Calf Strain
What is Calf Strain?
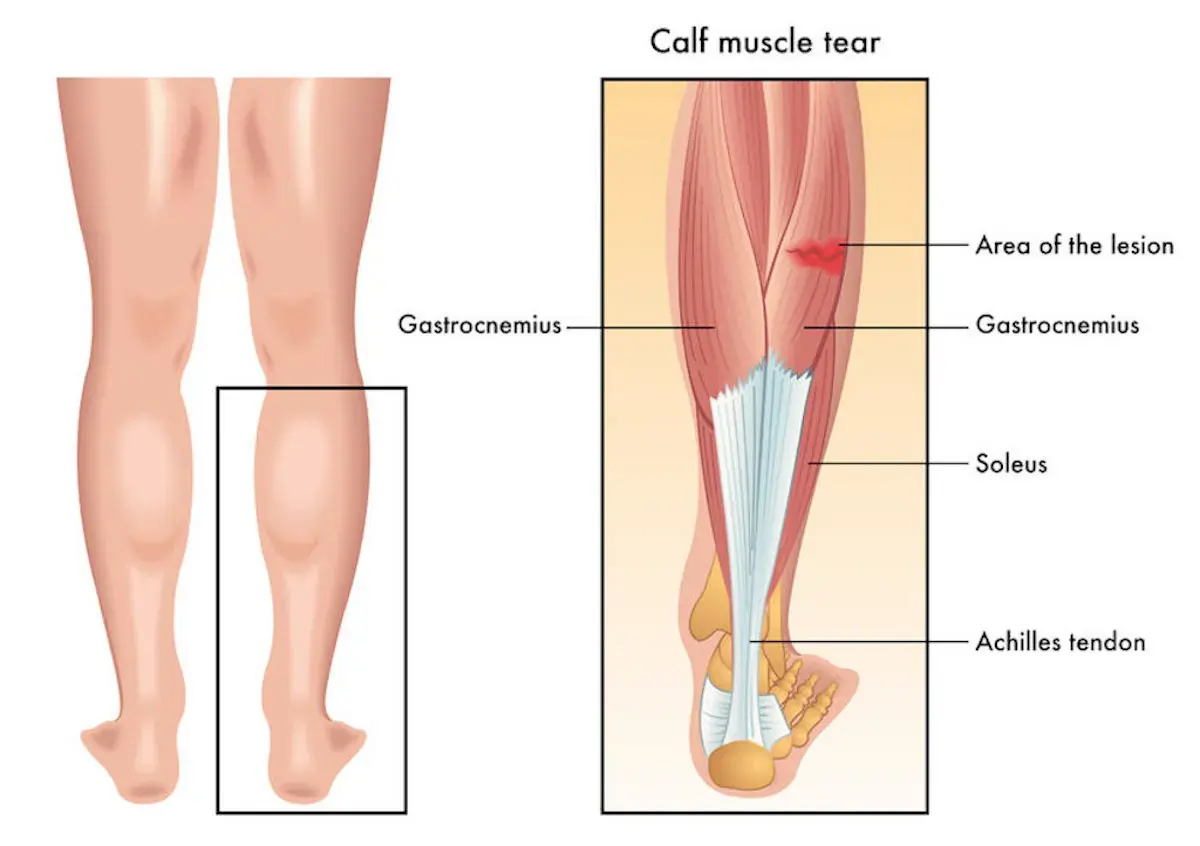
A calf strain, also known as a pulled calf muscle, is an injury to the muscles in the back of your lower leg. The gastrocnemius and soleus are the two primary muscles that make up this region, which is known as the calf.
These muscles work together to help you point your toes (plantar flexion) and flex your foot upward (dorsiflexion). It occurs when these muscles are overstretched or torn, often during sudden movements, sports activities, or intense physical exertion.
Calf strains can vary in severity from mild discomfort to significant pain and limited mobility. Common symptoms include sharp pain, swelling, and difficulty walking or bearing weight on the affected leg. Prompt treatment and proper rehabilitation are essential to prevent further injury and ensure a full recovery.
- Additional potential reasons for calf pain might be Achilles tendon ruptures or tendon injury, such as Achilles tendinopathy.
- The lower leg is a crucial biomechanical component of locomotion, particularly when explosive force and endurance are required for a particular activity. Injuries in this area affect athletes in a variety of sports. Sports featuring fast running, higher running loads, acceleration, and deceleration, as well as strenuous play or performance circumstances, are popular places for calf muscle strain injuries (CMSI).
