
What is the best oil for edema?
Extra virgin olive oil is applied topically to the skin of the foot and ankle to alleviate edema. The best benefits are obtained when 5–15 milliliters of extra virgin olive oil are applied topically.
What is the edema water pill?
Furosemide is a member of the class of medications known as loop diuretics, or water pills. Furosemide is used to treat swelling caused by congestive heart failure, liver disease, renal disease, and other illnesses, as well as fluid retention (edema).
What is the duration of edema?
Edema may be either transient or permanent, depending on the reason for your diagnosis. Usually, swelling subsides after a few days. Your swelling will be at its worst during the first two days and should begin to go down by the third day.
Can edema be lessened by bananas?
Potassium may assist reduce edema that is caused by an excess of salt. Therefore, eating bananas may help minimize foot swelling and the amount of extra fluid in your body.
What is edema’s first line of treatment?
Pregnancy, heart failure, liver failure, renal failure, or trauma can all cause the illness in younger people. Loop diuretics are typically the first drug prescribed by a physician when treating edema directly.
Does consuming water help those with edema?
Drink at least eight glasses of water each day to help eliminate edema if you are experiencing it. Avoiding alcohol is also a smart idea. This is due to the fact that alcohol tends to dehydrate the body, which makes your body eliminate fluids from the blood more quickly than it would otherwise.
What is the best fruit for edema?
To lessen edema, concentrate on including foods high in water, such as cucumbers and melons, as well as foods high in potassium, such as sweet potatoes and bananas. Remember the health advantages of fish’s omega-3 fatty acids and the anti-inflammatory qualities of spices like ginger and turmeric.
Is edema dangerous?
Edema can occur in one area of the body, be a mild and benign water retention issue that resolves on its own, be a sign of a serious illness that requires medical attention, or develop into a chronic and severe condition (such as lymphedema following cancer treatment or edema in one leg after deep vein thrombosis).
Does increasing water intake lessen edema?
The medical term for swelling is edema, and it may just affect one foot. It is possible to minimize edema by implementing effective techniques. Drinking plenty of water, elevating the feet frequently, and reducing salt intake can all help manage swollen feet.
Is it possible to cure edema?
The only way to treat edema is to address the underlying issue. Your doctor might prescribe a drug called a diuretic. Another name for this is a water tablet. These medications aid in the body’s urine-based removal of excess fluid and salt.
Are leg edemas permanent?
You can still take steps to reduce swelling, ease discomfort, and postpone some of the long-term damage that edema may cause, even if some types of it may be irreversible. Depending on the underlying cause, missing edema treatment can have different outcomes.
How is edema measured?
The most common techniques for measuring edema are as follows: Measurements of volume (with a water volumeter)
(A tape measure is used.) Girth measurements.
The length and depth of the depression are used to evaluate the pitting edema.
Is it possible to cure edema?
The only way to treat edema is to address the underlying issue. Your doctor might prescribe a drug called a diuretic. Another name for this is a water tablet. These medications aid in the body’s urine-based removal of excess fluid and salt.
Does walking help with edema?
Over the course of the day, edema and leg pain can be reduced with the use of walking and elastic stockings.
How can I naturally lessen edema?
Home treatments that are healthy
Put pressure on: If the arm or leg is affected by edema, using gloves, sleeves, or compression stockings may help.
transfer: It may be beneficial to transfer fluid back towards the heart by using the muscles in the swollen area of the body, especially the legs.
Lift the leg.
Protect, massage, and so on
Reduce the amount of salt you eat.
Is edema a dangerous illness?
Receive medical help immediately if your edema suddenly gets worse, is unpleasant, or appears for the first time. You should also seek help if you have breathing problems or chest pain. The latter could be a sign of pulmonary edema, a serious condition in which the lung cavities fill with fluid.
References
- Parmar, D. (2023, December 13). Edema – cause, symptoms, treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/edema/
- Edema. (2025, February 18). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12564-edema
- Wikipedia contributors. (2025, February 3). Edema. Wikipedia. https://en.wikipedia.org/wiki/Edema
- Brazier, Y. (2023, November 13). Everything you need to know about edema. https://www.medicalnewstoday.com/articles/159111
- Heitz, D. (2023, December 21). What you should know about Edema. Healthline. https://www.healthline.com/health/edema





17 Comments