Patellar Retinaculum Injury
Introduction:
A patellar retinaculum injury occurs when the fibrous connective tissues that support and stabilize the patella (kneecap) and direct its movement inside the femoral groove are damaged or torn.
Maintaining appropriate patellar alignment during knee flexion and extension is largely dependent on these retinal structures, particularly the medial and lateral patellar retinacula. Pain, edema, instability, and reduced knee function can be caused by injury to the patellar retinaculum, which can be caused by trauma, overuse, or abrupt twisting motions.
Knee stability must be restored, and other problems must be avoided with prompt diagnosis and treatment.
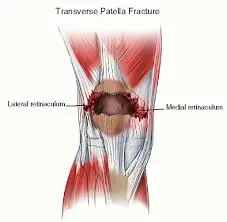
Anatomy of Patellar Retinaculum:
The patella is supported and stabilized on both sides by fibrous bands of connective tissue called the patellar retinaculum.
The medial femoral condyle, the surrounding soft tissues, and the medial edge of the patella are all included in the medial patellar retina. It is crucial for preventing the patella from moving laterally and contains fibers from the vastus medialis obliquus (VMO). It helps prevent medial patellar dislocation by containing fibers from the vastus lateralis and iliotibial band (ITB).
When combined, these components are essential for preserving patellar alignment, especially when the knee is moving. Dislocation, maltracking, or patellar instability can result from damage or imbalance in these retinacula.
Causes of Patellar Retinaculum Injury:
- Direct Trauma: The retinaculum may be overstretched or torn if a blow or fall strikes the knee directly.
- Patellar Dislocation or Subluxation: When the patella suddenly shifts, particularly laterally, the medial retinaculum is frequently harmed.
- Overuse or Repetitive Stress: Over time, activities that require a lot of knee bending, jumping, or twisting (like basketball or running) can put stress on the retinal tissues.
- Sudden Twisting Movements: The patellar stabilizers may be strained by abrupt direction changes made while the foot is planted.
- Muscle Imbalance: The retina may be under more stress if there is weakness or imbalance in the quadriceps muscles, especially between the vastus lateralis and VMO.
- Complications from surgery or injuries, Retinal strain, and changes in patellar kinematics can result from prior knee surgeries or injuries.
Symptoms of Patellar Retinaculum Injury:
- Kneecap pain, particularly when moving or applying pressure.
- Pain and swelling around the patella’s medial or lateral aspect.
- Abnormal patellar tracking or displacement that is felt or visible
- Bruising near the knee (where there has been severe trauma).
Diagnosis of Patellar Retinaculum Injury:
Imaging investigations and clinical examination are combined to diagnose a patellar retinaculum damage. Pain, edema, retinal tenderness, patellar alignment, and any indications of instability or irregular tracking during knee movement are all evaluated by the healthcare professional during the physical examination.
Retinal integrity and patellar stability may be assessed using specialized procedures, such as apprehension or patellar glide tests. While MRI is especially helpful for viewing soft tissue structures, such as the retinaculum, and detecting tears, inflammation, or related conditions, such as cartilage damage, X-rays can assist in ruling out fractures or dislocations.
Accurate diagnosis and suitable treatment planning are ensured by a comprehensive clinical and radiological evaluation.
Special Tests for Patellar Retinaculum Injury:
- Patellar Apprehension Test: Patellar instability is evaluated using the Patellar Apprehension Test. The patient is asked if they feel uncomfortable or uneasy as the examiner applies a lateral force to the patella while the knee is flexed. Patellar instability, which is frequently linked to retinal damage, may be indicated by a positive test result (the patient experiences pain or attempts to shield the knee).
- Patellar Grind Test: The patella’s mobility within the femoral groove is assessed by the patellar grind test. To look for evidence of aberrant patellar tracking or restricted motion, the examiner moves the patella laterally and medially. Abnormal tracking or limited gliding could indicate retinal injury.
These tests aid in confirming a diagnosis of patellar retinal injury when paired with imaging and clinical symptoms.
Treatment of Patellar Retinaculum Injury:
Medical Treatment:
Conservative methods are usually the first line of treatment for a patellar retinaculum damage, especially in mild to severe cases. In the early stages, R.I.C.E. (rest, ice, compression, and elevation) is crucial for minimizing pain and swelling. To manage pain and inflammation, doctors may prescribe nonsteroidal anti-inflammatory medications (NSAIDs).
To increase patellar stability and lessen stress on the retinaculum, physical therapy is essential to rehabilitation. It focuses on strengthening the quadriceps, especially the vastus medialis obliquus (VMO). Stretching exercises are also essential for improving flexibility and avoiding further injuries.
In more extreme situations, such as large tears or ongoing instability, surgery might be necessary to rebuild or repair the damaged retinal tissues. A systematic rehabilitation program is required following surgery in order to recover knee function and avoid recurrence.
Physical therapy Treatment:
Restoring knee stability, increasing strength, and minimizing pain are the main goals of physical therapy for patellar retinaculum injuries. To manage swelling and pain, the first phase usually consists of mild range-of-motion exercises and modalities like cold, heat, or ultrasound.
Strengthening the quadriceps, particularly the vastus medialis obliquus (VMO), is crucial as recovery advances to promote appropriate patellar tracking and lessen retinal stress. Stretching exercises that focus on the iliotibial band (ITB), hamstrings, and quadriceps help increase flexibility and avoid asymmetries. To guarantee good knee mechanics, functional exercises that replicate everyday tasks, like lunges or step-ups, are progressively added.
Bracing or taping techniques can be utilized to give extra support during movement in cases of chronic instability. Once the knee is stable and pain-free, proprioceptive training and sport-specific exercises may be part of advanced physical therapy interventions.