- A calf strain is a frequent muscle injury that can lead to further injury and a longer recovery period if improperly treated. The gastrocnemius muscle, a diarthrodial muscle that spans the knee and ankle, is more prone to damage.
Clinically Relevant Anatomy of Calf Strain:
It is composed of three muscles:
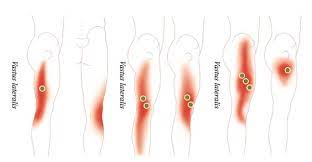
- Gastrocnemius: The majority of the calf is formed by this bigger, superficial muscle. It has two heads, a medial (inner) head and a lateral (outer) head. The medial head is most commonly injured in calf strains.
- Soleus: Behind the gastrocnemius is this deeper muscle. It is responsible for plantar flexion (pointing your toes downward) and helps with stability during standing and walking.
- plantaris: The rear of the lower thigh is home to this little, slender muscle. It plays a minor role in ankle movement and is not commonly injured in calf strains.
Epidemiology and Causes of Calf Strain:
- These long, biarticular muscles are more likely to fatigue during sports like sprinting because they must withstand strong internal stresses and quick changes in muscle length and contraction mode.
- However, studies have also demonstrated that calf muscle strains, such as ballet dancers, can occur from routine everyday activities and slow-lengthening muscular movements.
- Many sports activities, including dancing, football, soccer, tennis, and athletics, can strain calf muscles.
Who gets pulled calf muscles?
- A strained calf muscle can happen to anyone. However, athletes who frequently execute stop-and-go maneuvers with rapid bursts of speed are more likely to sustain these strains. This can occur in football, soccer, tennis, and running athletes.
- A strained calf muscle can occur in football, soccer, tennis, and running athletes.
- Age: An increased risk of strains during physical exercise may exist in individuals over 40.
Sex: Research has found that males are more prone than women to get calf muscle injuries.
Lack of conditioning: Before engaging in any physical activity, it’s critical to warm up, stretch, and condition your muscles in preparation for the start of a sports season. - Muscle quality: People with tight calf muscles are at high risk of calf injuries.
Characteristics of calf strain:
- Differentiating between different muscle strains in the calf complex is essential for creating an appropriate treatment plan, estimating the likelihood of recovery, and avoiding more injuries.
- The patient usually reports feeling as though they’ve been kicked in the rear of their leg or hearing a “pop” in the medial side of their posterior calf. I feel a stab of agony in my calf. Usually, there is substantial discomfort and edema for the next 24 hours.
Gastrocnemius strain:
- An eccentric strain on the gastrocnemius muscle tears its medial head when the knee is stretched and the ankle is dorsiflexed. The muscle known as the gastrocnemius tears when it tries to contract after growing.
- Subjective complaints of sudden, severe pain or tearing sensation at the back of the lower thigh, typically in the gastrocnemius’ medial belly or at the musculotendinous junction, are among the symptoms of gastrocnemius strain.
- On objective assessment there will be:
- sensitivity to touch where the damage is
- Swelling
- It might take several hours or days for bruises to appear.
- Muscle stretches will result in pain.
- When resisting plantarflexion, pain
- The most frequent soleus muscle injury is caused by a strain at the proximal medial musculotendinous junction. Less frequently than gastrocnemius injuries occur in the soleus. In addition, compared to gastrocnemius injuries, soleus strains typically manifest clinically as subacute injuries rather than as severe ones. Middle-aged patients who are physically active or in bad shape are often the ones who suffer from this ailment.
- In addition to the same symptoms as a gastrocnemius strain, the patient may also experience deeper and farther-reaching discomfort. Soleus muscle injuries may go unreported because soleus strains are sometimes confused with gastrocnemius strains or misdiagnosed as thrombophlebitis. When the Achilles tendon is squeezed, either 4 cm above the heel bone or further up in the calf muscle, it causes pain, known as a soleus strain. It might also occur if the calf muscle is contracted. Stretching the tendon and taking little steps might make the pain worse.
Plantaris strains:
- Although plantar traverses the knee and ankle joints as well, it is generally thought to be skeletal and is not frequently linked to calf strains. Injuries to the gastrocnemius and soleus muscles also show clinical signs, much as injuries to the plantar muscles.
- The person may be able to resume exercising while experiencing some soreness and stiffness during or after exercise, depending on the severity of the injury. In cases when injuries are more serious, it is easier to remember the precise mechanism of harm, and the person may be unable to move because of excruciating pain.
Grading of calf strains:
- There are three grades for muscle strains: I, II, and III. Grade III is the most serious.