Prevention:
Proper movement skills, flexibility, and strengthening are all important in preventing patellar retinaculum injury. Reducing stress on the retinaculum and maintaining appropriate patellar alignment are two benefits of strengthening the quadriceps, especially the vastus medialis obliquus (VMO).
Frequent stretching of the iliotibial band (ITB), hamstrings, and quadriceps helps increase flexibility and avoid imbalances that could lead to injury. To prepare the knee joint for movement and lessen the strain on the soft tissues, it is essential to do proper warm-up and cool-down exercises both before and after physical activity.
Injury risk can also be reduced by avoiding sudden, high-impact activities without enough planning and by wearing appropriate footwear that promotes healthy knee alignment. Using knee braces or taping techniques during high-risk activities can offer additional support and lower the risk of injury if there is a history of knee instability.
Complications:
If patellar retinaculum injury is not addressed or if rehabilitation is not sufficient, complications may develop. Patellar instability, in which the kneecap does not track correctly, is a frequent problem that causes frequent dislocations or subluxations. This instability may cause persistent pain and make it difficult to perform weight-bearing or knee-bending movements.
In certain situations, poor alignment or insufficient healing may result in ongoing pain and edema. Over time, there is also a chance of developing arthritis or cartilage damage in the knee joint, particularly if the retinal injury results in aberrant patellar movement.
Complications include infection, inadequate healing, or retinal tears that may arise if surgical treatment is necessary. Furthermore, inadequate post-operative rehabilitation may result in a failure to restore complete knee strength or function, which may contribute to chronic instability.
Prognosis:
The degree of the injury and the efficacy of treatment have a significant impact on the prognosis of patellar retinaculum injury. The prognosis is usually good in mild to moderate cases, and most people may resume their regular activities in a few weeks to months with the right conservative management, which includes rest, physical therapy, and strengthening exercises.
However, recuperation can take longer, usually a few months to a year, and surgery may be required in situations of significant injuries, chronic instability, or failed conservative treatment. If rehabilitation is actively followed after surgery and knee strength and stability are restored, the prognosis is also favorable.
Long-term consequences may be impacted by complications, including chronic instability or cartilage damage. All things considered, the likelihood of a full recovery and return to normal activities is greatly increased by early diagnosis, appropriate treatment, and commitment to rehabilitation regimens.
Conclusion:
To sum up, patellar retinaculum damage is a disorder that can have a major effect on knee function and stability. This injury can result in pain, edema, and, if ignored, long-term problems such as patellar instability or cartilage damage, regardless of whether it was caused by direct trauma, overuse, or muscle imbalances.
A good recovery depends on early diagnosis and effective treatment, which may include physical therapy or surgery if needed. The likelihood of such injuries can be decreased by prevention through strengthening, flexibility, and appropriate movement practices.
Most people can restore full knee function and resume their normal activities with the correct care, which lessens the effect of the injury on their day-to-day activities.
FAQs
How is a sprain of the medial patellar retina treated?
Treatments for joint swelling should include rest, NSAIDs (non-steroidal anti-inflammatory drugs), and ice. When recuperating from MPFL injuries, physical treatment is frequently beneficial. The patient’s functional recovery will be facilitated by physical therapy exercises that strengthen the weak knee.
How long does it take to heal from a tear in the patellar retina?
Recovery from a partial tear may take a few weeks to many months. Physical therapy, anti-inflammatory drugs, and immobilization all aid in this. After a patellar tendon tear, it takes about six months to fully recover.
Why does retinal pain occur?
Due to the flexor retinaculum’s limited range of motion, anything that occupies space in the tarsal tunnel may cause the area’s pressure to rise. Swollen varicose veins, a noncancerous tumor on the tibial nerve, and edema caused by other conditions like diabetes can all cause this.
Is it possible to damage your retinaculum?
Chronic tendon subluxation may result from harm or injury to the retinaculum, the tissues that support the tendons.
How much time does it take for the retina to heal?
In order for the retinaculum and any bone treatments to heal, recovery from surgery necessitates a somewhat extended period of immobilization, often ranging from two to six weeks.
What role does the retinaculum play in the knee?
This supports the study’s conclusion that the retinaculum is a robust, rigid structure that is positioned to withstand patellar medial movement. As a result, it is designed to serve as a patella static stabilizer.
Can the retina regenerate itself?
These tears must be recognized in order to start the appropriate treatment because they frequently do not heal well on their own.
Is a ligament the patellar retinaculum?
According to imaging studies and macroscopy, PFLs and retinacula are distinct structures. Compared to ligaments, the retinacula have more nerve fibers and elastic fibers in response to their particular purpose.
What is a tear in the retinaculum?
This weakens the sling, which results in instability and pain in the back and inside edge of the ankle and foot, particularly when lifting weights or doing forceful movements like sprinting and leaping.
How is damage to the lateral patellar retina treated?
Avoiding painful movements like jogging and leaping is the first step in treatment. Both non-surgical and surgical approaches are available as treatment alternatives. The RICE protocol—rest, ice, compression, and elevation—is a non-surgical treatment that helps manage pain and swelling.
How long does it take for a tear in the medial patellar retina to heal?
In addition to reducing edema, bracing the joint may assist stabilize the patella. A complete recovery is anticipated in 8–12 weeks after physical treatment is suggested.
References
- Ji, G., Wang, F., Zhang, Y., Chen, B., Ma, L., & Dong, J. (2012). Medial patella retinaculum plasty for treatment of habitual patellar dislocation in adolescents. International Orthopaedics, 36(9), 1819–1825. https://doi.org/10.1007/s00264-012-1544-3
- Hacking, C., & Moodaley, P. (2017b). Medial patellar retinaculum. Radiopaedia.org. https://doi.org/10.53347/rid-54736