Grade 1:
Symptoms:
- Sharp soreness during or after physical activity that may seem confined
- May be able to carry on with activities in the absence of pain or only minor discomfort
- stiffness and soreness following exercise
Signs:
- One-sided calf lift
- Unable to continue the activity
- severe discomfort after walking
- maybe swollen in the muscles
- There could be mild to moderate bruising.
Grade 2:
Symptoms:
- Soreness during or after physical activity that may seen as confined
- May be able to carry on with activities in the absence of pain or only minor discomfort
- Stiffness and soreness during exercise
- Unable to carry weight during exercise
Signs:
- discomfort when plantarflexion is engaged
- weakness and agony with resistant
- plantarflexion
- Loss of dorsiflexion
- Bilateral calf raise pain
Average time to return to sport:
- 16 – 21 days
Grade 3:
Symptoms:
- acute, sudden discomfort in the calf, usually at the musculotendinous junction
- unable to carry out the activity
- may show up with a lot of swelling and bruises.
- hours after the injury
Signs:
- unable to tighten the calf muscle
possibly a noticeable flaw - Positive results for Thomson’s test
Average time to return to sport:
- 6 months after surgery
Differential Diagnosis of calf strain:
- Achilles tendinopathy
- Plantar fasciopathy
- The following section discusses additional sports-related lower limb injuries that are comparable to calf strains in terms of symptoms and management.
- CECS stands for chronic exertional compartment syndrome. CECS starts as moderate pain while exercising and may go away thereafter. Later phases are characterized by earlier onset, increased discomfort, longer duration, and the need to stop activity. Common complaints include leg cramps, paraesthesia, numbness, and weakness. Exercise-induced increases in intramuscular blood flow lead to compartmental pressure, capillary compression, and ischemia, which is the etiology of CECS.
- Syndrome of Popliteal Artery Entrapment (PAES). The compression of an artery between a contracting muscle and the underlying bone, which usually happens during forceful ankle plantarflexion, results in functional PAES.
- Baker’s cyst
Assessment of calf strain:
- A thorough medical history and a subjective evaluation are acquired at the initial examination stage.
Objective assessment:
- Ankle and foot examinations while standing and in a supine posture
- AROM of ankle
- PROM of ankle
- Calf palpation and reiteration of the symptoms
- knee AROM and evaluating resistance
Imaging:
- Ultrasound (US) is considered the gold standard. Additionally, it can be used to rule out other conditions such as burst Baker’s cysts and deep vein thrombosis as well as assess the severity and scope of the muscle lesion.
- Because they require sudden direction changes and rapid speeds, running, volleyball, and tennis are the sports that cause calf muscle breaks down the most frequently. The grades for strained muscles are I through III. Common symptoms include stiffness, discoloration, and bruises around the strained muscle.
- Grade I: The most frequent and least serious kind of injury is a first-degree or light injury. In one to three weeks, sports would likely resume.
- Grade II: A partial muscle tear that prevents movement is considered second-degree or moderate damage. There is an observable loss in strength and range of motion, with noticeable bruising, swelling, and agony. Muscle fiber disruption can vary from 10% to 50%. After three to six weeks of recuperation, patients can return to their regular exercise routine.
- Grade III: Hemostases usually accompany third-degree or severe injuries that result in a complete rupture of the muscle. Bruising, soreness, edema, and pain are frequently experienced. Recovery is extremely individualized and may take months before you are completely healed and can resume your normal activities.
- This may happen with or without bleeding. The measurement of fluid collection provides information regarding the lesion’s extent. Regardless of whether there is a partial or whole rupture, the distance between the two muscles can be used to determine the extent of the injury. Axial US scans are the most useful in differentiating between partial and complete rupture because they can display the entire muscular belly in a single picture.
Treatment of calf strain:
- For calf strains, surgery is typically not necessary, but in the event of a total rupture, it could be.
- Conservative management includes:
- Management of soft tissue injuries
Steroid injection
Physiotherapy
It is imperative to remove any hematoma as soon as possible to prevent complications like myositis ossificans. - If the damage is more serious, using a temporary heel pad may help shorten the calf muscle and release stress while the injury heals. To prevent an imbalance in your gait, it might be wise to place heel pads in both shoes.
Physical Treatment of Calf Strain:
- RICE therapy, which stands for RICE calf muscles, is usually used immediately.
- Rest: To avoid more calf damage, stop running or engaging in other physical activity.
- Ice: For the first 48 hours following the injury, use an ice pack or cold compress to minimize swelling. This should be done for 20 to 30 minutes every 3 to 4 hours till the swelling goes down, as soon as possible after the accident.
- Compression: Wrapping or applying a compression bandage to the damaged area will help to reduce edema and fluid accumulation.
- Elevation: Lift your leg so that it is higher than your heart, if possible. To support your leg down, use pillows, blankets, or cushions.
- RICE can be administered at home, but it’s a good idea to ask your doctor if there are any specific instructions.
Avoid:
- putting heat on the damaged region.
- consuming alcoholic beverages.
- giving the calf a massage.
- strolling or engaging in physical exercise.
- After diagnosing your injury, your healthcare professional could suggest further therapies like:
- Pain relievers.
- Cover your lower leg with a soft cast or boot to keep it from shifting.
- Rest and giving the injury enough time to heal are the main treatments for calf strains, although, in more serious situations, surgery may be required.
- Dynamic stretches in the flexed (soleus) and straightened (gastrocnemius) knee positions can be used in place of mild passive stretching until the calf muscles are completely stretched without causing pain.
Initial treatment aims:
- to limit bleeding
- pain
- prevent complications.
- Protocols for managing soft tissue injuries are to be initiated as soon as the damage happens. The concepts of LOVE and PEACE are to be followed.
- Maintaining plantarflexion range of motion requires mild passive stretching activities that don’t cause pain. Later on, after the inflammation has subsided, stretching the muscles with a low load while wearing surface heat increases muscle elasticity.
- It is recommended to perform isotonic exercises for the antagonist’s tibialis anterior and peroneal in addition to light treatments for the injured muscle. In the initial days after an injury, light activity within pain tolerance will aid in promoting recovery
- To ensure a complete recovery, the calf muscles should be gradually loaded and strengthened through workouts. Your recovery will happen more quickly the sooner you begin loading exercises. Before fully returning to sport, plyometric workouts and a return to sport should be started.
- Long-lasting discomfort may result from strains, even with prompt and effective treatment. The effectiveness of the treatment is determined by the calf muscle’s ability to be completely stretched, the recovery of strength, the knee and ankle range of motion being normal, and the absence of any noticeable discomfort.
Outcome Measures of calf strain:
Additional physiotherapy techniques include:
- LEFS: Lower Extremity Functional Scale
- VAS: Visual Analogue Scale
- NPRS: Numeric Pain Rating Scale
- Testing muscular Strength: It’s critical to conduct muscular strength testing in the most objective manner feasible. Using a force platform to test the gastrocnemius and soleus muscles is one way to go about this. The distinction is whether you evaluate strength while seated or while standing. The assessment yields the maximum force as well as the force growth rate, which may occur at 150 or 300 ms.
Summary:
- Although a strain is frequently the source of calf muscle pain, other disorders such as deep vein thrombosis and Achilles tendinopathy or rupture can also produce similar symptoms. Healing durations can vary significantly depending on the degree of the strain and each patient’s reaction to treatment.
- Rest with Medical treatment combined with a gradual pain-free exercise regimen mostly recovers from the grade I and II strains, surgery is still required for ruptures. Exercises focusing on strength and conditioning are crucial for reloading the tissues and encouraging activity again.
FAQ:
What’s the healing time for a strain in the calf?
The muscle retains much of its typical strength and range of motion despite the small amount of internal blood. The muscle may also be sensitive and experience some slight pain.
What is the sensation of calf strain?
A calf strain is caused by a partial rupture of the gastrocnemius or soleus muscle from the apex of the Achilles tendon. The injury manifests and happens as an abrupt, acute pain at the back of the leg during running, sprinting, or lunging.
Is walking on a strained calf acceptable?
Short walks are beneficial for the mending muscle; nevertheless, stay away from extensive treks and standing for extended periods. To lessen the tension on your calf, go upward on your healthy leg and downward on your damaged leg. If a handrail is available, make use of it.
Can I run if my calf is sore?
Extreme discomfort when engaging in activities for the first two weeks after the accident. Walking, swimming, and cycling are excellent forms of exercise for the mending muscle. Don’t resume any running-related activities, though, until your calf has fully recovered its strength and range of motion.
References:
- Calf pain. (n.d.). causes, treatment, and prevention | healthdirect. https://www.healthdirect.gov.au/calf-pain
- Professional, C. C. M. (n.d.). Pulled Calf Muscle. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21558-pulled-calf-muscle
- Professional, C. C. M. (n.d.-b). Torn Calf Muscle. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21696-torn-calf-muscle
- Holadmin, & Holadmin. (2018, May 15). Calf Strains – Holistic Bodyworks. Holistic Bodyworks -. https://www.holisticbodyworks.com.au/calf-strain/




2 Comments